Abstract
Summary
RANKL-OPG should be explored in DMD patients to potentially provide targeted therapy. We quantified RANKL and OPG levels in DMD patients compared with controls. RANKL, OPG, and RANKL:OPG significantly declined with age in DMD patients suggesting some bone turnover markers are difficult to assess or use as therapeutic indicators.
Introduction
Osteoporosis in Duchenne muscular dystrophy (DMD) is multi-factorial in nature with high prevalence of fractures. RANKL-OPG should be explored to potentially provide targeted therapy for these patients. We quantified RANKL, OPG, and RANKL:OPG levels in DMD patients compared with controls and analyzed the influence of age, glucocorticoid use, ambulatory status, bone density, and fracture history.
Methods
DMD patients were enrolled at CHLA. Controls were recruited from general pediatric clinic and in collaboration with samples from a previously completed study. Free soluble RANKL and OPG levels were quantified using a sandwich ELISA.
Results
Fifty DMD patients and 50 controls were enrolled. DMD patients had a significant decline in RANKL, OPG, and RANKL:OPG with age (p = < 0.0001, p = 0.026, and p = 0.002, respectively) while healthy controls showed no significant change. RANKL trended lower in patients on glucocorticoids (p = 0.05), attributed to the significantly older age in the treatment group. RANKL and RANKL:OPG levels were significantly lower in the non-ambulatory group compared with the ambulatory group (p = 0.010 and 0.036 respectively), again likely due to their older age. There was no correlation of RANKL, OPG, or RANKL:OPG with DXA Z-score or presence of vertebral fractures.
Conclusion
There was significant decline in RANKL, OPG, and RANKL:OPG with age in DMD patients compared with controls, potentially due to disease severity or worsening osteoblastic function. This suggests some bone turnover markers may be difficult to assess or use as therapeutic indicators in DMD patients. Larger studies are needed to evaluate the role of RANKL-OPG in DMD patients to provide better targeted therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Duchenne muscular dystrophy (DMD) is the most common form of muscular dystrophy, affecting 1 in every 3500 to 5000 males and very rarely females [1]. Mutation in the dystrophin gene leads to progressive and severe muscle weakness with gradual loss of ambulation before 16 years of age [1]. Standard of care therapy involves the use of glucocorticoids, which has been shown to prolong ambulation as well as delay cardiac dysfunction, ventilatory support, and scoliosis [2, 3]. Persistent glucocorticoid use, progressive muscle weakness, and immobilization lead to poor bone health and secondary osteoporosis in patients with DMD with very few treatment options [4]. In a large retrospective study by Tian et al., the prevalence of overall fractures in their DMD cohort was approximately 80% with almost 60% having vertebral fractures by 18 years of age [5]. Therefore, it is important to gain further understanding of bone loss on a molecular level to provide better targeted therapy for these patients.
The receptor activator of nuclear factor kappa-Β ligand (RANKL)-osteoprotegerin (OPG) system is one such molecular pathway in bone remodeling that could be exploited to devise new, directed, therapy for DMD patients [6, 7]. RANKL, produced by osteoblasts, binds to its receptor on osteoclasts leading to their differentiation and maturation with subsequent increase in bone resorption [8]. OPG, a soluble decoy receptor, binds RANKL, inhibiting osteoclastogenesis and reducing bone resorption. The discovery of RANKL has given further insight into bone resorption regulation; however, its role in disease processes remains unclear [8].
There have been limited studies evaluating RANKL-OPG pathway in pediatrics. Prior reports have shown RANKL to be elevated in chronic inflammatory states as well as glucocorticoid exposure [9,10,11,12]. Thus, we aimed to quantify RANKL, OPG, and RANKL:OPG levels in a large DMD cohort and compare them to healthy, age and gender-matched, controls. In addition, we sought to correlate these levels with clinical measures such as age, glucocorticoid use, ambulatory status, bone density, and fracture history.
Materials and methods
Patients and controls
This cross-sectional study enrolled disease subjects from the multi-disciplinary DMD clinic as well as metabolic bone clinic at Children’s Hospital Los Angeles (CHLA). Inclusion criteria were ages 1–21 years with a genetic or biopsy-confirmed diagnosis of DMD. No patients were excluded. Age, ambulatory status, and glucocorticoid agent and dose were obtained from medical chart review. Treatment regimens were at the discretion of the primary neurologist and included daily prednisone, high-dose weekend prednisone, and daily deflazacort. Each DMD patient was then gender- and age-matched to a control subject.
Controls were recruited from general pediatric clinic at CHLA as well as in collaboration with serum samples stored from a previously completed study [13]. Inclusion criteria for the control group were ages 1–21 years, no known medical conditions, and no daily medications. Patients were excluded if they had sustained a fracture in the last 6 months.
This study was approved by the Institutional Review Board at the Children’s Hospital Los Angeles.
Biochemical determinants
Blood samples from CHLA and outside collaboration were collected upon consent and processed within 4–6 h. Samples were centrifuged, serum aliquoted, and frozen at − 80 °C until assayed. Free soluble RANKL levels were quantified using a sandwich enzyme-linked immunosorbent assay (ELISA) (Biomedica Medizinprodukte GmbH & Co KG, Vienna, Austria). The limit of detection for this assay is 0.01 pmol/L. Intra- and inter-assay precision is ≤ 5% and ≤ 3%, respectively. OPG was also measured using a sandwich ELISA (Biomedica Medizinprodukte GmbH & Co KG, Vienna, Austria). The limit of detection for this assay was 0.07 pmol/L, with intra- and inter-assay precision of ≤ 3% and ≤ 5%, respectively. The RANKL:OPG ratio was calculated for each patient by dividing the values of RANKL by OPG. Disease and control samples were run together at random.
Bone imaging
Bone imaging studies were collected retrospectively from the medical chart. Bone density was measured using dual-energy X-ray absorptiometry (DXA) (Hologic Horizon A-301054 m) with pediatric software analysis. Lumbar spine DXA at the level of L2–L4 was most consistently attained and used for analysis as it is one of the preferred sites for bone mineral density measurement in pediatrics [14]. Non-height-adjusted pediatric Z-scores were reported. Spinal posterior-anterior (PA) and lateral cervical, thoracic, and lumbar spine X-rays were done for assessment of presence of compression fracture.
Statistics
Descriptive statistics were used to summarize the distribution of variables. The results are presented as medians with interquartile range (IQR) due to the skewness of the distribution. Wilcoxon ranksum test was used to examine the difference in RANKL, OPG, and RANKL:OPG between two comparison groups such as subjects and controls. Kruskal-Wallis test was used to examine the difference in RANKL, OPG, and RANKL:OPG across age group. Correlation analyses were performed with Spearman’s non-parametric rank correlation. Differences in RANKL, OPG, and RANKL:OPG with glucocorticoid use and ambulatory status were examined using quantile regression model with age adjustment. All tests were two-tailed and conducted at the 5% significance level.
Results
Baseline characteristics
Fifty DMD patients and 50 controls were enrolled. Baseline clinical characteristics are shown in Tables 1 and 2. The mean age for both groups was 11.2 years ±0.67 (p = 0.99). Majority of DMD patients were non-ambulatory at the time of sampling and on glucocorticoids. Eight patients had osteoporosis in the setting of 1 or more vertebral fractures, none of whom were treated with bisphosphonates prior to sampling.
RANKL, OPG, and RANKL:OPG correlation with age
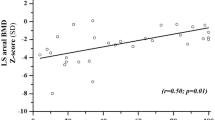
There was no difference in gender or age between the DMD group and healthy controls (Table 2). Correlation of RANKL by age for both DMD patients and controls is shown in Fig. 1. DMD patients had a significant decline in RANKL by age (p = < 0.0001) while healthy controls showed no significant change (p = 0.52). RANKL levels were then analyzed by age sub-groups, shown in Fig. 2. RANKL was significantly higher in the DMD group of 6–10 years compared with controls (p = 0.012). There was no statistical significance in RANKL between the remaining age groups (Fig. 2).
Comparison of RANKL levels between DMD patients and controls by age sub-groups. RANKL levels in pmol/L are on the y-axis with age sub-groups in years on the x-axis. IQR are shown by the shaded bar with median values lined within. Bars represent minimum and maximum values with outliers being more than 2 standard deviations above the median. There was significant difference of RANKL levels in the 6-–10-year age group
Similar to our RANKL results, DMD patients had a significant decline in OPG and RANKL:OPG ratio levels over time (p = 0.026 and p = 0.002, respectively) (Figs. 3 and 4). In contrast, control patients showed no significant decline in OPG or RANKL:OPG with age (p = 0.126 and p = 0.941, respectively) (Figs. 3 and 4). There was no significant difference in OPG or RANKL:OPG between DMD patients and controls when analyzed by age sub-groups.
RANKL, OPG, and RANKL:OPG by glucocorticoid use
Thirty-nine of the 50 DMD patients (78%) were treated with glucocorticoids at the time of sampling with a mean age of 12.3 years. Eleven patients were off steroids (physician or family choice) with a significantly lower mean age of 7.4 years (p = 0.004). Patients on glucocorticoids had a lower RANKL concentration approaching significance (median RANKL = 0.26 pmol/L) than those patients off treatment (median RANKL = 0.40 pmol/L, p = 0.05). In addition, patients on treatment had significantly lower OPG levels (median OPG = 3.7 pmol/L) compared with those patients off therapy (median OPG = 5.0, p = 0.023). There was no significant difference in the RANKL:OPG levels between the two groups. There was no significant difference in RANKL, OPG, or RANKL:OPG by glucocorticoid use after age-adjusted analysis. There was no significant difference in RANKL or RANKL:OPG levels between daily prednisone, daily deflazacort, or high-dose weekend prednisone treatment regimens.
RANKL, OPG, and RANKL:OPG by ambulatory status
Thirty-one of the 50 DMD patients (62%) were non-ambulatory at the time of sampling with a mean age of 13.4 years. The remaining 19 ambulatory patients had a significantly lower mean age of 7.6 years (p < 0.001). RANKL and RANKL:OPG levels were significantly lower in the non-ambulatory group (median RANKL = 0.22 pmol/L and RANKL:OPG = 0.06) compared with the ambulatory group (median RANKL = 0.31 pmol/L and RANKL:OPG = 0.07, p = 0.010 and 0.036 respectively). There was no significant difference in OPG levels (p = 0.64). No difference in RANKL, OPG, or RANKL:OPG was seen between the two groups after age-adjusted analysis.
RANKL and RANKL:OPG correlation with DXA
Seventeen of the 50 DMD patients (34%) had lumbar spine DXA evaluation completed at the time of analysis. There was no correlation noted between DXA Z-scores and RANKL level (Spearman r = − 0.10, p = 0.696) or RANKL:OPG (Spearman r = 0.08, p = 0.779).
RANKL, OPG, and RANKL:OPG correlation with vertebral fractures
Twenty of the 50 DMD patients had adequate spine films completed at the time of analysis. Of the 20 patients, 8 (40%) had one or more compression fractures. There was no significant difference in RANKL, OPG, or RANKL:OPG concentration in those with vertebral fractures compared with those without. Due to the small sample size, age adjustment analysis could not be completed; however, both groups had no significant difference in age.
Discussion
In our study, we found a significant decline in the RANKL, OPG, and RANKL:OPG levels with age only in the DMD cohort whereas in healthy controls, they were relatively unchanged over time. These findings could be explained by progressive impaired osteoblastic activity specifically seen in DMD patients resulting in decrease RANKL and OPG production over time. Rufo et al. reported significantly lower RANKL and RANKL:OPG in their 11 DMD patients compared with healthy controls [15]. Their group found that certain osteoblast transcription factors as well as bone morphogenic proteins were significantly decreased in DMD sera-treated mice compared with controls [15]. Furthermore, Nakagaki et al. demonstrated a reduced number of osteoblasts and osteoclasts per tissue area in mdx mice models compared with controls suggesting there may be intrinsic factors in DMD leading to poor osteoprogenitor cell differentiation, consequently impairing bone modeling and remodeling [16].
Interestingly, our data uncovered a significant difference in RANKL noted in the 6-–10-year age group compared with age-matched, healthy peers. To our knowledge, no previous pediatric studies have evaluated RANKL by age sub-groups in the DMD population. It is possible there are innate features unique to the DMD disease process during this time that allows upregulation of RANKL compared with other age groups. This could give insight into when more vigilant bone health surveillance is needed and is tempting to speculate that it may be a target period for treatment with RANKL antagonist therapy.
RANKL and OPG concentrations had a higher trend in those patients off glucocorticoid therapy compared with glucocorticoid-treated group, which we hypothesized was due to their significantly younger age. In addition, RANKL and RANKL:OPG levels were significantly higher in the ambulatory DMD group compared with those who were wheelchair bound, again likely due to the younger age group of those were still ambulatory. As DMD patients tend to lose ambulation by the second decade, it is possible by this time their circulating RANKL levels have naturally started to decline. After age adjustment, no difference in RANKL, OPG, and RANKL:OPG was seen in ambulatory status or glucocorticoid use further supporting our finding for age as a driving factor. Large, prospective, studies are needed to evaluate the effects of non-ambulatory status and glucocorticoid treatment and duration on RANKL and OPG levels as well as its clinical implication on bone resorption and ultimately osteoporosis commencement.
Only a small portion of DMD patients completed DXA and PA/Lateral spine films. There was no correlation with DXA severity and RANKL levels although the sample group was too small to perform any further analysis. There was no significant difference in RANKL levels in those with vertebral fractures compared with those without. Again, trends may have been difficult to assess due to small sample size.
There were limitations to our study. There is inadequate data on stability of RANKL or variation in secretion so random sampling may not be adequate to determine maximum free soluble ligand levels. In addition, other factors that influence bone resorption and could potentially influence RANKL levels such as PTH, Vitamin D status, and systemic cytokines were not evaluated. Other bone turnover markers such as C-telopeptide and N-telopeptide were also not obtained for comparison. Correlation of RANKL levels with duration of glucocorticoid therapy and non-ambulation was not examined due to difficulty obtaining clear duration from chart review as some patients had transferred care from other institutions and others took self-directed drug holidays. Pubertal status was also not analyzed and may have confounded the downward trend of RANKL, OPG, and RANKL:OPG with age given the known pubertal delay in DMD patients.
Lastly, BMD evaluation was only performed in a small subset of the DMD cohort due to insurance authorization issues. Height-adjusted Z-scores were not used due to inconsistent height measurements in the DMD patients. This may be inadequate in DMD patients with short stature as it can falsely lower their Z-score in comparison with healthy peers of normal height [14]. Thus, height-adjusted Z-score would have been more accurate in this patient population. Additional factors that affect BMD measurement in DMD patients include scoliosis, often requiring corrective hardware, as well as vertebral compression fractures which can artefactually elevate the BMD value for the affected vertebra [17]. Hence, arm span may be used as a surrogate for height measurement in future studies.
Conclusion
Our study is the first to report a significant decline in RANKL, OPG, and RANKL:OPG with age in DMD patients compared with healthy controls. This trend suggests some bone turnover markers may be difficult to assess as well as use as therapeutic indicators in DMD patients. In addition, there was significant difference in the 6-–10-year DMD subset compared with age-matched controls. Additional larger studies are needed to evaluate the role of RANKL-OPG in the bone phenotype of DMD patients to provide better targeted therapy for these patients.
References
Flanigan KM (2012) The muscular dystrophies. Semin Neurol 32(3):255–263
Balaban B, Matthews DJ, Clayton GH, Carry T (2005) Corticosteroid treatment and functional improvement in Duchenne muscular dystrophy: long-term effect. Am J Phys Med Rehabil 84(11):843–850
Yilmaz O, Karaduman A, Topaloglu H (2004) Prednisolone therapy in Duchenne muscular dystrophy prolongs ambulation and prevents scoliosis. Eur J Neurol 11(8):541–544
Birnkrant DJ, Bushby K, Bann CM, Alman BA, Apkon SD, Blackwell A, Case LE, Cripe L, Hadjiyannakis S, Olson AK, Sheehan DW, Bolen J, Weber DR, Ward LM (2018) Diagnosis and management of Duchenne muscular dystrophy, part 2: respiratory, cardiac, bone health, and orthopaedic management. Lancet Neurol 17(4):347–361
Tian C, Wong B, Hornung L, Khoury J, Miller L, Bange J, Rybalsky I, Rutter M (2014) Age-specific prevalence of osteoporosis and frequency of poor bone health indices in Duchenne muscular dystrophy. Neuromuscul Disord 24(9–10):857
Boyce BF, Xing L (2007) The RANKL/RANK/OPG pathway. Curr Osteoporos Rep 5(3):98–104
Boyce BF, Xing L (2008) Functions of RANKL/RANK/OPG in bone modeling and remodeling. Arch Biochem Biophys 473(2):139–146
Boyce BF, Xing L (2007) Biology of RANK, RANKL, and osteoprotegerin. Arthritis Res Ther 9(Suppl 1):S1
Rouster-Stevens KA, Langman CB, Price HE, Seshadri R, Shore RM, Abbott K, Pachman LM (2007) RANKL:osteoprotegerin ratio and bone mineral density in children with untreated juvenile dermatomyositis. Arthritis Rheum 56(3):977–983
Lien G, Ueland T, Godang K, Selvaag AM, Forre OT, Flato B (2010) Serum levels of osteoprotegerin and receptor activator of nuclear factor -kappaB ligand in children with early juvenile idiopathic arthritis: a 2-year prospective controlled study. Pediatr Rheumatol Online J 8:30
Tsentidis C, Gourgiotis D, Kossiva L, Doulgeraki A, Marmarinos A, Galli-Tsinopoulou A, Karavanaki K (2016) Higher levels of s-RANKL and osteoprotegerin in children and adolescents with type 1 diabetes mellitus may indicate increased osteoclast signaling and predisposition to lower bone mass: a multivariate cross-sectional analysis. Osteoporos Int 27(4):1631–1643
Wasilewska A, Rybi-Szuminska A, Zoch-Zwierz W (2010) Serum RANKL, osteoprotegerin (OPG), and RANKL/OPG ratio in nephrotic children. Pediatr Nephrol 25(10):2067–2075
Olney RC, Permuy JW, Prickett TC, Han JC, Espiner EA (2012) Amino-terminal propeptide of C-type natriuretic peptide (NTproCNP) predicts height velocity in healthy children. Clin Endocrinol 77(3):416–422
Crabtree NJ, Arabi A, Bachrach LK, Fewtrell M, El-Hajj Fuleihan G, Kecskemethy HH, Jaworski M, Gordon CM (2014) Dual-energy X-ray absorptiometry interpretation and reporting in children and adolescents: the revised 2013 ISCD pediatric official positions. J Clin Densitom 17(2):225–242
Rufo A, Del Fattore A, Capulli M, Carvello F, De Pasquale L, Ferrari S, Pierroz D, Morandi L, De Simone M, Rucci N, Bertini E, Bianchi ML, De Benedetti F, Teti A (2011) Mechanisms inducing low bone density in Duchenne muscular dystrophy in mice and humans. J Bone Miner Res 26(8):1891–1903
Nakagaki WR, Bertran CA, Matsumura CY, Santo-Neto H, Camilli JA (2011) Mechanical, biochemical and morphometric alterations in the femur of mdx mice. Bone 48(2):372–379
Fewtrell MS (2003) Bone densitometry in children assessed by dual x ray absorptiometry: uses and pitfalls. Arch Dis Child 88(9):795–798
Funding
This study was funded by Parent Project Muscular Dystrophy, The Growth and Bone Foundation at Children’s Hospital Los Angeles, and The Skirball Fellowship Research Award at the Children’s Hospital Los Angeles.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Pisit Pitukcheewanont had research funding from Ultragenyx, Amgen, and Shire; salary from Ascendis Pharma. Anna Ryabets-Lienhard has research funding from Ultragenyx, Amgen, and Shire. The remaining authors have nothing to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee. Informed consent was obtained for all subjects.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Akhtar Ali, S., Kang, H., Olney, R. et al. Evaluating RANKL and OPG levels in patients with Duchenne muscular dystrophy. Osteoporos Int 30, 2283–2288 (2019). https://doi.org/10.1007/s00198-019-05077-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-019-05077-5