Abstract
Arsenic is a human carcinogen that occurs ubiquitously in soil and water. Based on epidemiological studies, a benchmark dose (lower/higher bound estimate) between 0.3 and 8 μg/kg bw/day was estimated to cause a 1 % increased risk of lung, skin and bladder cancer. A recently published study by EFSA on dietary exposure to inorganic arsenic in the European population reported 95th percentiles (lower bound min to upper bound max) for different age groups in the same range as the benchmark dose. For toddlers, a highly exposed group, the highest values ranged between 0.61 and 2.09 µg arsenic/kg bw/day. For all other age classes, the margin of exposure is also small. This scenario calls for regulatory action to reduce arsenic exposure. One priority measure should be to reduce arsenic in food categories that contribute most to exposure. In the EFSA study the food categories ‘milk and dairy products,’ ‘drinking water’ and ‘food for infants’ represent major sources of inorganic arsenic for infants and also rice is an important source. Long-term strategies are required to reduce inorganic arsenic in these food groups. The reduced consumption of rice and rice products which has been recommended may be helpful for a minority of individuals consuming unusually high amounts of rice. However, it is only of limited value for the general European population, because the food categories ‘grain-based processed products (non rice-based)’ or ‘milk and dairy products’ contribute more to the exposure with inorganic arsenic than the food category ‘rice.’ A balanced regulatory activity focusing on the most relevant food categories is required. In conclusion, exposure to inorganic arsenic represents a risk to the health of the European population, particularly to young children. Regulatory measures to reduce exposure are urgently required.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Arsenic occurs ubiquitously in soil, rocks and water. In addition, environmental levels of arsenic have been increased by burning of fossil fuels and mining. Arsenic has been used in fertilizers, wood preservatives, insecticides and herbicides, although generally such products containing arsenic are heavily restricted or banned in the EU. One of the largest man-made catastrophes resulted from intake of drinking water which was contaminated with arsenic after new installation of supply wells (Golka et al. 2010). In the 1970s, a WHO-initiated campaign in Bangladesh switched from open dug wells to ground water as source of drinking water (Golka et al. 2010; Ahmad 2001; Bae et al. 2002). The installation of more than 4 million wells reduced waterborne diseases due to microbiologically contaminated water. However, geogenic well-water contamination with high arsenic concentrations resulted in toxicological risks. As a consequence of the WHO initiative, more than 50 million people in Bangladesh were put at risk of arsenic-induced diseases (Ahmad 2001; Golka et al. 2010; Bae et al. 2002; Khan et al. 2003). At least 100,000 people have been reported to suffer from cancerous skin lesions caused by arsenic (Golka et al. 2010), and the actual numbers may even be much higher. The man-made catastrophe led to increased knowledge of the association between oral arsenic exposure and cancer risk. Arsenic is a human group I carcinogen that causes skin, kidney, bladder and lung tumors (IARC 1973, 1980, 2004, 2012). Based on epidemiological studies, a benchmark dose between 0.3 and 8 µg/kg body weight/day was estimated to result in a 1 % increased risk of lung, skin and bladder tumors in humans (EFSA CONTAM Panel, 2009). Similarly, the Joint FAO/WHO Expert Committee on Food Additives (WHO 2011a) calculated that the lower benchmark dose that resulted in a 0.5 % increased risk of lung cancer was 3.0 µg/kg body weight/day (range 2–7 µg/kg body weight/day).
Although exposure to arsenic in Europe is much lower than in Bangladesh, the general population may still be exposed to critical levels. A recently published comprehensive study on dietary exposure to inorganic arsenic in the European population gives reasons for concern (EFSA Journal 2014). In this study, mean dietary exposure of arsenic to infants, toddlers and ‘other children’ (aged up to adolescence) ranged from 0.2 to 1.37 μg/kg bw/day. The 95th percentiles were between 0.36 and 2.09 μg/kg bw/day (EFSA 2014). These body doses result in a small or absent margin of exposure between exposure of the European population and the benchmark dose for increased risk of carcinogenesis. Although dietary exposure seems to represent the most relevant route in Europe, for some groups in the population the margin of exposure may also be relatively small when considering intake of drinking water. In Europe the parametric value for arsenic in drinking water is 10 µg/l (Directive 98/83/EC), which corresponds to the provisional guideline value provided by the WHO (WHO 2011b). WHO’s guideline value is designated as provisional on the basis of treatment performance and the level of analytical achievability. The maximum likelihood estimates under the assumption of a mode of action for carcinogenesis without threshold dose and using a linear risk extrapolation for bladder and lung cancer for populations (in the USA) exposed to 10 μg of arsenic per litre in drinking water are 12 and 18 per 10,000 population for females and 23 and 14 per 10,000 population for males, respectively (WHO 2011c). This additional cancer risk is higher than usually accepted for drinking water (1 per 1,000,000). Based on a daily drinking water consumption of 2 l by a person weighing 70 kg, a drinking water concentration of 10 µg/l arsenic equals 0.3 μg/kg bw/day, which is in the range of the aforementioned 1 % benchmark dose of carcinogenesis.
As a result of the relatively high exposure levels of the European population reported by EFSA (2014), the Advisory Board of the German Society of ToxicologyFootnote 1 analyzed the potential risk to human health given by the calculated exposure to arsenic (EFSA 2014).
Toxicological profile and mode of action
Chronic effects of arsenic include skin lesions, neurotoxicity (including developmental neurotoxicity), cardiovascular diseases, diabetes and cancer. The adverse effect with the highest relevance for arsenic risk evaluation is carcinogenicity. Carcinogenic mechanisms of arsenic have already been comprehensively discussed (Beyersmann and Hartwig 2008; Tokar et al. 2010; Bustaffa et al. 2014; Sinha et al. 2013). Briefly, arsenite [more recently also named arsenate(III)] increases the generation of hydrogen peroxide and superoxide anions. A further well-documented mechanism is its interaction with cysteine residues in zinc finger domains. The formation of complexes with arsen(III) species leads to substitution of zinc and, consequently, to changes in structure and loss of protein function (Zhou et al. 2014). A characteristic of proteins with zinc finger domains is their ability to interact with nucleic acids; therefore, this class of proteins is involved in DNA transcription, modification and repair. Moreover, arsenic has been shown to deregulate cell proliferation and induce epigenetic alterations such as altered methylation patterns of promoters, leading to gene expression alterations (review: Bustaffa et al. 2014) and suppression of P53. Arsenic does not cause point mutations, but induces micronuclei, chromosomal aberrations and DNA strand breaks (review: Beyersmann and Hartwig 2008). It has been shown that carcinogens and, under certain circumstances, even genotoxic compounds may act by threshold mechanisms (Hengstler et al. 2003). It is possible that arsenic, which is not DNA-reactive and acts by indirect mechanisms (such as reactive oxygen generation and DNA repair inhibition), may work by a ‘practical/apparent threshold’ mechanism (Bolt et al. 2004). However, it is not yet entirely clear which of the variety of mechanisms induced by arsenic prevail in the carcinogenic process (Beyersmann and Hartwig 2008; WHO 2011c). Hence, considering the variety of mechanisms, it is difficult to conclude whether arsenic acts by a threshold mechanism with the possibility deriving a safe level or whether a safe level cannot be determined. In this situation, it may be reasonable to accept the no-threshold assumption and use the conservative ALARA (‘as low as reasonable achievable’) concept for risk management. This concept will be the basis of the following paragraphs in this article. It should, however, be considered that research in future may replace this paradigm for arsenic by a ‘practical/apparent threshold’ concept.
Human exposure
Food analysis often provides total arsenic levels, which comprises both inorganic and organic arsenicals. In general, inorganic arsenic forms exhibit a far higher degree of toxicity compared to naturally occurring organic arsenic forms. Inorganic arsenic in food and drinking water occurs as arsenate (iAsV) or as arsenite (iAsIII). In organisms, the majority of iAsV is converted to iAsIII (Watanabe and Hirano 2013); therefore, both forms are usually not differentiated during risk evaluation. By contrast, fish and seafood contain high amounts of organic forms of arsenic, such as arsenobetaine and arsenocholine (Watanabe and Hirano 2013). Among arsenic in organic forms, arsenobetaine is most abundant, but various arsenosugars and arsenolipids may also occur (Francesconi 2010). Arsenobetaine is not metabolized in humans and is thus considered to be of minor toxicological relevance. The potential risk of arsenosugars and arsenolipids in seafood is less clear. These forms are metabolized to dimethylarsinate, which is the major metabolite generated after intake of inorganic arsenic. It is unknown whether toxicologically relevant intermediates appear; however, limited data on arsenosugars indicate low toxicity. Data on the toxicity of arsenolipids are lacking (Francesconi 2010). Taken together, a major fraction of arsenic in seafood does not seem to be toxicologically relevant, although there is some scientific concern and a need for further clarification.
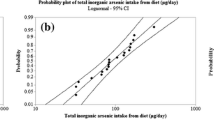
Recently, EFSA has provided data on human exposure based on 103,773 food samples (including drinking water) in order to obtain an overview of the chronic dietary exposure to arsenic in Europe and on the main food sources of exposure (EFSA 2014). From the totality of measurements, 2753 samples refer to inorganic arsenic, while for the remainder (101,020 samples) the reported total arsenic was converted by EFSA to inorganic arsenic by applying appropriate conversion factors. The estimate of dietary exposure to iAs resulted in the highest value in the younger population. Across the different surveys, the mean dietary exposure in the young age groups (infants, toddlers and other children) ranged from 0.20 to 0.45 μg/kg bw/day for the minimum to the maximum lower bound estimate and from 0.47 to 1.37 μg/kg bw/day for the minimum to the maximum upper bound estimate, with the maximum value estimated in infants. For the 95th percentile, the minimum to the maximum lower bound estimate ranged from 0.36 to 1.04 μg/kg bw/day and the minimum to the maximum upper bound estimate from 0.81 to 2.09 μg/kg bw/day, with the highest level estimated in toddlers. In the adult population, the mean dietary exposure to iAs was in the range between 0.09 and 0.38 μg/kg bw/day (minimum lower bound to maximum upper bound), and between 0.14 and 0.64 μg/kg bw/day (minimum lower bound to maximum upper bound) for the 95th of the dietary exposure.
According to the EFSA report (2014), the main contribution to the dietary exposure to iAs comes from the food group ‘grain-based processed products’ (non rice-based) in most of the age groups in the population, with the exception of infants and toddlers. In all age classes, further important contributors were rice, milk and dairy products as well as drinking water (Fig. 1a–c). In infants and toddlers (Fig. 1a, two upper panels), milk and dairy products were the main contributors and drinking water was also an important contributor. Uncertainty comes from the fact that it is not known how much rice is used in infant food. For example, three portions (90 g/day) of rice-based infant food could represent an important source of iAs (1.59–1.96 μg/kg bw/day).
Main food groups contributing to mean chronic dietary exposure of inorganic arsenic in a European population. The x-axis shows the percentage contribution. Information is given separately for individual age groups (from EFSA 2014). a Infants and toddlers, b other children, c adults
Exposure is mainly driven by the consumption levels and not because of high concentrations with the exception of rice which may have remarkably high contents. In particular ‘grain-based processed products (non rice-based)’ made a large contribution to the overall exposure to iAs because of the high consumption. Wheat bread and rolls were the most dominant contributors to iAs exposure within ‘grain-based processed products (non rice-based).’ The arsenic concentrations measured in rice and rice products were high, 95th percentile of the concentration being 250 µg arsenic per kg for some brown rice species (Table 2). In general, brown rice contains more arsenic than white rice because of the relatively high content in the husks. The high arsenic content is due to the ability of rice roots to take up arsenic which is in the soil through polluted irrigation water and through historic contamination with As-based pesticides (Abedin et al. 2002a, b). Currently, modified rice plants with a lower propensity to take up arsenic represent a cutting-edge topic in plant research (Wang et al. 2015; Li et al. 2014). However, improved alternatives to currently used rice plants are not yet available.
Necessity of regulatory activities to reduce inorganic arsenic exposure of the general population
When the mean and 95th percentile dietary exposure published by EFSA are compared with benchmark doses of extra cancer risk, an overlap can be observed between the mean exposure and the lower confidence limit of the 1 % benchmark dose (Table 1). The situation is particularly critical for the younger population; however, the margin of exposure is also small or even non-existent for all other age classes. In conclusion, the European population is exposed to doses of arsenic that can be assumed to contribute to the background cancer risk.
Because of relatively high concentrations of arsenic in rice compared to other food sources, it may be tempting to recommend reduced consumption of rice and rice products to consumers, as recently suggested by the German Federal Institute for Risk Assessment (BfR 2015). However, perhaps the most important finding of the EFSA study (2014) is that it demonstrated that a reduced consumption of rice and rice products is of only limited value for the European population. Therefore, consuming rice and rice-based products ‘in moderation and varying these products with products based on other cereals’ (BfR 2015) is a valid recommendation but will only have a moderate influence on total arsenic exposure for the average consumer. The reason for the moderate contribution of rice to overall arsenic exposure is its relatively low contribution to the average total European diet. Nevertheless, it may be a relevant message to consumers, currently consuming high amounts of rice and rice products.
Besides reducing consumption, one further step in reducing arsenic exposure would be the introduction of threshold values for food, in which extremely high arsenic concentrations have been observed. Besides rice, a further example can be taken from the EFSA study (2014) which is seaweed, with concentrations of inorganic arsenic up to 448 µg/kg. Likewise, dietary supplements based on algae were analyzed and found to contain 6134 µg/kg inorganic arsenic. Even though these food groups contribute little to overall human exposure, the extreme concentrations seem to be unjustifiable and such products with high contents of inorganic arsenic should no longer be allowed on the market. It is important that binding threshold values in food groups are introduced beginning with the food groups contributing most to the exposure.
A particularly difficult challenge is the regulation of arsenic in rice, which is not of highest priority for the general population in Europe. Of course, the situation is different in Asian countries. China, where rice contributes more to total diet, has introduced a threshold value of 150 µg arsenic/kg rice. However, a consequence of implementation of this threshold would be that a relatively high fraction of currently sold brown rice would have to be discarded, considering their reported arsenic content in the EFSA analysis (Table 2). For scientific reasons, the ALARA principle should be applied; however, it may be difficult to achieve a consensus on what should be considered as ‘reasonable’ (‘R’). A transient compromise might be to first introduce different threshold values for white and red/brown rice if the 150 µg/kg threshold is unsustainable. However, rice-based products intended as food for infants and young children should be strictly regulated because of the already very high overall exposure of arsenic to children.
Another relevant aspect is the regulation of arsenic in drinking and mineral water. Mean inorganic arsenic concentrations of tap water range between 1.1 and 2.0 µg/l, and the 95th percentiles were between 5.7 and 5.8 µg/l (EFSA 2014). This is a pleasing achievement considering the established limit value of 10 µg/l for drinking water. Since drinking water represents an important contribution to overall arsenic exposure (Fig. 1), it should be discussed whether the 10 µg/l threshold should be reduced. The authors are aware of regions in Italy where arsenic in drinking water is relatively high (Cubadda et al. 2015). Notably, an increased incidence of cancer cases has been observed in this region (DIEP 2014). Reduction in the threshold would be challenging in this region at least within a short time (Cubadda et al. 2015). Therefore, it is important to search for technical solutions to reduce arsenic in drinking water, which may be achieved by water pipelines from less contaminated regions or by filters.
The highest mean occurrence of inorganic arsenic was found in still mineral waters, with mean estimated concentrations of 5.8 µg/l (medium bound). Although 93 % of the mineral water samples were below the 10 µg/l threshold (EFSA 2014), some samples were in the range of 200 µg/l, which increased the mean. For natural mineral waters, a maximum level of 10 µg/l is stipulated for total arsenic (tAs) (Directive 2003/40/EC). Clearly, exceeding levels are not tolerated. Data on the quality of drinking water in Europe reported by the national authorities for 2008–2010 (http://ec.europa.eu/environment/water/water-drink/pdf/report2014/1_EN_ACT_part1_v3.pdf) showed for large supplies that the vast majority of member states are in compliance with the requirements for arsenic. Regional elevated arsenic levels in drinking water have been reported, e.g., by Hungary where non-compliance was mainly observed in the deep groundwater of the southeastern Great Plains. Germany’s report (2015) on drinking water quality for years 2011–2013 shows only marginal deviations from arsenic’s parametric value in the range of 0.1 % (2011) of the analyzed samples. In addition, further activities should be undertaken to reduce substantially the exposure toward arsenic focusing on the most relevant food categories. Those activities will require long-term planning, and some proposals are discussed in the following sections.
The dietary exposure overview of the EFSA (Fig. 1) offers a basis to develop strategies for efficiently reducing exposure of the general population to arsenic. Our considerations start with the observation that exposure scenarios are complex with many contributing food categories; hence, rather than a focus on one specific food category, a balanced reduction in the main sources of exposure seems to be an efficient strategy. The primary approach should be to reduce arsenic in the food groups contributing most to the exposure in a specific age group. For example, infants will benefit most from a reduction of arsenic in milk and dairy products, food for infants and drinking water (Fig. 1a). Reduced arsenic in ‘grain-based processed products (non rice-based)’ would be particularly helpful for adults (Fig. 1c).
A long-term strategy is required to reduce arsenic in these food groups. This is only feasible by reducing the arsenic concentration in soil and water where the agricultural products are grown. This would require evaluating concentrations of arsenic in agricultural products in order to be able to identify specific regions of interest where measure should be taken to reduce the arsenic load. Additionally, the most contaminated products should be identified and measures taken to avoid their consumption. Because of logistic challenges and high costs, these measures to reduce arsenic in food will be a long-term and stepwise process and harmonization of regulating actions will be challenging.
Risk management discussions
The new EFSA exposure study (Table 1) gives a differentiated overview of current exposure of the general European population to inorganic arsenic. However, the problem of the small or even absent margin between arsenic exposure and carcinogenic doses is not a new fact. Nevertheless, until now, the authorities have not yet introduced binding threshold values for the major sources of arsenic.
The authors can understand that the relatively high costs would be an obstacle to reduction measures that would be required and that logistic challenges have to be mastered. Currently, many foods are produced in a way that inherently causes them to contain relatively high arsenic concentrations. The most widespread reason for this is that arsenic in water and soil is taken up by agricultural plants. Agricultural production in which soil and water with high arsenic concentrations is avoided, or the introduction of agricultural crops which accumulate less arsenic represent challenging long-term projects. Unfortunately, rapid improvements will be logistically difficult and relatively expensive. Long-term strategies should be established and will be a driving force for reducing arsenic in foods, for example, by introducing binding threshold values in food that will be reduced in a stepwise fashion over several years. It should be considered that the Commission Regulation (EU) 2015/1006 of 25 June 2015 has taken a step forward in issuing that a limit value of 0.1 mg/kg for rice destined for the production of foods for infants and young children will come into force from January 1, 2016.
Moreover, efforts to inform the consumers should be increased as there is relatively little awareness in the general population that current exposure to arsenic is critical. This may be explained by the fact that arsenic occurs ‘naturally’ in soil as well as water and the knowledge that humans have been poisoned by arsenic since millennia. The oldest scientifically testified environmental exposure to arsenic is the Tyrolean Neolithic mummy, ‘Ötzi,’ who died between 3359 and 3105 BC (review; Bolt 2012). Hair analysis of ‘Ötzi’ demonstrated high arsenic contents of 44 µg/g hair, which is much higher than that of contemporary non-exposed reference populations (0.116–0.141 µg As/g hair). Evidence suggests that ‘Ötzi’ was involved in copper working, which involved high exposure to arsenic (Bolt 2012). Other historical examples of arsenic exposure include women who used arsenic to enhance their skin beauty, horses which were given arsenic to produce a gleaming coat and athletes who used it for doping. Such examples may have desensitized risk perception.
Nevertheless, the risk to the general population is real. The authors hope that this commentary helps to draw attention to the very real health problems caused by arsenic and bring about scientifically justified additional regulations to reduce human exposure.
Notes
The Advisory Committee of the German Society of Toxicology is elected by the members of the German Society of Toxicology and consists of representatives from academia, industry and administration in order to guarantee a broad range of toxicological competence. The Advisory Committee presents and justifies its activities to the members of the German Society of Toxicology, for example at the yearly plenary meeting. The German Society of Toxicology is the largest scientific toxicological organization in Europe, with more than 1200 members. In the past 10 years, the Advisory Committee has already published review articles about nanotoxicology (Gebel et al. 2014), bisphenol A (Hengstler et al. 2011), alternative methods to animal experiments (Lilienblum et al. 2008) and REACH (Hengstler et al. 2006). Commentaries to arsenic have not yet been published by the Advisory Board.
References
Abedin MJ, Cresser MS, Meharg AA, Feldmann J, Cotter-Howells J (2002a) Arsenic accumulation and metabolism in rice (Oryza sativa L.). Environ Sci Technol 36(5):962–968
Abedin MJ, Feldmann J, Meharg AA (2002b) Uptake kinetics of arsenic species in rice plants. Plant Physiol 128(3):1120–1128
Ahmad K (2001) Report highlights widespread arsenic contamination in Bangladesh. Lancet 358:133
Bae M, Watanabe C, Inaoka T, Sekiyama M, Sudo N, Bokul MH, Ohtsuka R (2002) Arsenic in cooked rice in Bangladesh. Lancet 360(9348):1839–1840 (Erratum in: Lancet. 2002 Mar 22;361(9362):1060)
Beyersmann D, Hartwig A (2008) Carcinogenic metal compounds: recent insight into molecular and cellular mechanisms. Arch Toxicol 82(8):493–512
BfR (2015) Rice and rice products contain high levels of inorganic arsenic. 14/2015, 11.06.2015
Bolt HM (2012) Arsenic: an ancient toxicant of continuous public health impact, from Iceman Ötzi until now. Arch Toxicol 86(6):825–830
Bolt HM, Hengstler JG (2011) Most cited articles: ethanol-induced hepatotoxicity, anticarcinogenic effects of polyphenolic compounds in tea, dose-response modeling, novel roles of epoxide hydrolases and arsenic-induced suicidal erythrocyte death. Arch Toxicol 85(12):1485–1489
Bolt HM, Foth H, Hengstler JG, Degen GH (2004) Carcinogenicity categorization of chemicals-new aspects to be considered in a European perspective. Toxicol Lett 151(1):29–41
Bustaffa E, Stoccoro A, Bianchi F, Migliore L (2014) Genotoxic and epigenetic mechanisms in arsenic carcinogenicity. Arch Toxicol 88(5):1043–1067
Chen JG, Chen YG, Zhou YS, Lin GF, Li XJ, Jia CG, Guo WC, Du H, Lu HC, Meng H, Zhang XJ, Golka K, Shen JH (2007) A follow-up study of mortality among the arseniasis patients exposed to indoor combustion of high arsenic coal in Southwest Guizhou Autonomous Prefecture, China. Int Arch Occup Environ Health 81(1):9–17
Chen JG, Lin GF, Chen YG, Jia CG, Zhou YS, Meng H, Guo WC, Golka K, Liu KJ, Shen JH (2009) Arseniasis prevalence and mortality in a multiethnic, endemic township in Guizhou, China. Int Arch Occup Environ Health 82(4):499–508
Commission Directive 2003/40/EC of 16 May 2003 establishing the list, concentration limits and labelling requirements for the constituents of natural mineral waters and the conditions for using ozone-enriched air for the treatment of natural mineral waters and spring waters. Off J L 126:0034–0039. (22/05/2003)
Commission regulation (EU) 2015/1006 of 25 June 2015 amending regulation (EC) No. 1881/2006 as regards maximum levels of inorganic arsenic in foodstuff
Cubadda F, D’Amato M, Mancini FR, Aureli F, Raggi A, Busani L, Mantovani A (2015) Assessing human exposure to inorganic arsenic in high-arsenic areas of Latium: a biomonitoring study integrated with indicators of dietary intake. Ann Ig 27(1):39–51. doi:10.7416/ai.2015.2021
DIEP (2014) (Dipartimento di Epidemiologica del Servizio Sanitario Regionale Regio Lazio) Valuazione Epidemiologica delli effeti sulla salute in relazione alla contaminazione de arsenic nelle acque potabili. Studio di coorate di mortalità nellepopulazione resindente in provincia di Viterbo, 1990–2010. https://www.google.com/search?q=valutazione+epidemiologica+degli+effetti+sulla+salute
EFSA (2005) Opinion of the scientific committee on a request from EFSA related to a harmonised approach for risk assessment of substances which are both genotoxic and carcinogenic. EFSA J 282:1–31
EFSA (2014) Dietary exposure to inorganic arsenic in the European population. EFSA J 12(3):3597. doi:10.2903/j.efsa.2014.3597
EFSA Contam Panel (EFSA Panel on Contaminants in the Food Chain) (2009) Scientific Opinion on Arsenic in Food. EFSA J 7(10):1351
Francesconi KA (2010) Arsenic species in seafood: origin and human health implications. Pure Appl Chem 82(2):373–381
Gebel T, Foth H, Damm G, Freyberger A, Kramer PJ, Lilienblum W, Röhl C, Schupp T, Weiss C, Wollin KM, Hengstler JG (2014) Manufactured nanomaterials: categorization and approaches to hazard assessment. Arch Toxicol 88(12):2191–2211
Germany’s report 2015 (2015) Bericht des Bundesministeriums für Gesundheit und des Umweltbundesamtes an die Verbraucherinnen und Verbraucher über die Qualität von Wasser für den menschlichen Gebrauch (Trinkwasser) in Deutschland. http://www.umweltbundesamt.de/publikationen/
Golka K, Hengstler JG, Marchan R, Bolt HM (2010) Severe arsenic poisoning: one of the largest man-made catastrophies. Arch Toxicol 84(8):583–584
Hengstler JG, Bogdanffy MS, Bolt HM, Oesch F (2003) Challenging dogma: thresholds for genotoxic carcinogens? The case of vinyl acetate. Annu Rev Pharmacol Toxicol 43:485–520
Hengstler JG, Foth H, Kahl R, Kramer PJ, Lilienblum W, Schulz T, Schweinfurth H (2006) The REACH concept and its impact on toxicological sciences. Toxicology 220(2–3):232–239
Hengstler JG, Foth H, Gebel T, Kramer PJ, Lilienblum W, Schweinfurth H, Völkel W, Wollin KM, Gundert-Remy U (2011) Critical evaluation of key evidence on the human health hazards of exposure to bisphenol A. Crit Rev Toxicol 41(4):263–291
IARC (International Agency for Research on Cancer) (1973) Arsenic and inorganic arsenic compounds. In: Some inorganic and organometallic compounds, vol. 2. IARC Monographs on the Evaluation of Carcinogenic Risk of Chemicals to Humans, International Agency for Research on Cancer, Lyon, France, pp 48–73
IARC (International Agency for Research on Cancer) (1980) Arsenic and arsenic compounds. In: Some metals and metallic compounds, vol. 23. IARC Monographs on the Evaluation of Carcinogenic Risk of Chemicals to Humans, International Agency for Research on Cancer, Lyon, France, pp 39–141
IARC (International Agency for Research on Cancer) (2004) Arsenic and arsenic compounds. In: Some drinking water disinfectants and contaminants, including arsenic, vol 84. IARC Monographs on the Evaluation of Carcinogenic Risk of Chemicals to Humans, pp 239–270
IARC (International Agency for Research on Cancer) (2012) Arsenic and arsenic compounds. In: Arsenic, metals, fibres and dusts, vol 100C. IARC Monographs on the Evaluation of Carcinogenic Risk of Chemicals to Humans, pp 41–94
JECFA (Joint FAO/WHO Expert Committee on food additives) (2010) 72nd meeting. Summary and Conclusions, issued 16th March 2010
Khan MM, Sakauchi F, Sonoda T, Washio M, Mori M (2003) Magnitude of arsenic toxicity in tube-well drinking water in Bangladesh and its adverse effects on human health including cancer: evidence from a review of the literature. Asian Pac J Cancer Prev 4(1):7–14
Li J, Dong F, Lu Y, Yan Q, Shim H (2014) Mechanisms controlling arsenic uptake in rice grown in mining impacted regions in South China. PLoS One 9(9):e108300
Lilienblum W, Dekant W, Foth H, Gebel T, Hengstler JG, Kahl R, Kramer PJ, Schweinfurth H, Wollin KM (2008) Alternative methods to safety studies in experimental animals: role in the risk assessment of chemicals under the new European Chemicals Legislation (REACH). Arch Toxicol 82(4):211–236
Lin GF, Du H, Chen JG, Lu HC, Guo WC, Meng H, Zhang TB, Zhang XJ, Lu DR, Golka K, Shen JH (2006) Arsenic-related skin lesions and glutathione S-transferase P1 A1578G (Ile105Val) polymorphism in two ethnic clans exposed to indoor combustion of high arsenic coal in one village. Pharmacogenet Genom 16(12):863–871
Lin GF, Du H, Chen JG, Lu HC, Kai JX, Zhou YS, Guo WC, Zhang XJ, Lu DR, Golka K, Shen JH (2007) Glutathione S-transferases M1 and T1 polymorphisms and arsenic content in hair and urine in two ethnic clans exposed to indoor combustion of high arsenic coal in Southwest Guizhou, China. Arch Toxicol 81(8):545–551
Lin GF, Meng H, Du H, Lu HC, Zhou YS, Chen JG, Golka K, Lu JC, Shen JH (2010a) Factors impacting on the excess arseniasis prevalence due to indoor combustion of high arsenic coal in a hyperendemic village. Int Arch Occup Environ Health 83(4):433–440
Lin GF, Du H, Chen JG, Lu HC, Guo WC, Golka K, Shen JH (2010b) Association of XPD/ERCC2 G23591A and A35931C polymorphisms with skin lesion prevalence in a multiethnic, arseniasis-hyperendemic village exposed to indoor combustion of high arsenic coal. Arch Toxicol 84(1):17–24
Lin GF, Gong SY, Wei C, Chen JG, Golka K, Shen JH (2012) Co-occurrence of arseniasis and fluorosis due to indoor combustion of high fluorine and arsenic content coal in a rural township in northwest China: epidemiological and toxicological aspects. Arch Toxicol 86(6):839–847
Shen JH, Lin GF, Du H, Lu HC, Golka K, Chen JG (2010) Possible involvement of ethnicity and clan consanguinity in the modulation of arseniasis risk in a multiethnic, hyper-endemic village exposed to indoor combustion of high arsenic-content coal. In: Christopher T. Grace (ed) Coal combustion research. Nova Science Publishers
Sinha D, Biswas J, Bishayee A (2013) Nrf2-mediated redox signaling in arsenic carcinogenesis: a review. Arch Toxicol 87(2):383–396
Tokar EJ, Benbrahim-Tallaa L, Ward JM, Lunn R, Sams RL 2nd, Waalkes MP (2010) Cancer in experimental animals exposed to arsenic and arsenic compounds. Crit Rev Toxicol 40(10):912–927
Wang X, Peng B, Tan C, Ma L, Rathinasabapathi B (2015) Recent advances in arsenic bioavailability, transport, and speciation in rice. Environ Sci Pollut Res Int 22(8):5742–5750
Watanabe T, Hirano S (2013) Metabolism of arsenic and its toxicological relevance. Arch Toxicol 87(6):969–979
WHO (World Health Organization) (2011a) Seventy-second report of the Joint FAO/WHO Expert Committee on food additives, In: Evaluation of certain contaminants in food, vol 959. WHO Technical Reports Series, pp 1–105
WHO (World Health Organization) (2011b) Guidelines for drinking-water quality, 4th edn. http://www.who.int/water_sanitation_health/publications/2011/dwq_guidelines/en/
WHO (World Health Organization) (2011c) Arsenic in Drinking-water. Background document for development of WHO Guidelines for Drinking-water Quality. http://www.who.int/water_sanitation_health/publications/2011/arsenic/en/
Zhou X, Sun X, Mobarak C, Gandolfi AJ, Burchiel SW, Hudson LG, Liu KJ (2014) Differential binding of monomethylarsonous acid compared to arsenite and arsenic trioxide with zinc finger peptides and proteins. Chem Res Toxicol 27(4):690–698. doi:10.1021/tx500022j
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
Jan Georg Hengstler is co-author of editorials about arsenic poisoning by contaminated drinking water (Golka et al. 2010) and arsenic-induced suicidal erythrocyte death (Bolt and Hengstler 2011). Klaus Golka is author of the aforementioned editorial and co-author of the following basic research articles and one book chapter on arsenic in Chinese coals in Southwest Guizhou and in Northwest China and its impact on health of the local population: Golka et al. (2010), Lin et al. (2006, 2007, 2010a, b, 2012), Chen et al. (2007, 2009) and Shen et al. (2010). Tom Gebel has spent several years of scientific research on the toxicology of arsenic. In this context, several papers were published as author and as co-author. Part of this work has been financed by European Union research grants. All other authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Gundert-Remy, U., Damm, G., Foth, H. et al. High exposure to inorganic arsenic by food: the need for risk reduction. Arch Toxicol 89, 2219–2227 (2015). https://doi.org/10.1007/s00204-015-1627-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00204-015-1627-1