Abstract
In order to survey changes and activities in the polycyclic aromatic hydrocarbon (PAH)-metabolizing enzymes implicated in lung cancer susceptibility studies, we investigated enzyme induction by 2–5-ring-sized ‘biomarker’ PAHs in rat liver and lung, and the activities in five human lung specimens. Naphthalene, phenanthrene, pyrene, chrysene, and benzo[a]pyrene (BaP) were administered to rats for 3 days (25–128 mg/kg/day) and the responses compared with those of model inducers. PAH treatment increased the CYP1A-catalyzed activity of pyrene 1-hydroxylation and 7-ethoxyresorufin O-deethylation in rat liver by up to 28- and 279-fold, and in rat lung by up to 22- and 51-fold, respectively. 1-Naphthol (hUGT1A6), 1-hydroxypyrene (hUGT1A6/1A9), and entacapone (hUGT1A9) are markers of PAH-glucuronidating human uridine diphosphate-glucuronosyltransferases (UGT). These activities increased up to 6.4-fold in rat liver and up to 1.9-fold in rat lung. NADPH:quinone oxidoreductase 1 (NQO1) and glutathione S-transferase activities increased up to 5.3- and 1.6-fold (liver), and up to 4.4- and 1.4-fold (lung), respectively. CYP1A showed the best liver-to-lung relationship (R 2 = 0.90). The inducing efficiency by PAHs differed extensively: control ≤ naphthalene < phenanthrene, pyrene << chrysene < BaP. In human lung (non-smokers), the marker activities of CYP1A1, UGT1A6/1A9, and NQO1 were lower than those in rat lung. Epoxide hydrolase activity was 1,000-fold higher than the pulmonary CYP1A1 activities. Human UGT and NQO1 displayed large variations (>60-fold), many times greater than the experimental (inducible/constitutive) variation in the rat. Kinetics of 1-hydroxypyrene glucuronidation showed two low-K m forms both in rat and human lung. Since the 2–4-ring PAHs (major constituents) were poor enzyme inducers, it appears that the PAH-metabolizing pathways are mainly induced by BaP-type minor constituents. Gene–environmental interactions which magnify polymorphic variability in pulmonary bioactivation/detoxification capacity probably play a key role in individual susceptibility to (or protection against) chemically induced lung cancer. Hence, human exposure to PAH mixtures with high content of BaP-type hydrocarbons confers a potentially higher health risk than PAH mixtures with low content of procarcinogens.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Polycyclic aromatic hydrocarbons (PAHs) are carcinogenic environmental pollutants arising from incomplete combustion or pyrolysis of organic material. Exposure to PAHs has been associated with adverse effects on human health, including the risk of cancer (ACGIH 2005; IARC 1985). Humans are exposed to PAHs via a variety of sources such as diet, tobacco smoking, and environment (Hecht 2002). Of greatest concern is, however, the health of employees in factories and other areas where PAH measurements show high uptake levels. The body burden of PAH workers may well exceed by 10–1,000 times the values of non-occupationally exposed people (Grainger et al. 2004; Huang et al. 2004; UBA 1998; Yang et al. 1999). In practice, the internal exposure levels are assessed by biological monitoring. Urinary metabolites of naphthalene, phenanthrene, chrysene, pyrene, and benzo[a]pyrene (BaP) are biomarkers of PAH exposure, and for this reason, studies into these PAHs are of interest to occupational exposure and hazard assessment (Angerer et al. 1997; Grimmer et al. 1997). The first four of these compounds belong to the main constituents of PAH mixtures, whereas BaP denotes a much smaller but hazardous fraction of poorly volatile (particulate), large molecular size substances in which BaP and many other compounds are procarcinogens (ACGIH 2005; Bouchard and Viau 1999; Elovaara et al. 1995a).
Drug and carcinogen metabolizing enzymes are regarded as one class of environmental susceptibility genes (Guengerich 2000; Pelkonen and Nebert 1982; Pelkonen et al. 1999; Thier et al. 2003). In the case of lung cancer, polymorphism in metabolic genes confers a much higher risk in smokers than in non-smokers, indicating that genetic polymorphism per se is not crucial in the absence of carcinogenic exposure (Vineis 2004). The complex relationship between polymorphism, carcinogen dose, and lung cancer is influenced by enzyme induction of pathways which biotransform PAH procarcinogens into highly mutagenic diol epoxides, radical cations, and o-quinones (Conney 1982; Gelboin 1980; Penning et al. 1999). Many of the cancer susceptibility enzymes are coordinately inducible proteins. This means that the intraindividual tissue activity levels may vary multifold due to gene–environmental interactions.
The following PAH metabolizing ‘susceptibility’ enzymes were studied in this work: CYP1A1 (Nebert et al. 2004; Shimada et al. 1992; Shimada and Fujii-Kuriyama 2004), microsomal epoxide hydrolase (mEH) (Gelboin 1980; Kiyohara et al. 2002), NADPH:quinone oxidoreductase 1 (NQO1) (Jaiswal 2000; Joseph and Jaiswal 1994), uridine diphosphate (UDP)-glucuronosyltransferase (UGT) (Burchell et al. 1998; Bock et al. 1998; Zheng et al. 2002), and glutathione S-transferase (GST) (Hayes et al. 2005). CYP1A1 is inducibly expressed in human lung (Hukkanen et al. 2002; Kim et al. 2004a). Both 7-ethoxyresorufin O-deethylase (EROD) and pyrene 1-hydroxylase (PH) are markers of CYP1A1 activity. Pyrene is hydroxylated to 1-OHP (1-hydroxypyrene) mainly by CYP1A1 in lung microsomes from smokers (Elovaara et al. 1995b). This reaction is highly catalyzed by CYP1A1, less by CYP1B1 and CYP1A2, while 2A6, 2C8, 2C9*1, 2C19, 2D6, 2E1, and 3A4 show little activity (Kim et al. 2004b). 1-Naphthol, 1-OHP, and entacapone are sensitive substrates for detecting UGT1A induction (Elovaara et al. 2004; Luukkanen et al. 1997). These are markers for hUGT1A6, hUGT1A6/1A9, and hUGT1A9, respectively. Also, other human UGT1A forms can glucuronidate 1-OHP and entacapone (Luukkanen et al. 2005). BaP, 3-methylcholanthrene (MC), β-naphthoflavone (BNF) are typical inducers of Ah receptor (AhR) regulated gene expression (Bock et al. 1998; Nioi and Hayes 2004). α-Naphthoflavone (ANF) is a prototype flavonoid with inhibitory (CYP1A1) and stimulatory (CYP3A4) effects on BaP metabolism (Koley et al. 1997; Shou et al. 1994). l-Buthionine-[S,R]-sulfoximine (BSO) is an inhibitor of glutathione synthesis and a selective inducer of phase II enzymes (Manning and Franklin 1990). Ethoxyquin (EQ) is a phenolic antioxidant and monofunctional inducer of NQO1, GST, and UGT1A6 (Buetler et al. 1995; Nioi and Hayes 2004).
Polycyclic aromatic hydrocarbons in tobacco smoke induce CYP1A enzyme activities in human lung (Anttila et al. 2001; Kim et al. 2004a; Vainio et al. 1995), liver (Pelkonen et al. 1986), and placenta (Myllynen et al. 2005). A high degree of work-related exposure to PAHs probably also results in enzyme induction, particularly in employees who smoke. Occupational exposure measurements show that the uptake of PAHs known as potent inducers (BaP) is relatively very low (Gundel et al. 2000). Hence, the BaP dose alone may not evoke any marked enzyme induction in human lung. The question is do the more abundant but less hazardous 2–4-ring sized PAHs act as coinducers of enzymes that activate/detoxify procarcinogens in PAH mixtures.
Since susceptibility to or protection against chemical carcinogenesis is partially determined by differences in the biotransformation of procarcinogens, we used a rat model to evaluate the hepatic and pulmonary enzyme induction of carcinogen metabolizing phase I and II activities in animals treated with the PAH-mixture marker substances naphthalene, phenanthrene, pyrene, chrysene, and BaP (see Fig. 1). The inducibility by these 2–5-ring PAHs was compared with that by ANF, BNF, MC, EQ, and BSO. The sensitivity of our methods enabled us to quantify the enzyme activities CYP1A1, NQO1, mEH, and UGT in five human lungs and compare the human and animal data. The enzyme kinetics of 1-OHP glucuronidation (1-OHP UGT) could be determined in rat and human lung microsomes.
Materials and methods
Chemicals
Naphthalene (99%), phenanthrene (96–98%), pyrene (98%), chrysene (98%), BaP (> 97%), and MC (98%), 1-naphthol; 1-naphthyl β-d-glucuronide (sodium salt, 99% pure), ANF, BNF (95%), EQ (75%), 1,2-epoxy-3-(p-nitrophenoxy)propane (NP-oxide), 3-(p-nitrophenoxy)-1,2-propane diol (NP-diol), uridine 5′-diphosphate-glucuronic acid (UDPGA, triammonium salt), 7-ethoxyresorufin, and bovine serum albumin were purchased from Sigma-Aldrich (St Louis, MO, USA, or Steinheim, Germany). 1-OHP was from Acros Organics (Geel, Belgium). Entacapone [(E)-2-cyano-N,N-diethyl-3-(3,4-dihydroxy-5-nitrophenyl) propenamide; OR-611] was kindly provided by Orion Pharma (Espoo, Finland). 1-Pyrenyl β-d-glucuronide and entacapone 3-O-β-d-glucuronide were synthesized in the University of Helsinki (Luukkanen et al. 2001). The purity of the latter substances was ≥ 97.5%. Other reagents were of the highest grade available.
Animals and study design
Sixty female Wistar rats (298 ± 32 g, from the Helsinki University Breeding Centre) were housed in plastic cages bedded with aspen wood shavings in an air-conditioned room (23–25°C) with artificial lighting from 07:00 to 19:00 h. They had free access to the pellet chow (Rat Chow R3, Astra Ewos Ab, Södertälje, Sweden) and tap water. Four or eight rats per group were treated for 3 days with the doses shown for naphthalene (1.0 mmol/kg on day 1; 0.50 mmol/kg on day 2 and 3); phenanthrene, pyrene, chrysene (0.50 mmol/kg); BaP, MC (0.10 mmol/kg, ip); ANF, BNF (0.24 mmol/kg, ip); EQ (1.0 mmol/kg, ig); and with BSO (0.9 mmol/kg, ig) which was administered in tap water (100 mg/2.5 ml/kg body weight, twice a day, ig). All other agents were administered in olive oil (3 ml/kg). The first five substances were given both by oral gavage (day 1) and by ip administration (day 2 and 3). Inducer and vehicle-treated control animals were killed 24 h after the third dose. Food was withdrawn 3 h before each treatment and before sacrifice. Blood (6–8 ml) was drawn under CO2 anesthesia by cardiac puncture with heparin-rinsed plastic syringes and transferred in plastic tubes (in an ice bath). The livers were perfused in situ with phosphate buffered saline, removed, weighed, cooled in ice, and stored frozen (−70°C). The experiments were approved by the local Ethical Committee for Animal Studies (the guidelines of the European Convention for the Protection of Vertebrate Animals Used for Experimental and Other Scientific Purposes were followed).
Human lung specimens
Human lung samples were obtained from the University Hospital of Oulu. All donors (two females and three males, age 25–71 years) were non-cancerous lung surgery patients, current non-smokers diagnosed with emphysema, atelectasis (perhaps hereditary), or granulomatous lesions (post tuberculosis). Use of the lung tissue was approved by the Ethics Committee of the Medical Faculty of the University of Oulu, Finland. The samples were placed on ice after the surgical excision, cut into pieces, frozen in liquid nitrogen, and stored at −80°C until use. Microsome and cytosol fractions were prepared by differential ultracentrifugation and the protein determined as described (Nakajima et al. 1995), and then stored at −70°C until biochemical analyses.
Preparation of microsomes and cytosol
The thawed livers and lungs were homogenized in three volumes (w/v) of cold 0.15 M KCl–50 mM Na–K–phosphate buffer (pH 7.4) with a Potter–Elvehjem glass homogenizer (Thomas tubes with Teflon pestle). Enzyme fractions were prepared at 5°C by differential ultracentrifugation. The supernatant of the first centrifugation (10,000 g, 15 min) was run at 106,000 g for 60 min to obtain the cytosol fraction as a supernatant (stored at −70°C). The microsomal pellet was suspended in 3 or 6 ml (lung/liver) of buffer, and centrifuged (106,000 g, 60 min). The washed microsomal pellet was briefly homogenized (resuspended) in the freezing buffer containing 10% glycerol to give a protein content of 10–20 mg/ml, and divided in aliquots which were stored at −70°C until use. The protein concentrations were determined (Lowry et al. 1951) using commercial protein standards (Preciset® Eiweiss/Protein, Boehringer Mannheim, Mannheim, Germany).
Enzyme activity analyses
Alanine aminotransaminase (ALT) was determined in blood plasma (obtained by centrifugation 3,000 g for 20 min, at 20°C) using enzyme reagent kits from Medix Biochemica (Kauniainen, Finland). EROD activity was determined by a fluorometric method (Prough et al. 1978) in human lung microsomes (Anttila et al. 2001) and in rat lung and liver microsomes (Elovaara et al. 1991). mEH was determined by quantitative high-performance liquid chromatography (HPLC) methods as described previously (Nakajima et al. 1995). Briefly, the mEH activity toward 1.7 mM NP-oxide was determined by analysis of the product NP-diol (at 315 nm) or the activity toward 0.3 mM styrene oxide by analysis of the product styrene diol (at 215 nm) by an HPLC method (Giuliano et al. 1980). The NQO1 activity was measured kinetically at 30°C (Ernster 1967). Briefly, the dicoumarol (0.010 mM)-sensitive reduction of 2,6-dichlorophenolindophenol (0.04 mM DCPIP) was followed at 600 nm using NADPH (0.1 mM) as the reductant, cytosolic protein from rat liver or lung (2–20 μg), or human lung (200–320 μg), 40 mM Tris–HCl buffer, pH 7.5, and 0.08% Triton X-100 in a final volume 2.1 ml (or 1.2 ml). The reaction was started with NADPH after a 5-min preincubation at 30°C. The activity was calculated by the molar absorption coefficient 20.8 mM−1 cm−1 for DCPIP. The GST activity toward 1-chloro-2,4-dinitrobenzene (CDNB) was recorded kinetically at 25°C with a spectrophotometric method (Habig et al. 1974). Briefly, the reaction mixture (2.5 ml) contained 1.0 mM CDNB, 1.2 mM GSH, 0.02% Triton X-100 in 90 mM potassium phosphate buffer (pH 6.5), and cytosolic protein from rat liver (4–14 μg) or lung (17–60 μg).
Pyrene hydroxylation
The reaction mixture (final volume 250 μl) contained microsomal protein from rat liver (5–10 μg) or lung (70–200 μg) with 0.15 M KCl–50 mM Na–K–phosphate buffer (pH 7.4), and pyrene (94 μM, added in dimethylsulfoxide). The reaction was started (after a 6-min preincubation at 37°C) with 25 μl of 10 mM NADPH (1 mM), incubated for 10 min at 37°C and stopped with 50 μl of ice-cold 15% ZnSO4. After a 15 min protein precipitation (at 4°C), 1 ml acetonitrile was added to the tubes, mixed, and centrifuged (10,000 rpm, 10 min, 20°C). A 20 μl aliquot of the obtained supernatants was analyzed with a reversed phase C18 column (Waters Spherisorb S3 ODS2, 4.6 mm × 100 mm) and a Waters Spherisorb S5 ODS2 (4.6 mm × 30 mm) guard column in a Shimadzu HPLC/Class VP 5.021 chromatography system (Shimadzu, Kyoto, Japan) fitted with two LC-10AD pumps, an SCL-10AVP system controller, an SIL-10A autoinjector and an RF-10A fluorescence detector (λ ex = 242 nm, λ em = 388 nm). 1-OHP (RT = 2.8 min) and pyrene (RT = 6.8 min) were eluted with 75% acetonitrile in 0.5% aqueous acetic acid at a flow rate of 1.1 ml/min. 1-OHP was quantitated by peak area calculation with a 7-point (0–600 nM) linear calibration curve (r > 0.99). The enzyme reaction was linear with incubation time and protein concentration.
1-OHP glucuronidation
The reaction mixture contained 25 μl of rat liver microsomes (0.3–3 μg protein) in 0.5% bovine serum albumin; 115 μl of 50 mM K/Na–phosphate buffer–0.15 M KCl (pH 7.4) with 10 mM MgCl2; 100 μl of 50 mM K/Na–phosphate buffer–0.15 M KCl (pH 7.4) with 11 mM UDPGA (samples) or without UDPGA (controls). The reaction was started (after a 5–7 min preincubation at 37°C) with 10 μl of 150 or 7,500 μM 1-OHP in dimethylsulfoxide, incubated for 10 min, stopped with 50 μl of cold 15% ZnSO4 solution, cooled for 15 min in an ice bath (protein precipitation) before addition of 500 μl of acetonitrile. The tubes were vortex-mixed (10 s), sonicated (2 min), and centrifuged (10,000 g, 10 min, at 20°C). The supernatants were analyzed as described previously (Luukkanen et al. 2001) in a Shimadzu HPLC/Class VP 5.021 chromatography system (Shimadzu) using an RF-10Axl fluorescence detector (λ ex = 242 nm, λ em = 382 nm) and 60% acetonitrile in a 0.5% aqueous acetic acid for isocratic reverse-phase C18 runs. 1-Pyrenyl β-d-glucuronide was used for product identification (RT = 2.5 min) and quantitation by 6-point (0–56 nM) linear calibration curves (r ≥ 0.99) and peak area calculation. The enzyme reaction was linear with incubation time (≤ 30 min) and protein concentration (0.3–4 μg/250 μl).
Entacapone glucuronidation
The incubation mixture (final volume 250 μl, in Eppendorf tubes) contained 50 mM phosphate buffer (pH 7.4), 3 mM MgCl2, 250 μM entacapone (added in assay buffer), and 20–50 μg (rat liver) or 50–100 μg (rat lung) microsomal protein. The reaction was started with 50 μl of 25 mM UDPGA (5 mM), incubated for 15 min at 37°C, and stopped with 25 μl of cold 4 M perchloric acid. After protein precipitation (10 min in ice-bath) the tubes were mixed and centrifuged (14,000 rpm, 5 min). The supernatants (liver) were analyzed in a Shimadzu HPLC/Class VP 5.021 chromatography system (Shimadzu) equipped with a Nova-Pak C18 column (4 μm, 150 mm × 3.9 mm; Waters Co., Milford, MA, USA), SPD-10AV UV-VIS detector (at 305 nm) and an SIL-10A autoinjector. Acetonitrile—0.5% acetic acid in Millipore H2O (25:75, v/v) was used as the mobile phase for isocratic runs (flow rate 1 ml/min) and calibration was based on a 7-point (0.4–4.0 μM) concentration curve (R 2 > 0.99). The lung activities were analyzed with an Agilent 1100 series HPLC with the column switching technique as reported by Keski-Hynnilä et al. (2001). Briefly, 25 μl of the internal standard (600 ng/ml tolcapone glucuronide) was added to the lung samples. Two hundred and fifty microliters of the supernatant was neutralized with 10 μl of 4 M NaOH before analysis. Entacapone glucuronide was quantitated with a Sciex API300 triple quadrupole mass spectrometer (Sciex, Concord, Canada) equipped with an electrospray ion source. The loss of the glucuronic acid moiety was monitored in the negative ion mode. Calibration was based on a 7-point (38–379 ng/ml) concentration curve (R 2 > 0.99). Entacapone 3-O-β-d-glucuronide was used for the product identification and quantitation by peak area calculation. The enzyme reactions were linear with incubation time (< 60 min) and protein concentration (10–100 μg/250 μl).
1-Naphthol glucuronidation
This activity was determined at 37°C (10 min incubation) in a 250-μl reaction mixture, containing microsomal protein from rat lung (15–41 μg) or liver (38–91 μg), and a 250 or 500 μM 1-naphthol concentration, respectively. Otherwise the reaction conditions were as in the 1-OHP UGT assay. The supernatants of the lung (1:11, v/v) and liver (1:31, v/v) were diluted in 30% acetonitrile–0.5% aqueous acetic acid (eluent) for isocratic analysis (5 μl injection, flow rate 0.9 ml/min) with a reverse-phase C18 guard cartridge (Spherisorb S5 ODS2, 30 mm × 4.6 mm) and an analytical column S3 ODS2, 150 mm × 4.6 mm (Waters Spherisorb, Wexford, Ireland) using an RF-10Axl fluorescence detector (λ ex = 290 nm, λ em = 332 nm) and an SIL-10ADvp auto injector in a Shimadzu HPLC/Class VP 6.12 SP2 chromatography system. 1-Naphthol β-d-glucuronide was used for product identification (RT = 4.1 min) and quantitation by 6-point linear calibration curves (0.1–1.5 μM; r = 1.00) and peak area calculation. The enzyme reaction was linear with incubation time (≤ 20 min; protein 150 μg/250 μl) and protein concentration (lung, 13–80 μg/250 μl; liver, 37–300 μg/250 μl; 10 min incubation).
Enzyme kinetics
Apparent kinetic constants (K m and V max) were determined by fitting the initial glucuronidation velocities (V) and substrate (S) concentrations to the Michaelis–Menten equation by a non-linear least-squares method (Leonora v1.0, Cambridge University Press, UK). The Eadie–Hofstee plotting method (V versus V/S) was applied to explore the biphasic nature of 1-OHP UGT kinetics.
Statistical analyses
Rat liver and lung enzyme activity values were LN transformed to compute the coefficient of determination (R 2) by simple bivariate linear regression statistics (Table 2). Twelve of the 57 scatter plots are shown in Fig. 2 to illustrate some typical features observed in enzyme activity correlation behavior. Student’s t-test was used for statistical analysis of rat group results.
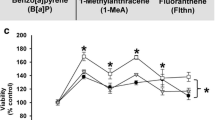
Relationships between PAH-metabolizing phase I and II enzymes activities, as shown for the two CYP1A marker activities, PH and EROD, and the glucuronidation activities toward N-UGT, 1-OHP UGT, and E-UGT in rat lung and liver (left and middle panels, respectively). Correlations between the hepatic and pulmonary enzyme activity are shown in the panels to the right
Results
Inducibility of PAH-metabolizing enzyme activities in rat liver and lung
The 3-day treatments with single PAHs and model enzyme inducers were well tolerated by the rats, only after the first naphthalene dose (1.0 mmol/kg) did the rats exhibit nausea, but not after the dose was halved on day 2 and 3. The liver weights were slightly increased by most treatments. There were no significant effects on the lung or kidney organ weights, or the plasma ALT levels (data not shown).
The effects of exposure to the PAHs naphthalene, phenanthrene, pyrene, chrysene, and BaP are compared in Table 1. The CYP1A1 marker activity of EROD and PH increased in rat liver up to 279- and 28-fold, the corresponding increases in rat lung being up to 56- and 22-fold, respectively. The glucuronidation rate of 1-naphthol (1N-UGT), 1-hydroxypyrene (1-OHP UGT), and entacapone (E-UGT) increased up to 6.4-fold in rat liver and up to 1.9-fold in rat lung. NQO1 and GST activities increased up to 5.3- and 1.6-fold (liver), and up to 4.4- and 1.4-fold (lung), respectively. Despite the multifold CYP1A induction, the tissue-specific activities of EROD and PH increased less than the UGT, NQO1, or GST activities. The hepatic and pulmonary induction profiles were similar. The inducing efficiency by naphthalene, phenanthrene, pyrene, chrysene, and BaP was dependent on the PAH molecular size and structure. NQO1 was the only activity inducible by all individual PAHs, i.e., also by naphthalene. Otherwise this 2-ring PAH proved ineffective, while the effects by BaP were comparable with those evoked by BNF, MC, BSO + MC, or EQ + MC.
The hepatic activities of EROD, PH, N-UGT, 1-OHP UGT, E-UGT in control rat microsomes were about 9, 11, 4, 19, and 6 times greater than the corresponding pulmonary activities (Table 1). The GST activity was eight times greater in the liver than in the lung. The hepatic and pulmonary levels of NQO1 were similar in 9 of 13 subgroups. Only the groups treated with MC, BSO + MC, EQ, or EQ + MC exhibited a 2–3-fold greater activity in the liver than in the lung. BaP treatment enhanced the hepatic glucuronidation of 1-naphthol, 1-OHP, and entacapone 4.8-, 2.1-, and 6.4-fold, respectively, but less than twofold the glucuronidation in the lung. Chrysene was also an inducer of these UGTs, while naphthalene, phenanthrene, and pyrene were ineffective.
Hepatopulmonary relationships between phase I and II enzyme activities
The phase I and II enzyme activities in rat lung and liver were all inducible (Table 1). Linear regression statistics revealed that the relationships between EROD, PH, N-UGT, 1-OHP UGT, E-UGT, and NQO1 activities in the liver (R 2 = 0.66–0.96) and the lung (R 2 = 0.46–0.90) were similar (Table 2). These activities correlated less well with the overall GST activity in rat liver (R 2 = 0.40–0.77) and lung (R 2 = 0.13–0.39, P ≤ 0.02). The R 2 value (0.13–0.96) describing a weak to strong relationship between the hepatic and pulmonary activities increased in the order: GST << UGT1A < NQO1 < CYP1A (PH, EROD). In Fig. 2, the plots for the CYP1A marker activities (60 rats) showed a strong linear relationship between PH and EROD both in the liver and the lung (R 2 = 0.90–0.96). Also for the UGT1A marker activities, a good linear relationship was shown both in the liver and the lung (R 2 = 0.75–0.96). A strong linear relationship was found even between the liver-to-lung levels of PH, denoting CYP1A activity (R 2 = 0.90). The R 2 values for the liver-to-lung levels of the tested UGT1A activities ranged from 0.36 to 0.62 (Fig. 2). AhR regulated tissue activities (CYP1A1, UGT1A, NQO1) correlated with each other better (R 2 = 0.46–0.96) than with the GST activity (R 2 = 0.13–0.72).
PAH-metabolizing enzyme activities in human lung of non-smokers
Pyrene hydroxylation was 63–153-fold slower, and that of 1-OHP glucuronidation 2–171-fold slower in human lung microsomes than the (mean) pulmonary rates in BaP-induced rats (Tables 1, 3). Activity of mEH both toward styrene oxide and NP-oxide was high in human lung microsomes. The mEH levels were 3–4 orders of magnitude greater than the pulmonary EROD and PH activities. The UGT activity was low in lung microsomes, except for one sample, which glucuronidated 1-OHP between 37 and 69 times faster than the other four samples. The NQO1 measurements showed that this cytosolic activity was both high and variable (64-fold variability) in human lungs.
Glucuronidation kinetics in rat and human lung
1-Hydroxypyrene glucuronidation kinetics were compared in human and rat lung microsomes. The initial velocities assayed over 1–300 μM 1-OHP concentrations indicated multiphasic enzyme kinetics (Fig. 3). The plots obtained by computing the velocities over 1–10 μM 1-OHP concentration range obeyed hyperbolic kinetics, giving the apparent constants for control and BaP rats: K m1 = 0.8 μM, V max1 = 0.40 nmol/min/mg; K m1 = 0.6 μM, V max1 = 0.58 nmol/min/mg, respectively (Fig. 3, mid panels). By using the Eadie–Hofstee plot method (Fig. 3, right-side panels), we could resolve two components both in control (K m1, K m2 = 0.8, 63 μM, V max1, V max2 = 0.39, 1.84 nmol/min/mg) and BaP-induced rat lungs (K m1, K m2 = 0.6, 55 μM, V max1, V max2 = 0.57, 2.51 nmol/min/mg). In human lung, the glucuronidation of 1-OHP seemed to be catalyzed by two low-K m forms (Fig. 3). The results on UGT kinetics are summarized in Table 4. Note that BaP was a modest inducer of 1-OHP glucuronidation in rat lung, and the intrinsic clearance values (V max/K m) of the K m1-form (500 and 984 μl/min/mg) were 6–12 times greater in rat lung microsomes than in human lung microsomes (83 μl/min/mg). The human K m2 enzyme (68 μl/min/mg) was a better catalyst than the rat form.
Enzyme kinetics of 1-OHP UGT in pooled rat lung microsomes of control and BaP-treated groups, and the enzyme kinetics in human lung microsomes from a non-smoking individual (K13) (bottom line panels). The apparent K m and V max values shown in the panels to the left and in the middle were calculated by the Michaelis–Menten equation. The panels on the right side show the K m and V max values obtained by the Eadie–Hofstee plot method
Discussion
Polycyclic aromatic hydrocarbon-metabolizing enzyme activities and their inducibility by individual ‘biomarker’ PAHs were investigated in the rat to predict effects inducible in human lung by exposure to environmental and industrial PAH mixtures.
In the rat, the efficacy of individual PAHs to enhance pulmonary PH and EROD activity ranged from no effect up to a 22- and 51-fold increase, the order range for the compounds being: naphthalene, phenanthrene < pyrene << chrysene < BaP. As an inducer, BaP proved to be as effective as BNF or MC. Our results and those by Shimada et al. (1992) indicate that the BNF induces EROD activity in rat liver (324-fold versus 678-fold) and lung (57-fold versus 5-fold).
NQO1 activity in the rat showed comparable liver-to-lung tissue levels. Induction by naphthalene, phenanthrene, and pyrene was modest both in rat lung (≤1.5-fold) and liver (≤1.8-fold) compared with a 4.4- to 5.3-fold increase seen after BaP, respectively. The combined treatment with a monofunctional (EQ) and a bifunctional (MC) inducer of NQO1 was anticipated to result in a maximum expression (Nioi and Hayes 2004). This was observed in the liver as a 20-fold increased activity. In the lung, the EQ + MC co-induced activity (7.0-fold) was near to the maximum induced by BNF alone (7.6-fold). The clearly lower inducibility of NQO1 in the lung than that occurring in the liver as noticed with MC may imply enzyme inactivation/target organ toxicity by this lung carcinogen. The order of inducer efficiency in the liver was naphthalene, phenanthrene, pyrene, BSO < ANF << chrysene, EQ < BaP, BNF, MC < BSO + MC < EQ + MC, and in the lung, phenanthrene, BSO < naphthalene, pyrene, EQ < ANF << chrysene, MC < BSO + MC < BaP < EQ + MC, BNF.
The glucuronidation of 1-naphthol (≤2.0-fold) and 1-OHP (≤2.7-fold) was inducible in rat lung as was the glucuronidation of the antiparkinsonian drug entacapone (≤2.1-fold), which is a hUGT1A9 substrate (Elovaara et al. 2004). The rank order of the individual PAH treatments to increase glucuronidation was: naphthalene, phenanthrene, pyrene << chrysene, MC < BaP < BNF. Glucuronidation of PAH phenols yields products excreted in urine and bile (Bock et al. 1998).
Glutathione S-transferase alpha, mu, and pi forms catalyze glutathione conjugation to CDNB (Hayes and Pulford 1995). This overall GST activity increased only up to 1.6 times in rat lung. In human lung, this GST activity was increased only by 20% in smokers compared with that in non-smokers (Nakajima et al. 1995). Despite numerous epidemiological lung cancer studies, the etiological role of functional/genetic polymorphism in pulmonary GSTs has remained elusive (Thier et al. 2003; Ye et al. 2006; Vineis 2004).
The hepatic activities of all the other rat enzymes except NQO1 were many times higher than the corresponding pulmonary activities. In control rat liver, the EROD, PH, N-UGT, 1-OHP UGT, E-UGT, and GST activities were 9, 11, 4, 19, 6, and 8 times greater, respectively, than the lung activity. In BaP-induced liver, these activities were 52, 14, 10, 20, 21, and 10 times greater, respectively, than the lung activity. The hepatic and pulmonary induction profiles by individual PAHs were similar, whereas the efficiency differed widely: control ≤ naphthalene < phenanthrene, pyrene << chrysene < BaP. A similar rank order was reported for the inducibility of phenanthrene metabolism in rat liver microsomes by single PAHs (Jacob et al. 1982). The response by BaP was in the same range as the induction levels found in BNF- or MC-treated rats. In conclusion, the inducing efficiency by naphthalene, phenanthrene, and pyrene is weak compared to the efficiency by the two well-known bay-region PAH carcinogens: chrysene and BaP.
Enzyme kinetics of 1-OHP UGT in rat lung microsomes suggested catalysis by at least two inducible forms in the low-K m range 0.6–63 μM. The apparent intrinsic clearance by these two components was 1.6–1.9 times lower in control rats than in the BaP-induced rats. Also, in human lung microsomes, 1-OHP was glucuronidated by two forms in the K m range 6–11 μM. We were able to evaluate the glucuronidation kinetics in one individual (K13) who had an exceptionally high pulmonary enzyme activity (552 pmol/min/mg). In the other four subjects, the UGT activity was too low (8–15 pmol/min/mg) to permit an evaluation of enzyme kinetics. Our results support the current understanding that the UGT1A6 and 1A9 are two low-K m enzymes with a constitutive and inducible expression in human liver and lung, catalyzing the glucuronidation and elimination of PAH phenols (Bock et al. 1998; Luukkanen et al. 2001).
The enzyme activities in human lung were many times lower than the average activities in control rats, this trend being observed for EROD (20–27-fold), PH (5–7-fold), 1-OHP UGT (6–380-fold), and NQO1 (17–1,126-fold). Human mEH activity was 7–9 times higher than the activity in control rat lung (1.27 ± 0.16 nmol/min/mg, n = 6, 0.35 mM NP-oxide; E. Elovaara, unpublished results). Since the lung samples came from non-smoking patients, the CYP1A1 marker activities were low. The EROD values were 80–100 times lower than the average lung activity in cigarette smokers (62 ± 52 pmol/min/mg, n = 33) (Anttila et al. 2001). Also, the PH activity was lower than that in most smokers (Elovaara et al. 1997; Vainio et al. 1995). No marked pulmonary induction of AhR-regulated enzymes could be inferred from the EROD and PH results.
Although humans are exposed to airborne PAH mixtures, the estimated pulmonary uptake of potent inducers such as BaP seems frequently to be too low to cause a maximum CYP1A1 induction in human lung (Gundel et al. 2000). CYP1A1 induction levels may thus critically depend on the total PAH uptake, which in turn may vary from one individual to another due to co-exposure of many PAH sources attributable to life style, medication, environment, or occupation (Bouchardt and Viau 1999). Such differences in the internal exposure may explain some of the large variations (200-fold) observed in EROD activity among lung cancer patients (Anttila et al. 2000). The constitutive expression of CYP1A1 is very low in human lung (Hukkanen et al. 2002; Kim et al. 2004a). It is therefore evident that CYP1A1 catalyzed bioactivation of PAH procarcinogens to DNA reactive products (Penning et al. 1999; Shimada and Fujii-Kuriyama 2004) depend on its inducible expression in human lung (Vineis 2004).
The activity of NQO1 in human lung was about 17–1,000 times lower than the basal levels in rat lung. The human activities varied by up to 64-fold in subjects whose PH and EROD levels were too low to indicate CYP1A1 induction. This large interindividual variation is probably explained by genetic polymorphisms. The associations between low-activity/low-inducibility NQO1 genotypes and human lung cancer risk have been reviewed by Ross and Siegel (2004). NQO1 is a PAH-inducible enzyme in human lung (Schlager and Powis 1990; Jaiswal 2000). It is induced even by naphthalene, which is transformed into reactive and redox active o-quinones, inducing NQO1 via electrophilic and oxidative stress (Ross and Siegel 2004). NQO1 protects against chemical toxicity and neoplasia by catalyzing two-electron reduction of highly reactive PAH quinones (Joseph and Jaiswal 1994; Penning et al. 1999). The anticarcinogenic properties of NQO1 are attributable to its role in antioxidant defense and stabilization of the tumor suppressor protein p53 (Asher et al. 2004).
The specific activity of mEH toward styrene oxide and NP-oxide was over 1,000 times greater than the corresponding PH and EROD activities in human lung. As shown previously (Nakajima et al. 1995), the mean pulmonary activity of mEH (NP-oxide) in smokers is about 5,000 times and, in non-smokers, about 80,000 times greater than the corresponding activity of BaP hydroxylation. Despite a 13-fold increase in BaP hydroxylation, no co-induction of mEH was detected in the smokers’ lungs. mEH catalyzes the formation of dihydrodiols which are either activated by oxygenation to diol epoxides (ultimate carcinogens) or converted to excretable products, usually, by glucuronidation or sulfation (Gelboin 1980; Conney 1982). The results of the many epidemiological studies into the associations between polymorphic mEH genotypes (low/high activity) and lung cancer risk are conflicting (Kiyohara et al. 2002). Interindividual differences in this highly expressed enzyme may have little impact on the PAH-metabolizing capacity of mEH in human lung.
In human lung, the glucuronidation rate could be probed only with 1-OHP. This is a sensitive substrate for detecting hUGT1A6/hUGT1A9-related activity (Luukkanen et al. 2001; Paakki et al. 2000). Several recombinant forms of human UGT1A family (1A1, 1A4, 1A6, 1A7, 1A8, 1A9, 1A10) are able to glucuronidate 1-OHP (Luukkanen et al. 2005). The UGT activity in human lung microsomes (0.008–0.552 nmol/min/mg) was 380 to 6 times lower than the activity in control rats (3.03 ± 0.33 nmol/min/mg). UGT levels in human lung varied widely, both in this (69-fold) and our previous studies (700-fold; 0.0003–0.216 nmol/min/mg) (Vainio et al. 1995). Evidence is emerging that UGT polymorphisms may play a role in the susceptibility to smoking-related cancer (Jinno et al. 2003; Wells et al. 2004).
In conclusion, the EROD, PH, NQO1, mEH, 1-OHP UGT measurements were limited to five lung samples from non-smoking non-cancer patients. Nevertheless, extensive interindividual differences could already be found among the human activities of UGT and NQO1, and these were relatively greater than the experimental (inducible/constitutive) variation in the rat. The activities attributable to pyrene oxidation (CYP1A1) and glucuronidation (UGT1A6/1A9) were very low in human lung when compared with that of mEH and NQO1. It appears that the CYP1A1 expression is dictated by the degree of enzyme induction while the large variability in expression of UGT1A and NQO1 is predominantly dictated by one’s genetic constitution. If the PAH-metabolizing activities could be tested in lung samples from individuals with high occupational PAH exposure (via lung and skin), and compared with our results, we might well find up to 100 times higher EROD and PH activities, higher and more variable NQO1 and UGT activities, and least changes in mEH activity. Since the 2–4-ring PAHs (major constituents in PAH mixtures) were poor enzyme inducers compared with BaP (minor constituent), it appears that enzyme induction in human lung is a response evoked mainly by exposure to carcinogenic BaP-type hydrocarbons. Gene–environmental interactions which magnify polymorphic variability in pulmonary bioactivation/detoxification capacity probably play a significant role in individual susceptibility to (or protection against) chemically induced lung cancer. Exposure to PAH mixtures with a high content of BaP-type hydrocarbons appears to confer a potentially higher health risk than PAH mixtures with a low content of procarcinogens.
Abbreviations
- ALT:
-
Alanine aminotransaminase
- ANF:
-
α-Naphthoflavone
- BNF:
-
β-Naphthoflavone
- BaP:
-
Benzo[a]pyrene
- BSO:
-
l-Buthionine-[S,R]-sulfoximine
- CDNB:
-
1-Chloro-2,4-dinitrobenzene
- CYP or P450:
-
Cytochrome P450
- DCPIP:
-
2,6-Dichlorophenolindophenol
- EQ:
-
Ethoxyquin
- EROD:
-
7-Ethoxyresorufin O-deethylase
- E-UGT:
-
Entacapone UGT
- GST:
-
Glutathione S-transferase
- HPLC:
-
High-performance liquid chromatography
- MC:
-
3-Methylcholanthrene
- mEH:
-
Microsomal epoxide hydrolase
- NQO1:
-
NADPH:quinone oxidoreductase 1 [NMO1, quinone reductase, DT-diaphorase]
- NP-oxide (EPNP):
-
1,2-Epoxy-3-(p-nitrophenoxy)propane
- NP-diol:
-
3-[p-Nitrophenoxy]-1,2-propane diol
- N-UGT:
-
1-Naphthol UGT
- 1-OHP:
-
1-Hydroxypyrene
- PH:
-
Pyrene 1-hydroxylase
- PAH:
-
Polycyclic aromatic hydrocarbon
- UDP:
-
Uridine diphosphate
- UDPGA:
-
UDP-glucuronic acid
- UGT:
-
UDP-glucuronosyltransferase
References
ACGIH (2005) Polycyclic aromatic hydrocarbons (PAHs): BEI®, 7th edn. Documentation ACGIH®. Publication #7DOC-735. American Conference of Governmental Industrial Hygienists, Cincinnati, 17 pp
Angerer J, Mannschreck C, Gundel J (1997) Biological monitoring and biochemical effect monitoring of exposure to polycyclic aromatic hydrocarbons (a review). Int Arch Occup Environ Health 70:365–377
Anttila S, Lei X-D, Elovaara E, Karjalainen A, Sun W, Vainio H, Hankinson O (2000) An uncommon phenotype of poor inducibility of CYP1A1 in human lung is not ascribable to polymorphisms in the AHR, ARNT, or CYP1A1 genes. Pharmacogenetics 10:741–751
Anttila S, Tuominen P, Hirvonen A, Nurminen M, Karjalainen A, Hankinson O, Elovaara E (2001) CYP1A1 levels in lung tissue of tobacco smokers and polymorphisms of CYP1A1 and aromatic hydrocarbon receptor. Pharmacogenetics 11:501–509
Asher G, Lotem J, Sachs L, Shaul Y (2004) p53-dependent apoptosis and NAD(P)H:quinone oxidoreductase 1. Meth Enzymol 382(part B):278–293
Bock KW, Gschaidmeier H, Heel H, Lehmkoster T, Munzel PA, Raschko F, Bock-Hennig B (1998) AH receptor-controlled transcriptional regulation and function of rat and human UDP-glucuronosyltransferase isoforms. Adv Enzyme Regul 38:207–222
Bouchard M, Viau C (1999) Urinary 1-hydroxypyrene as a biomarker of exposure to polycyclic aromatic hydrocarbons: biological monitoring strategies and methodology for determining biological exposure indices for various work environments. Biomarkers 4:159–187, and references therein
Buetler TM, Gallagher EP, Wang C, Stahl DL, Hayes JD, Eaton DL (1995) Induction of phase I and phase II drug-metabolizing enzyme mRNA, protein, and activity by BHA, ethoxyquin, and oltipraz. Toxicol Appl Pharmacol 135:45–57
Burchell B, Brierley CH, Monaghan CH, Clarke DJ (1998) The structure and function of the UDP-glucuronosyltransferase gene family. Adv Pharmacol 42:335–338
Conney AH (1982) Induction of microsomal enzymes by foreign chemicals and carcinogen by polycyclic aromatic hydrocarbons: GHA Clowes Memorial Lecture. Cancer Res 42:4875–4917
Elovaara E, Engström K, Nakajima T, Park SS, Gelboin HV, Vainio H (1991) Metabolism of inhaled styrene in acetone-, phenobarbital-, and 3-methylcholanthrene pretreated rats: stimulation and stereochemical effects by induction of cytochromes P450IIE1, P450IIB and P450IA. Xenobiotica 21:651–661
Elovaara E, Heikkilä P, Pyy L, Mutanen P, Riihimäki V (1995a) Significance of dermal and respiratory uptake in creosote workers: exposure to polycyclic aromatic hydrocarbons and urinary excretion of 1-hydroxypyrene. Occup Environ Med 52:196–203
Elovaara E, Raunio H, Pelkonen O, Vainio H (1995b) Oxidation of pyrene in human liver and lungs. Hum Exp Toxicol 14:821
Elovaara E, Karjalainen A, Vanhala E, Anttila S, Luukkanen L, Vainio H (1997) Effect of asbestos on PAH-metabolizing enzyme activities in lungs from smoking and non-smoking lung cancer surgery patients. In: ISSX proceedings (6th European ISSX Meeting), Göteborg, Sweden, vol. 11, p 64
Elovaara E, Mikkola J, Luukkanen L, Antonio L, Fournel-Gigleux S, Burchell B, Magdalou J, Taskinen J (2004) Assessment of catechol induction and glucuronidation in rat liver microsomes. Drug Metab Dispos 32:1426–1433
Ernster L (1967) DT diaphorase. Meth Enzymol 10:309–317
Gelboin HV (1980) Benzo(alpha)pyrene metabolism, activation and carcinogenesis: role and regulation of mixed-function oxidases and related enzymes. Physiol Rev 60:1107–1166
Giuliano KA, Lau EP, Fall RR (1980) Simplified liquid chromatographic assay for epoxide hydrolase. J Chromatogr 202:447–452
Grainger J, Huang W, Li Z, Selvin E, Walcott C, Smith C, Turner WE, Wang R, Patterson DG Jr (2004) PAH reference range levels in the U.S. population by measurement of urinary monohydroxy metabolites. Polycyclic Aromatic Comp 24:385–404
Grimmer G, Jacob J, Dettbarn G, Naujack KW (1997) Determination of urinary metabolites of polycyclic aromatic hydrocarbons (PAH) for the risk assessment of PAH-exposed workers. Int Arch Occup Environ Health 69:231–239
Guengerich FP (2000) Metabolism of chemical carcinogens. Carcinogenesis 21:345–351
Gundel J, Schaller KH, Angerer J (2000) Occupational exposure to polycyclic aromatic hydrocarbons in a fireproof stone producing plant: biological monitoring of 1-hydroxypyrene, 1-, 2-, 3- and 4-hydroxyphenanthrene, 3-hydroxybenz(a)anthracene and 3-hydroxybenzo(a)pyrene. Int Arch Occup Environ Health 73:270–274
Habig WH, Pabst MJ, Jacoby WB (1974) Glutathione S-transferases. The first step in mercapturic acid formation. J Biol Chem 249:7130–7139
Hayes JD, Pulford DJ (1995) The glutathione S-transferase supergene family. Regulation of GST and the contribution of the isozymes to cancer chemoprotection and drug resistance. Crit Rev Biochem Mol Biol 30:455–600
Hayes JD, Flanagan JU, Jowsey IR (2005) Glutathione transferases. Annu Rev Pharmacol Toxicol 45:51–88
Hecht SS (2002) Human urinary carcinogen metabolites: biomarkers for investigating tobacco and cancer. Carcinogenesis 23:907–922
Huang W, Grainger J, Patterson DG Jr, Turner WE, Caudill SP, Needham LL, Pirkle JL, Sampson EJ (2004) Comparison of 1-hydroxypyrene exposure in the US population with that in occupational exposure studies. Int Arch Occup Environ Health 77:491–498
Hukkanen J, Pelkonen O, Hakkola J, Raunio H (2002) Expression and regulation of xenobiotic-metabolizing enzymes cytochrome P450 (CYP) enzymes in human lung. Crit Rev Toxicol 32:391–411
IARC (1985) IARC monographs on the evaluation of the carcinogenic risk of chemicals to humans, vol. 35, Polynuclear aromatic compounds. Part 4, Bitumens, coal-tars and derived products, shale oils and soots. IARC, Lyon, France
Jacob J, Schmoldt A, Grimmer G (1982) Influence of monooxygenase inducers on the metabolic profile of phenanthrene in rat liver microsomes. Toxicology 25:333–343
Jaiswal AK (2000) Regulation of genes encoding NAD(P)H:quinone oxidoreductases. Free Radic Biol Med 29:254–262
Jinno H, Saeki M, Saito Y, Tanaka-Kagawa T, Hanioka N, Sai K, Kaniwa N, Ando M, Shirao K, Minami H, Ohtsu A, Yoshida T, Saijo N, Ozawa S, Sawada J (2003) Functional characterization of human UDP-glucuronosyltransferase 1A9 variant, D256N, found in Japanese cancer patients. J Pharmacol Exp Ther 306:688–693
Joseph P, Jaiswal AK (1994) NAD(P)H:quinone oxidoreductase1 (DT diaphorase) specifically prevents the formation of benzo[a]pyrene quinone-DNA adducts generated by cytochrome P4501A1 and P450 reductase. Proc Natl Acad Sci USA 91:8413–8417
Keski-Hynnilä H, Raanaa K, Forsberg M, Männistö P, Taskinen J, Kostiainen R (2001) Quantitation of entacapone glucuronide in rat plasma by on-line coupled restricted access media column and liquid chromatography–tandem mass spectrometry. J Chromatogr B Biomed Sci Appl 759:227–236
Kim JH, Sherman ME, Curriero FC, Guengerich FP, Strickland PT, Sutter TR (2004a) Expression of cytochromes P450 1A1 and 1B1 in human lung from smokers, non-smokers, and ex-smokers. Toxicol Appl Pharmacol 199:210–219
Kim YD, Todoroki H, Oyama T, Isse T, Matsumoto A, Yamaguchi T, Kim H, Uchiyama I, Kawamoto T (2004b) Identification of cytochrome P450 isoforms involved in 1-hydroxylation of pyrene. Environ Res 94:262–266
Kiyohara C, Otsu A, Shirakawa T, Fukuda S, Hopkin JM (2002) Genetic polymorphisms and lung cancer susceptibility: a review. Lung Cancer 37:241–256
Koley AP, Buters JTM, Robinson RC, Markowitz A, Friedman FK (1997) Differential mechanisms of cytochrome P450 inhibition and activation by alpha-naphthoflavone. J Biol Chem 272:3149–3152
Lowry O, Rosebrough N, Farr L, Randall R (1951) Protein measurement with the Folin phenol reagent. J Biol Chem 193:265–275
Luukkanen L, Elovaara E, Lautala P, Taskinen J, Vainio H (1997) Characterization of 1-hydroxypyrene as a novel marker substrate of 3-methylcholanthrene-inducible phenol UDP-glucuronosyltransferase(s). Pharmacol Toxicol 80:152–158
Luukkanen L, Mikkola J, Forsman T, Taavitsainen P, Taskinen J, Elovaara E (2001) Glucuronidation of 1-hydroxypyrene by human liver microsomes and human UDP-glucuronosyltransferases UGT1A6, UGT1A7, and UGT1A9: development of a high-sensitivity glucuronidation assay for human tissue. Drug Metab Dispos 29:1096–1101
Luukkanen L, Taskinen J, Kurkela M, Kostiainen R, Hirvonen J, Finel M (2005) Kinetic characterization of the 1A subfamily of recombinant human UDP-glucuronosyltransferases. Drug Metab Dispos 33:1017–1026
Manning BW, Franklin MR (1990) Induction of rat UDP-glucuronosyltransferase and glutathione S-transferase activities by l-buthionine-S,R-sulfoximine without induction of cytochrome P-450. Toxicology 65:149–159
Myllynen P, Pasanen M, Pelkonen O (2005) Human placenta: a human organ for developmental toxicology research and biomonitoring. Placenta 26:361–371 (review)
Nakajima T, Elovaara E, Anttila S, Hirvonen A, Camus A-M, Hayes JD, Ketterer B, Vainio H (1995) Expression and polymorphism of glutathione S-transferases in human lungs: risk factors in smoking-related lung cancer. Carcinogenesis 16:707–711
Nebert DW, Dalton TP, Okey AB, Gonzalez FJ (2004) Role of aryl hydrocarbon receptor-mediated induction of the CYP1 enzymes in environmental toxicity and cancer. J Biol Chem 23:23847–23850
Nioi P, Hayes JD (2004) Contribution of NAD(P)H:quinone oxidoreductase 1 to protection against carcinogenesis, and regulation of its gene by Nrf2 basic-region zipper and the arylhydrocarbon receptor basic helix-loop-helix transcription factors. Mutat Res 555:149–171
Paakki P, Stockmann H, Kantola M, Wagner P, Lauper U, Huch R, Elovaara E, Kirkinen P, Pasanen M (2000) Maternal drug abuse and human placental term xenobiotic and steroid metabolizing enzymes in vitro. Environ Health Perspect 108:141–145
Pelkonen O, Nebert D (1982) Metabolism of polycyclic aromatic hydrocarbons: etiologic role in carcinogenesis. Pharmacol Rev 34:189–221
Pelkonen O, Pasanen M, Kuha H, Gachalyi B, Kairaluoma M, Sotaniemi EA, Park SS, Friedman FK, Gelboin HV (1986) The effect of cigarette smoking on 7-ethoxycoumarin O-deethylase and other monooxygenase activities in human liver: analyses with monoclonal antibodies. Br J Clin Pharmacol 22:125–134
Pelkonen O, Raunio H, Rautio A, Lang M (1999) Xenobiotic-metabolizing enzymes and cancer risk: correspondence between genotype and phenotype. IARC Sci Publ 148:77–88 (review)
Penning TM, Burczynski ME, Hung CF, McCoull KD, Palackal NT, Tsuruda LS (1999) Dihydrodiol dehydrogenases and polycyclic aromatic hydrocarbon activation: generation of reactive and redox active o-quinones. Chem Res Toxicol 12:1–18 (review)
Prough RA, Burke MD, Mayer RT (1978) Direct fluorometric methods for measuring mixed-function oxidase activity. Meth Enzymol 52(part C):373–377
Ross D, Siegel D (2004) NAD(P)H:quinone oxidoreductase 1 (NQO1, DT-diaphorase) functions and pharmacogenetics. Meth Enzymol 382(part B):115–144
Schlager JJ, Powis G (1990) Cytosolic NAD(P)H:(quinone-acceptor)oxidoreductase in human normal and tumor tissue: effects of cigarette smoking and alcohol. Int J Cancer 45:403–409
Shimada T, Fujii-Kuriyama Y (2004) Metabolic activation of polycyclic aromatic hydrocarbons to carcinogens by cytochrome P450 1A1 and 1B1. Cancer Sci 95:1–6
Shimada T, Yun CH, Yamazaki H, Gautier JC, Beaune PH, Guengerich FP (1992) Characterization of human lung microsomal cytochrome P-450 1A1 and its role in the oxidation of chemical carcinogens. Mol Pharmacol 41:856–864
Shou M, Grogan J, Mancewicz JA, Krausz KW, Gonzalez FJ, Gelboin HV, Korzekwa KR (1994) Activation of CYP3A4: evidence for the simultaneous binding of two substrates in a cytochrome P450 active site. Biochemistry 33:6450–6455
Thier R, Bruning T, Roos PH, Rihs H-P, Golka K, Ko Y, Bolt HM (2003) Markers of genetic susceptibility in human environmental hygiene and toxicology: the role of selected CYP, NAT and GST genes. Int J Hyg Environ Health 206:149–171
UBA (1998) Umweltbundesamt: Umwelt-Survey, Berlin 1998. http://www.umweltbundesamt.de/survey/us98/pak.htm
Vainio H, Elovaara E, Luukkanen L, Anttila S, Ulmanen I, Fournel-Gigleux S, Ouzzine M, Pillot T, Magdalou M (1995) Expression and co-induction of CYP1A1 and UGT1*6 in human lungs. Eur J Drug Metab Pharmacokinet 20:47–48
Vineis P (2004) Individual susceptibility to carcinogens. Oncogene 23:6477–6483
Wells PG, Mackenzie PI, Chowdhury JR, Guillemette C, Gregory PA, Ishii Y, Hansen AJ, Kessler FK, Kim PM, Chowdhury NR, Ritter JK (2004) Glucuronidation and the UDP-glucuronosyltransferases in health and disease. Drug Metab Dispos 32:281–290 (review)
Yang M, Koga M, Katoh T, Kawamoto T (1999) A study for the proper application of urinary naphthols, new biomarkers for airborne polycyclic aromatic hydrocarbons. Arch Environ Contam Toxicol 36:99–108
Ye Z, Song H, Higgins JP, Pharoah P, Danesh J (2006) Five glutathione S-transferase gene variants in 23,452 cases of lung cancer and 30,397 controls: meta-analysis of 130 studies. PLoS Med 3(4):e91 [Epub 2006 March 7]
Zheng Z, Fang JL, Lazarus P (2002) Glucuronidation: an important mechanism for detoxification of benzo[a]pyrene in aerodigestive tract tissues. Drug Metab Dispos 30:397–403
Acknowledgments
We wish to thank Ms. Maria Pihlaja and Ms. Ulla Peltonen for skillful technical assistance. UGT studies were associated with the BMH4-CT97-2621 project supported by the Commission of the European Communities.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Elovaara, E., Mikkola, J., Stockmann-Juvala, H. et al. Polycyclic aromatic hydrocarbon (PAH) metabolizing enzyme activities in human lung, and their inducibility by exposure to naphthalene, phenanthrene, pyrene, chrysene, and benzo(a)pyrene as shown in the rat lung and liver. Arch Toxicol 81, 169–182 (2007). https://doi.org/10.1007/s00204-006-0135-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00204-006-0135-8