Abstract
5-Sulphooxymethylfurfural (SMF), an electrophilic metabolite of the abundant Maillard product 5-hydroxymethylfurfural (HMF), was intraperitoneally administered to FVB/N mice. At a dosage of 250 mg/kg, most animals died after 5–11 days due to massive damage to proximal tubules. At lower dosages, administered repeatedly, tubules also were the major target of toxicity, with regeneration and atypical hyperplasia occurring at later periods. Additionally, hepatotoxic effects and serositis of peritoneal tissues were observed. SMF is a minor metabolite of HMF in conventional mice, but HMF is an excellent substrate for a major sulphotransferase (hSULT1A1) in humans. Parental FVB/N mice and FVB/N-hSULT1A1/2 mice, carrying multiple copies of the hSULT1A1/2 gene cluster, were exposed to HMF in drinking water (0, 134 and 536 mg/kg body mass/day) for 12 weeks. Nephrotoxic effects and enhanced proliferation of hepatocytes were only detected at the high dosage. They were mild and, surprisingly, unaffected by hSULT1A1/2 expression. Thus, SMF was a potent nephrotoxicant when administered as a bolus, but did not reach levels sufficient to produce serious toxicity when generated from HMF administered continuously via drinking water. This was even the case in transgenic mice expressing clearly higher HMF sulphation activity in liver and kidney than humans.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
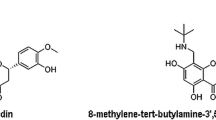
During the preparation of food numerous, new compounds are formed. One of them, present at high levels in many foods, is 5-hydroxymethylfurfural (HMF) (structural formula in Fig. 1). It is generated when reducing hexose moieties are heated in the presence of amino acids or proteins (Mauron 1981) and via acid-catalysed thermal dehydration of fructose, sucrose and glucose (Antal et al. 1990). Various studies conducted in the 1960s and 1970s consistently showed low acute and subchronic toxicity of HMF in mice and rats [reviewed by Ulbricht et al. (1984)]. However, HMF has a number of structural alerts (furan ring, α,β-unsaturated carbonyl group and allylic hydroxyl group) that point to a possible risk of genotoxic and carcinogenic activity. Indeed, it was reported that HMF initiates and promotes preneoplastic lesions (aberrant crypt foci) in rat colon (Zhang et al. 1993). HMF also demonstrated tumour-initiating activity in mouse skin, using 12-O-tetradecanoylphorbol-13-acetate as the promoter, the effect being statistically significant in the study conducted by Surh et al. (1994), but not in the initial study reported by Miyakawa et al. (1991). In a 2-year gavage study, HMF did not show evidence of carcinogenic activity in Fischer 344N rats of both sexes and in male B6C3F1 mice (NTP 2010). However, in female B6C3F1 mice, it clearly increased the incidence of hepatomas at dosages of 188 and 375 mg/kg body mass (5 times per week, equivalent to mean daily dosages of 134 and 268 mg/kg, respectively). At these doses, the incidence of hepatomas was 53 and 52%, respectively, compared to a value of 28% for the actual negative control and 22% for the mean historical negative control. The third dosage group (750 mg/kg body mass) was not included in the evaluation of carcinogenic potential because of the reduced survival and the presence of the treatment-related clinical signs. Older estimates of the mean daily intake of HMF from food are in the range of 30–150 mg per person, equivalent to 0.4–2.1 mg/kg body mass for a person of 70 kg (Ulbricht et al. 1984; Janzowski et al. 2000). Estimates from newer studies from Spain (Rufian-Henares and de la Cueva 2008), Norway (Husøy et al. 2008) and Germany (Abraham et al. 2011) are somewhat lower. A margin of exposure cannot be calculated, as appropriate carcinogenicity data are only available for two dosage levels. However, since HMF induced hepatocellular adenomas in 25% of all animals (female mice, after subtracting the spontaneous tumour incidence) even at the lowest dosage tested, it is clear the margin of exposure is below 60–300, which is exceptionally low in comparison with other food-borne carcinogens.
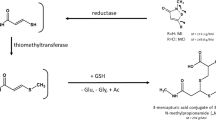
Surh and Tannenbaum (1994) found that HMF can be activated to an electrophilic sulphuric acid ester, SMF (Fig. 1), in the presence of rat hepatic cytosolic preparations fortified with the cofactor 3′-phosphoadenosine-5′-phosphosulphate. Topically applied to mouse skin, SMF exhibited higher skin tumour-initiating activity than the parent compound HMF (Surh et al. 1994). We demonstrated that biotransformation of HMF to SMF also occurs in the mouse in vivo (Monien et al. 2009). Nearly 500 ppm of the initial HMF dose reached the circulation as SMF; an unknown additional amount of SMF may have been further metabolized or reacted with cellular structures directly at the site of its formation. Interestingly, the most abundant human sulphotransferase (SULT), SULT1A1, showed higher catalytic efficiency toward HMF than any rodent form studied (Glatt and Sommer 2006). For this reason, mice and rats may not be ideal for testing the safety of HMF. Therefore, we used two alternative models. In the first model, we directly administered the reactive metabolite, SMF, to animals by intraperitoneal injection. We choose this route of administration, as natural exposure to SMF occurs via transformation of HMF within the body, rather than direct intake in the diet. Moreover, it was unlikely that the oral administration of a reactive phase-2 metabolite would lead to an appreciable systemic bioavailability. The second model involved the application of HMF in drinking water to wild-type and transgenic mice expressing high levels of human SULT1A1 and SULT1A2 in many tissues, including colonic mucosa (Dobbernack et al. 2011). Both enzymes show high catalytic efficiency using HMF as the substrate (Glatt and Sommer 2006). In this model, SMF is generated within cells and, thus, its relative levels in different tissues and cells may differ from those occurring after intraperitoneal administration of SMF. Moreover, since the tissue distribution of human SULT1A1 and SULT1A2 is similar in humans and in the transgenic mice used (Dobbernack et al. 2011), this model may best reflect human exposure to SMF.
Materials and methods
Test compounds
HMF (CAS 67-47-0, purity 99 ± 1%, determined by various methods) was a gift of Südzucker AG (Mannheim, Germany). SMF (CAS 159091-35-7; purity >99%, determined by various methods) was synthesized (Monien et al. 2009) in the laboratory of Dr. A. Seidel (Grosshansdorf, Germany).
Animals
FVB/N mice are particularly suited for gene-transfer into germ cells. Therefore, this strain was used. Wild-type FVB/N mice were purchased from Harlan-Winkelmann (Borchen, Germany) and acclimatized for a period of at least 7 days before treatment. Transgenic FVB/N mice, harbouring multiple copies of the human SULT1A1-SULT1A2 gene cluster in chromosome 9, were propagated as a homozygous line in our laboratory (Dobbernack et al. 2011). They were bread with wild-type FVB/N mice to produce hemizygous mice for the experiments (subsequently termed FVB/N-hSULT1A1/2 mice).
Animals were kept under standard temperature, humidity and timed lighting conditions. They were fed a standard mouse chow, V1124-000 (Ssniff Spezialdiäten GmbH, Soest, Germany) and had free access to tap water.
Expression of endogenous SULTs in murine tissues undergoes pronounced ontogenetic changes in the first weeks after birth (Alnouti and Klaassen 2006). Treatment was started at an age of 8–12 weeks, when the animals had surpassed this phase. Due to high sexual dimorphisms of expression of endogenous SULTs (Alnouti and Klaassen 2006), both sexes were used when testing HMF. In contrast, the ultimate genotoxicant SMF was only investigated in male wild-type mice. In the experiments, animals were housed individually. All animal experiments were performed with permission of the Landesamt für Umwelt, Gesundheit und Verbraucherschutz of the State of Brandenburg.
HMF sulphation rates in hepatic cytosolic fractions (expressed as nmol/min/mg protein) were determined as 25 (wild-type males), 117 (wild-type females), 304 (hemizygous transgenic males), 374 (hemizygous transgenic females) and 67 (humans) nmol/min/mg protein (substrate concentration 2.5 mM; means of 2–4 animals or humans); the corresponding values for kidney were 22, 30, 214, 126 and 6 nmol/min/mg, respectively [for details see (Florian et al. 2012)]. The transgenic animals expressed hSULT1A1 and hSULT1A2 protein in all these tissues (Dobbernack et al. 2011). However, since hSULT1A1 levels were higher than those of hSULT1A2—like in humans—(Dobbernack et al. 2011) and HMF is a better substrate for the former enzyme (Glatt and Sommer 2006), the enhanced HMF sulphation activity in transgenic animals appears to be primarily mediated by hSULT1A1.
Treatment regimen
Background information
The experiments were primarily designed to study whether SMF, administered directly or formed metabolically from HMF, is able to induce the formation of aberrant crypt foci in the colon of mice. The results have been presented elsewhere (Florian et al. 2012). The same animals were used in the present study for investigating adverse effects in tissues other than colon.
The doses of HMF used [536 mg (4.3 mmol) and 134 mg (1.1 mmol)/kg body mass/d] were based on doses employed in the study of the National Toxicology Programme of the USA (NTP) (2010). In the first experiment, SMF was used at a dose [250 mg (1.1 mmol)/kg body mass/treatment] equimolar to the lower HMF dose. In a pilot experiment, we had administered this dose to a small number of animals to study the formation of DNA adducts (the result was negative, but the 32P post-labelling method used was inadequate for the detection of these adducts, as noticed later as). The animals appeared to tolerate this dose well, but were killed within 48 h. Therefore, we did not recognize delayed effects, a mistake manifested in experiment 1 with SMF (next paragraph).
Experiments with SMF
SMF has a half-life time of 2 h in aqueous solution at 37°C (Glatt and Sommer 2006). It was dissolved in saline immediately before use. It was verified that less than 2% of the test compound was decomposed before injection. In all experiments, it was administered intraperitoneally to young adult male FVB/N mice (8- to 12-week old at first treatment). In the first experiment, 35 animals received a single dose of 250 mg (1.1 mmol) SMF/kg. An equal number of animals was only treated with saline and served as control. Due to the dramatic effect of SMF in this experiment, not all control animals were required for histological analysis. The remaining 14 animals were used in a second experiment with the aim to better estimate the maximum tolerated dose level. Four animals per group were treated twice (with an interval of 7 days) at dosages of 31.25 mg (0.14 mmol), 62.5 mg (0.27 mmol) and 125 mg (0.55 mmol) SMF/kg. The other two animals were used as negative controls. The animals were killed 8 weeks after the last treatment. The third (final) experiment involved 105 animals divided into four treatment groups. The groups received four intraperitoneal administrations of the following test compounds at one-week intervals: 62.5 mg (0.27 mmol) SMF/kg (number of animals, n = 35), 125 mg (0.55 mmol) SMF/kg (n = 15), 10 mg azoxymethane/kg (n = 20) or the vehicle only (saline, n = 35), with intervals of 1 week between the treatments. The azoxymethane-treated animals were only used as a positive control for the induction of aberrant crypt foci and tumours in colon; other tissues were not histologically examined. Subgroups of animals were killed at varying times after the last treatment, as indicated in Table 3. Animals were randomly assigned to these groups and subgroups at the beginning of the experiment.
Experiment with HMF
HMF was given in the drinking water. The dosages were based on those used in a 2-year gavage study (750, 375 and 188 mg/kg body mass, 5 times per week) conducted in the NTP study (2010). The high and low dosages of that study are equivalent to 536 mg (4.3 mmol) and 134 mg (1.1 mmol) per kg body mass, respectively, if given daily rather than only five times a week. Male and female wild-type FVB/N and heterozygous FVB/N-hSULT1A1/2 animals (6 animals per group, 8 weeks old at the beginning of the treatment) received these dosages in drinking water daily for 12 weeks. The concentration of HMF in the flasks was adjusted to the average daily water consumption. The drinking water was changed weekly. The stability of HMF in water over this period was verified using HPLC–UV analyses.
Tissue preparation and histology
The animals were killed by cervical dislocation. Organs were removed and prepared in a standardized procedure. A thorough pathologic anatomical examination was performed on each animal. Samples of various tissues (specified in the results section) were fixed in 4% buffered (pH 7.0) formalin for 24 h, embedded in paraffin, cut into 2-μm sections and stained. Three different stainings were used for neighbouring sections: haematoxylin-eosin, Perl’s blue and Okajima’s stain for haemoglobin (Romeis 1989). Tissue sections were viewed under a light microscope (E 1000, Nikon, Düsseldorf, Germany).
In the study on HMF, renal damage was scored in coded samples from the individual animals based on the following five pathomorphological parameters: cell death, mononuclear infiltrates with regenerates, interstitial nephritis, tubulitis and tubular damage; each parameter got a score from 0 (no damage) to 3 (strong damage). They were added to give the total score, which therefore could range between 0 and 15. Scoring was performed by a veterinarian who had conducted her habilitation work on kidney pathology.
Immunohistochemical detection of proliferation marker
Ki-67-immunohistochemistry was performed in kidney and liver sections in HMF-treated and control animals in order to detect proliferative cells as described previously (Bauer-Marinovic et al. 2006). In short, slides were immersed in boiling Target Retrieval Solution (ChemMateTM, DakoCytomation, Hamburg, Germany) and incubated overnight with primary antibody for Ki-67 (TEC-3, DakoCytomation) diluted in antibody diluent (DakoCytomation). A polymer-conjugated secondary antibody [N-Histofine® Simple Stain Mouse MAX PO (Rat), Nichirei Bioscience, Tokyo, Japan] was applied followed by visualization via diaminobenzidine (DakoCytomation).
Results
Effects of SMF directly administered to mice
Experiment 1 (single treatment with 250 mg SMF/kg)
SMF-treated animals appeared apathetic compared to vehicle-treated controls in the first hours after the injection. They recovered quickly and no obvious differences from the controls were noticed in the next 4 days. However, on days 5 and 6, several SMF-treated animals died and the others had developed impaired body conditions, such as rough fur, boarded abdomen, reluctance to move and hunched posture as well as lethargy or recumbency. A total of 20 of 35 animals died between days 5 and 11 after SMF treatment. Ten moribund animals were euthanized between days 6 and 9. The remaining five animals of the SMF group survived and were killed at varying later time points (2–40 weeks after the treatment) for preliminary histological analysis (which agreed with findings from the much more comprehensive final experiment and thus are not presented).
The mice killed in moribund state had pale and swollen kidneys as well as hepatomegaly on dissection. There was dark discoloration of the faeces. Acute necrosis of fatty tissue at the caudal pole of the right kidney was detected in one animal. Two animals showed adhesions between liver and intestine as well as between liver and kidney.
Histopathological lesions in SMF-treated animals, compared to controls, were observed in liver and kidneys (summarized in Table 1), but not in the other tissues investigated (myocardium, urinary bladder, lung, pancreas, spleen, stomach, duodenum, jejunum, ileum, caecum and colon). In six of ten animals >75% of the tubules in the kidney cortex had undergone acute necrosis (Fig. 2a, b). Acute necrosis was more pronounced in proximal tubules, but also occurred in distal tubules to a lesser extent. Massive formation of proteinaceous casts was observed in the outer and inner stripe of the renal medulla as well as in the collecting ducts (Fig. 2c). Glomerular lesions were mild and involved focal necrosis of parietal cells of the Bowman’s capsule. Mild granulocytic infiltrates were present in some glomeruli.
Renal and hepatic lesions in FVB/N mice killed 6–9 days after a single intraperitoneal administration of SMF (250 mg/kg). All sections were stained with haematoxylin and eosin. a acute tubular necrosis in kidney cortex; b high-magnification view of necrotic tubules; c protein casts in the outer strip of the renal medulla; d nodular hyperplasia and disarray of hepatic architecture; e acute centrilobular necrosis of liver–note the swollen Kupffer cells (arrows) and the absence of reactive leucocytic infiltrates
Hepatic lesions were present in all SMF-treated animals. There was scattered acute necrosis of hepatocytes. In some cases, clusters of necrotic cells were located in centrilobular areas (Fig. 2e), whereas in most cases, the necrotic cells were single cells scattered throughout the lobule. Three animals showed nodular hyperplasia (Fig. 2d). Pleomorphism of hepatocytes and cellular hyperplasia was found in four animals. Swelling of Kupffer cells was observed in all animals (Fig. 2e). Focal fibrosis, fibrin exudates along with infiltrates of macrophages and lymphocytes were present in the overlaying liver serosa of five animals. Three animals showed focal coagulation necrosis of hepatocytes adjacent to the organ surface. None of these histological anomalies (summarized in Table 1) was observed in control animals.
Experiment 2 (two treatments with 31.25–125 mg SMF/kg)
After the unexpected high toxicity in the initial experiment, we tested several lower dosages in relatively small groups of animals. Body condition was not altered in any SMF treatment group compared to controls through the time of killing, 8 weeks after the second treatment. Hepatomegaly was present in six animals (in 2 of 4 mice at the high dosage, 3 of 4 mice at the middle dosage and 1 of 4 mice at the low dosage). Likewise, adhesions of liver to the diaphragm or the right kidney were observed (in 3 high-dosage and all 4 mid-dosage animals).
Histological lesions observed in experiment 2 are summarized in Table 2. Significant morphological lesions were serositis and fibrosis of the serosal surfaces of tissues that got into direct contact with the intraperitoneally administered compound (liver, stomach, intestine, kidneys and spleen). Adhesion between the hepatic and the renal serosal surface was detected in some animals. Regenerative tubules and protein casts were present in the kidneys of animals treated with 125 mg SMF/kg. No significant morphologic lesions were detected in lung, myocardium, pancreas, duodenum, colon (apart from serositis in one animal) and urinary bladder. No morphological lesions were observed in the control group.
Experiment 3 (4 treatments with 62.5 and 125 mg SMF/kg, extended observation period)
The mean body masses of mice showed no statistically significant differences at any time point or dosage compared to the negative control group [see Florian et al. (2012)].
Kidneys and livers of vehicle-control and SMF treatment groups were analysed for histopathological changes (Table 3; Fig. 3). All 14 animals of the high-SMF-dosage group (killed at varying times) had developed fibrosis of the hepatic surface (Fig. 3c; Table 3) and, except two animals, also of the renal serosa (Table 3). In the liver, this effect also occurred in most animals (20/35) of the low-SMF-dosage group, but not in vehicle-control animals (0/31). Proteinaceous casts in the kidneys were observed in 93% of the animals (13/14) of the high-SMF-dosage group, but only in 23% (8/35) and 16% (5/31) of the low-dosage and vehicle-control groups, respectively (Table 3). Regenerative tubules (Fig. 3a) were present up to week 14 after the last treatment with SMF in all animals of the high-dosage group (8/8), but were less common in the low-dosage subgroups (5/21) and vehicle-control subgroups (1/18) killed in same observation period (Table 3). They were absent in all three groups at later time points. Focal hyperplasia and in some cases also atypical hyperplasia (Fig. 3b) of renal tubules were detected in 2 of 10 mice treated with SMF after 20 weeks and in 8 of 10 animals after 40 weeks (Table 3).
Renal and hepatic lesions in FVB/N mice after four intraperitoneal treatments with SMF (125 mg/kg/treatment, with one-week intervals). All sections were stained with haematoxylin and eosin. a regenerative tubules 8 weeks after the last SMF treatment; b hyperplasia of renal tubules 14 weeks after the last SMF treatment; c marked fibrosis of the hepatic serosal surface 14 weeks after the last SMF treatment–arrows mark mature collagen
In addition, a number of minor histological anomalies were detected in the liver of some animals. Pigment storage was noticed in 8 of 10 animals at the first observation period after SMF treatment and in a single SMF-treated animal at a later observation point. Single-cell necrosis was sporadically observed in SMF-treated animals, whereas focal infiltrations were found in various animals of the vehicle-control and low-SMF-dosage groups, but not in the high-SMF-dosage group.
Effects of HMF in wild-type and transgenic (high-SULT) mice
Consumption of drinking water and food as well as body mass development was similar in HMF-treated (134 or 536 mg/kg/d) and control animals [see Florian et al. (2012)]. Kidneys and livers of wild-type FVB/N and transgenic FVB/N-SULT1A1/2 mice treated with HMF did not show any macroscopic changes compared to control animals. Likewise, no changes were microscopically detected in liver. Minor lesions were observed in kidney. They involved cell deaths, mononuclear infiltrates, limited areas of interstitial nephritis, tubulitis and/or tubular damage. Damage areas ranged from only few cells to areas with a maximal extension of 300 μm (Fig. 1A-B of Supplementary Material). The lesions were combined to a score. In all four experimental series (wild-type males, transgenic males, wild-type females and transgenic females), the highest median scores were observed in the high-HMF-dosage group (Fig. 4). This consistency suggests that the effects were real in all groups, although statistical significance could only be demonstrated for the wild-type female series. Our findings are similar to those reported for HMF in a 3-month gavage study in C3B6F1 mice (NTP 2010): in that study, the incidences of minimal to mild cytoplasmic alteration of the kidney were significantly increased in males of the 188-, 375- and 750-mg/kg-dosage groups.
Pathomorphological score of the kidney of wild-type FVB/N (wt) and transgenic FVB/N-SULT1A1/2 (tg) mice receiving 0, 134 or 536 mg HMF/kg body mass/day in the drinking water for 12 weeks. Values for the individual animals (points) and their medians (lines) are presented. *p < 0.05 (Mann–Whitney U test compared to vehicle control)
Additionally, we studied the expression of the proliferation marker Ki-67 in sections of renal and hepatic tissue. An increased proliferation would indicate a regenerative activity of the tissue as a result of previous lesions occurring over the course of twelve experimental weeks. However, Ki-67-immunoreactivity in kidneys was largely restricted to infiltrating mononuclear cells in areas of interstitial nephritis (Fig. 1B-C of Supplementary Material). Kidneys were semi-quantitatively scored in three grades according to the frequency of Ki-67-positive cells. The results suggest increased infiltration by proliferative cells: eight of 24 animals in the high-HMF-dosage groups showed grade-2 and/or grade-3 responses (males and females, wild-type and transgenic animals combined), whereas only six and four of 24 animals reached grade-2 responses in the other groups (low HMF dosage and negative controls, respectively) (Table 1 of Supplementary Material). In the liver, Ki-67 immunoreactivity was primarily detected in hepatocytes rather than infiltrating cells (Fig. 1D of Supplementary Material). Only in female transgenic mice of the high dosage, the count of Ki-67-positive hepatocytes was significantly higher compared with the control group (Fig. 5).
Count of Ki-67-positive hepatocytes in liver sections of wild-type FVB/N (wt) and transgenic FVB/N-SULT1A1/2 (tg) mice receiving 0, 134 or 536 mg HMF/kg body mass/day in the drinking water for 12 weeks. Values for the individual animals (points) and their medians (lines) are presented. *p < 0.05 (Mann–Whitney U test compared to vehicle control)
Discussion
In experiments designed to study the induction of aberrant crypt foci, we detected high acute toxicity of SMF. After a single dose of 250 mg/kg, 20 of 35 mice died within 5–11 days. Ten further animals that were in extremely bad conditions were euthanized. However, all but one animals (4 of 4 in experiment 2 and 13 of 14 in experiment 3) receiving the next lower dosage (125 mg/kg) survived the treatment. Thus, the acute lethal dose for 50% of the treated animals (LD50) of SMF was above 125 mg/kg, but below 250 mg/kg. Three major target sites for SMF were detected, the serosas of organs located in the peritoneal cavity, the liver and the kidneys.
Serositis and reactive fibrosis were observed in the liver and kidneys of nearly all animals dosed at 125 or 250 mg SMF/kg. Spleen, stomach and/or intestines were also affected in some animals. Serositis and reactive fibrosis are indicative for local tissue damage after the intraperitoneal injection, probably due to the alkylating properties of SMF.
Sulpho conjugates are terminal metabolites of numerous xenobiotics and are excreted in bile or urine. If they are produced elsewhere, concentrative uptake into liver and kidney often occurs. We have shown that SMF is a substrate for human organic anion transporters (OAT) 1 and 3 (Bakhiya et al. 2009). These transporters are expressed in renal tubules with high tissue and cell selectivity; they mediate the renal excretion of numerous anionic metabolites of drugs and other xenobiotics (Burckhardt and Burckhardt 2003). Various other anion transporters, such as OATPs (organic anion transporting peptides), MRPs (multidrug-resistance-associated proteins) and BCRP (breast cancer resistance protein), able to transport organic anions across cells, occur in liver (Chandra and Brouwer 2004) and may be involved in the uptake of SMF (e.g., when administered intraperitoneally) or its extrusion (e.g., when formed by hepatic SULTs from HMF). This biological mechanism may play a role in the hepatic and renal organotropism observed with SMF.
Acute hepatic necrosis was present in all ten animals that had received 250 mg SMF/kg and were available for analysis. Foci of hepatic hyperplasia were developed in three animals. This hyperplasia represents an early stage in hepatic tumorigenesis. Interestingly, a single intraperitoneal dose of 5-chloromethylfurfural, an uncharged analogue of SMF, induced high incidences and multiplicities of hepatomas in newborn mice (Surh et al. 1994). However, hepatic damage by SMF, apart from serositis and fibrosis, was essentially restricted to the highest dosage level (250 mg/kg) in our study.
SMF induced the most impressive lesions in the kidneys. Nearly all proximal tubules were completely destroyed in the moribund mice euthanized in the initial experiment, in which a dosage of 250 mg SMF/kg was used. Therefore, it is probable that renal failure was the cause of the many spontaneous deaths in this group of animals. In the subsequent experiments, lower dosages were used and histological analyses were conducted at later stages (4–40 weeks after the last treatment). Although tubular necrosis was still observed in individual animals in week 4, sequelae dominated the histological lesions observed in this experiment. Regeneration of renal tubules was found until week 14, whereas proteinaceous casts were still present in week 40 after the last SMF treatment. Atypical hyperplasia was absent in control animals, but was seen with a lag period in SMF-treated animals. Its incidence in SMF-treated animals increased to 80% (8 of 10 mice) by the latest study time, 40 weeks after treatment. Further studies would be required to see whether these hyperplasias progress to clear cell carcinomas.
Humans are not directly exposed to SMF, but this short-lived reactive molecule may be metabolically formed from a common heat-induced food constituent, HMF. Therefore, the question arises whether the SMF formed during this biotransformation can reach levels sufficient to evoke adverse effects in humans. This is difficult to test in conventional mouse and rat models due to species-dependent differences in the SULT. Among the human, rat and mouse SULT forms tested, human SULT1A1 demonstrated the highest catalytic efficiency (Glatt and Sommer 2006; Sommer 2006). Moreover, this form is distributed at high levels in many different tissues (Teubner et al. 2007). Recently, we constructed a series of mouse lines harbouring the human SULT1A1-SULT1A2 gene cluster, including large flanking sequences containing regulatory elements (Dobbernack et al. 2011). The lines differed in the number of copies of the SULT1A1-SULT1A2 gene cluster integrated into the mouse genome. To be on the safe side, we used the line with the highest copy number (approximately 43 in hemizygous animals) in the present study. A copy number polymorphism of the SULT1A1 gene occurs in humans, with up to five copies being detected in some subjects (Hebbring et al. 2007). Liver, kidney and colon mucosa of these animals express clearly higher HMF SULT activity than corresponding tissues of wild-type mice [“Animals” section; further information in Florian et al. (2012)]. Nevertheless, HMF–administered at high dosages via the drinking water for 12 weeks–only showed mild toxic effects to both wild-type and transgenic mice, primarily in kidneys; as the effects were similar in both mouse strains, it is not clear whether SMF was causally involved in the toxicity. As outlined in preceding sections, SMF is actively taken up from blood into proximal tubule cells by organic anion transporters. Therefore, blood levels of SMF will be important. Nearly 500 ppm of the HMF dose reaches the circulation as SMF in male wild-type FVB/N mice (Monien et al. 2011). As a first estimate, this level may be approximately 12-fold higher (6,000 ppm) in transgenic animals, which express 12-fold higher HMF SULT activity in the liver, a large organ with high xenobiotic-metabolizing activities. At a dosage of 536 mg (4.3 mmol) HMF/kg, this would be 5.8 mg (25.8 μmol) SMF/kg, which is less than a dosage of SMF [31.25 mg (140 μmol)/kg] that did not produce detectable toxicity in our study. In this comparison, it was not taken into account that HMF was administered for 84 days, whereas SMF was only given once in the mentioned experiment (experiment 1). However, it is also evident from our experiments that splitting the dosage of SMF into a number of lower dosages given at separate times strongly reduces its toxicity. A dosage of 250 mg (1.1 mmol) SMF/kg given at once was lethal for most animals in experiment 1. When the same total dosage was given over a period of 3 weeks (4 treatments with 62.5 mg/kg/treatment at one-week intervals) in experiment 3, only relatively mild toxicity was noticed.
In the present study, a dosage of HMF of 536 mg/kg/d was required to produce some toxic effects. This dosage is far above the highest estimate for the average daily intake in humans, 150 mg per person (Ulbricht et al. 1984), equivalent to 2.1 mg/kg for a person of 70 kg body mass. Toxic effects at this high dosage of HMF were mild even in mice showing high HMF SULT activity [approximately 5-fold higher in liver compared to human samples (Florian et al. 2012)]: taken together, these data suggest that the relatively high HMF SULT activity in humans, compared to conventional animal models, does not pose a significant risk for nephro- and hepatotoxic effects of HMF ingested from food.
What remains to be studied is a possible genotoxic activity of HMF and SMF in vivo and its role in the carcinogenic effects observed with HMF. Recently, Durling et al. (2009) reported that HMF induced DNA damage, as assessed by the comet assay, in various mammalian cell lines in culture. This effect was independent of the presence of HMF SULT activity or hSULT1A1 expression. However, the minimal concentration for a positive test was extremely high [25 mM in control V79 and V79-hP-PST cells (expressing hSULT1A1), 100 mM in the other cell lines used], far above the K m of hSULT1A1 for HMF [2.5 mM (Glatt and Sommer 2006)]. On the contrary, HMF showed another genotoxic effect, the induction of sister chromatid exchanges, even at 19.8 μM in hSULT1A1-expressing V79 cells; this effect was clearly dependent on the expression of hSULT1A1 (Glatt et al. 2005). Likewise, HMF induced gene mutations (Glatt and Sommer 2006) and formed DNA adducts, as detected by UPLC-MS/MS analysis (B. Monien, G. Barknowitz and H. R. Glatt, manuscript in preparation) in V79-hP-PST, but not in parental V79 cells. In this context, it is interesting to know that HMF induced hepatic tumours in female, but not male, mice. This sex specificity correlates with a markedly (4.7-fold) higher hepatic HMF SULT activity in female, compared to male, wild-type mice (“Animals” section). The chief target tissues were the same in the NTP study on HMF (NTP 2010) and in the present study on SMF: liver and kidneys, but the order of the strength of the effects was reverse. In the NTP study, liver was the site of tumorigenesis, with mild microscopic changes being observed in kidneys in the 3-month study; in contrast, SMF destroyed the tubules, but only showed moderate toxicity to liver in our study. However, the toxicokinetic situation is different between the studies. After HMF administration, SMF is primarily formed in the liver and has to be exported into the circulation to produce effects in other tissues; in contrast, uptake of SMF into liver cells is required to induce hepatotoxic effects after the direct administration of the metabolite SMF.
Interestingly, furfuryl alcohol, a congener of HMF lacking the aldehyde group in 2 position, showed some evidence of carcinogenic activity in an inhalation study based on increased incidences of renal tubule neoplasms in male B6C3F1 mice (NTP 1999). Thus, furfuryl sulphate, a mutagenic metabolite of furfuryl alcohol (Glatt et al. 2012), may be a better substrate for hepatic export systems and/or renal import systems. Moreover, furfuryl alcohol indicated some carcinogenic activity in the mucosa of the nasal cavity of mice and rats (NTP 1999), another tissue with high SULT activity (Tamura et al. 1997). Finally, furfuryl alcohol formed the same benzylic DNA adducts in mouse tissues, as are formed by furfuryl sulphate in cell-free systems (Monien et al. 2011). Altogether, a possible role of sulphation in the carcinogenic effects observed in animal models with hydroxymethylated furan derivatives deserves further investigations.
References
Abraham K, Gürtler R, Berg K, Heinemeyer G, Lampen A, Appel KE (2011) Toxicology and risk assessment of 5-hydroxymethylfurfural in food. Mol Nutr Food Res 55:667–678
Alnouti Y, Klaassen CD (2006) Tissue distribution and ontogeny of sulfotransferase enzymes in mice. Toxicol Sci 93:242–255
Antal MJ Jr, Mok WS, Richards GN (1990) Mechanism of formation of 5-(hydroxymethyl)-2-furaldehyde from d-fructose and sucrose. Carbohydr Res 199:91–109
Bakhiya N, Monien B, Frank H, Seidel A, Glatt HR (2009) Renal organic anion transporters OAT1 and OAT3 mediate the cellular accumulation of 5-sulfooxymethylfurfural, a reactive, nephrotoxic metabolite of the Maillard product 5-hydroxymethylfurfural. Biochem Pharmacol 78:414–419
Bauer-Marinovic M, Florian S, Müller-Schmehl K, Glatt HR, Jacobasch G (2006) Dietary resistant starch type 3 prevents tumor induction by 1,2-dimethylhydrazine and alters proliferation, apoptosis and dedifferentiation in rat colon. Carcinogenesis 27:1849–1859
Burckhardt BC, Burckhardt G (2003) Transport of organic anions across the basolateral membrane of proximal tubule cells. Rev Physiol Biochem Pharmacol 146:95–158
Chandra P, Brouwer KL (2004) The complexities of hepatic drug transport: current knowledge and emerging concepts. Pharm Res 21:719–735
Dobbernack G, Meinl W, Schade N, Florian S, Wend K, Voigt I, Himmelbauer H, Gross M, Liehr T, Glatt HR (2011) Altered tissue distribution of 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine DNA adducts in mice transgenic for human sulfotransferases 1A1 and 1A2. Carcinogenesis 32:1734–1740
Durling LJ, Busk L, Hellman BE (2009) Evaluation of the DNA damaging effect of the heat-induced food toxicant 5-hydroxymethylfurfural (HMF) in various cell lines with different activities of sulfotransferases. Food Chem Toxicol 47:880–884
Florian S, Bauer-Marinovic M, Taugner F, Dobbernack G, Monien BH, Meinl W, Glatt HR (2012) Study of 5-hydroxymethylfurfural and its metabolite 5-sulfooxymethylfurfural on induction of colonic aberrant crypt foci in wild-type mice and transgenic mice expressing human sulfotransferases 1A1 and 1A2. Mol Nutr Food Res. doi:10.1002/mnfr.201100574
Glatt HR, Sommer Y (2006) Health risks by 5-hydroxymethylfurfural (HMF) and related compounds. In: Skog K, Alexander J (eds) Acrylamide and other health hazardous compounds in heat-treated foods. Woodhead Publishing, Cambridge, pp 328–357
Glatt HR, Schneider H, Liu Y-G (2005) V79-hCYP2E1-hSULT1A1, a cell line for the sensitive detection of genotoxic effects induced by carbohydrate pyrolysis products and other food-borne chemicals. Mutat Res 580:41–52
Glatt HR, Schneider H, Murkovic M, Monien BH, Meinl W (2012) Hydroxymethyl-substituted furans: mutagenicity in Salmonella typhimurium strains engineered for expression of various human and rodent sulphotransferases. Mutagenesis 27:41–48
Hebbring SJ, Adjei AA, Baer JL, Jenkins GD, Zhang J, Cunningham JM, Schaid DJ, Weinshilboum RM, Thibodeau SN (2007) Human SULT1A1 gene: copy number differences and functional implications. Hum Mol Genet 16:463–470
Husøy T, Haugen M, Murkovic M, Jöbstl D, Stølen LH, Bjellaas T, Rønningborg C, Glatt HR, Alexander J (2008) Dietary exposure to 5-hydroxymethylfurfural from Norwegian food and correlations with urine metabolites of short-term exposure. Food Chem Toxicol 46:3697–3702
Janzowski C, Glaab V, Samimi E, Schlatter J, Eisenbrand G (2000) 5-Hydroxymethylfurfural: assessment of mutagenicity, DNA-damaging potential and reactivity towards cellular glutathione. Food Chem Toxicol 38:801–809
Mauron J (1981) The Maillard reaction in food; a critical review from the nutritional standpoint. Prog Food Nutr Sci 5:5–35
Miyakawa Y, Nishi Y, Kato K, Sato H, Takahashi M, Hayashi Y (1991) Initiating activity of eight pyrolysates of carbohydrates in a two-stage mouse skin tumorigenesis model. Carcinogenesis 12:1169–1173
Monien BH, Frank H, Seidel A, Glatt HR (2009) Conversion of the common food constituent 5-hydroxymethylfurfural into a mutagenic and carcinogenic sulfuric acid ester in the mouse in vivo. Chem Res Toxicol 22:1123–1128
Monien BH, Herrmann K, Meinl W, Glatt HR (2011) Furfuryl alcohol: mutagenicity and DNA adducts in Salmonella typhimurium strains expressing human sulfotransferase 1A1 and formation of the same adducts in mouse tissues in vivo. Carcinogenesis 32:1533–1539
NTP (1999) Toxicology and carcinogenesis studies of furfuryl alcohol (CAS No.98-00-0) in F344/N rats and B6C3F1 mice (inhalation studies). Natl Toxicol Program Tech Report Ser 482:1–248
NTP (2010) Toxicology and carcinogenesis studies of 5-(hydroxymethyl)-2-furfural (CAS No. 67–47-0) in F344/N rats and B6C3F1 mice (gavage studies). Natl Toxicol Program Tech Report Ser 554:1–180
Romeis B (1989) Mikroskopische Technik/Romeis. München—Wien—Baltimore, Urban & Schwarzenberg
Rufian-Henares JA, de la Cueva SP (2008) Assessment of hydroxymethylfurfural intake in the Spanish diet. Food Addit Contam Part A 25:1306–1312
Sommer Y (2006) 5-(Hydroxymethyl)-2-furfural: Sulfokonjugation und ihre Bedeutung für die Genotoxizität. University of Potsdam, Potsdam
Surh YJ, Tannenbaum SR (1994) Activation of the Maillard reaction product 5-(hydroxymethyl) furfural to strong mutagens via allylic sulfonation and chlorination. Chem Res Toxicol 7:313–318
Surh YJ, Liem A, Miller JA, Tannenbaum SR (1994) 5-Sulfooxymethylfurfural as a possible ultimate mutagenic and carcinogenic metabolite of the Maillard reaction product, 5-hydroxymethylfurfural. Carcinogenesis 15:2375–2377
Tamura H, Miyawaki A, Inoh N, Harada Y, Mikoshiba K, Matsui M (1997) High sulfotransferase activity for phenolic aromatic odorants present in the mouse olfactory organ. Chem-Biol Interact 104:1–9
Teubner W, Meinl W, Florian S, Kretzschmar M, Glatt HR (2007) Identification and localization of soluble sulfotransferases in the human gastrointestinal tract. Biochem J 404:207–215
Ulbricht RJ, Northup SJ, Thomas JA (1984) A review of 5-hydroxymethylfurfural (HMF) in parenteral solutions. Fundam Appl Toxicol 4:843–853
Zhang X-M, Chan CC, Stamp D, Minkin S, Archer MC, Bruce WR (1993) Initiation and promotion of colonic aberrant crypt foci in rats by 5-hydroxymethyl-2-furaldehyde in thermolyzed sucrose. Carcinogenesis 14:773–775
Acknowledgments
We thank Ms. Swetlana König, Elisabeth Meyer and Elke Thom for excellent technical assistance, Dr. Gunhild Kozianowski (Südzucker AG, Mannheim, Germany) for a gift of HMF, and Drs. Albrecht Seidel and Heinz Frank (Biochemical Institute for Environmental Carcinogens, Prof. Dr. Gernot Grimmer Foundation, Grosshansdorf, Germany) for synthesizing SMF. This work has been carried out with support from the European Commission, Priority 5 on Food Quality and Safety (Contract no FOOD-CT-2003-506820 Specific Targeted Project), “Heat-generated food toxicants—identification, characterization and risk minimization”. This publication reflects the authors views and not necessarily those of the EC. The information in this document is provided as is and no guarantee or warranty is given that the information is fit for any particular purpose. The user thereof uses the information at his/her sole risk and liability.
Conflict of interest
Authors declare not having any financial or personal interest, nor having an association with any individuals or organizations that could have influenced inappropriately the submitted work.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bauer-Marinovic, M., Taugner, F., Florian, S. et al. Toxicity studies with 5-hydroxymethylfurfural and its metabolite 5-sulphooxymethylfurfural in wild-type mice and transgenic mice expressing human sulphotransferases 1A1 and 1A2. Arch Toxicol 86, 701–711 (2012). https://doi.org/10.1007/s00204-012-0807-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00204-012-0807-5