Abstract
Summary
Low vitamin D in patients with hip fracture is common. In the present study, 407 of 872 (47%) patients had serum calcidiol less than 50 nmol/L. Patients with low vitamin D had more delirium, more new hip fractures, and more medical readmissions, but not more orthopedic complications after 1 year.
Introduction
We wanted to study the relation between vitamin D level and postoperative orthopedic and medical complications in patients with hip fracture. In addition, we investigated the effect of giving a single-dose cholecalciferol 100.000 IU.
Methods
Data were taken from the local hip fracture register. Logistic regression analyses including vitamin D level and potentially confounding variables were performed for complications and readmissions.
Results
A total of 407 (47%) of 872 included hip fractures had low vitamin D at baseline. A total of 155 (18%) developed delirium, and the risk was higher in vitamin D-deficient patients (odds ratio (OR) 1.48, 95% confidence interval (CI) 1.04 to 2.12; p = 0.03). A total of 261 (30%) were readmitted for non-hip-related conditions. Low vitamin D was associated with a higher risk of medical readmissions within 30 days (OR 1.64 (1.03 to 2.61); p = 0.036) and 12 weeks (OR 1.47 (95% CI 1.02 to 2.12); p = 0.039). There was a higher risk of a new hip fracture (OR 2.84 (95% CI 1.15 to 7.03) p = 0.024) in vitamin D-deficient patients. A total of 105 (12%) developed at least one orthopedic complication, with no correlation to baseline vitamin D. Among vitamin D-deficient patients, those receiving a single-dose of 100.000 IU cholecalciferol had fewer orthopedic complications (OR 0.32 (95% CI 0.11 to 0.97) p = 0.044) the first 30 days after surgery.
Conclusion
Low vitamin D at admission for hip fracture increased the risk of delirium, a new hip fracture, and medical readmissions, but not orthopedic complications. The role of vitamin D supplementation to prevent orthopedic complications requires further study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The number of hip fractures is estimated to increase worldwide to 2.6 million by 2025 and 4.5 million in 2050 [1]. Hip fracture rates have declined in Norway the past years [2], but the forecasted aging of the population might increase the absolute number of fractures [3]. Management of these fractures and change in preventive strategies will remain an important task for healthcare systems globally. Patients with hip fractures are usually elderly, with preexisting comorbidities including cognitive impairment and frequent polypharmacy [4]. Hip fractures are potentially life-changing events that may lead to impaired physical function, loss of independence, or death [5]. Acute surgery is almost always required, which increases the risk of surgical and medical complications in an already vulnerable patient [6]. Up to half of the patients may not regain their pre-fracture level of mobility [7], and every third hip fracture patients require readmission within 1 year after surgery [4, 8]. Improved treatment and secondary prophylaxis may mitigate the adverse effects of hip fractures and reduce associated costs.
Patients with hip fractures have been reported to suffer from low vitamin D [9, 10]. Recent studies have identified acute drops in vitamin D level directly after a fracture [11, 12]. Adequate vitamin D level is important in maintaining bone health, bone mineralization, and bone resorption, as vitamin D is the key controller of calcium and skeletal homeostasis [13, 14]. Low levels of vitamin D may cause secondary hyperparathyroidism leading to high bone turnover followed by bone loss and mineralization defects [15], as well as increased risk of fractures [10, 15]. In addition, low levels of 25-hydroxyvitamin D (25(OH)D) have been associated with an increased risk of falls [16, 17], adding to an already increased risk of a second hip fracture after an initial hip fracture. Vitamin D supplementation may prevent fractures [18] and has been shown to reduce the risk of falls [19].
There is an ongoing debate regarding optimal doses of vitamin D regimens for supplementation and diagnostic methodology [20]. In addition, the recommended level of circulating 25(OH)D varies from 30 to 100 nmol/L, depending on local recommendations [21]. The influence of vitamin D on bone healing and postoperative complications is not fully understood. Orthopedic surgeons prescribe vitamin D and calcium to fracture patients to increase the fracture healing process. However, strategies and guidance on fracture healing supplementation are poor, and no human studies have shown clinically relevant increased fracture healing with supplementation of vitamin D. To our knowledge, no studies have found an association between vitamin D levels and postoperative complications after hip fractures. If ensuring an adequate level of vitamin D could reduce the risk of complications and readmissions after a hip fracture, this would be a welcome, and most likely cost-effective, addition to the care.
From May 2014, we routinely measured 25(OH)D in hip fracture patients aiming to improve our secondary fracture prevention. From August 2015, we recommended a loading dose of 100.000 IU cholecalciferol orally for all patients while admitted, in addition to our previous recommendation of 0.5 to 1 g calcium and 800 IU vitamin D daily. The main object of this study was (1) to understand the relation between vitamin D deficiency and postoperative orthopedic complications, especially healing problems. (2) Furthermore, we wanted to assess the relation between vitamin D and medical complications and deaths within 1 year. (3) To study adherence to routines on giving cholecalciferol to hip fracture patients, and (4) evaluate the effect of adding a single-dose cholecalciferol 100.000 IU as a standard treatment.
Patients and methods
Patient inclusion and exclusion
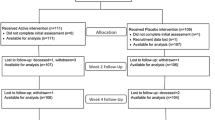
All patients admitted with a hip fracture at Oslo University Hospital registered in the local hip fracture register from May 7th, 2014, to June 9th, 2018, were considered for inclusion in the study. A total of 1152 fractures in 1122 patients were assessed. Patient inclusion criteria were (i) hip fracture requiring surgery (femoral neck fracture, trochanteric, or sub-trochanteric fracture), (ii) available serum 25(OH)D level, and (iii) patients resided in the hospital catchment area. Information on deceased patients was obtained from the National Population Register. In 23 cases, a second hip fracture occurred within 1 year, and this was considered to be related to the preceding fracture. In these cases, only the first fracture was included. A second hip fracture occurring after 1 year was included in the study as a separate event (n = 7). This left a total of 872 fractures in 865 patients for analysis (Fig. 1).
Definitions
Vitamin D was quantified by liquid chromatography–tandem mass spectrometry with determination of 25 hydroxyvitamin D2 (25(OH)D2) and 25 hydroxyvitamin D3 (25(OH)D3) levels (Hormone Laboratory, Oslo University Hospital, Oslo, Norway) [22]. The combined concentration of 25(OH)D2 and 25(OH)D3 was considered the patients’ 25(OH)D. Blood was drawn the first or second postoperative day. Vitamin D deficiency was defined as serum 25(OH)D level less than 50 nmol/L. Orthopedic complications were defined as complications related to the hip fracture and initial surgery within 1 year, including surgical site infection, hematoma/bleeding, Trendelenburg gait, peroneal nerve palsy, avascular necrosis, hip instability, mechanical failure of internal fixation, peri-implant-fracture, and non-union. A medical complication was defined as any medical event including infection, renal, respiratory, cardiovascular, gastrointestinal, musculoskeletal, or neurological event that required hospitalization within 1 year after the hip fracture.
Statistical analysis
Continuous data were presented with means and standard deviations (SD), and categorical data were presented as frequencies and proportions. Bivariate analyses were done with Students t test or chi-square test. Logistic regression analyses were performed on variables from the bivariate analyses with a p value < 0.1. These regression analyses were done to adjust for potentially confounding variables. ASA class, gender, age, and pre-fracture level of care were chosen a priori as covariates as they were believed to potentially influence the outcome. In addition, when looking for an effect of the cholecalciferol loading dose, we also added osteoporosis treatment as a co-variate to reduce the risk of a false-positive finding due to selection bias. The outcome variables of both sets of regression analyses were incidence of complications, readmissions, and deaths. We estimated the variance inflation factor (VIF) to detect multicollinearity of the independent variables. Significance was set at p < 0.05. Statistical analysis was performed using SPSS for Windows version 26 (SPSS Inc., Chicago, IL).
Results
Baseline characteristics
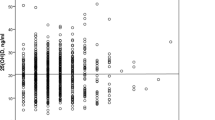
Mean age was 81 years (range 40 to 104, SD 11.5). A total of 571 (66%) were female and 322 (37%) were in ASA group 1 or 2 (Table 1). Mean vitamin D level was 52 (range 12 to 134, SD 21.4). With 50 nmol/L as a threshold for deficiency, 407 (47%) were vitamin D deficient and 88 (10%) of them had vitamin D level below 25 nmol/L, indicating severe vitamin D deficiency.
A total of 247 (28%) patients developed one or more medical complications during the initial stay (Table 2). The most common were acute post-hemorrhagic anemia 143 (16%), urinary tract infection 129 (15%), and pneumonia 76 (9%). In addition, 155 (18%) were registered with delirium, 84 (21%) in the deficient group, and 71 (15%) in the non-deficient group. The risk of delirium was higher in vitamin D-deficient patients (OR 1.48, 95% CI 1.04 to 2.12; p = 0.03). Thirty-three (4%) developed deep venous thrombosis (DVT) or pulmonary embolism while admitted or within 1 year after discharge, with 21 (5%) in the vitamin D-deficient group and 12 (3%) in the non-deficient group (OR 2.07 (95% CI 1.0 to 4.3); p = 0.05).
Vitamin D status and fracture-related complications
A total of 105 (12%) patients developed one or more orthopedic complications within the first year after hip fracture. There was no relation between vitamin D deficiency and the risk of an orthopedic complication (Table 2). Among the patients with orthopedic complications, 71 (8%) required secondary surgery within 1 year.
Vitamin D deficiency and risk for readmission to hospital
A total of 261 (30%) patients were readmitted for non-hip-related conditions within 1 year (Table 3). Low vitamin D was associated with a higher risk of medical readmissions at 30 days and 12 weeks post-fracture (Table 3). Analyses of separate diagnoses and diagnosis groups revealed no single diagnosis driving this difference. The most common causes of medical readmission were infections (n = 118), with pneumonia as the most common (n = 62), followed by urinary tract infection (n = 53). Gastrointestinal conditions (n = 50) were also common. A total of 122 (14%) patients were admitted 2 or more times, up to a maximum of 6 readmissions the first year. A contralateral hip fracture within 1 year was more common in the vitamin D-deficient group. A total of 200 (23%) patients died within 1 year after the first hip fracture. There was no statistically significant relation between vitamin D deficiency and mortality (Table 3).
Vitamin D loading dose
After the change of routines in August 2015, the treatment with cholecalciferol loading dose went from 7 of 244 (3%) to 459 of 628 (73%; p < 0.001) (Table 4). The proportion of patients recommended a daily supplement of at least 800 IU vitamin D daily after discharge decreased from 237 (97%) to 541 (86%; p < 0.001). At the same time, patients who were evaluated or treated for osteoporosis increased from 145 (60%) to 529 (85%). We investigated a potential effect of the loading dose of cholecalciferol on orthopedic complications, secondary surgeries, medical readmissions, and mortality, as well as a contralateral hip fracture, analyzing only the vitamin D-deficient patients (n = 407). There was a statistically significant correlation between early (within 30 days) orthopedic complications and revision surgeries, and the single-dose of cholecalciferol (Table 5).
Discussion
We found a high rate of complications during admission and after discharge, emphasizing that patients with hip fractures are vulnerable. Our results confirm that hip fracture patients suffer from low levels of vitamin D which may indicate that elderly with hip fractures do not receive necessary vitamin D supplementation to maintain good bone health. However, the effect of vitamin D supplementation and optimal vitamin D doses for fracture prevention is debated. Some studies and meta-analyses have shown a benefit of vitamin D supplementation [18, 19] in fracture prevention, but several report no effect of vitamin D alone, regardless of dose [23,24,25]. High doses of vitamin D have even been reported to increase the risk of falls and fractures [26].
Orthopedic complications
Contrary to our initial hypothesis, vitamin D deficiency was not a risk factor for delayed healing or other fracture-related complications in our population. Due to the effects of vitamin D on bone, fracture healing complications could be expected in vitamin D-deficient patients. The literature lacks comprehensive data, and findings are not conclusive. Similar to our results, Bodendorfer et al. found no correlation between 25(OH)D levels and healing complications or reoperations [27]. Equally, two small case-control studies identified no difference in the prevalence of vitamin D deficiency in patients with a delayed union or non-union compared to normal fracture healing [28, 29]. Others have demonstrated several cases of low serum vitamin D in patients with non-union or delayed union compared with normal bone healing [30,31,32], implying that vitamin D levels may affect non-union rate. Brinker et al. suggested that there may be an effect of vitamin D deficiency on clinical fracture healing, as 68% of their patients with non-union were vitamin D deficient [31]. In a review, Gorter et al. maintained that vitamin D has a role in fracture healing, but the available data are too inconsistent to conclude [33].
Medical complications
Almost 30% of our patients had a medical complication while admitted, which is more than the 20% reported by Fakler et al. [34]. Contrary to Fakler et al., we found that acute medical complications during the initial stay seemed unrelated to vitamin D status. One of three patients in our material was readmitted due to medical complications within 1 year. This is consistent with previous findings [4, 8]. There was a statistically significant higher risk of medical readmission during the first 3 months in patients with low levels of 25(OH)D. An association has been suggested between low 25(OH)D and increased inflammation due to its effect in innate and acquired host defense [35]. Miller et al. suggest that inflammation, measured on serum interleukin-6, may contribute to prolonged rehabilitation after hip fracture [36]. In elderly with comorbidities, fatigue and inactivity after a hip fracture can lead to infection or exacerbation of a preexisting disease which may further explain the correlation.
Other complications
Twenty-three (3%) patients sustained a second hip fracture during the first year with a higher risk in the vitamin D-deficient group. This finding is in line with previous studies, suggesting that low serum vitamin D is associated with an increased risk of falls [16, 17], and subsequent new hip fracture [9, 10]. Interestingly, we found that vitamin D-deficient patients had a higher risk of delirium during the primary hospital stay. This is consistent with the case-control study of Torbergsen et al., who found that 51% of hip fracture patients had delirium during hospitalization and that concentrations of 25(OH)D were lower in cases compared with controls [37]. The proportion of patients with delirium in our material was low compared to Torbergsen et al. where delirium was a key variable and actively sought [37]. During our study period, patients were not routinely tested for delirium; hence, most patients have likely been diagnosed based on a clinical impression with clear symptoms, such as active confusion or agitation. Vitamin D receptors are located in the brain cortex and hippocampus, which are important areas for cognition, neurotransmission, and neuroimmune modulation, including anti-inflammatory and antioxidant effects [38]. Neurotransmission, inflammation, and chronic stress are factors in the delirium pathophysiology hypothesis, and vitamin D and other antioxidants inhibit inflammation [39]. Therefore, delirium in vitamin D-deficient patients may be caused by increased inflammation as a consequence of reduced anti-inflammatory activity caused by low 25(OH)D.
We also found a correlation between low vitamin D and deep vein thrombosis and pulmonary embolism. Reduced vitamin D level has previously been associated with increased risk of venous thromboembolism [40, 41]. Koyama et al. suggested that vitamin D3 exerts anticoagulant effects by upregulating thrombomodulin and downregulating tissue factor expression in acute leukemia cells [41]. In addition, Khademvatani et al. found a significantly higher prevalence of patients with deficient 25(OH)D in the DVT group compared to the control group [40]. However, the prospective population-based study of Brodin et al. found no association between normal serum levels of 25(OH)D and decreased future risk of venous thromboembolism [42]. In addition, a large case-control study found that vitamin D supplementation not was associated with a decreased risk of venous thrombosis after extensive statistical adjustments, suggesting a spurious correlation in previous studies [43].
Cholecalciferol loading dose
Adherence to the new routine with a 100,000-IU cholecalciferol loading dose was achieved in three in four patients (Table 4). We consider this a reasonable goal attainment, bearing in mind that some patients probably had contraindications and others declined this treatment. Interestingly, the proportion of patients receiving osteoporosis treatment increased at the same time as the vitamin D loading dose routine was started, even though the routines for osteoporosis treatment remained unchanged. This may reflect that the attention to medical prevention in general increased through the efforts to implement the change in treatment recommendations. We saw no signs of a negative effect of the single cholecalciferol dose. The cholecalciferol loading dose was on the contrary inversely correlated with early orthopedic complications and early reoperations (Table 5). However, this needs to be interpreted with caution, as low vitamin D was not a risk factor for orthopedic complications (Table 2), and the confidence intervals were wide. Even though we adjusted for known risk factors, there is a possibility that patients not receiving the single-dose of cholecalciferol were a priori at a higher risk of early complications. On the other hand, if there is a true effect of the additional vitamin D, it is reasonable that this effect is most pronounced in the short term, as oral supplementation of a high dose of vitamin D may have its strongest effect between 7 and 30 days after supplementation [44].
Strengths and limitations
This study is descriptive in nature, and no conclusion may be drawn on cause and effect. Especially, the analyses on the potential effect of vitamin D supplements must be interpreted with caution. Several of the statistically significant findings have wide confidence intervals. Our study, however, has a large sample size. We have a complete register with a large amount of data on our patients which makes it possible to do comparative analyses. The cholecalciferol loading dose was given at the hospital and the compliance was therefore high. There was no difference in diagnostic methodology since vitamin D levels were measured in the same way by the same laboratory throughout the period.
The main limitation of our study was the retrospective collecting of important outcome data. The baseline data were collected prospectively, but data after discharge, except mortality, were collected by chart review. To decrease the risk of losing data, we excluded patients living outside the hospital catchment area. In our health system, the patients belong by home address to one single hospital for acute cases, and if they are traveling and admitted somewhere else, they will be referred to the responsible hospital as soon as possible. We cannot ignore the risk that vitamin D deficiency in the present material is merely a marker of morbidity, as suggested in the study of Autier et al. [45]. We did, however, not find no clear evidence of this when examining vitamin D status against ASA grade, age, gender, or permanent nursing home residency, nor when examining collinearity. There was also no correlation between vitamin D deficiency and mortality. More detailed baseline data would have been helpful to further examine this, for instance being able to control for BMI. Most patients were recommended continuous supplementation with vitamin D and calcium, but we have no evidence to what extent this was carried out. Almost no repeat measurements of vitamin D were available. Finally, we have performed multiple comparisons and cannot exclude that the statistically significant findings are by chance.
Conclusion
Low levels of vitamin D were not correlated with orthopedic complications and mortality, but with the risk of medical readmissions. There was a higher risk of delirium and a new hip fracture in patients with vitamin D deficiency. Three-fourth received 100,000 IU cholecalciferol as per routine. There was a correlation between patients receiving the cholecalciferol loading dose and a lower risk of early orthopedic complications. Patients who received the loading dose did not have lower risk medical readmissions or other complications. The consequences of low vitamin D levels in hip fracture patients and the effect of vitamin D supplementation need to be examined further in large prospective or randomized trials.
Data availability
The database is available on request from the last author (ffrihagen@gmail.com).
References
Gullberg B, Johnell O, Kanis JA (1997) World-wide projections for hip fracture. Osteoporos Int 7(5):407–413. https://doi.org/10.1007/pl00004148
Omsland TK, Holvik K, Meyer HE, Center JR, Emaus N, Tell GS, Schei B, Tverdal A, Gjesdal CG, Grimnes G, Forsmo S, Eisman JA, Sogaard AJ (2012) Hip fractures in Norway 1999-2008: time trends in total incidence and second hip fracture rates: a NOREPOS study. Eur J Epidemiol 27(10):807–814. https://doi.org/10.1007/s10654-012-9711-9
Sogaard AJ, Holvik K, Meyer HE, Tell GS, Gjesdal CG, Emaus N, Grimnes G, Schei B, Forsmo S, Omsland TK (2016) Continued decline in hip fracture incidence in Norway: a NOREPOS study. Osteoporos Int 27(7):2217–2222. https://doi.org/10.1007/s00198-016-3516-8
Watne LO, Torbergsen AC, Conroy S, Engedal K, Frihagen F, Hjorthaug GA, Juliebo V, Raeder J, Saltvedt I, Skovlund E, Wyller TB (2014) The effect of a pre- and postoperative orthogeriatric service on cognitive function in patients with hip fracture: randomized controlled trial (Oslo Orthogeriatric Trial). BMC Med 12:63. https://doi.org/10.1186/1741-7015-12-63
Haentjens P, Magaziner J, Colon-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, Boonen S (2010) Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med 152(6):380–390. https://doi.org/10.7326/0003-4819-152-6-201003160-00008
Ali AM, Gibbons CE (2017) Predictors of 30-day hospital readmission after hip fracture: a systematic review. Injury 48(2):243–252. https://doi.org/10.1016/j.injury.2017.01.005
Vochteloo AJ, Moerman S, Tuinebreijer WE, Maier AB, de Vries MR, Bloem RM, Nelissen RG, Pilot P (2013) More than half of hip fracture patients do not regain mobility in the first postoperative year. Geriatr Gerontol Int 13(2):334–341. https://doi.org/10.1111/j.1447-0594.2012.00904.x
Teixeira A, Trinquart L, Raphael M, Bastianic T, Chatellier G, Holstein J (2009) Outcomes in older patients after surgical treatment for hip fracture: a new approach to characterise the link between readmissions and the surgical stay. Age Ageing 38(5):584–589. https://doi.org/10.1093/ageing/afp124
Sprague S, Petrisor B, Scott T, Devji T, Phillips M, Spurr H, Bhandari M, Slobogean GP (2016) What is the role of vitamin D supplementation in acute fracture patients? A systematic review and meta-analysis of the prevalence of hypovitaminosis D and supplementation efficacy. J Orthop Trauma 30(2):53–63. https://doi.org/10.1097/bot.0000000000000455
Torbergsen AC, Watne LO, Wyller TB, Frihagen F, Stromsoe K, Bohmer T, Mowe M (2015) Vitamin K1 and 25(OH)D are independently and synergistically associated with a risk for hip fracture in an elderly population: a case control study. Clin Nutr 34(1):101–106. https://doi.org/10.1016/j.clnu.2014.01.016
Binkley N, Coursin D, Krueger D, Iglar P, Heiner J, Illgen R, Squire M, Lappe J, Watson P, Hogan K (2017) Surgery alters parameters of vitamin D status and other laboratory results. Osteoporos Int 28(3):1013–1020. https://doi.org/10.1007/s00198-016-3819-9
Ettehad H, Mirbolook A, Mohammadi F, Mousavi M, Ebrahimi H, Shirangi A (2014) Changes in the serum level of vitamin d during healing of tibial and femoral shaft fractures. Trauma Mon 19(1):e10946. https://doi.org/10.5812/traumamon.10946
Fischer V, Haffner-Luntzer M, Amling M, Ignatius A (2018) Calcium and vitamin D in bone fracture healing and post-traumatic bone turnover. Eur Cell Mater 35:365–385. https://doi.org/10.22203/eCM.v035a25
Ray M (2019) Vitamin D and fracture healing: an ongoing puzzle. Int J of Orth 6(5):1050–1060. https://doi.org/10.17554/j.issn.2311-5106.2019.06.302
Lips P (2001) Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications. Endocr Rev 22(4):477–501. https://doi.org/10.1210/edrv.22.4.0437
Flicker L, Mead K, MacInnis RJ, Nowson C, Scherer S, Stein MS, Thomasx J, Hopper JL, Wark JD (2003) Serum vitamin D and falls in older women in residential care in Australia. J Am Geriatr Soc 51(11):1533–1538. https://doi.org/10.1046/j.1532-5415.2003.51510.x
Faulkner KA, Cauley JA, Zmuda JM, Landsittel DP, Newman AB, Studenski SA, Redfern MS, Ensrud KE, Fink HA, Lane NE, Nevitt MC (2006) Higher 1,25-dihydroxyvitamin D3 concentrations associated with lower fall rates in older community-dwelling women. Osteoporos Int 17(9):1318–1328. https://doi.org/10.1007/s00198-006-0071-8
Bischoff-Ferrari HA, Willett WC, Wong JB, Giovannucci E, Dietrich T, Dawson-Hughes B (2005) Fracture prevention with vitamin D supplementation: a meta-analysis of randomized controlled trials. JAMA 293(18):2257–2264. https://doi.org/10.1001/jama.293.18.2257
Bischoff-Ferrari HA, Dawson-Hughes B, Staehelin HB, Orav JE, Stuck AE, Theiler R, Wong JB, Egli A, Kiel DP, Henschkowski J (2009) Fall prevention with supplemental and active forms of vitamin D: a meta-analysis of randomised controlled trials. BMJ 339:b3692. https://doi.org/10.1136/bmj.b3692
Patton CM, Powell AP, Patel AA (2012) Vitamin D in orthopaedics. J Am Acad Orthop Surg 20(3):123–129. https://doi.org/10.5435/JAAOS-20-03-123
Dawson-Hughes B, Heaney RP, Holick MF, Lips P, Meunier PJ, Vieth R (2005) Estimates of optimal vitamin D status. Osteoporos Int 16(7):713–716. https://doi.org/10.1007/s00198-005-1867-7
Cashman KD, Dowling KG, Skrabakova Z, Kiely M, Lamberg-Allardt C, Durazo-Arvizu RA, Sempos CT, Koskinen S, Lundqvist A, Sundvall J, Linneberg A, Thuesen B, Husemoen LL, Meyer HE, Holvik K, Gronborg IM, Tetens I, Andersen R (2015) Standardizing serum 25-hydroxyvitamin D data from four Nordic population samples using the vitamin D standardization program protocols: shedding new light on vitamin D status in Nordic individuals. Scand J Clin Lab Invest 75(7):549–561. https://doi.org/10.3109/00365513.2015.1057898
Yao P, Bennett D, Mafham M, Lin X, Chen Z, Armitage J, Clarke R (2019) Vitamin D and calcium for the prevention of fracture: a systematic review and meta-analysis. JAMA Netw Open 2(12):e1917789. https://doi.org/10.1001/jamanetworkopen.2019.17789
Bolland MJ, Grey A, Avenell A (2018) Effects of vitamin D supplementation on musculoskeletal health: a systematic review, meta-analysis, and trial sequential analysis. Lancet Diabetes Endocrinol 6(11):847–858. https://doi.org/10.1016/S2213-8587(18)30265-1
Bolland MJ, Grey A (2014) A case study of discordant overlapping meta-analyses: vitamin d supplements and fracture. PLoS One 9(12):e115934. https://doi.org/10.1371/journal.pone.0115934
Bischoff-Ferrari HA, Dawson-Hughes B, Orav EJ, Staehelin HB, Meyer OW, Theiler R, Dick W, Willett WC, Egli A (2016) Monthly high-dose vitamin D treatment for the prevention of functional decline: a randomized clinical trial. JAMA Intern Med 176(2):175–183. https://doi.org/10.1001/jamainternmed.2015.7148
Bodendorfer BM, Cook JL, Robertson DS, Della Rocca GJ, Volgas DA, Stannard JP, Crist BD (2016) Do 25-hydroxyvitamin D levels correlate with fracture complications? J Orthop Trauma 30(9):e312–e317. https://doi.org/10.1097/BOT.0000000000000639
Haining SA, Atkins RM, Guilland-Cumming DF, Sharrard WJ, Russell RG, Kanis JA (1986) Vitamin D metabolites in patients with established non-union of fracture. Bone Miner 1(3):205–209
Boszczyk AM, Zakrzewski P, Pomianowski S (2013) Vitamin D concentration in patients with normal and impaired bone union. Pol Orthop Traumatol 78:1–3
Pourfeizi HH, Tabriz A, Elmi A, Aslani H (2013) Prevalence of vitamin D deficiency and secondary hyperparathyroidism in nonunion of traumatic fractures. Acta Med Iran 51(10):705–710
Brinker MR, O’Connor DP, Monla YT, Earthman TP (2007) Metabolic and endocrine abnormalities in patients with nonunions. J Orthop Trauma 21(8):557–570. https://doi.org/10.1097/BOT.0b013e31814d4dc6
Ravindra VM, Godzik J, Dailey AT, Schmidt MH, Bisson EF, Hood RS, Cutler A, Ray WZ (2015) Vitamin D levels and 1-year fusion outcomes in elective spine surgery: a prospective observational study. Spine (Phila Pa 1976) 40(19):1536–1541. https://doi.org/10.1097/BRS.0000000000001041
Gorter EA, Hamdy NA, Appelman-Dijkstra NM, Schipper IB (2014) The role of vitamin D in human fracture healing: a systematic review of the literature. Bone 64:288–297. https://doi.org/10.1016/j.bone.2014.04.026
Fakler JK, Grafe A, Dinger J, Josten C, Aust G (2016) Perioperative risk factors in patients with a femoral neck fracture - influence of 25-hydroxyvitamin D and C-reactive protein on postoperative medical complications and 1-year mortality. BMC Musculoskelet Disord 17:51. https://doi.org/10.1186/s12891-016-0906-1
Kroner Jde C, Sommer A, Fabri M (2015) Vitamin D every day to keep the infection away? Nutrients 7(6):4170–4188. https://doi.org/10.3390/nu7064170
Miller RR, Cappola AR, Shardell MD, Hawkes WG, Yu-Yahiro JA, Hebel JR, Magaziner J (2006) Persistent changes in interleukin-6 and lower extremity function following hip fracture. J Gerontol A Biol Sci Med Sci 61(10):1053–1058. https://doi.org/10.1093/gerona/61.10.1053
Torbergsen AC, Watne LO, Frihagen F, Wyller TB, Brugaard A, Mowe M (2015) Vitamin deficiency as a risk factor for delirium. Eur Geriatr Med 6(4):314–318. https://doi.org/10.1016/j.eurger.2014.09.002
Annweiler C, Montero-Odasso M, Llewellyn DJ, Richard-Devantoy S, Duque G, Beauchet O (2013) Meta-analysis of memory and executive dysfunctions in relation to vitamin D. J Alzheimers Dis 37(1):147–171. https://doi.org/10.3233/JAD-130452
MacLullich AMJ, Ferguson KJ, Miller T, de Rooij SEJA, Cunningham C (2008) Unravelling the pathophysiology of delirium: a focus on the role of aberrant stress responses. J Psychosom Res 65(3):229–238. https://doi.org/10.1016/j.jpsychores.2008.05.019
Khademvatani K, Seyyed-Mohammadzad MH, Akbari M, Rezaei Y, Eskandari R, Rostamzadeh A (2014) The relationship between vitamin D status and idiopathic lower-extremity deep vein thrombosis. Int J Gen Med 7:303–309. https://doi.org/10.2147/IJGM.S64812
Koyama T, Shibakura M, Ohsawa M, Kamiyama R, Hirosawa S (1998) Anticoagulant effects of 1alpha,25-dihydroxyvitamin D3 on human myelogenous leukemia cells and monocytes. Blood 92(1):160–167
Hansen J-B, Jorde R, Svartberg J, Brox J, Vik A, Brækkan SK, Grimnes G, Lerstad G, Brodin EE (2017) Serum levels of vitamin D are not associated with future risk of venous thromboembolism. Thromb Haemost 109(05):885–890. https://doi.org/10.1160/th12-10-0728
Vuckovic BA, van Rein N, Cannegieter SC, Rosendaal FR, Lijfering WM (2015) Vitamin supplementation on the risk of venous thrombosis: results from the MEGA case-control study. Am J Clin Nutr 101(3):606–612. https://doi.org/10.3945/ajcn.114.095398
Kearns MD, Alvarez JA, Tangpricha V (2014) Large, single-dose, oral vitamin D supplementation in adult populations: a systematic review. Endocr Pract 20(4):341–351. https://doi.org/10.4158/EP13265.RA
Autier P, Boniol M, Pizot C, Mullie P (2014) Vitamin D status and ill health: a systematic review. Lancet Diabetes Endocrinol 2(1):76–89. https://doi.org/10.1016/S2213-8587(13)70165-7
Acknowledgments
Elise Berg Vesterhus, Oslo University Hospital, for database maintenance.
Funding
Oslo University Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethics approval
The hip fracture register and data collection were approved by the Hospital Data Protection Officer (2014/12309) and Regional Ethics Committee South Eastern Norway (2014/1433).
Consent to participate
Preapproved waiver for quality audit Hospital Data Protection Officer (PVO 2014/12309, PVO 2015/18831, and PVO 2020/11011) and Regional Ethics Committee South Eastern Norway (2014/1433).
Consent for publication
Preapproved waiver for quality audit Hospital Data Protection Officer (PVO 2014/12309, PVO 2015/18831, and PVO 2020/11011) and Regional Ethics Committee South Eastern Norway (2014/1433).
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ingstad, F., Solberg, L.B., Nordsletten, L. et al. Vitamin D status and complications, readmissions, and mortality after hip fracture. Osteoporos Int 32, 873–881 (2021). https://doi.org/10.1007/s00198-020-05739-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-020-05739-9