Abstract
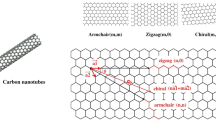
Carbon nanotubes (CNTs) are an important class of nanomaterials, which have numerous novel properties that make them useful in technology and industry. Generally, there are two types of CNTs: single-walled nanotubes (SWNTs) and multi-walled nanotubes. SWNTs, in particular, possess unique electrical, mechanical, and thermal properties, allowing for a wide range of applications in various fields, including the electronic, computer, aerospace, and biomedical industries. However, the use of SWNTs has come under scrutiny, not only due to their peculiar nanotoxicological profile, but also due to the forecasted increase in SWNT production in the near future. As such, the risk of human exposure is likely to be increased substantially. Yet, our understanding of the toxicological risk of SWNTs in human biology remains limited. This review seeks to examine representative data on the nanotoxicity of SWNTs by first considering how SWNTs are absorbed, distributed, accumulated and excreted in a biological system, and how SWNTs induce organ-specific toxicity in the body. The contradictory findings of numerous studies with regards to the potential hazards of SWNT exposure are discussed in this review. The possible mechanisms and molecular pathways associated with SWNT nanotoxicity in target organs and specific cell types are presented. We hope that this review will stimulate further research into the fundamental aspects of CNTs, especially the biological interactions which arise due to the unique intrinsic characteristics of CNTs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Within decades of the discovery of engineered nanomaterials, nanotechnology has shown tremendous potential in multiple industries for the production of electronic, electric, mechanical, construction, and medicinal products. Although a wide variety of nanomaterials have shown promising characteristics for incorporation in industrial applications and products, the potential benefits could be offset by toxic effects, which have already been observed from in vitro and in vivo models that were exposed to nanomaterials (De Jong and Borm 2008; El-Ansary and Al-Daihan 2009).
With the high amount of global investment toward the research and development of nanotechnology in the twenty first century, the CNTs and engineered CNT-reinforced composite materials are made more ready than the past to pave into the real-world applications in multi-sectors such as biomedicine in particular vehicle for therapeutic delivery, radiotherapy and hyperthermia treatment agent (Yang et al. 2007a), tissue engineering scaffold, antimicrobials and biosensors (Zhang et al. 2010), electronics (transistors) (Avouris et al. 2007), nanoelectromechanics (Mahar et al. 2007), constructions (Lee et al. 2010), food industry (packaging) (Azeredo 2009), environmental sustainment (filters, adsorbents, hydrogen storage for fuel cells) (Mauter and Elimelech 2008; Sahaym and Norton 2008), and others. In fact, there is a growing trend of incorporation of CNTs and derivatives into the industrial and consumer products ranging from the advanced electronic equipment and gadgets, automotive parts, sports goods to regular household items at the time of writing (Maynard and Michelson 2006).
Despite such a wide range of applications, the toxicity of carbon nanotubes (CNTs) is of prime concern, with several groups indicating their similarity to asbestos fibers (Poland et al. 2008). However, many studies also suggest that such attributes in CNT toxicity are unfounded (Huczko and Lange 2001; Huczko et al. 2001; Pantarotto et al. 2003; Schipper et al. 2008; Zhao et al. 2008). These inconsistencies seem to arise because of differences in experimental settings. Although some points of view have been reconciled, most aspects of CNT toxicity remain uncertain. Indeed, the complexity of CNT toxicity in both in vivo and in vitro studies has been attributed to various intrinsic factors including length, type of functionalization, concentration/dosage, duration of exposure, method of exposure, and even the dispersant used to solubilize the nanotubes.
This review aims to synthesize and further analyze representative data on the nanotoxicity of SWNTs by first considering how SWNTs are absorbed, distributed, accumulated, and excreted in a biological system, and subsequently, how SWNTs induce organ-specific toxicity in the body. A re-evaluation of these studies reveals new insights and toxicological paradigms, which can explain the current toxicity profile of SWNTs, particularly in terms of issues such as cell-type-specific effects, mechanism of cell injury, and organ-specific toxicity.
Toxicokinetics of SWNTs
Understanding of the kinetics SWNTs upon entry into the body may help researchers qualify and quantify potential tissue-specific impacts. However, systemic biodistribution or toxicokinetic profiling of pristine SWNTs is far from complete. Efforts to elucidate the toxicokinetics of SWNTs are further complicated by the number of variables which affect SWNT toxicity. Several of these factors are described in this section.
Routes of exposure
Unlike MWNTs, which are more ubiquitously distributed in the environment from natural or anthropogenic combustion processes, SWNTs are exclusive in availability, which can be attributed to the fact that transition-metal catalysts are required for SWNT synthesis (Bang et al. 2004; Lam et al. 2006; Murr 2008; Murr et al. 2004, 2005; Tang et al. 2005). Therefore, people who work in manufacturing facilities and laboratories are at higher risk of chronic inhalation exposure to the as-grown material. Owing to their lightweight characteristics, pristine SWNT powders are easily dispersed in air and deposited on horizontal surfaces, such as bench tops and exposed skin, during manipulations such as material transfer, vortexing, and ultrasonication (Lam et al. 2004, 2006). Inhalation and dermal contact are therefore of great concern as the major route of SWNT uptake in the occupational setting.
Indeed, a number of studies have shown that a significant amount of airborne particulates is released during tip sonication, as well as during weighing and transferring (Johnson et al. 2010). The airborne concentration of SWNTs is estimated to be ≤53 μg/m3 under careful handling during small-scale production processes. At the maximum concentration, the workers could reach a total lung burden of 5–10 g of SWNTs within 1–2 years of working with the materials (Maynard et al. 2004).
However, workers may be exposed to a larger amount of SWNTs through dermal contact rather than the respiratory route. Analysis of the gloves worn by workers that handled SWNTs from four sites demonstrated an estimated dermal load of ≈0.2–6 mg SWNTs per hand after each session of material handling (Maynard et al. 2004). With dimensions similar to that of a virus, SWNTs may be translocated to any tissue or organ in the body where they can interact with various cellular components away from the site of deposition.
Biodistribution, accumulation, and excretion of SWNTs
Despite the recognition of dermal and inhalation routes as major pathways through which SWNTs can enter the human body, the biodistribution of SWNTs is underexplored. Toxicokinetic investigations of pristine SWNTs associated with gastrointestinal (GI) tract entry are also lacking.
Several reports about the biodistribution of SWNTs have been reported based on intravenous administration into mammalian models. For instance, near-IR fluorescence spectroscopy and histopathological findings by Cherukuri et al. (2006) demonstrated fast clearance (half-life, t 1/2 ≈ 1 h) from the systemic circulation and significant accumulation of pristine SWNTs dispersed in 1 % Pluronic F108 (75 μg/animal) between 0.5 and 24 h after injection (Cherukuri et al. 2006). The uptake of SWNTs in the reticuloendothelial system (RES) was also evident in an early study by Yang et al. (2007a, b), whose results demonstrated significant accumulation of the 13C-tagged SWNTs in the lung (≈90 % injected dose per gram tissue, ID/g), liver (≈17 % ID/g), and spleen (≈15 % ID/g) of mice 1 day after exposure (200 μg/animal) (Yang et al. 2007b). A decreased SWNT burden in the lung and liver was observed 7 and 28 days after exposure, whereas the SWNT concentration in the spleen increased over the same period (Yang et al. 2007b). Contrary to the findings reported by Cherukuri et al. (2006), the study by Yang et al. (2007a, b) did not recover SWNTs in the urinary or fecal excretions (Cherukuri et al. 2006; Yang et al. 2007b). Such discrepancies could be attributed to the fact that the SWNTs used in Yang’s experiment were aggregates with diameters estimated to be between 10 and 20 nm, which is in contrast to the SWNTs administered by Cherukuri et al. (2006) that were shown to be well dispersed and remained as individual tubes in vivo (Cherukuri et al. 2006; Yang et al. 2007b).
In a separate study, Singh et al. (2006) administered 111In-labeled diethylenetriaminepentaacetic acid (DTPA) functionalized SWNTs, with and without free amine groups, to mice (60 μg/animal) intravenously (Singh et al. 2006). After 30-min exposure, both functionalized SWNTs, with and without free amine groups, partitioned into different organs in the following order: muscle > skin > blood > kidney. They reported a slightly longer half-life (t 1/2) of ≈3 h for [111In]DTPA-SWNTs with the free amine groups and ≈3.5 h for [111In]DTPA-SWNTs without the free amine groups. Furthermore, a more efficient renal clearance was observed when administered at high dose (completely excreted 18 h after exposure to 400 μg/animal) (Singh et al. 2006). The half-life reported by Singh et al. (2006) is considerably longer than the amine-functionalized radio-tagged SWNTs reported by McDevitt et al. (2007b) in a mouse model, where only <3 % ID/g of conjugates was detected in blood 1-h post-injection, and all of the constructs were cleared into urine within a few hours of exposure (McDevitt et al. 2007b; Singh et al. 2006). Cherukuri et al. (2006) argued that one time point might have been missed in the calculation, leading to a prolonged blood half-life in the study by Singh et al.; however, it is also possible that the result could be attributed to the aggregation of radio-labeled SWNTs (estimated diameter 13–39.5 nm), compared with those individual nanotubes used by McDevitt et al. (2007b) with a diameter ≤10 nm (Cherukuri et al. 2006; McDevitt et al. 2007b; Singh et al. 2006). Conversely, the fast renal excretion of SWNTs with high molecular weight, exceeding the maximum size of molecules that can pass through glomerular filtration, also raised questions by McDevitt et al. (2007a). This suggested that the detected [111In] activity could have been independent of the SWNTs and instead could be attributed to the detachment and instability of DTPA binding (McDevitt et al. 2007a).
In a comparative study into the biodistribution of SWNTs non-covalently functionalized with phospholipid–PEG (PL–PEG) and labeled with 64CuCl2 in mice, Liu et al. (2007) described the high uptake of short-chain PEGylated SWNTs by the liver (≈30–40 %), with a shorter blood circulation half-life (t 1/2 = 0.5 h) and a higher in vivo retention of the total 64Cu radioactivity (≈80 %) relative to SWNTs functionalized with long-chain PEG (≈20 % liver uptake, t 1/2 = 2 h, ≈70 % of the total radioactivity retained in vivo) 1 day after injection (Liu et al. 2007). The results obtained by Liu et al. (2007) suggest a significant retention of the functionalized SWNTs solely in the liver, which could result from the appended surface chemical groups and small dimension of the well-exfoliated SWNTs. Hence, functionalization of SWNTs with longer appended functional groups may help to prolong circulation half-life and reduce non-specific accumulation in the body (Liu et al. 2007).
A murine biodistribution study by Villa et al. (2008) also suggested the predominant accumulation of short SWNTs, with negatively charged surfaces, in the liver and kidney (Villa et al. 2008). Their results showed that 1 h after injection, the 111In-labeled SWNT conjugated with 1,4,7,10-tetraazacyclododecane-1,4,7,10-tetraacetic acid (DOTA), and phosphorothioate backbone modified DNA oligonucleotides (ODNFAM) was present in significant abundance in the liver (≈23 % ID/g), kidney (≈23 % ID/g), and spleen (≈7 % ID/g). After 24 and 96 h, the SWNT retention in kidney and liver decreased to two-thirds of the concentration at 1-h post-exposure, whereas the number of SWNTs in the spleen remained unchanged (Villa et al. 2008).
In a study by McDevitt et al. (2007a), it was found that SWNTs with more negatively charged surface (i.e., attached with more DOTA moieties) demonstrated less non-specific retention in the organs (McDevitt et al. 2007a). Indeed, the predominant distribution sites of radio-labeled DOTA-functionalized SWNTs (diameter 1–20 nm, mean length ≈40 nm) were the kidney (specifically in the renal cortex), liver, and spleen, according to whole-body PET and CT images taken 3 and 24 h after intravenous (i.v.) and intraperitoneal (i.p.) injection into mice (12 µg/mice) (McDevitt et al. 2007a). Their results showed that the i.p.-injected SWNTs were not so widely distributed in the liver and spleen compared with the i.v.-administered constructs (reduced by 40–50 %), indicating slow dissipation of the constructs from the peritoneal region. Remarkably, the SWNTs that entered through both pathways demonstrated faster clearance from the kidney but slower dissipation from the liver and spleen. The results also showed that the SWNTs in the blood were beginning to be excreted into the urine 1 h after injection, and ≈0.4 % ID/g of the constructs remained in the blood 20-h post-injection (McDevitt et al. 2007a). The mechanism of renal excretion, however, remains unknown.
Ligand–receptor binding might play an important role in biodistribution when the SWNTs are conjugated to target a specific ligand. 24 h after injection of radiolabel-functionalized SWNTs into mice bearing disseminated lymphoma (where the tumor tissues were in the bone marrow, spleen, kidney, and liver; listed in order of tumor abundance), McDevitt et al. (2007b) described predominant distribution of the specific targeting antibody-conjugated SWNTs (CNT-[111In]DOTA-Rituximab) in the liver (≈48 % ID/g), spleen (≈21 % ID/g), kidney (≈10 %ID/g), and, to a lesser extent, bone (femur, ≈5 % ID/g) (McDevitt et al. 2007b). Importantly, no such accumulation was detected in the non-tumor-bearing mice, suggesting specific binding of the antibody-conjugated SWNT to the lymphoma cells. Modest retention, however, was also observed in tumor-bearing mice administered with non-specific targeting construct (CNT-[111In]DOTA-Lintuzumab) and a control (CNT-NH2-[111In]DOTA), whereas only low retention of the non-specific targeting constructs was observed in the tumor-free mice. Although the target organs with tumor infiltration coincided with those that are prone to SWNT retention in normal mice models, as seen in reports by Cherukuri et al. (2006), Yang et al. (2007a, b), and Singh et al. (2006), differential uptake in tissues for tumor-bearing and non-tumor-bearing mice administered with specific targeting antibody-coated SWNTs strongly suggested that the localization of SWNTs in RES organs and kidneys was likely caused by Rituximab-CD20 binding, rather than non-specific distribution (Cherukuri et al. 2006; Singh et al. 2006; Yang et al. 2007b).
In summary, the route of exposure, dimension, and surface chemistry of SWNTs are prime factors, which influence the fate of SWNTs in a mammalian body, possibly through moderation of the interaction between blood proteins and the SWNTs (Aggarwal et al. 2009). Overall, the results suggest a tendency of RES-mediated uptake of SWNTs and distribution to systemic organs (liver, spleen, and kidney) once the SWNTs enter into the blood stream. In fact, accumulation of nanoparticles in these organs has been widely reported (Casals et al. 2008; Deng et al. 2007). However, accumulation of SWNTs was also reported in other organs to a small extent, and the potentially long-term effects of which should not be undermined; this could be better justified by knowledge of the dynamics of SWNTs at the cellular, or even the molecular level.
Organ-specific toxicity of SWNTs
Pulmonary toxicity
Simulation of respiratory entry for SWNTs has been complicated by problems such as the dissolution of SWNTs in aqueous solutions and methods of administration in model animals. Several techniques, including intratracheal instillation (ITI), pharyngeal aspiration (PA), intratracheal fast instillation (ITFI), and inhalation, were used by various groups to study SWNT-induced toxicity in the lungs.
Among the earliest studies, Huczko et al. (2001) and Warheit et al. (2004) used ITI for nanotube exposure in the lungs of rodent models, which involved placing a SWNT bolus directly into the lower respiratory tract using a catheter (Huczko et al. 2001; Warheit et al. 2004). Although Huczko et al. (2001) reported negative findings for inflammatory responses and abnormal respiratory function from bronchoalveolar lavage (BAL) cytology and pulmonary function tests in guinea pigs instilled with 25 mg of soot containing SWNTs and MWNTs (Huczko et al. 2001), Warheit et al. (2004) reported severe SWNT-induced toxicity in Sprague–Dawley rats exposed to 5 mg/kg of body weight of SWNTs (30–40 wt% amorphous carbon, 5 wt% Ni, 5 wt% Co, in bundles of ≈30 nm). Some of the SWNT-induced toxicity included transient pulmonary injuries and inflammation, increased neutrophil counts, and increased lactate dehydrogenase (LDH) levels in the BAL (Warheit et al. 2004). The SWNT-instilled rats also developed multifocal granulomas that were observable 1 week after exposure, which transformed to diffused multifocal macrophage-containing granulomas after 1 month; this contained inclusions of macrophage-like multinucleate giant cells centered around or enclosed in the SWNT bolus (Warheit et al. 2004) (Fig. 1). Although the ITI method effectively preserved the dose of particles that was intended to be delivered to the lungs, the rate and distribution of entry of the administered particles deviated from the natural inhalation route. Consequently, the administered particles were unevenly distributed in the lungs, resulting in decreased lung burdens, altered clearance patterns, and the development of a different pathological profile compared with that of intratracheal inhalation of the equivalent dosage (Li et al. 2007a). These phenomena, in addition to the different model organisms, might have affected the early findings (Huczko et al. 2001; Warheit et al. 2004).
Using the PA delivery method, Shvedova et al. (2005) also observed granulomatous inflammation and epitheloid granulomas associated with micrometer-scale SWNT aggregates in the lungs, which were accompanied with collagen and elastin deposited within granulomatous lesions and distant sites, following administration of 10–40 µg of acid-purified HiPco SWNTs (ϕ: 1–4 nm, 0.23 wt% Fe) to the mice (Shvedova et al. 2005). Diffuse interstitial fibrosis and thickening of the alveolar wall were also observed in regions away from the SWNT aggregates (Fig. 1). Importantly, the fibrotic response intensified significantly after 60 days, relative to observations during 28-day post-exposure. The exposure to SWNTs also leads to an early (1-day post-exposure) increase in 4-hydroxy-2-nonenal (4-HNE), a marker for oxidative stress; an increase in proliferation of alveolar type II (AT-II) cells; a likely implication of pulmonary injuries; and an increase in the level of TNFα and IL1β pro-inflammatory cytokines (Shvedova et al. 2005). A dose-dependent increase in the number of polymorphonuclear leukocytes (PMNs) as well as elevated levels of LDH, glutathione (GSH), and γ-glutamyl transferase (GGT) were evidenced 3 days after administration. Although the levels of LDH and GSH increased over the 28 days, the GGT levels continued to increase until 60-day post-exposure (Shvedova et al. 2005). Lymphocytes and macrophages began to infiltrate the lungs 3–7 days after exposure. Fibrogenic TGFβ1 was also found to be increased after 7-day post-exposure, but returned to the control level after 28 days, corresponded to macrophage recruitment. Although the PA approach may also be subject to the bolus effect, similar to that of ITI, the findings of this study showed a clear dose- and time-dependent relationship for the pathological development during the course of experiments. Remarkably, the purified SWNTs administered with doses corresponding to the permission exposure limit (PEL) for graphite defined by OSHA induced lasting inflammatory effects in the lung for up to 2 months; this eventually transformed into interstitial fibrosis, even at regions away from the SWNT deposition area, independent of inflammation. Overall, the results demonstrated a direct relationship between granuloma formation and aspiration of SWNTs.
In a separate study, Lam et al. (2004) investigated the pulmonary toxicity induced by SWNTs using ITFI (Lam et al. 2004). Despite the ITF-employed catheter-assisted tracheal entry of the particles similar to that of the ITI method, the SWNT suspensions were nebulized with the help of a syringe during administration, thus effectively preventing the blockage of the airways by aggregates or a bolus of SWNTs, which could help to generate results with improved physiological relevance. The authors investigated the comparative effects of three SWNT samples with different purity profiles. The mice were intra-tracheally instilled with different doses (0.1 or 0.5 mg per animal) of electric-arc-synthesized SWNTs (25.99 wt% Ni, 5.01 wt% Y, 0.53 wt% Fe), raw HiPco SWNTs (26.9 wt% Fe, 0.78 wt% Ni), or purified HiPco products (2.14 wt% Fe) and were observed at 7- or 90-day post-exposure (Lam et al. 2004). With a concentration of 0.1 mg, there was no mortality, granulomas, or inflammatory lesions in both the 7- and 90-day group. The mice that received a higher dose of similar SWNTs (0.5 mg), however, responded with pathological features (weight loss, sluggishness), interstitial granulomas, and inflammations (two out of four mice in the 7-day group and two out of five mice in the 90-day group), in addition to mortality with pulmonary edema and other histopathological features (two out of four mice in the 7-day group and three out of five mice in the 90-day group died within 4–7 days of the instillation) (Lam et al. 2004). Although there was no mortality reported for raw or purified HiPco SWNTs, mild or abundantly distributed epitheloid granulomas embedded with SWNTs were found in the lungs of treated mice from both of the 7- and 90-day groups that received a low- and high dose of SWNTs, respectively (Lam et al. 2004). Inflammatory lesions were present in the lungs of mice from both of the 90-day groups treated with 0.1 or 0.5 mg of raw or purified HiPco SWNTs. Despite the varying Fe contents in the two HiPco SWNT samples (≈25 % in difference), dose-dependent lung lesions (interstitial granulomas) were consistently observed in the treated mice, suggesting that the development of granulomas was likely to be triggered by the SWNTs rather than the Fe impurities (Lam et al. 2004). In contrast, no granuloma was observed in the lungs of mice treated with the same dosage of carbon black or quartz. The occurrence of interstitial granulomas was inferred to be due to the inadequacy of the macrophage-mucociliary clearance mechanism in the removal of the nanotubes from the lungs. In short, the results demonstrated that the electric-arc- and HiPco-produced SWNTs were more toxic than quartz or carbon black at similar dose of exposure (Lam et al. 2004).
Shvedova et al. (2008) conducted a comparative study on non-purified SWNTs (17.7 wt% Fe, 0.16 wt% Cu, 0.049 % Cr, and 0.046 % Ni) administered by inhalation and PA in C57BL/6 mice (Shvedova et al. 2008). The mice were exposed to SWNTs (ϕ: 0.8–1.2 nm, L: 100–1,000 nm) by inhalation of aerosolized nanotubes (5 mg/m3, 5 h/day, 4 days), which contributed to a total lung burden of 5 μg SWNTs, or PA with 5, 10, and 20 μg of SWNTs. In the aspiration group, the SWNTs induced pronounced and acute inflammatory reactions after 1 day of exposure, which was characterized by a dose-dependent increase in the number of PMNs, elevated level of LDH, release of pro-inflammatory cytokines (TNFα and IL-6), the fibrogenic factor TGF-β, and the accumulation of proteins in the BAL fluid. At 24-h post-inhalation, the mice displayed inflammatory changes similar to that of the aspiration group, with the highest increase in the levels of TNFα and IL-6 during 7 and 28 days after the exposure. This was in addition to a 33.3 % increase in the mutation rate for the K-ras oncogene compared with that of the air-control group (Shvedova et al. 2008). Inhalation of SWNTs also resulted in chronic inflammatory effects, where the number of PMNs, alveolar macrophages, total number of cells, and TGF-β values remained higher than the air-control group throughout the 28-day observation period. Other features, such as bronchiolar epithelial cell hypertrophy (with or without hyperplastic changes), altered breathing mechanics, and oxidative damages represented by decreased protein thiols, increased accumulation of lipid peroxidation product malondialdehyde, reduction of total antioxidant capacity, and an increased number of oxidative modified proteins (i.e., protein carbonyls) persist after 1, 7, and 28 days (Shvedova et al. 2008). Furthermore, 7 and 28 days after inhalation, there was a significant depletion in GSH, the formation of anucleated alveolar macrophages, and a persistent increase in K-ras oncogene mutations compared with the control. In the aspiration group, however, the number of K-ras mutations was almost the same as in the control (Shvedova et al. 2008). 28 days after exposure, both groups of mice, treated by different exposure techniques, showed prominent interstitial fibrosis and evenly distributed granulomas in the lungs, whereas the inhalation group showed a higher amount of collagen deposition and a fourfold increase in fibrosis compared with the aspiration group (Shvedova et al. 2008). These results demonstrate that the inhalation uptake of aerosolized SWNTs produces stronger, acute, and chronic inflammatory reactions in the lungs of mice compared with PA with aggregated SWNTs. In fact, progressive and dose-dependent oxidative damages and interstitial fibrosis were among the major recurrent findings that were observed in most of the pulmonary toxicity studies for SWNTs (Mangum et al. 2006; Park et al. 2011; Shvedova et al. 2005, 2007; Tyurina et al. 2011).
Although overwhelming toxicological data are available for various in vivo models, the extent to which SWNTs are detached into individual fibrous forms from the agglomerates in the human body could not be addressed experimentally. However, incidental inhalation of nanomaterials has been documented in human subjects in a rare case of environmental contamination by SWNTs after the World Trade Center (WTC) disaster, during which the presence of heavy metals, hydrocarbon gases, and a high temperature resulted in the large-scale generation and environmental release of SWNTs. Individualized SWNTs were recovered in lung biopsy samples from four out of seven workers who did not have a history of smoking, but developed serious respiratory symptoms that got worse years after they worked for a particular period at the WTC site (Wu et al. 2010). Furthermore, SWNTs were found in three out of four patients with extensive interstitial pneumonitis, and in one patient with bronchiolitis and pulmonary fibrosis, but not in a patient with non-necrotizing granulomas (Wu et al. 2010). Other dust particles at the WTC site (chrysotile asbestos, magnesium silicate, calcium sulfate, and aluminum silicate) were also extracted from these biopsy samples. Although the association of SWNTs and respiratory symptoms cannot be thoroughly justified in this study, successful retrieval of SWNTs from the lungs of the workers confirmed that the nanomaterial may de-agglomerate and be retained in the body for an extended period of time.
Cardiac toxicity
Li et al. (2007b) showed that the toxic impact of respired SWNTs may venture far beyond the lungs (Li et al. 2007b). Similarly, the acid-purified HiPco SWNTs administered by PA induces subacute increase of oxidative stress (Shvedova et al. 2005), as indicated by the activation of the oxidative stress marker heme oxygenase-1 (HO-1) 7 days after exposure in the aorta (fourfold), heart (3.5-fold) and lung (sixfold), accompanied with a significant decrease in the glutathione/oxidized glutathione (GSH/GSSG) ratio and a dramatic increase in the oxidatively modified protein content (protein carbonyls) of the aortic mitochondria (Li et al. 2007b). Consistently, significant mitochondrial DNA damage was also observed in aortic tissues of mice exposed to 10 and 40 μg of HiPco SWNTs 7, 28, and 60 days after exposure (Li et al. 2007b).
The same group also evaluated the impact of SWNTs (20 μg) against atherosclerosis development in ApoE−/− mice, a hyperlipidemic model that displayed accelerated manifestations of atherosclerosis because it lacked the apolipoprotein E gene (Li et al. 2007b). After exposure to 20 μg of SWNTs for 8 consecutive weeks, there was a significant enlargement of the atheroma lesion in aorta and brachiocephalic artery, an increase in the marker of monocytes/macrophages (Mac-3), and increased vascular cell adhesion molecule 1 (Vcam1) immunostained in atheroma plaques within the brachiocephalic artery of SWNT-exposed mice, relative to the control mice (Li et al. 2007b). Although the SWNT-exposed mice fed with combined diet did not show significant changes in the interleukin-6 (IL-6) levels, monocyte chemoattractant protein-1 (MCP1), interferon-γ (IFN-γ), tumor necrosis factor-α (TNF-α), and IL-12, relative to the vehicle control, the mitochondrial DNA expression was decreased, which corresponds to significant mitochondrial DNA damages associated with SWNT treatment (Li et al. 2007b). Although it remains unclear how the aspirated SWNTs contributed to the cardiovascular effects, the findings highlighted the potential of SWNTs to cause systemic toxicity in vulnerable subjects.
In a subsequent cardiovascular study, Legramante et al. (2009) demonstrated that respiratory exposure to SWNTs can also lead to altered cardiac autonomic regulation (Fig. 1) (Legramante et al. 2009). Following instillation of a phosphate buffer saline (PBS) vehicle or suspension of acid-purified SWNTs (ϕ: 1.2–1.6 nm, length: 2–5 nm) to rats at 2-week interval (≈350 μg per animal per session), the group observed a statistically significant reduction in the heart rates of SWNT-exposed rats, compared with the controls, 2 and 4 weeks after the first instillation. The SWNT-instilled rats also showed a gradual decreased number of baroreflex sequences compared with the controls at 0-, 1-, 2-, and 4-week time points, independent of the changes in heart rate measured at similar time points (Legramante et al. 2009). However, they did not observe any significant changes in the systolic or diastolic arterial pressures and baroreflex sensitivity for both treatment groups throughout the observation period (Legramante et al. 2009).
Both the study from Li et al. (2007b) and Legramante et al. (2009) indicated the possibility of direct or indirect involvement of SWNTs in promoting the pathologic development of cardiovascular systems (Legramante et al. 2009; Li et al. 2007b). The authors suggested that the aortic and carotid baroreceptor control might be desensitized because of cytokine-mediated downstream events or altered pulmonary mechanics from the primary impact of SWNTs against the lungs, or deposition of translocated SWNTs in cardiac tissues (Legramante et al. 2009; Li et al. 2007b). Validation is therefore needed to confirm the findings and to unveil the mechanism of SWNT-induced cardiac regulation changes in detail.
Dermal toxicity
Compared with the amount of data available on the respiratory toxicities, only a few studies have been dedicated to skin exposure to SWNTs. The earliest of such investigation was carried out by Huczko and Lange (2001), in which they administered filter paper patches that contained aqueous suspensions of soot with SWNTs to four human subjects with allergic conditions, as well as ocular instillations of similar soot mixtures to rabbits (Huczko and Lange 2001). They did not observe any abnormalities from either the treatment groups or the controls throughout the experimental period (Huczko and Lange 2001). However, the SWNTs used in their study were not characterized in terms of dimensions, impurity content, or mass.
With adequate characterization, Murray et al. (2009) studied the effects of HiPco SWNTs (purified: 0.23 wt% Fe and non-purified: 30 wt% Fe, 80 % dispersed) in animal and cellular skin models; they found that dermal exposure of SWNTs can lead to sequential oxidative stress events and inflammation, similar to that of respiratory exposure, and causes structural changes of mammalian skin (Murray et al. 2009). A dose-dependent increase in skin thickness and epidermal cell count was also observed by the group in hairless SKH-1 mice that had been subjected to topical exposure of 40, 80, and 160 µg of unpurified SWNTs per day for 5 days. At the highest dose of SWNTs, in addition to increased skin thickness and epidermal cell count, significant collagen accumulation and inflammatory reactions (as indicated by elevated mast cell numbers and activities, myeloperoxidase activity, inflammation of hair follicles, adipose tissue, and sebaceous gland) were observed (Fig. 1) (Murray et al. 2009). Remarkably, the skin flaps of the SWNT-exposed mice showed a significant dose-dependent increase of protein carbonyl content, suggesting that oxidative stress might be the major event that fuels skin inflammation and pathological changes (Murray et al. 2009). Therefore, SWNTs are likely to induce oxidative damage through dermal contact of the nanotubes and not only when taken up by mammals through inhalation, both of which can result in oxidative-driven consequences.
Gastrointestinal toxicity
Limited toxicity investigations have been performed on SWNTs following GI exposure. Folkmann et al. (2009) found that both SWNTs and C60 induced genotoxicity in secondary organs following GI exposure (Folkmann et al. 2009). Rats with single intragastric administration of C60 fullerenes (ϕ: 0.7 nm, purity: 99.9 %, agglomerated) and SWNTs (ϕ: 0.9–1.7 nm, length: <1 μm, agglomerated, with 2 wt% Fe, traces of Co, Ni, and Mn) dispersed in either saline solution or corn oil (0.064 or 0.64 mg per kg body weight) exhibited a significant increase in 8-oxo-7,8-dihydro-2′-deoxyguanosine (8-oxodG) in the liver and lungs of the animals 24 h after exposure (Folkmann et al. 2009). Notably, both the corn oil and saline nanomaterial preparations produced the same degree of 8-oxodG, suggesting that the absorption of SWNTs and C60 through the intestine are not influenced by the agglomeration of the particles. The 8-oxodG levels reached their highest in the liver, followed by the lung, for both types of particle, whereas there were no significant changes in 8-oxodG concentration in the colon of the treated animals (Folkmann et al. 2009). The expression of proteins associated with the 8-oxodG-removal function, 8-oxoguanine DNA glycosylase (OGG1), was found to be significantly elevated in the liver of rats treated with C60 in saline and oil preparations, whereas no significant changes were observed for SWNTs. There were also no significant changes in the expression of other oxidative stress markers such as heme oxygenase 1 (HO1), mutY homolog (E. coli) (MUTYH), endonuclease VIII-like 1 (E. coli) (NEIL1), and nudix (nucleoside diphosphate linked moiety X)-type motif 1 (NUDT1) in all of the tested animals. The genotoxicity associated with SWNTs and C60 was absent in the colon, which was attributed to the agglomeration of the particles and the high proliferation rate of colonic cells compared with liver and lungs cells (Folkmann et al. 2009).
In a separate study, SWNTs were found to be present in transport vesicles of intestinal columnar epithelial cells and macrophages in submucous epithelium, confirming intestinal absorption of the particles following gastrogavage administration of SWNTs (ϕ: 0.8–1.2 nm, length: 50–300 nm, with 0.1 wt% Si) dispersed in normal saline at doses of 5, 50, 100, 300, 400, and 500 mg/kg for 10 days (Yang et al. 2010). The SWNTs were localized mainly in the ileum and, to a lesser extent, in the jejunum where the abundance of SWNTs demonstrated dose- and time-dependent manners (Yang et al. 2010). Remarkably, the SWNTs were also discovered in secondary organs including neurons and neurites in the brain, heart, and liver. The majority of SWNTs at lower concentrations (5, 50, 100, 300 mg/kg) were found to reside in lysosomes, but higher doses of SWNTs (400 and 500 mg/kg) resulted in the accumulation of SWNTs within mitochondria in addition to the lysosomes, with only negligible amounts of SWNTs seen in the nucleus and cytoplasm. Importantly, the mitochondrial and lysosomal SWNT load appeared to be well regulated with particular dynamics. Specifically, at a SWNT concentration of 500 mg/kg, autophagy blockage by 3-methyladenine or anti-chaperone-mediated autophagy (CMA) siRNA increased the mitochondrial SWNT content and decreased the lysosomal fraction of SWNTs. Interestingly, this trend was reversed in response to energy deprivation (Yang et al. 2010). This toxic effect appeared to be related to the organelle damages caused by SWNTs and was only detected in mice administered with high doses of the SWNTs (400 and 500 mg/kg). The reactive oxygen species (ROS) production triggered by SWNTs was found to be confined within the mitochondria and led to the dose-dependent release of β-galactosidase from lysosomes (Fig. 1). The mitochondrial membrane potential (MMP) was decreased with time, as ROS production increased within 35 min of co-incubation of the mitochondria homogenates with SWNTs, confirming the role of the mitochondria as the primary target organelle of SWNT-induced intracellular damages (Yang et al. 2010).
In short, these studies demonstrated that SWNTs can be readily absorbed through digestive entry, distributed to other organs, and can exert damaging effect toward mitochondria (Folkmann et al. 2009; Yang et al. 2010). These findings, together with several other studies being discussed in this review, imply that the redox activities of SWNTs may not be entirely due to the presence of metal catalysts, but also to the π electron-rich SWNTs, which may be instrumental in ROS generation within biological environment.
Molecular mechanisms of SWNTs nanotoxicity
Cellular uptake, intracellular trafficking, and exocytosis of SWNTs
Cellular transport mechanisms such as endocytosis, phagocytosis, pinocytosis and passive diffusion serve vital regulatory role of nutrient, proteins and fluid acquisition, elimination of infectious agents and toxic waste from the living cells. However, the same mechanism also permits the internalization of the nanomaterials and its aggregates which span nano- to micrometers in dimensions after it enters into the body. Endocytosis comprises of several energy-dependent uptake mechanisms which may occur in the presence or absence of clathrin involvement (Doherty and McMahon 2009). In clathrin-independent endocytosis (CME) or synonymously, receptor-mediated endocytosis (RME), the cargoes are wrapped up into the clathrin-coated pits by curvature of plasma membrane, the structure fuses into clathrin-coated vesicles which subsequently detached from the plasma membrane, the contents are thus being delivered into the cells. Classification of cellular uptake mechanisms seems to be varied according to different views (Doherty and McMahon 2009; Iversen et al. 2011; Oh and Park 2014). According to Doherty and McMahon (2009), phagocytosis which occurs specifically in monocytes, neutrophils, dendritic cells and macrophages is classified as CIE, along with the clathrin-independent carriers/GPI-AP enriched early endosomal compartment (CLIC/GEEC) pathway, macropinocytosis, and other pathways which have been characterized in the very recent decades (Doherty and McMahon 2009). In CIE, the cargoes are transferred into the cells through pathway-specific plasma membrane invaginations, for example: caveolae for CLIC/GEEC pathway, cargo shape-dependent invaginations for phagocytosis and cell surface protrusions for macropinocytosis. Pinocytosis, another endocytotic pathway for fluid incorporation of the cells from the extracellular environment, can be differentiated from macropinocytosis by the smaller size of vesicles formed (i.e., ≈100 nm) than the later (0.2–5 μm), and the type of cargo being internalized (i.e., fluid for pinocytosis, fluid and particles for macropinocytosis) (Oh and Park 2014). Endocytosis can accommodate the internalization of nanomaterials of micrometers in diameter when interface at low density with the cell membrane (Zhang et al. 2009).
Particles can also gain entry into the cells without energy dependency through passive diffusion across the lipid bilayer of plasma membrane. This method, however, appeared to be relatively inefficient for nanomaterial uptake, where there is not only a tendency for the smaller nanomaterials to be taken up by the cells through this pathway, only few particles managed to cross the barrier, and some of them have induced damage to the erythrocyte membrane being studied (Shang et al. 2014).
Several of the current findings supported endocytosis as the major uptake pathway of SWNTs in mammalian cells (Fig. 2). As described by Kam et al. (2006), high fluorescence levels could be detected in HeLa cervical cancer cells and HL60 human promyelocytic leukemia cells after incubation for 1–3 h (≈200 nm in length) of the SWNTs that were conjugated with alexa fluor 488-labeled bovine serum albumin (BSA) and streptavidin (SA), or Cy3- and FITC-labeled DNA at 37 °C (Kam et al. 2006). Importantly, a decreased fluorescence intensity was observed in cells that had been pretreated with the endocytosis inhibitor (NaN3) or incubated at 4 °C following exposure to the conjugated SWNTs, suggesting that endocytosis is the uptake mechanism of protein- and DNA-conjugated SWNTs (Fig. 2). Reduced fluorescence intensities were also observed in cells incubated with SWNT–BSA conjugates with prior hypertonic treatment using a sucrose or K+-depleted medium. As hypertonic treatment or K+-depletion hinders the formation of clathrin-coated vesicles, this result confirmed that SWNTs might enter into the cells through a clathrin-dependent endocytotic pathway (Fig. 2) (Kam et al. 2006). In contrast, the uptake of SWNT–BSA was unchanged in cells that were pretreated with the cholesterol sequesters, filipin and nystatin, which disrupts caveolae and lipid-raft pathways, suggesting little or no involvement of caveolae-dependent endocytosis in the cellular entry of SWNT conjugates (Kam et al. 2006).
Cellular uptake of SWNTs in mammalian cells. SWNTs are taken up by energy-dependent mechanisms including RME, pinocytosis, and phagocytosis. Following uptake, SWNTs localize to the lysosomes, endosome-like vesicles, the cell membrane and cell nucleus. While some SWNTs form aggregates within cells, a fraction of SWNTs is expelled by exocytosis
In a separate study, Cherukuri et al. (2004) observed a linear increase in SWNT uptake per cell during 24 h incubation of mouse peritoneal macrophage-like cells with Pluronic F108-dispersed SWNTs, and reduction of SWNT uptake by 60 % when similarly treated cells were incubated at 27 °C, as compared to 37 °C, which is consistent with the temperature-dependent nature of macrophage phagocytotic activity (Fig. 2) (Cherukuri et al. 2004). The findings imply that the uptake of Pluronic-dispersed SWNTs by macrophages is likely to occur though phagocytosis.
Indeed, the direct observation of the cellular uptake of SWNTs using transmission electron microscopy (TEM) and confocal microscopy to image the translocation of SWNTs into human monocyte-derived macrophages (HMMs), reveals the intracellular distribution of SWNTs in lysosomes following 2 days incubation of 5 mg/mL SWNT (Porter et al. 2007). After 4 days of incubation, the majority of the SWNT bundles were seen in endosome-like vesicles. Fusion and parallel alignment of the long axes of SWNTs with the cell membrane were also observed, in which some of these bundles merged with or passed through lysosomal membranes and localized within the cell nucleus, causing cell mortality in a dose-dependent manner (Porter et al. 2007). These results suggested that the uptake of SWNTs could be mediated through clathrin-dependent endocytosis and phagocytosis, but not through caveolae-dependent endocytosis.
To investigate whether exocytosis occurs for the internalized SWNTs conjugates in a biological environment, Jin et al. (2008) traced the movement of SWNT–DNA conjugates in and out of the 3T3 mouse fibroblast cells in real time using the single-particle tracking (SPT) method (Fig. 2) (Jin et al. 2008). The results indicated that 50.8 % of SWNT–DNA conjugates interact with the cells, including the adsorption (6.2 %) or confined diffusion (12.7 %) of SWNT–DNA onto the plasma membrane as well as slow uptake by the cells through endocytosis and confined diffusion of SWNTs in endosomes, which were followed by the formation of aggregates within cells or exocytosis of particles by the cells (5.9 %). In addition, desorption from the cells occurred for some of the SWNTs prior to internalization (7.4 %). The SWNTs had undergone exocytosis at a rate almost similar to that of endocytosis, leaving a small amount of the SWNTs that remained intracellular. The results demonstrated that the uptake and excretion of SWNT–DNA was actively controlled by the cells, suggesting that the SWNTs could be internalized through endocytosis, preserved within the cells, or recycled to the plasma membrane for excretion (Jin et al. 2008). Similarly, exocytosis of SWNTs was also observed by Cheng et al. (2008), during which the SWNT–PEG–FITC conjugates were seen to be initially internalized through active transportation in HeLa cells, to reside in cytoplasm of the cells, and were then released from the cells after the particles were removed from the medium (Cheng et al. 2008).
Despite the current imaging and spectroscopy information unequivocally support the fact that SWNTs can be taken up, retained, or excreted within nucleated cells (Porter et al. 2007; Tong et al. 2012), the ability of SWNTs to gain entry into anucleated cells, such as erythrocytes, is debatable. Using confocal microscopy, Sachar and Saxena (2011) showed that the fluorescent-tagged SWNTs may enter into the erythrocytes through a passive mechanism after 1 h exposure (Sachar and Saxena 2011), whereas Raman spectroscopic data from Donkor et al. (2009) suggests that there was no evidence of uptake by erythrocytes after 2 h incubation with SWNTs (Donkor et al. 2009). Given the absence of endocytic receptors on normal mature erythrocytes, it is plausible that the uptake of SWNTs by erythrocytes, as reported by Sachar and Saxena (2011) may have been occurred through other mechanism(s), such as passive uptake, which has been shown with titanium dioxide, polystyrene, and gold nanoparticles (Geiser et al. 2005; Rothen-Rutishauser et al. 2006); the SWNTs might also have been associated with the erythrocyte membrane instead of entering the cells.
Although most findings have indicated that the SWNTs gain entry into the cells through energy-dependent uptake mechanisms, it is important to note that the toxicity of nanoparticles may not always be associated with cellular uptake. Bhabra et al. (2009) demonstrated that the cobalt–chromium nanoparticles cause a similar extent of apoptosis and DNA damage in fibroblast cells by ATP and intercellular signaling pathways, regardless of the presence of protective placental cellular barrier cultured in between the SWNTs and fibroblast layer (Bhabra et al. 2009). The presence of this indirect mechanism suggests the possibility that SWNTs being deposited in particular organ (such as the lung following inhalation of the material) may exert systemic effects. It is therefore crucial for future studies to provide valid data with regard to the link between cellular uptake and toxicity of SWNTs.
Cellular toxicity of SWNTs
Confounding factors in the cytotoxicity testing protocol
A large number of studies reporting the cytotoxicity of SWNTs for in vitro mammalian cell models involved utilization of cell proliferation assay(s), such as the MTT and alamar blue assays. Although these assays have been commonly used in many pharmacological studies, Worle-Knirsch et al. (2006) have reported a great disparity between the viability values measured using MTT, WST-1, and LDH leakage assays in A549 human alveolar carcinoma epithelial cells treated with SWNTs (50 μg/mL, 24–98 h) (Worle-Knirsch et al. 2006). In particular, a significant reduction in the viability was only evident in MTT assays throughout the experiments (Worle-Knirsch et al. 2006). The contradictory nature of the MTT assay compared with the others was affirmed with the absence of changes to the MMP and cell death of the A549 cells receiving similar treatments. Finally, TEM imaging showed the association of MTT-formazan crystals with SWNTs, which were inseparable by chemical or heat treatment (Worle-Knirsch et al. 2006). Later, a cytotoxicity assessment using alamar blue, neutral red, and coomassie brilliant blue were confirmed to be disrupted by the presence of SWNTs through the adsorption of the dye compounds onto the nanotube surfaces (Casey et al. 2007; Davoren et al. 2007; Monteiro-Riviere and Inman 2006; Monteiro-Riviere et al. 2009; Pacurari et al. 2008; Worle-Knirsch et al. 2006). Therefore, the data generated using these assays need to be interpreted with cautions.
Effects of dispersants on the SWNT-induced cytotoxicity
SWNTs are known to bundle into tight aggregates of different sizes during synthesis due to van der Waals attraction forces (Coleman et al. 2004; Girifalco et al. 2000). It is a common practice for the powder-form nanomaterial to be uniform in size and transformed into stable homogeneous suspensions prior to administration into the cells through in vitro toxicity assays; these requirements have been accomplished conventionally by sonication of the SWNTs in various dispersants.
However, previous studies have suggested that the morphological and surface characteristics of SWNTs, and their availability to the cells, may be altered due to the dispersant used, thus affecting the cytotoxic outcome (Jia et al. 2005; Sun and Zhang 2008). In addition, the dispersant might possess non-specific toxicity toward certain cell types and cause false-positive results in the evaluation of the cytotoxicity of SWNTs (Dong et al. 2008, 2009). Indeed, surfactants such as 1 wt% sodium dodecyl sulfate (SDS) and 1 wt% sodium dodecylbenzene sulfonate (SDBS), a commonly used dispersant for SWNTs, have been demonstrated to induce apoptotic morphological changes in 1321N1 human astrocytoma cells, regardless of the presence of SWNTs after a brief exposure (≤1 h) (Dong et al. 2009). Even surfactants that are known to be biocompatible, such as 1 % pluronic F108, have been found to induce a slight reduction in viability when introduced to human dermal fibroblasts as a vehicle control after 48 h incubation (Sayes et al. 2006).
In addition, dispersants could also influence the physicochemical properties of the SWNTs and possess a surface modification effect. Using Western blot and tandem mass spectrometry, Dutta et al. (2007) demonstrated that the proteins in fetal bovine serum (including caseins, glycoproteins, lipoproteins, and globulins), human serum, and plasma (particularly albumin) were effectively adsorbed onto the surface of SWNTs when included as an additive of the dispersants (Dutta et al. 2007). A subsequent study by Ge et al. (2011), using atomic force microscopy analysis also showed that bovine fibrinogen (BFG), gamma globulin (γIg), transferrin (Tf), and BSA binds to the surface of SWNTs through the hydrophobic amino acid residues phenylalanine, tryptophan, and tyrosine, which arrange into aggregates or become layered on top of the molecules until a thermodynamically stable state is achieved. The number of protein molecules stacked upon each other on the SWNT surface was ranked according to the order BFG > γIg > Tf > BSA, which is proportional to the abundance of the hydrophobic residues and the size of the protein (Ge et al. 2011). Importantly, the cytotoxicity of the materials (30 μg/mL; 6 and 12 h exposure) followed a time- and dose-dependent relationship in THP-1 human acute monocytic leukemia cells and human umbilical vein endothelial cells (HUVEC). At 12-h post-exposure, the viability of the THP-1 cells was decreased in the following order: pristine SWNTs > SWNT–BSA > SWNT–Tf > SWNT–γIg > SWNT–BFG, whereas the loss of viability for HUVEC was demonstrated in the sequence: pristine SWNT > SWNT–γIg > SWNT–Tf > SWNT–BSA > SWNT–BFG (Ge et al. 2011). The same trend was displayed when using LIVE/DEAD fluorescence staining in THP-1 cells after 12 h exposure to the materials. Hence, not only did the protein–SWNT interaction affect the in vitro toxicity profile, this relationship could also exist and exert physiological effects in vivo.
Effects of surface modifications on SWNT-induced cytotoxicity
Study of carboxyl-functionalized SWNTs has shed some light on the influence of surface modification toward the toxicity profile of SWNTs. Several studies have revealed that SWNT–COOH drastically reduced the viability of HUVEC cells (Gutierrez-Praena et al. 2011), Caco-2 colon adenocarcinoma cells (Tang et al. 2005), and human gingival fibroblasts (HGF) (Cicchetti et al. 2011), as compared to pristine SWNTs. For example, SWNT–COOH has shown to induce a significant dose-dependent reduction of cell proliferation, which is accompanied by increased ROS as well as the emergence of apoptotic nuclei, micronuclei (MN), and DNA damage in human gingival fibroblasts (HGF) (Cicchetti et al. 2011). However, such cytotoxic effects were absent in cells treated with pristine SWNTs. Similarly, the extent of SWNT–COOH-induced ROS, oxidative damage, and lipid peroxidation could be illustrated in Caco-2 cells, which was accompanied by a significant increase in catalase (CAT), superoxide dismutase (SOD), and glutathione peroxidase (GSH-Px) levels as the glutathione reductase (GR) and GSH levels were significantly reduced (Pichardo et al. 2012).
Furthermore, Sachar and Saxena (2011) showed that the undesirable ramifications of SWNT–COOH were not limited to the exposed nucleated cells (Sachar and Saxena 2011). It was found that SWNT–COOH induces a dose-dependent reduction for the recovery of cultured erythrocytes, which was more severe for SWNT–COOH compared with pristine SWNTs at an equivalent dose (50 μg/mL). They also found that brief exposure to SWNT–COOH (≤25 μg/mL, ≤2 h) was sufficient to cause severe membrane damage and a time-dependent increase in cell death for the erythrocytes, which is a feature that did not occur with pristine SWNTs under similar experimental conditions (Sachar and Saxena 2011). Although certain functionalizations have been shown to decrease the detrimental effects of SWNTs (Dumortier et al. 2006; Klumpp et al. 2006; Krajcik et al. 2008; Liu et al. 2009; Sayes et al. 2006), carboxylation of SWNTs offers no protection, instead it aggravates the intrinsic toxicity of SWNTs. Thus, specific testing is often required in order to unfold the efficiency of each surface modification strategy.
Effects of metal catalyst contaminants on SWNT-induced cytotoxicity
Depending on the synthesis method, SWNTs may contain a number of toxic metals as contaminants. These metals include Co, Fe, Ni, and Mo, all of which have documented toxic effects. The content of these contaminants in the SWNT samples has been reported to be an important determinant of toxicity. Following the detection of hydroxyl radicals (·OH), which only present in the suspensions of non-purified SWNTs (26 wt% Fe) and not in purified SWNTs (0.23 wt% Fe), Kagan et al. (2006) found that treatment of zymosan-stimulated or phorbol myristate acetate (PMA)-stimulated murine macrophages (RAW 264.7) with 120 μg/mL non-purified SWNTs for ≤2 h, led to the depletion of the antioxidant GSH by ≈50 % and the increase of accumulated lipid hydroperoxides by ≈3–4 time. However, exposure of the cells with a similar concentration of purified SWNTs only resulted in around twofold induction of lipid hydroperoxides (Kagan et al. 2006). These effects were partially remedied by addition of extracellular catalase to scavenge the hydroxyl radicals. Indeed, GSH depletion appeared to be caused by the iron-induced formation of ·OH radicals, owing to the intracellular production of superoxide radicals (O2 −), whereas nitric oxide (NO) production remained unchanged in the macrophage exposed to both purified and non-purified SWNTs (Kagan et al. 2006).
In agreement with these findings, ·OH radicals were observed in JB6P+ murine epidermal cells after 5 min incubation with non-purified SWNTs (30 wt% Fe, 0.12 mg/mL), which was attenuated by catalase (H2O2 scavenger) and deferoxamine (metal chelator) (Murray et al. 2009). Dose-dependent reduction of GSH was also evident in JB6P+ cells exposed to non-purified and purified SWNT, but non-purified SWNTs resulted in more prominent GSH depletion than purified SWNTs (Murray et al. 2009). In addition, specific dose-dependent induction of AP-1 transcription activator was also observed in JB6P+ exposed to non-purified SWNTs, whereas no such induction was observed with purified SWNTs.
Pathways associated with SWNT-induced toxicity
Despite overwhelming reports on the toxicity of SWNTs for in vivo studies, many questions regarding to their toxicity mechanism remain unanswered. Most studies, to date, implicate that SWNTs induce dose- and time-dependent cell death in different cell types by activating many pathways at once, mostly involving generation of ROS and DNA damage (Pacurari et al. 2008). Indeed, MN formation and the increase in gamma H2AX foci indicative of double-strand breaks (DSBs) were observed in human lymphocytes and human fibroblasts following the treatment of SWNTs (Cveticanin et al. 2009).
Exposure to SWNTs has been shown to activate PARP1, AP-1, NFκB, p38, and AKT in a dose-dependent manner in normal mesothelial cells (Pacurari et al. 2008). Cell-cycle-associated genes such as p16, BAX, p57, HRK, CDC, and CDC37 were also up-regulated in HEK293 cells following exposure to SWNTs, whereas CDK2, CDK4, CDK6, and cyclin D3 were down-regulated (Cui et al. 2005). Similarly, down-regulation of signal transduction-associated genes, such as MAD2, JAK1, TTK, PCDHA9, and ERK were evident. Further immunoblot analysis showed that SWNTs can inhibit the protein expression of adhesion-associated proteins such as laminin, fibronectin, cadherin, FAK, and collagen IV.
Interestingly, changes in the expression of drug-metabolizing enzymes, such as CYP1A1, CYP1B1, CYP2S1, and CYP19A1, were observed in human respiratory tract cells (NHBE and A549) after the treatment of SWNTs (100 μg/mL, 24 h exposure) (Hitoshi et al. 2012). Down-regulation of CYP1A1 and CYP1B1 may be, in part, due to the reduced binding of the aryl hydrocarbon receptor (AhR) to the enhancer region of CYP1A1 and CYP1B1 (Hitoshi et al. 2012). The exact mechanism by which SWNTs affect the AhR-CYP axis remains to be further elucidated. Together, these results suggest that SWNTs can regulate multiple pathways simultaneously to manifest their cytotoxic effects in a cell-type-dependent manner.
Conclusions
CNTs, particularly SWNTs, are an important class of new materials that have numerous properties, making them useful in technology and industry. The predicted increase in manufacture and industrial use of SWNTs imply that the risk of human exposure to the nanomaterial might increase dramatically in the near future. As such, a comprehensive understanding of the toxicological profile of various SWNTs is crucial in order to assess the hazards they present. Although early studies have shown that SWNTs could have features of both nanoparticles and conventional fibers, such as asbestos, recent reports suggest that SWNTs may have toxic effects beyond those anticipated for their mass exposure. For instance, more toxic effects have been observed in SWNTs for numerous cell types, compared with the same nanoparticulate mass for carbon and quartz, which are commonly used yardsticks for harmful particles.
However, it should be noted that there is, as yet, no definitive in vivo or human exposure study available that can address the true hazard of SWNTs. Most in vivo studies to date possess potential artifactual effects, which can be attributed to large mats and aggregates forming during the exposure procedures. SWNTs may have local effects through the induction of oxidative stress and inflammation, and an unexpected ability for granuloma formation and fibrogenesis; they might also possess the potential to translocate from their portal of entry to other tissues and cause secondary damage. This should remain an important question to be answered in CNT research.
Evidently, more research is needed to gain an insight into the mechanism of the adverse effects induced by SWNTs to identify the best ways to measure the associated SWNT toxicity in biological systems in order to protect those that are exposed to these new materials. A number of issues pertaining to SWNT nanotoxicity must be addressed.
Firstly, a set of standard reference SWNTs is needed so that the potential risk of any functionalized SWNT may be compared with known materials, with regard to specific parameters such as length, surface modification, charges, and so on. Secondly, standard experimental protocols, such as animal models, cell assays, quantification, and characterization methodologies, should be established in order for a toxicological profile to be established from studies across various laboratories, which can be compared effectively. Thirdly, the careful design of long-term studies into the absorption, deposition, metabolism, and excretion of pristine and functionalized SWNTs in animal models are urgently needed. Fourthly, probing of the pathways that contribute to the cytotoxicity of SWNTs is required to understand the intrinsic cellular sensitivity and tolerance to toxicity of particular cell types, which can pave the way for future applications in vivo. Finally, the use of traditional toxicology assays for the evaluation of SWNTs nanotoxicity should be treated with caution in light of the peculiar properties of SWNTs and the uncertainty of their nature, mechanism, and exposure response. Until better information becomes available, handling of SWNTs should be considered in the same way as other hazardous nanomaterials in workplace risk assessments, implying similar control and assessment approaches.
References
Aggarwal P, Hall JB, McLeland CB, Dobrovolskaia MA, McNeil SE (2009) Nanoparticle interaction with plasma proteins as it relates to particle biodistribution, biocompatibility and therapeutic efficacy. Adv Drug Deliv Rev 61(6):428–437. doi:10.1016/j.addr.2009.03.009
Avouris P, Chen Z, Perebeinos V (2007) Carbon-based electronics. Nat Nanotechnol 2(10):605–615. doi:10.1038/nnano.2007.300
Azeredo H (2009) Nanocomposites for food packaging applications. Food Res Int 42(9):1240–1253
Bang JJ, Guerrero PA, Lopez DA, Murr LE, Esquivel EV (2004) Carbon nanotubes and other fullerene nanocrystals in domestic propane and natural gas combustion streams. J Nanosci Nanotechnol 4(7):716–718
Bhabra G, Sood A, Fisher B et al (2009) Nanoparticles can cause DNA damage across a cellular barrier. Nat Nanotechnol 4(12):876–883. doi:10.1038/nnano.2009.313
Casals E, Vázquez-Campos S, Bastús NG, Puntes V (2008) Distribution and potential toxicity of engineered inorganic nanoparticles and carbon nanostructures in biological systems. Trends Anal Chem 27(8):672–683
Casey A, Herzog E, Davoren M, Lyng F, Byrne H, Chambers G (2007) Spectroscopic analysis confirms the interactions between single walled carbon nanotubes and various dyes commonly used to assess cytotoxicity. Carbon 45(7):1425–1432
Cheng J, Fernando KA, Veca LM et al (2008) Reversible accumulation of PEGylated single-walled carbon nanotubes in the mammalian nucleus. ACS Nano 2(10):2085–2094. doi:10.1021/nn800461u
Cherukuri P, Bachilo SM, Litovsky SH, Weisman RB (2004) Near-infrared fluorescence microscopy of single-walled carbon nanotubes in phagocytic cells. J Am Chem Soc 126(48):15638–15639. doi:10.1021/ja0466311
Cherukuri P, Gannon CJ, Leeuw TK et al (2006) Mammalian pharmacokinetics of carbon nanotubes using intrinsic near-infrared fluorescence. Proc Natl Acad Sci USA 103(50):18882–18886. doi:10.1073/pnas.0609265103
Cicchetti R, Divizia M, Valentini F, Argentin G (2011) Effects of single-wall carbon nanotubes in human cells of the oral cavity: geno-cytotoxic risk. Toxicol In Vitro 25(8):1811–1819. doi:10.1016/j.tiv.2011.09.017
Coleman JN, Fleming A, Maier S et al (2004) Binding kinetics and SWNT bundle dissociation in low concentration polymer-nanotube dispersions. J Phys Chem B 108(11):3446–3450
Cui D, Tian F, Ozkan CS, Wang M, Gao H (2005) Effect of single wall carbon nanotubes on human HEK293 cells. Toxicol Lett 155(1):73–85. doi:10.1016/j.toxlet.2004.08.015
Cveticanin J, Joksic G, Leskovac A, Petrovic S, Sobot AV, Neskovic O (2009) Using carbon nanotubes to induce micronuclei and double strand breaks of the DNA in human cells. Nanotechnology 21(1):015102. doi:10.1088/0957-4484/21/1/015102
Davoren M, Herzog E, Casey A et al (2007) In vitro toxicity evaluation of single walled carbon nanotubes on human A549 lung cells. Toxicol In Vitro 21(3):438–448. doi:10.1016/j.tiv.2006.10.007
De Jong WH, Borm PJ (2008) Drug delivery and nanoparticles: applications and hazards. Int J Nanomed 3(2):133–149
Deng X, Jiab G, Wang H et al (2007) Translocation and fate of multi-walled carbon nanotubes in vivo. Carbon 45(7):1419–1424
Doherty GJ, McMahon HT (2009) Mechanisms of endocytosis. Annu Rev Biochem 78:857–902. doi:10.1146/annurev.biochem.78.081307.110540
Dong L, Joseph KL, Witkowski CM, Craig MM (2008) Cytotoxicity of single-walled carbon nanotubes suspended in various surfactants. Nanotechnology 19(25):255702. doi:10.1088/0957-4484/19/25/255702
Dong L, Witkowski CM, Craig MM, Greenwade MM, Joseph KL (2009) Cytotoxicity effects of different surfactant molecules conjugated to carbon nanotubes on human astrocytoma cells. Nanoscale Res Lett 4(12):1517–1523. doi:10.1007/s11671-009-9429-0
Donkor A, Su Z, Mandal H, Jin X, Tang X (2009) Carbon nanotubes inhibit the hemolytic activity of the pore-forming toxin pyolysin. Nano Res 2(7):517–525. doi:10.1007/s12274-009-9049-0
Dumortier H, Lacotte S, Pastorin G et al (2006) Functionalized carbon nanotubes are non-cytotoxic and preserve the functionality of primary immune cells. Nano Lett 6(7):1522–1528. doi:10.1021/nl061160x
Dutta D, Sundaram SK, Teeguarden JG et al (2007) Adsorbed proteins influence the biological activity and molecular targeting of nanomaterials. Toxicol Sci 100(1):303–315. doi:10.1093/toxsci/kfm217
El-Ansary A, Al-Daihan S (2009) On the toxicity of therapeutically used nanoparticles: an overview. J Toxicol 2009:754810. doi:10.1155/2009/754810
Folkmann JK, Risom L, Jacobsen NR, Wallin H, Loft S, Moller P (2009) Oxidatively damaged DNA in rats exposed by oral gavage to C60 fullerenes and single-walled carbon nanotubes. Environ Health Perspect 117(5):703–708. doi:10.1289/ehp.11922
Ge C, Du J, Zhao L et al (2011) Binding of blood proteins to carbon nanotubes reduces cytotoxicity. Proc Natl Acad Sci USA 108(41):16968–16973. doi:10.1073/pnas.1105270108
Geiser M, Rothen-Rutishauser B, Kapp N et al (2005) Ultrafine particles cross cellular membranes by nonphagocytic mechanisms in lungs and in cultured cells. Environ Health Perspect 113(11):1555–1560
Girifalco L, Hodak M, Lee RS (2000) Carbon nanotubes, buckyballs, ropes, and a universal graphitic potential. Phys Rev B 62(19):13104
Gutierrez-Praena D, Pichardo S, Sanchez E, Grilo A, Camean AM, Jos A (2011) Influence of carboxylic acid functionalization on the cytotoxic effects induced by single wall carbon nanotubes on human endothelial cells (HUVEC). Toxicol In Vitro 25(8):1883–1888. doi:10.1016/j.tiv.2011.05.027
Hitoshi K, Katoh M, Suzuki T, Ando Y, Nadai M (2012) Changes in expression of drug-metabolizing enzymes by single-walled carbon nanotubes in human respiratory tract cells. Drug Metab Dispos 40(3):579–587. doi:10.1124/dmd.111.043455
Huczko A, Lange H (2001) Carbon nanotubes: experimental evidence for a null risk of skin irritation and allergy. Fuller Sci Technol 9(2):247–250
Huczko A, Lange H, Całko E, Grubek-Jaworska H, Droszcz P (2001) Physiological testing of carbon nanotubes: are they asbestos-like? Fuller Sci Technol 9(2):251–254
Iversen T-G, Skotland T, Sandvig K (2011) Endocytosis and intracellular transport of nanoparticles: present knowledge and need for future studies. Nano Today 6(2):176–185
Jia G, Wang H, Yan L et al (2005) Cytotoxicity of carbon nanomaterials: single-wall nanotube, multi-wall nanotube, and fullerene. Environ Sci Technol 39(5):1378–1383
Jin H, Heller DA, Strano MS (2008) Single-particle tracking of endocytosis and exocytosis of single-walled carbon nanotubes in NIH-3T3 cells. Nano Lett 8(6):1577–1585. doi:10.1021/nl072969s
Johnson DR, Methner MM, Kennedy AJ, Steevens JA (2010) Potential for occupational exposure to engineered carbon-based nanomaterials in environmental laboratory studies. Environ Health Perspect 118(1):49–54. doi:10.1289/ehp.0901076
Kagan VE, Tyurina YY, Tyurin VA et al (2006) Direct and indirect effects of single walled carbon nanotubes on RAW 264.7 macrophages: role of iron. Toxicol Lett 165(1):88–100. doi:10.1016/j.toxlet.2006.02.001
Kam NW, Liu Z, Dai H (2006) Carbon nanotubes as intracellular transporters for proteins and DNA: an investigation of the uptake mechanism and pathway. Angew Chem Int Ed Engl 45(4):577–581. doi:10.1002/anie.200503389
Klumpp C, Kostarelos K, Prato M, Bianco A (2006) Functionalized carbon nanotubes as emerging nanovectors for the delivery of therapeutics. Biochim Biophys Acta 1758(3):404–412. doi:10.1016/j.bbamem.2005.10.008
Krajcik R, Jung A, Hirsch A, Neuhuber W, Zolk O (2008) Functionalization of carbon nanotubes enables non-covalent binding and intracellular delivery of small interfering RNA for efficient knock-down of genes. Biochem Biophys Res Commun 369(2):595–602. doi:10.1016/j.bbrc.2008.02.072
Lam CW, James JT, McCluskey R, Hunter RL (2004) Pulmonary toxicity of single-wall carbon nanotubes in mice 7 and 90 days after intratracheal instillation. Toxicol Sci 77(1):126–134. doi:10.1093/toxsci/kfg243
Lam CW, James JT, McCluskey R, Arepalli S, Hunter RL (2006) A review of carbon nanotube toxicity and assessment of potential occupational and environmental health risks. Crit Rev Toxicol 36(3):189–217
Lee J, Mahendra S, Alvarez PJ (2010) Nanomaterials in the construction industry: a review of their applications and environmental health and safety considerations. ACS Nano 4(7):3580–3590. doi:10.1021/nn100866w
Legramante JM, Valentini F, Magrini A et al (2009) Cardiac autonomic regulation after lung exposure to carbon nanotubes. Hum Exp Toxicol 28(6–7):369–375. doi:10.1177/0960327109105150
Li JG, Li WX, Xu JY et al (2007a) Comparative study of pathological lesions induced by multiwalled carbon nanotubes in lungs of mice by intratracheal instillation and inhalation. Environ Toxicol 22(4):415–421. doi:10.1002/tox.20270
Li Z, Hulderman T, Salmen R et al (2007b) Cardiovascular effects of pulmonary exposure to single-wall carbon nanotubes. Environ Health Perspect 115(3):377–382. doi:10.1289/ehp.9688
Liu Z, Cai W, He L et al (2007) In vivo biodistribution and highly efficient tumour targeting of carbon nanotubes in mice. Nat Nanotechnol 2(1):47–52. doi:10.1038/nnano.2006.170
Liu Z, Tabakman SM, Chen Z, Dai H (2009) Preparation of carbon nanotube bioconjugates for biomedical applications. Nat Protoc 4(9):1372–1382. doi:10.1038/nprot.2009.146
Mahar B, Laslau C, Yip R, Sun Y (2007) Development of carbon nanotube-based sensors—a review. Sens J IEEE 7(2):266–284
Mangum JB, Turpin EA, Antao-Menezes A, Cesta MF, Bermudez E, Bonner JC (2006) Single-walled carbon nanotube (SWCNT)-induced interstitial fibrosis in the lungs of rats is associated with increased levels of PDGF mRNA and the formation of unique intercellular carbon structures that bridge alveolar macrophages in situ. Part Fibre Toxicol 3:15. doi:10.1186/1743-8977-3-15
Mauter MS, Elimelech M (2008) Environmental applications of carbon-based nanomaterials. Environ Sci Technol 42(16):5843–5859
Maynard A, Michelson E (2006) The nanotechnology consumer products inventory. Woodrow Wilson International Center for Scholars, Washington, DC, Accessed March 23
Maynard AD, Baron PA, Foley M, Shvedova AA, Kisin ER, Castranova V (2004) Exposure to carbon nanotube material: aerosol release during the handling of unrefined single-walled carbon nanotube material. J Toxicol Environ Health A 67(1):87–107. doi:10.1080/15287390490253688
McDevitt MR, Chattopadhyay D, Jaggi JS et al (2007a) PET imaging of soluble yttrium-86-labeled carbon nanotubes in mice. PLoS One 2(9):e907. doi:10.1371/journal.pone.0000907
McDevitt MR, Chattopadhyay D, Kappel BJ et al (2007b) Tumor targeting with antibody-functionalized, radiolabeled carbon nanotubes. J Nucl Med 48(7):1180–1189. doi:10.2967/jnumed.106.039131
Monteiro-Riviere NA, Inman AO (2006) Challenges for assessing carbon nanomaterial toxicity to the skin. Carbon 44(6):1070–1078
Monteiro-Riviere NA, Inman AO, Zhang LW (2009) Limitations and relative utility of screening assays to assess engineered nanoparticle toxicity in a human cell line. Toxicol Appl Pharmacol 234(2):222–235. doi:10.1016/j.taap.2008.09.030
Murr LE (2008) Microstructures and nanostructures for environmental carbon nanotubes and nanoparticulate soots. Int J Environ Res Public Health 5(5):321–336
Murr LE, Bang JJ, Esquivel EV, Guerrero PA, Lopez DA (2004) Carbon nanotubes and nanocrystal forms, and complex nanoparticle aggregates in common fuel-gas combustion sources and the ambient air. J Nanopart Res 6:241–251
Murr LE, Garza KM, Soto KF et al (2005) Cytotoxicity assessment of some carbon nanotubes and related carbon nanoparticle aggregates and the implications for anthropogenic carbon nanotube aggregates in the environment. Int J Environ Res Public Health 2(1):31–42
Murray AR, Kisin E, Leonard SS et al (2009) Oxidative stress and inflammatory response in dermal toxicity of single-walled carbon nanotubes. Toxicology 257(3):161–171. doi:10.1016/j.tox.2008.12.023
Oh N, Park JH (2014) Endocytosis and exocytosis of nanoparticles in mammalian cells. Int J Nanomed 9(Suppl 1):51–63. doi:10.2147/IJN.S26592
Pacurari M, Yin XJ, Zhao J et al (2008) Raw single-wall carbon nanotubes induce oxidative stress and activate MAPKs, AP-1, NF-kappaB, and Akt in normal and malignant human mesothelial cells. Environ Health Perspect 116(9):1211–1217. doi:10.1289/ehp.10924
Pantarotto D, Partidos CD, Hoebeke J et al (2003) Immunization with peptide-functionalized carbon nanotubes enhances virus-specific neutralizing antibody responses. Chem Biol 10(10):961–966
Park EJ, Roh J, Kim SN, et al (2011) A single intratracheal instillation of single-walled carbon nanotubes induced early lung fibrosis and subchronic tissue damage in mice. Arch Toxicol 85(9):1121–1131. doi:10.1007/s00204-011-0655-8
Pichardo S, Gutierrez-Praena D, Puerto M et al (2012) Oxidative stress responses to carboxylic acid functionalized single wall carbon nanotubes on the human intestinal cell line Caco-2. Toxicol In Vitro 26(5):672–677. doi:10.1016/j.tiv.2012.03.007
Poland CA, Duffin R, Kinloch I et al (2008) Carbon nanotubes introduced into the abdominal cavity of mice show asbestos-like pathogenicity in a pilot study. Nat Nanotechnol 3(7):423–428. doi:10.1038/nnano.2008.111
Porter AE, Gass M, Muller K, Skepper JN, Midgley PA, Welland M (2007) Direct imaging of single-walled carbon nanotubes in cells. Nat Nanotechnol 2(11):713–717. doi:10.1038/nnano.2007.347
Rothen-Rutishauser BM, Schurch S, Haenni B, Kapp N, Gehr P (2006) Interaction of fine particles and nanoparticles with red blood cells visualized with advanced microscopic techniques. Environ Sci Technol 40(14):4353–4359
Sachar S, Saxena RK (2011) Cytotoxic effect of poly-dispersed single walled carbon nanotubes on erythrocytes in vitro and in vivo. PLoS One 6(7):e22032. doi:10.1371/journal.pone.0022032
Sahaym U, Norton MG (2008) Advances in the application of nanotechnology in enabling a ‘hydrogen economy’. J Mater Sci 43(16):5395–5429
Sayes CM, Liang F, Hudson JL et al (2006) Functionalization density dependence of single-walled carbon nanotubes cytotoxicity in vitro. Toxicol Lett 161(2):135–142. doi:10.1016/j.toxlet.2005.08.011
Schipper ML, Nakayama-Ratchford N, Davis CR et al (2008) A pilot toxicology study of single-walled carbon nanotubes in a small sample of mice. Nat Nanotechnol 3(4):216–221. doi:10.1038/nnano.2008.68
Shang L, Nienhaus K, Nienhaus GU (2014) Engineered nanoparticles interacting with cells: size matters. J Nanobiotechnol 12:5. doi:10.1186/1477-3155-12-5
Shvedova AA, Kisin ER, Mercer R et al (2005) Unusual inflammatory and fibrogenic pulmonary responses to single-walled carbon nanotubes in mice. Am J Physiol Lung Cell Mol Physiol 289(5):L698–L708. doi:10.1152/ajplung.00084.2005
Shvedova AA, Kisin ER, Murray AR et al (2007) Vitamin E deficiency enhances pulmonary inflammatory response and oxidative stress induced by single-walled carbon nanotubes in C57BL/6 mice. Toxicol Appl Pharmacol 221(3):339–348. doi:10.1016/j.taap.2007.03.018
Shvedova AA, Kisin E, Murray AR et al (2008) Inhalation vs. aspiration of single-walled carbon nanotubes in C57BL/6 mice: inflammation, fibrosis, oxidative stress, and mutagenesis. Am J Physiol Lung Cell Mol Physiol 295(4):L552–L565. doi:10.1152/ajplung.90287.2008
Singh R, Pantarotto D, Lacerda L et al (2006) Tissue biodistribution and blood clearance rates of intravenously administered carbon nanotube radiotracers. Proc Natl Acad Sci USA 103(9):3357–3362. doi:10.1073/pnas.0509009103
Sun L, Zhang Y (2008) The biocompatibility of carbon nanotubes. Sheng Wu Yi Xue Gong Cheng Xue Za Zhi 25(3):742–746
Tang T, Chen X, Meng X, Chen H, Ding Y (2005) Synthesis of multiwalled carbon nanotubes by catalytic combustion of polypropylene. Angew Chem Int Ed Engl 44(10):1517–1520. doi:10.1002/anie.200461506
Tong L, Liu Y, Dolash BD et al (2012) Label-free imaging of semiconducting and metallic carbon nanotubes in cells and mice using transient absorption microscopy. Nat Nanotechnol 7(1):56–61. doi:10.1038/nnano.2011.210
Tyurina YY, Kisin ER, Murray A et al (2011) Global phospholipidomics analysis reveals selective pulmonary peroxidation profiles upon inhalation of single-walled carbon nanotubes. ACS Nano 5(9):7342–7353. doi:10.1021/nn202201j
Villa CH, McDevitt MR, Escorcia FE et al (2008) Synthesis and biodistribution of oligonucleotide-functionalized, tumor-targetable carbon nanotubes. Nano Lett 8(12):4221–4228. doi:10.1021/nl801878d
Warheit DB, Laurence BR, Reed KL, Roach DH, Reynolds GA, Webb TR (2004) Comparative pulmonary toxicity assessment of single-wall carbon nanotubes in rats. Toxicol Sci 77(1):117–125. doi:10.1093/toxsci/kfg228
Worle-Knirsch JM, Pulskamp K, Krug HF (2006) Oops they did it again! Carbon nanotubes hoax scientists in viability assays. Nano Lett 6(6):1261–1268. doi:10.1021/nl060177c
Wu M, Gordon RE, Herbert R et al (2010) Case report: lung disease in World Trade Center responders exposed to dust and smoke: carbon nanotubes found in the lungs of World Trade Center patients and dust samples. Environ Health Perspect 118(4):499–504. doi:10.1289/ehp.0901159
Yang J, Li W, Li Q, Wu S, Yu B, Jing X (2007a) Oxygen adsorption by carbon nanotubes and its application in radiotherapy. IET Nanobiotechnol 1(1):10–14. doi:10.1049/iet-nbt:20060017
Yang S-T, Guo W, Lin Y et al (2007b) Biodistribution of pristine single-walled carbon nanotubes in vivo. J Phys Chem C 111(48):17761–17764
Yang Z, Zhang Y, Yang Y et al (2010) Pharmacological and toxicological target organelles and safe use of single-walled carbon nanotubes as drug carriers in treating Alzheimer disease. Nanomedicine 6(3):427–441. doi:10.1016/j.nano.2009.11.007
Zhang S, Li J, Lykotrafitis G, Bao G, Suresh S (2009) Size-Dependent Endocytosis of Nanoparticles. Adv Mater 21:419–424. doi:10.1002/adma.200801393
Zhang Y, Bai Y, Yan B (2010) Functionalized carbon nanotubes for potential medicinal applications. Drug Discov Today 15(11–12):428–435. doi:10.1016/j.drudis.2010.04.005
Zhao Y, Xing G, Chai Z (2008) Nanotoxicology: are carbon nanotubes safe? Nat Nanotechnol 3(4):191–192. doi:10.1038/nnano.2008.77
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ong, LC., Chung, F.FL., Tan, YF. et al. Toxicity of single-walled carbon nanotubes. Arch Toxicol 90, 103–118 (2016). https://doi.org/10.1007/s00204-014-1376-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00204-014-1376-6