Abstract
This study was designed to evaluate the combined effect of probiotic Lactobacillus rhamnosus and bacteriophage SA11 on the control of antibiotic-sensitive Staphylococcus aureus (ASSA) and antibiotic-resistant S. aureus (ARSA) under the simulated intestinal conditions. The survivability of ASSA and ARSA were determined in the simulated phosphate-buffered saline (PBS)-, trypticase soy broth (TSB)-, and milk-based gastric juices adjusted to pH 2.0, 3.0, and 5.0 at 37 °C for 30 min. The inhibitory effect of bacteriophage SA11 and probiotic on the growth of ASSA and ARSA was evaluated in the simulated intestinal juices at 37 °C for 20 h. The least reductions in the numbers of ASSA and ARSA were observed in the milk-based gastric juices at pH 2.0 (<1 log). No significant changes in the teichoic acid-mediated sliding motility were observed for ASSA and ARSA after 30-min exposure to the simulated gastric juices (pH 2.0, 3.0, and 5.0), responsible for the enhanced bacterial attachment to the epithelial cells. The bacteriophage SA11 was stable down to pH 5.0 and up to 0.06 % bile salts. The bacteriophage SA11 combined with probiotic effectively inhibited the growth of ASSA and ARSA in the simulated intestinal conditions, showing more than 4 log reduction. The relative expression levels of adhesion-related genes (clfA, eno, and fnbA) and efflux-related genes (mdeA, norB, and norC) were less decreased in ARSA than in ASSA after exposure to the simulated gastrointestinal conditions. These results might shed light on the application of bacteriophage to control the ingested antibiotic-resistant foodborne pathogens in the intestinal tract.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the last decade, the overuse and misuse of antibiotics have mainly resulted in the rapid increase in antibiotic-resistant bacteria, which can eventually lead to serious health problems. Long-term antibiotic use can cause an imbalance of indigenous intestinal microflora and furthermore result in a selective pressure towards stress-resistant bacteria, known as cross-resistance (Mathur and Singh 2005; Hammad and Shimamoto 2010). Ingested antibiotic-resistant pathogenic bacteria encounter mechanical, chemical, and biological barriers, including acidic pH, proteolytic enzymes, detergents, peristaltic action, and indigenous enteric microflora, during the gastrointestinal transit (Bourlioux et al. 2003). In order to pass through the stomach and reach the large intestine alive, however, bacteria have evolved several survival strategies such as acid tolerance response (ATR) system and bile resistance mechanism (Gunn 2000; Foster 2001). In addition, food matrices can cause change in gastric acidity and provide protective effect to ingested bacterial pathogens (Barmpalia-Davis et al. 2008; Koseki et al. 2011). The inhibitory effect of gastrointestinal fluids can thus be overestimated, while the viability of ingested antibiotic-resistant bacterial pathogens can possibly be underestimated in the gastrointestinal tract (GIT) (Smith 2003). Therefore, it is necessary to evaluate the fate of bacterial pathogens exposed to the GI conditions and develop novel preventive and therapeutic approaches as antibiotic alternatives.
Probiotics, “the live feed supplements which beneficially affect the host animal by improving its intestinal microbial balance”, have been well known as holistic approach in the GIT to provide health benefits, including the modulation of intestinal microflora, the competitive exclusion of pathogens, and stimulation of immune system (Fuller 1989; Servin and Coconnier 2003; Collado et al. 2007; Woo and Ahn 2013). Recently, bacteriophages control has received much research attention to preventing and treating infectious diseases due to their specificity to bacterial hosts, effectiveness against antibiotic-resistant bacteria, and no adverse side effects (Matsuzaki et al. 2005; Atterbury et al. 2007; Bardina et al. 2012). Since the inhibitory mechanisms of bacteriophages against the host bacteria are different from the modes of action of antibiotics, the use of bacteriophages has the potential for controlling antibiotic-resistant pathogens (Matsuzaki et al. 2005). However, little is known about the combined effect of probiotic and bacteriophage on the inhibition of antibiotic-resistant bacterial pathogens exposed to the simulated intestinal conditions. Staphylococcus aureus, an opportunistic pathogen, is a frequent cause of nosocomial infections. Many studies have been reported that S. aureus can colonize the intestinal tract through hospitalized patients (Vesterlund et al. 2006; Bhalla et al. 2007). The production of staphylococcal enterotoxins (SEs) and toxic shock syndrome toxin 1 (TSST-1) plays an important role in the pathogenesis of S. aureus infections, leading to foodborne disease outbreaks and intestinal colonization (Bhalla et al. 2007; Pereira et al. 2009). Therefore, the objectives of this study were to evaluate the survival of antibiotic-resistant S. aureus (ARSA) in the different medium-based solutions adjusted to pH 2.0, 3.0, and 5.0 during the simulated gastric transit and also assess the possibility of using probiotic combined with bacteriophage as an antibiotic alternative as evaluated by the susceptibility of ARSA to the simulated intestinal conditions.
Materials and methods
Bacterial strains and culture conditions
Strains of Staphylococcus aureus ATCC 13301 and S. aureus CCARM 3080 obtained from American Type Culture Collection (ATCC, Manassas, VA, USA) and Culture Collection of Antibiotic Resistant Microbes (CCARM, Seoul, Korea), respectively, were cultured in trypticase soy broth (TSB) (BD, Becton, Dickinson and Co., Sparks, MD, USA) at 37 °C for 24 h. According to the predetermined antibiotic susceptibilities (data not shown), S. aureus ATCC 13301 and S. aureus CCARM 3080 were assigned to ASSA and ARSA, respectively. Strain of Lactobacillus rhamnosus GG was kindly provided by Dr. Azlin Mustapha of the Department of Food Science at the University of Missouri (Columbia, MO, USA). Probiotic strain was grown anaerobically in de Man Rogosa Sharpe broth (MRS; Difco, BD) supplemented with 0.05 % l-cysteine hydrochloride at 37 °C for 24 h. All strains were harvested by centrifugation at 5,000×g for 10 min at 4 °C. The harvested cells were washed twice with sterile 0.1 % peptone water.
Bacteriophage propagation
Staphylococcus bacteriophage SA11 purchased from the Bacteriophage Bank at Hankuk University of Foreign Studies (Yongin, Gyeonggi, Korea) belongs to the Siphoviridae family, containing a linear, double-stranded DNA genome (Kim and Myung 2012). The bacteriophage SA11 was propagated at 37 °C for 24 h in TSB containing S. aureus ATCC 13301 as an appropriate host strain. After the bacteriophage propagation, the supernatant obtained by centrifugation at 5,000 × g for 10 min was filtered through a 0.2-μm filter to eliminate residual bacterial lysates. The titre of bacteriophage SA11 was determined by using soft agar overlay method. The filtrate was serially (1:10) diluted with phosphate-buffered saline (PBS; pH 7.4). Each decimal dilution (100 μl) was gently mixed with the host cells (108 CFU/ml) in 0.5 % TSB soft agar and then immediately poured onto the prewarmed base agar. The plates were incubated at 37 °C for 24 h to quantify the bacteriophage expressed as plaque-forming unit (PFU).
Simulated gastric transit assay
The simulated gastric juice was prepared by dissolving 0.3 % pepsin in basal PBS, TSB, or milk and adjusted to pH 2.0, 3.0, and 5.0 by using 6 N hydrochloric acid (HCl). Approximately 107 CFU/ml of S. aureus cells were inoculated in different media (PBS, TSB, or milk) of varying pH levels and then incubated anaerobically for 30 min at 37 °C in a GasPak anaerobic system (BBL, Cockeysville, MD, USA) with Anaerogen (Oxoid, ltd, Hampshire, UK).
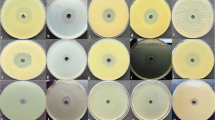
Bacterial sliding motility assay
The bacterial sliding motility was measured according to the sliding motility assay (Kaito and Sekimizu 2007). S. aureus cells exposed to the PBS- or TSB-based gastric juices at 37 °C for 30 min were centrifuged at 3,000×g for 20 min, rinsed with PBS, and adjusted to 1 × 108 CFU/ml. Each culture (2 μl) was stabbed into the centre of soft agar plates (0.24 % agar). The plates were incubated at 37 °C for 24 h. The diameters of circle zone on the plates were measured using a metric ruler. The sliding motility for each treatment was expressed as per cent compared to the control.
Acid and bile susceptibility assay
The susceptibility of bacteriophage SA11 to acid and bile salts was evaluated in TSB adjusted to pH 2.0, 3.0, 4.0, 5.0, 6.0, 7.0, and 8.0 with 6 N HCl and serially diluted (1:2) at concentration of 0.45 % bile salts. Approximately 107 PFU/ml of bacteriophage SA11 was inoculated in the prepared TSB at different levels of pHs and bile salts and then incubated at 37 °C for 20 h anaerobically. The numbers of bacteriophage SA11 were enumerated to evaluate the acid and bile susceptibilities.
Simulated intestinal transit assay
For the intestinal transit assay, the simulated intestinal juice was prepared by suspending 0.03 % bile salt in TSB adjusted to pH 8.0 with 6 N NaOH (TSB-8). Approximately 107 CFU/ml of S. aureus cells were inoculated anaerobically in the simulated intestinal juice with L. rhamnosus and/or bacteriophage SA11 and incubated at 37 °C for 20 h. Treatments included TSB-8, L. rhamnosus (LR), bacteriophage SA11 (SA11), and L. rhamnosus and SA11 (LR+SA11).
RNA extraction and cDNA synthesis
RNA was extracted according to the protocol of RNeasy Protect Bacteria Mini kit (Qiagen, Hilden, Germany). The cells (0.5 ml) exposed to the simulated gastric (TSB-3) and intestinal (TSB-8, LR, SA11, LR+SA11) juices were mixed with 1 ml of RNA protect Bacteria Reagent and centrifuged at 5,000×g for 10 min. The harvested cells were lysed with a buffer containing lysozyme. The lysates were mixed with ethanol to extract RNA using an RNeasy mini column. The genomic DNA was removed by a Wipe buffer. The cDNA synthesis was carried out according to the QuantiTech reverse transcription procedure (Qiagen). The RNA extracts were mixed with a master mixture of reverse transcriptase, RT buffer, and RT primer mix and then incubated at 42 °C for 15 min followed by 95 °C for 3 min to inactivate the reverse transcriptase. The cDNA synthesized was used as a template for quantitative RT-PCR assay.
Quantitative RT-PCR assay
The reaction mixture (20 μl) containing 10 μl of 2 × QuantiTect SYBR Green PCR Master, 2 μl of each primer, 2 μl of cDNA, and 4 μl of RNase-free water was amplified using an iCycler iQ™ system (Bio-Rad Laboratories, Hemel Hempstead, UK). The oligonucleotides (Erofins MWG Operon; Huntsville, AL, USA) used as primers of S. aureus are listed in Table 1. The PCR mixture was denatured at 95 °C for 30 s, followed by 45 cycles of 95 °C for 5 s, 55 °C for 20 s, and 72 °C for 15 s. The relative gene expression levels were estimated using the comparative method (Livak and Schmittgen 2001). The C T values of target genes in S. aureus cells exposed to the simulated gastric and intestinal juices were compared to the C T values obtained from the untreated cells (control). The 16S ribosomal RNA as the reference gene was used for target gene normalization.
Statistical analysis
All analyses were carried out in duplicate on three replicates. Data were analysed using the Statistical Analysis System software. The general linear model and least significant difference (LSD) procedures were used to compare means. Significant mean differences were estimated by Fisher’s LSD at P < 0.05.
Results and discussion
This study describes the inhibitory effect of probiotic combined with bacteriophage SA11 against ASSA and ARSA in the simulated intestinal condition. Relatively few studies have been conducted to assess the bacteriophage effect against ingested foodborne pathogens. Thus, this study is a new approach to investigate the potential of using bacteriophage in combination with probiotic function for controlling ingested antibiotic-resistant foodborne pathogens in the GIT.
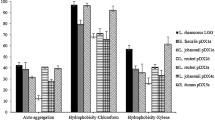
Survival of S. aureus in the simulated gastric juices at various pHs
The acid tolerance of ASSA and ARSA was evaluated in the simulated PBS-, TSB-, and milk-based gastric juices adapted at pH 2.0, 3.0, and 5.0 (Fig. 1). The viabilities of ASSA and ARSA were not affected by pH 3.0 and 5.0, while those were significantly decreased depending on the composition of basic media and the physiological state of strains at pH 2.0. ASSA was more susceptible to pH 2.0 than ARSA in the simulated PBS- and TSB-based gastric juices. The numbers of ASSA were reduced by 2.8 and 6.0 log, respectively, in PBS- and TSB-based gastric juices. This suggests that antibiotic-resistant bacteria can induce adaptation to subsequent stress, known as cross-protection that describes the phenomenon in which mono-stress-adapted bacteria can easily acquire resistance to additional stresses (Greenacre et al. 2006; Xu et al. 2008). No significant difference was observed between the numbers of ASSA and ARSA in milk-based gastric juices adapted at pH 2.0, showing <1 log reduction. This result implies that food matrices can provide protective effect against acid stress under the gastric condition for ingested pathogenic bacteria, resulting in an increase in bacterial survivability (Zhu et al. 2006; Ceuppens et al. 2012). This protective effect is mainly due to the binding ability and buffering capacity of food components (Zhu et al. 2006; Barmpalia-Davis et al. 2008). Therefore, the surviving bacteria after gastric transit within food matrices can be released into the duodenum (pH 8) with high numbers, which undergo continuous multiplication and infectious process. The sliding abilities of ASSA and ARSA exposed to the simulated PBS- and TSB-based gastric juices at pH 3.0 (PBS-3 and TSB-3) and pH 5.0 (PBS-3 and TSB-3) were evaluated based on the colony-spreading force of growing cells (Fig. 2). Compared to the untreated control, the colony-spreading abilities of ASSA and ARSA were not significantly changed after exposure to PBS-3, TSB-3, PBS-3, and TSB-3, ranging 93–111 %. Teichoic acid-mediated sliding motility is mainly involved in the attachment of Gram-positive bacteria (Kaito and Sekimizu 2007). The observations suggest that ASSA and ARSA can enhance the abilities to attach to human epithelial cells, which plays an important role in pathogenesis (Kaito and Sekimizu 2007).
Reduction (log N 30/N 0) of antibiotic-sensitive S. aureus (ASSA; grey square) and antibiotic-resistant S. aureus (ARSA; filled square) exposed to the PBS-, TSB-, and milk-based gastric juices adjusted to pH 2 (a), pH 3 (b), and pH 5 (c) at 37 °C for 30 min. Bars with different uppercase letters (a–c) and lowercase letters (a–b) are significantly different within ASSA (grey square) and ARSA (filled square), respectively, at P < 0.05. N 0 and N 30 represent the inoculum level (7.12 log CFU/ml) and the bacterial count after incubation of 30 min, respectively. Asterisk (*) indicates the significant difference between ASSA (grey square) and ARSA (filled square)
Sliding motility (%) of antibiotic-sensitive S. aureus (ASSA; white doted bar) and antibiotic-resistant S. aureus (ARSA; dark doted bar) exposed to the PBS- and TSB-based gastric juices adjusted to pH 3 (PBS-3 and TSB-3) and pH 5 (PBS-5 and TSB-5) at 37 °C for 30 min. The untreated S. aureus was normalized to 100 %
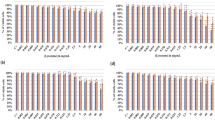
Effect of pH and bile salts on the stability of bacteriophage SA11
The pH and bile salt susceptibilities of bacteriophage SA11 were evaluated as shown in Fig. 3. The viability of bacteriophage SA11 was significantly affected at pH below 4.0, showing the bacteriophage counts below the limit of detection (<1 log PFU/ml) (Fig. 3a). This is in good agreement with previous reports that bacteriophages are stable at a pH range of 5–8 (Chow and Rouf 1983). The stability of bacteriophage SA11 was decreased at pH 5.0 with increasing incubation time. The bacteriophage counts were 6.8, 6.5, and 5.6 log PFU/ml after 2, 10, and 20 h of incubation at pH 5.0. The numbers of bacteriophage remained high above pH 7.0 regardless of incubation time. The susceptibility of bacteriophage SA11 to bile salts was slightly decreased with increasing the concentration (Fig. 3b). No significant changes in the bacteriophage counts were observed until 0.06 % bile salts. The results imply that the bacteriophage SA11 is applicable for controlling S. aureus in the intestinal tract.
Viability of S. aureus in the simulated intestinal juices treated with probiotic and bacteriophage
The inhibitory effect of probiotic combined with bacteriophage SA11 on the growth of ASSA and ARSA was evaluated in the simulated intestinal juices (Fig. 4). The growth of ASSA and ARSA in the simulated intestinal condition was significantly inhibited by L. rhamnosus (LR), bacteriophage (SA11), and combination (LR + SA11) compared to the control. The number of ASSA was significantly decreased to 3.5 log CFU/ml in the intestinal juice treated with bacteriophage SA11 when compared to ARSA (7.0 log CFU/ml) after 10 h of incubation (Fig. 4a). This might be due to the altered specific carbohydrate receptors on the surface of ARSA, leading to the decrease in bacteriophage adsorption (Muller-Merbacha et al. 2007; Bleackley et al. 2009). The inhibitory effect of LR, SA11, and LR plus SA11 was more noticeable against ASSA than ARSA after 20 h of incubation (Fig. 4b). This suggests that ARSA might induce cross-protective phenomenon in the simulated intestinal conditions (Greenacre et al. 2006). Bacteriophage SA11 effectively inhibited the growth of ASSA and ARSA after 10 h of incubation, while L. rhamnosus was effective against ASSA and ARSA after 20 h of incubation. This suggests that the lytic activity of bacteriophage SA11 was predominant at 10 h of incubation, while the probiotic activity was increased at 20 h. The growth of probiotics produces metabolites such as organic acids, hydrogen peroxide, and bacteriocins, which are responsible for anti-pathogenic activity in the intestinal tract (Oelschlaeger 2010). The highest reductions in the numbers of ASSA and ARSA were observed at the combined treatment (LR+SA11), showing more than 4 log reductions at 10 and 20 h of incubation. Unlike ASSA, these results were not enough to clearly explain the combined effect of bacteriophage SA11 and L. rhamnosus against ARSA. Although further studies are required to elucidate the possible mechanisms of the combined effect of bacteriophage SA11 and L. rhamnosus in the simulated intestinal tract, this can be assumed that the reversible receptors and/or charge on the surface of ARSA was possibly altered by probiotic metabolites in the simulated intestinal conditions, resulting in an enhanced affinity between bacteriophages and host cells.
Survival of antibiotic-sensitive S. aureus (ASSA; white doted bar) and antibiotic-resistant S. aureus (ARSA; dark doted bar) exposed to the simulated intestinal juices treated with Lactobacillus rhamnosus (LR; 7.32 log CFU/ml), bacteriophage (SA11; 7.07 log PFU/ml), and L. rhamnosus combined with bacteriophage (LR+SA11) at 37 °C for 10 h (a) and 20 h (b). The dotted line indicates the inoculum level of S. aureus (7.45 log CFU/ml). Bars with different uppercase letters (a–c) and lowercase letters (a–d) are significantly different within ASSA (white doted bar) and ARSA (dark doted bar), respectively, at P < 0.05
Gene expression patterns of ASSA and ARSA exposed to under simulated gastrointestinal conditions
The relative expression of adhesion-related genes (clfA, eno, and fnbA) and efflux-related genes (mdeA, norB, and norC) was observed in ASSA and ARSA exposed to the simulated gastric juice containing 0.3 % pepsin in TSB of pH 3.0 (TSB-3) for 30 min and the simulated intestinal juices containing 0.03 % bile salt in TSB of pH 8.0 (TSB-8) with L. rhamnosus (LR), bacteriophage SA11 (SA11), and L. rhamnosus and SA11 (LR+SA11) for 20 h (Fig. 5). Most genes were down-regulated in all treatments, while the genes, clfA, fnbA, and norC, were up-regulated in both ASSA and ARSA exposed to LR. The relative expression levels of clfA gene were increased to 1.8-fold in ASSA and 1.2-fold in ARSA when exposed to LA (Fig 5a). The eno and fnbA genes were up-regulated 1.5-fold and more than threefold in ARSA, respectively, after 20-h exposure to TSB-8 (Fig. 5b, c). The genes, clfA, eno, and fnbA, encode clumping factor, laminin-binding protein, and fibrinogen-binding protein, respectively, leading to increased staphylococcal virulence and resistance to host phagocytosis (O’Connell et al. 1998; Lei et al. 2011). The overexpression of clfA, eno, and fnbA is highly associated with the ability of S. aureus to form biofilm cells, adhere to epithelial cells, and evade the host immune system (Vancraeynest et al. 2004; Nemati et al. 2009; Stutz et al. 2011). The highest expression levels of mdeA, norB, and norC were observed in ARSA, showing 2.2-fold at LR, 0.3-fold at TSB-8, and 3.5-fold at LR, respectively (Fig. 5d, e, f). The expression of efflux-related genes (mdeA, norB, and norC) plays an important role in increasing antibiotic resistance of S. aureus (Huang et al. 2004; DeMarco et al. 2007; Truong-Bolduc et al. 2011). The relative expression levels of most genes were less decreased in ARSA than in ASSA at all treatments. This suggests that adhesion-related genes (clfA, eno, and fnbA) and efflux-related genes (mdeA, norB, and norC) can contribute to enhanced antibiotic resistance and bacterial pathogenicity (Huang et al. 2004). Therefore, the results emphasize the importance of controlling the ingested antibiotic-resistant pathogens in the intestinal tract. Although bacteriophages can be a promising approach to control bacterial infection, genome-based study is needed to understand the ecological interaction between bacteriophages and host bacteria in the complex gut environment (Abedon et al. 2011; Ventura et al. 2011).
Relative expression of adhesion-related (clfA, A; eno, B; and fnbA, C) and efflux-related (mdeA, D; norB, E; and norC, F) genes in Staphylococcus aureus exposed to the simulated gastric juice containing 0.3 % pepsin in TSB of pH 3.0 (TSB-3) and intestinal juices containing 0.03 % bile salt in TSB of pH 8.0 (TSB-8) with L. rhamnosus (LR), bacteriophage SA11 (SA11), and L. rhamnosus and SA11 (LR + SA11). Means with different letters (A–D) on the bars within antibiotic-sensitive S. aureus (ASSA; grey square) and different letters (a–d) on the bars within antibiotic-resistant S. aureus (ARSA; filled square) are significantly different at P < 0.05. Asterisk (*) indicates the significance between ASSA (grey square) and ARSA (filled square) at P < 0.05
In conclusion, this study highlights the potential application of bacteriophage in combination with probiotic for controlling ingested ARSA in the simulated intestinal conditions. The most significant findings in this study were that (1) high numbers of S. aureus exposed to the simulated gastric juices with dynamic pH and different nutrient base could reach the intestinal tract and show high sliding motility responsible for bacterial attachment to the epithelial cells; (2) the bacteriophage SA11 combined with probiotic L. rhamnosus effectively inhibited the growth of ASSA and ARSA under the intestinal condition, which can be an alternative way to prevent foodborne bacterial infection; (3) the enhanced antibiotic resistance and virulence potential were attributed to the up-regulation of adhesion-related and efflux-related genes. These results might provide useful information to control ingested foodborne pathogens and improve intestinal microflora. Further study is needed to characterize the relationship among bacteriophages, food components, indigenous microflora, and epithelial cells in the complex GIT.
References
Abedon ST, Kuhl SJ, Blasdel BG, Kutter EM (2011) Phage treatment of human infections. Bacteriophage 1:66–85
Atterbury RJ et al (2007) Bacteriophage therapy to reduce Salmonella colonization of broiler chickens. Appl Environ Microbiol 73:4543–4549
Bardina C, Spricigo DA, Cortes P, Llagostera M (2012) Significance of the bacteriophage treatment schedule in reducing Salmonella colonization of poultry. Appl Environ Microbiol 78:6600–6607
Barmpalia-Davis IM, Geornaras I, Kendall PA, Sofos JN (2008) Differences in survival among 13 Listeria monocytogenes strains in a dynamic model of the stomach and small intestine. Appl Environ Microbiol 74:5563–5567
Bhalla A, Aron D, Donskey C (2007) Staphylococcus aureus intestinal colonization is associated with increased frequency of S. aureus on skin of hospitalized patients. BMC Infect Dis 7:105
Bleackley J, Cooper J, Kaminski M, Sandilands S (2009) The reduction of T7 phage adsorption in Escherichia coli B23 cells treated with sub-lethal levels of kanamycin. J Exp Microbiol Immunol 13:89–92
Bourlioux P, Koletzko B, Guarner F, Braesco V (2003) The intestine and its microflora are partners for the protection of the host. Am J Clin Nutr 78:675–683
Ceuppens S, Uyttendaele M, Hamelink S, Boon N, Van de Wiele T (2012) Inactivation of Bacillus cereus vegetative cells by gastric acid and bile during in vitro gastrointestinal transit. Gut Pathog 4:11
Chow MS, Rouf MA (1983) Isolation and partial characterization of two Aeromonas hydrophila bacteriophages. Appl Environ Microbiol 45:1670–1676
Collado MC, Meriluoto J, Salminen S (2007) Role of commercial probiotic strains against human pathogen adhesion to intestinal mucus. Lett Appl Microbiol 45:454–460
DeMarco CE, Cushing LA, Frempong-Manso E, Seo SM, Jaravaza TAA, Kaatz GW (2007) Efflux-related resistance to norfloxacin, dyes, and biocides in bloodstream isolates of Staphylococcus aureus. Antimicrob Agents Chemother 51:3235–3239
Foster JW (2001) Acid stress response of Salmonella and E. coli: survival mechanisms, regulation, and implications for pathogenesis. J Microbiol 39:89–94
Fuller R (1989) Probiotics in man and animals. J Appl Bacteriol 66:365–378
Greenacre EJ, Lucchini S, Hinton JCD, Brocklehurst TF (2006) The lactic acid-induced acid tolerance response in Salmonella enterica Serovar Typhimurium induces sensitivity to hydrogen peroxide. Appl Environ Microbiol 72:5623–5625
Gunn JS (2000) Mechanisms of bacterial resistance and response to bile. Microbes Infect 2:907–913
Hammad AM, Shimamoto T (2010) Towards a compatible probiotic-antibiotic combination therapy: assessment of antimicrobial resistance in the Japanese probiotics. J Appl Microbiol 109:1349–1360
Huang J et al (2004) Novel chromosomally encoded multidrug efflux transporter MdeA in Staphylococcus aureus. Antimicrob Agents Chemother 48:909–917
Kaito C, Sekimizu K (2007) Colony spreading in Staphylococcus aureus. J Bacteriol 189:2553–2557
Kim MS, Myung H (2012) Complete genome of Staphylococcus aureus phage SA11. J Virol 86:10232
Koseki S, Mizuno Y, Sotome I (2011) Modeling of pathogen survival during simulated gastric digestion. Appl Environ Microbiol 77:1021–1032
Lei MG, Cue D, Roux CM, Dunman PM, Lee CY (2011) Rsp inhibits attachment and biofilm formation by repressing fnbA in Staphylococcus aureus MW2. J Bacteriol 193:5231–5241
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2−∆∆CT Method. Methods 25:402–408
Mathur S, Singh R (2005) Antibiotic resistance in food lactic acid bacteria–a review. Int J Food Microbiol 105:281–295
Matsuzaki S et al (2005) Bacteriophage therapy: a revitalized therapy against bacterial infectious diseases. J Infect Chemother 11:211–219
Muller-Merbacha M, Kohler K, Hinrichs J (2007) Environmental factors for phage-induced fermentation problems: replication and adsorption of the Lactococcus lactis phage P008 as influenced by temperature and pH. Food Microbiol 24:695–702
Nemati M, Hermans K, Devriese LA, Maes D, Haesebrouck F (2009) Screening of genes encoding adhesion factors and biofilm formation in Staphylococcus aureus isolates from poultry. Avian Pathol 38:513–517
O’Connell DP, Nanavaty T, McDevitt D, Gurusiddappa S, Höök M, Foster TJ (1998) The fibrinogen-binding MSCRAMM (clumping factor) of Staphylococcus aureus has a Ca2+-dependent inhibitory site. J Biol Chem 273:6821–6829
Oelschlaeger TA (2010) Mechanisms of probiotic actions - A review. Int J Med Microbiol 300:57–62
Pereira V, Lopes C, Castro A, Silva J, Gibbs P, Teixeira P (2009) Characterization for enterotoxin production, virulence factors, and antibiotic susceptibility of Staphylococcus aureus isolates from various foods in Portugal. Food Microbiol 26:278–282
Servin AL, Coconnier MH (2003) Adhesive of probiotic strains to the intestinal mucosa and interaction with pathogens. Best Pract Res Clin Gastroenterol 17:741–754
Smith JL (2003) The role of gastric acid in preventing foodborne disease and how bacteria overcome acid conditions. J Food Prot 66:1292–1303
Stutz K, Stephan R, Tasara T (2011) SpA, ClfA, and FnbA genetic variations lead to staphaurex test-negative phenotypes in bovine mastitis Staphylococcus aureus isolates. J Clin Microbiol 49:638–646
Truong-Bolduc QC et al. (2011) Implication of the norB efflux pump in the adaptation of S. aureus to growth at acid pH and resistance to moxifloxacin. Antimicrob Agents Chemother:AAC.00289-00211
Vancraeynest D, Hermans K, Haesebrouck F (2004) Genotypic and phenotypic screening of high and low virulence Staphylococcus aureus isolates from rabbits for biofilm formation and MSCRAMMs. Vet Microbiol 103:241–247
Ventura M, Sozzi T, Turroni F, Matteuzzi D, Sinderen D (2011) The impact of bacteriophages on probiotic bacteria and gut microbiota diversity. Genes & Nutrition 6:205–207
Vesterlund S, Karp M, Salminen S, Ouwehand AC (2006) Staphylococcus aureus adheres to human intestinal mucus but can be displaced by certain lactic acid bacteria. Microbiology 152:1819–1826
Woo J, Ahn J (2013) Probiotic-mediated competition, exclusion and displacement in biofilm formation by food-borne pathogens. Lett Appl Microbiol 56:307–313
Xu H, Lee HY, Ahn J (2008) Cross-protective effect of acid-adapted Salmonella enterica on resistance to lethal acid and cold stress conditions. Lett Appl Microbiol 47:290–297
Zhu H, Hart CA, Sales D, Roberts NB (2006) Bacterial killing in gastric juice—effect of pH and pepsin on Escherichia coli and Helicobacter pylori. J Med Microbiol 55:1265–1270
Acknowledgments
This study was supported by Research Grant from Kangwon National University.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Erko Stackebrandt.
Rights and permissions
About this article
Cite this article
Woo, J., Ahn, J. Assessment of synergistic combination potential of probiotic and bacteriophage against antibiotic-resistant Staphylococcus aureus exposed to simulated intestinal conditions. Arch Microbiol 196, 719–727 (2014). https://doi.org/10.1007/s00203-014-1013-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00203-014-1013-z