Abstract
Summary
We analyzed women and newborn outcome after maternal exposure to BPs. BPs have no teratogenic effect on the 36 analyzed pregnancies compared to unexposed controls matched on women underlying diseases (either systemic disease, either “bone” disease) but some outcome differed: neonatal complications rate in systemic diseases and live birth rate in bone diseases).
Introduction
The effect of bisphosphonates (BPs) during pregnancy remains unclear. We aimed to study pregnancy outcomes in women exposed to BPs during pregnancy.
Methods
Data for cases and controls were from the French Reference Centre of Teratogenic Agents. Cases were women who received BPs in the 6 weeks before or during a pregnancy and had systemic or bone diseases. We included two respectively matched control groups: women with systemic diseases not exposed to BPs and healthy women not exposed to BPs or any teratogenic agent. Four controls were assigned to each case.
Results
Thirty-six women were exposed to BPs including 5 just before pregnancy and 30 during the first trimester; 23 had systemic diseases (systemic lupus erythematosus, n = 5; rheumatoid arthritis, n = 5; other, n = 13) and 13 had bone diseases. Rate of observed congenital malformations did not differ in women with a systemic or a bone disease compared to their respective controls (respectively 2/23 [8.7%] vs 2/92 [2.2%], p = 0.178 and 0/13 [0%] vs 0/52 [0%], p = 1.00). Among women with systemic diseases, non-specific neonatal complications were more frequent for cases (4/16 [25.0%] vs 4/64 [6.3%], p = 0.027). Among women with bone disorders, the live birth rate was lower for cases than healthy controls (8/10 [80%] vs 50/50 [100%], p = 0.025).
Conclusion
We found no major teratogenic effects of BPs, but rates of neonatal complications were increased for women with systemic diseases, as were spontaneous abortions for women with bone diseases likely linked to the severity of the underlying diseases and concomitant medications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bisphosphonates (BPs) are the most widely used agents in the current pharmacological arsenal against osteoclast-mediated bone loss [1]. Their main indications are osteoporosis and malignancies, including bone metastasis, multiple myeloma, or malignant hypercalcemia. Although these conditions mainly affect older people, BPs can be used in young women of childbearing age. BPs are indicated in the treatment of corticosteroid-induced osteoporosis, which could affect young people with systemic diseases [2, 3]. They are also commonly prescribed for preventing and treating various other rare skeletal conditions, such as fibrodysplasia; low bone density linked, for example, to anorexia nervosa; and osteogenesis imperfect [4].
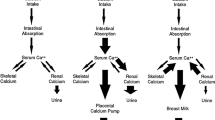
A critical pharmacological characteristic of BPs is their extremely high affinity for bone tissues. BPs bind with very high affinity to hydroxyapatite crystals, and thus bone mineral with this strong affinity, BPs can achieve a high local concentration throughout the entire skeleton [5]. However, the skeletal retention depends on the availability of hydroxyapatite binding sites. BPs are preferentially incorporated into sites of active bone remodeling or turnover [6].
After administration, part of the BPs that does not bind bone tissue is rapidly cleared from the circulation by renal excretion, and the remaining part is retained in the skeleton and slowly released. The duration of bone turn-over suppression and BP release is largely a function of the BP’s avidity for mineral matrix binding. The most potent BP, zoledronic acid, effectively suppresses biochemical markers of bone resorption for up to 1 year in women with postmenopausal osteoporosis [7]. Nevertheless, the precise biologic half-lives of the currently used BPs remain debated, largely because of technical challenges required to determine BP levels in urine and serum. Estimates for alendronate suggest a half-life of more than 10 years after a single intravenous administration [8], and for pamidronate, urinary excretion could be detected up to 8 years after administration [9]. In addition, low-molecular-weight BPs such as alendronate have shown placental transfer in rats [10] and in humans, with a possible fetal uptake [11].
Therefore, with all these elements—long half-life, placental transfer, and high affinity for high-turnover bones (including fetal skeleton)—fetuses of women exposed to BPs in the months before or during pregnancy might be significantly exposed to BPs. In animal studies, BPs showed a teratogenic effect. In rats exposed to BPs during pregnancy, fetuses showed reduced fetal weight and abnormal diaphyseal bone structure [10] and tooth development (with high-dose BPs) [12]. Moreover, rats in one study showed maternal hypocalcemia and parturition problems [13].
These data are worrisome for the use BPs in women of childbearing age because the drugs may affect a current or later pregnancy due to their long-term bone retention and release. Moreover, long-term effects of in-utero exposure to BPs have never been studied. For these reasons, BPs are contraindicated in pregnant women and used with caution in women of childbearing age. However, almost half of pregnancies are not planned; thus, a pregnancy in a young woman who took BPs is a rare event but may occur.
Only scarce human data are available in the literature and are difficult to interpret. Only two limited-size case/control study were published (including respectively 21 and 24 pregnant women), and the lack of disease-matched controls limits the interpretation of the former [14, 15]. Other data came mainly from multiple case reports and thus do not allow any comparison. In 2011, Stathopoulos et al. collected 78 cases of the literature (including the two abovementioned case control studies) and cannot formally exclude any effect on gestational age, birth weight, hypocalcemia, spontaneous abortion, or malformation, due to the absence of appropriate controls [16].
In total, little is known about the effects of BPs on fetuses and fetal development, particularly skeletal development. This study used data from the French Reference Centre of Teratogenic Agents to compare pregnancy and newborn outcomes in women exposed and not exposed to BPs during or in the months before pregnancy.
Patients and methods
Patients
Data for cases and controls were collected from the French Reference Centre of Teratogenic Agents (Centre de Référence sur les Agents Tératogènes [CRAT], www.lecrat.fr) database. This reference center provides advice and recommendations, based on the most updated current knowledge, to practitioners and patients about the potential teratogenic, fetotoxic, or neonatal risks of exposure to any medication during pregnancy and breastfeeding. Practitioners can contact this center for advice regarding any medical exposure of uncertain effect during pregnancy. Since 1975, and using a standard form, the CRAT database has collected cases of exposure to any medications during pregnancy for which it has been contacted, generally in the early stages of pregnancy, for advice about the risks of this exposure on the ongoing pregnancy. Then, until the post-partum period, the form is prospectively completed with information about drug discontinuation, obstetrical complications, pregnancy outcome, and newborn characteristics. More than 62,000 cases are included in the database.
Cases
Cases in the CRAT database were women who had been exposed to BPs during pregnancy or within the 6 weeks before pregnancy. All BPs were included. Because the underlying disease might affect the pregnancy outcome, cases were divided into two groups: (1) “systemic disease cases,” including women with systemic diseases treated with BPs mainly for corticosteroid-induced osteoporosis and (2) “bone disease cases,” including women without any systemic disease and receiving BPs for primary non-malignant bone diseases. Women with malignant bone lesions exposed to BPs were excluded because they received other teratogenic or abortive agents.
Controls
Controls in the CRAT database were women who had never been exposed to BPs. As for cases, two groups were defined, and four controls were matched to each case: (1) The first control group was “systemic disease controls,” including women with systemic diseases identified in the CRAT database by the following keywords: systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), and anti-phospholipid syndrome (APS). These controls were matched to cases according to the underlying disease when possible, but the selection process was blinded to all other characteristics and other drug exposures. (2) Since it was not possible to find a control group of pregnant women with non-malignant bone diseases not exposed to BPs, the second control group consisted of “healthy controls” who were randomly chosen. These patients were healthy pregnant women registered in the CRAT database who did not have any underlying disease but who contacted the CRAT because of exposure to drugs for which the absence of a teratogenic effect is clearly established in the literature.
Data collection
The following maternal characteristics were recorded: age, obstetric history, and underlying and any maternal diseases. For BP exposure, data on the drug compound, indication, dosage, route of administration, duration of treatment, and timing of exposure during pregnancy were collected. Exposure to all other medications, including dosage, route of administration, and duration, were also recorded.
Data on pregnancy outcomes and newborn characteristics were collected at birth or during the first 2 months of life. In case of spontaneous abortion or early pregnancy termination (voluntary or for medical reasons), fetopathological data (if available) were collected. For live births, data on gestational age, birth size and weight, occurrence, and type of neonatal complication or congenital malformation were collected.
Statistical analyses
Data are described as number (percentage) and median and interquartile range [IQR]. Characteristics of women and pregnancies were compared between cases and controls. Systemic disease cases were compared to systemic disease controls and bone disease cases to healthy controls. Quantitative variables were compared by the non-parametric Mann-Whitney test, and qualitative variables were compared bychi-square test or Fisher’s exact test. Statistical analysis involved use of R-Cran statistical software. p < 0.05 was considered statistically significant.
Results
Characteristics of cases and controls
Between 1987 and 2014, 39 women exposed to BPs were recorded in the CRAT database, including 3 with hypercalcemia related to neoplasia, who were excluded. Thus, data for 36 exposed women were analyzed. At the time of pregnancy, the median age was 32 years [IQR 27–36] and 7 BP-exposed patients (19.4%) were primiparous.
Among the exposed women, 23 had a systemic inflammatory disease, including SLE in 5 (1 with associated APS), RA in 5, isolated APS in 1, systemic vasculitis in 6 (Behçet disease, n = 3; Takayasu’s disease, n = 2; and polyarteritis nodosa, n = 1), and other inflammatory diseases in 6 (Crohn’s disease, n = 2; systemic sclerosis, Still’s disease, pemphigus, and multiple sclerosis, n = 1 each) (Table 1).
Compared to the 92 controls with systemic inflammatory disorders but not exposed to BPs, the 23 systemic disease cases did not differ in age or previous obstetrical history (Table 1). Controls had various systemic diseases, including SLE (n = 40), RA (n = 24), SLE + APS (n = 11), APS alone (n = 1), systemic vasculitis (n = 3: Behcet disease, n = 1; vasculitis with granuloma, n = 2), and other inflammatory diseases (n = 13: cryopyrin-associated periodic syndrome, sarcoidosis, non-specified connective tissue disease, and Sjögren’s syndrome, n = 2 each; Crohn’s disease, juvenile inflammatory arthritis, n = 1 each; systemic sclerosis, n = 3).
The 13 cases with bone diseases had heterogeneous bone disorders: osteoporosis (n = 9, including steroid-induced osteoporosis in patients with asthma, n = 2; Cushing disease, n = 1), pheochromocytoma (n = 1), and other benign disorders (n = 4: fibrodysplasia, osteogenesis imperfecta, algodystrophy, hyperparathyroidism with hypercalcemia, n = 1 each). The women exposed to Bps were significantly older than the 52 healthy controls (36 vs 32 years; p = 0.034).
Drug exposure
BP exposure
Among the 36 cases exposed to BPs, 5 (13.8%) were exposed within the 6 weeks before pregnancy and 31 (86.1%) during pregnancy, mainly during the first trimester (30/31, 96.8%). All 23 cases with systemic disease received oral BPs: risedronate in 15 (65.2%), alendronate in 6 (26.1%), and etidronate and unknown in 1 each (Table 1). BP was prescribed to prevent or treat corticosteroid-induced osteoporosis in all cases. For the 13 cases with bone disease, BPs were alendronate for 9 (69.2%), pamidronate for 2 (15.4%), and etidronate, ibandronate, and risedronate for 1 each (Table 2). One patient received both etidronate and alendronate. Three patients (23.1%) received intravenous BPs (pamidronate, n = 2; ibandronate, n = 1).
Concomitant drug exposure
Among women with systemic disease, as compared with the 92 controls (Table 1), cases more frequently received steroids, methotrexate, colchicine, proton pump inhibitors, and sex hormones but less frequently anti-malarial drugs (p = 0.019) (Table 1). These differences were probably linked to a higher proportion of RA among cases and SLE among controls. Several cases and controls received teratogenic medications, but with no significant differences between the two groups. These drugs were cyclophosphamide (p = 0.491), vitamin K antagonist (p = 0.691), beta-blockers (p = 1.00), angiotensin-converting enzyme inhibitors (p = 0.142), and mycophenolate mofetil (p = 0.345). After patients contacted the CRAT for advice on exposures and recommendations, all teratogenic medications were stopped.
Pregnancy and newborn outcomes
Women with systemic disease
The frequency of voluntary interruption of pregnancies did not significantly differ between cases and controls (2/23 [8.7%] vs 11/92 [12.0%]; p = 0.703), but the rate of therapeutic terminations of pregnancies was higher for cases than controls (4/23 [17.4%] vs 1/92 [1.1%], p = 0.006; Table 1). Cases and controls did not differ when analyzing therapeutic or voluntary pregnancy termination together (6/23 [26.1%] vs 12/92 [13.0%], p = 0.195).
With BP exposure, two therapeutic abortions were decided for severe maternal conditions and two for fetal reasons (potential risk of malformation linked to methotrexate exposure but no malformation observed, and polymalformative syndrome detected on ultrasound, n = 1 each). Among the remaining pregnancies, cases (n = 17) and controls (n = 80) did not differ in the rate of spontaneous abortions (1/17 [5.9%] vs 15/80 [18.8%], p = 0.290) or in utero-fetal deaths (0/17 [0%] vs 1/80 [1.3%], p = 1.00), which resulted in a comparable live birth rate (16/17 [94.1%] vs 64/80 [80.0%], p = 0.291). Cases and controls did not differ in infant birth weight, length, or gestational age at birth (Table 1).
For live births, cases and controls did not differ in rate of congenital malformations (1/16 [6.3%] vs 1/64 [1.6%], p = 0.276) and did not differ when including fetuses with fetopathological data available (cases, n = 2; controls, n = 3; 2/18 [11.1%] vs 2/67 [3.1%], p = 0.196). Finally, both malformations occurred in a fetus whose mother was exposed to BPs during the first trimester (all women in this group were exposed before pregnancy or during the first trimester, during the at risk period). The two malformations in infants from women exposed to BPs were polymalformative syndromes (Table 3). The first one (systemic disease case no. 1) was premature (26 weeks of amenorrhea) and had malformations known to be associated with prematurity [17,18,19]. The second one (systemic disease case no. 2) had malformations evocative of mycophenolate mofetil exposure syndrome [20]. Cases and controls did not differ in cesarean section rate (5/16 [31.3%] vs 22/64 [34.3%], p = 1.00), but the rate of neonatal complications was higher for cases than controls (4/16 [25.0%] vs 4/64 [6.3%] p = 0.027). These complications were various and none could be specifically linked to BPs (Table 4). Notably, no neonatal hypocalcemia was observed.
Women with bone disease and healthy controls
The rate of voluntary pregnancy interruptions was higher for women with non-malignant bone diseases than controls (3/13 [23.1%] vs 1/52 [1.9%], p = 0.023) (Table 2), and one therapeutic pregnancy termination occurred in the control group. When analyzing therapeutic or voluntary pregnancy termination, the differences were no longer significant (3/13 [23.1%] vs 2/52 [3.8%], p = 0.051). However, among the remaining 10 BP-exposed cases and 50 controls, spontaneous abortions were more frequent among cases than controls (2/10 [20%] vs 0/50 [0%], p = 0.025), which resulted in a significantly lower birth rate in cases than controls (8/10 [80%] vs 50/50 [100%], p = 0.025). The birth rate did not differ by intravenous or oral BP administration (2/3 [66.7%] vs 6/7 [85.7%], p = 1.0). For the live births, cases and controls did not differ in infant birth weight, length, or gestational age at birth. No congenital malformation was observed. In both group, no unborn underwent fetopathological examination. Cases and controls did not differ in rate of neonatal complications (1/10 [10%] vs 5/50 [10%], p = 1.00). No neonatal hypocalcemia was observed.
Discussion
This study is the largest focusing on the outcome of pregnancies and newborns for mothers exposed to BPs. We found no major teratogenic effect of BPs and no effect on fetal growth, weight, or gestational age at birth. However, we found an increased rate of spontaneous abortions in women exposed to BPs for bone diseases and an increased rate of non-specific neonatal complications for exposed women with systemic diseases. Nevertheless, in both cases, these differences could be explained by the underlying disease and associated medications.
Regarding the increased rate of spontaneous abortions in the bone disease group, cases were compared to healthy controls and the rate of spontaneous abortion observed in the control group (0%) was lower than the expected rate, approximatively 12% in the general population in France [21]. Finally, the increased rate of spontaneous abortion found in the bone disease group may be due to causes other than BP exposure. One abortion occurred in a 40-year-old patient with very severe asthma that required long-term medium- to high-dose steroids. Abortion occurred between 5 and 6 weeks of amenorrhea. The second occurred in a36-year-old patient with a history of pheochromocytoma at 9 weeks of amenorrhea. Age may also have favored these spontaneous abortions. Nevertheless, we could not exclude a possible role of BPs, because a higher rate of spontaneous abortion was previously found in women exposed to alendronate than controls (20.8 vs 7%) in a study of 24 patients with systemic and bone diseases [15]. However, we found no difference when comparing the rate of live births between systemic disease cases and controls, both groups being exposed to various agents.
As in two previous series [14, 15], we did not find an increased risk of teratogenic effect of BPs. Nevertheless, the literature contains some reports of congenital malformations, and Stathopoulos et al. found a total of three malformations among the 78 reported cases in the literature [16, 22, 23], and we here report two additional cases. However, in the literature, as in our cases, each malformation or polymalformative syndrome was different, which does not suggest any typical malformative pattern associated with exposure to BPs. Also, the prescription of BPs in women of childbearing age is frequently linked to a disease that requires the prescription of other medications, many of them teratogenic. For example, in the present study, the most severe polymalformative syndrome was related to exposure to mycophenolate. We also observed advanced bone maturation in one fetus. However, this finding should be interpreted with caution because it occurred in the fetus exposed to mycophenolate mofetil also and has never been described before, in exposed fetuses nor in children receiving BPs [24, 25].
In contrast to one study showing reduced birth weight and birth term in patients exposed to BPs [15], our study provides reassuring data on newborn characteristics and outcomes, with no difference in birth weight, length, and gestational age between cases and controls. These reassuring results agree with the Levy et al. study [14] that compared women exposed to BPs and controls not exposed to BPs or any teratogenic agents. However, this previous study did not provide any data on the underlying diseases and the reasons for prescription of BPs for comparison to our results.
Finally, we found a higher rate of non-specific neonatal complications in systemic disease cases. This finding was not reported in the only previous study that analyzed neonatal complications [14]. However, in this group, BPs were mainly prescribed for prevention of steroid-induced osteoporosis. Thus, women receiving BPs were more likely to require steroids for a more severe or active disease and therefore were at increased risk of neonatal complications due to their underlying systemic disease or their steroid exposure. Finally, the nature and heterogeneity of the observed neonatal complications did not indicate a clear imputability of BPs in their occurrence. Also, we did not observe any case of neonatal hypocalcemia, but exposure to BPs in the third trimester of pregnancy was rather infrequent (only 4 cases). In addition, this complication was previously described in patients exposed to BPs after an important accumulation of exposure or at later stages of pregnancy [23, 26, 27]. Thus, this complication should be monitored in newborns in cases of late maternal exposure during pregnancy.
The strengths of the present study are the systematic and standardized prospective follow-up of pregnancies registered in the CRAT database and the use of specific control groups for each type of indication of BPs, which has never been done before. This was particularly true for women with systemic diseases, who are clearly exposed to increased risk of complications due to their underlying diseases. Also to our knowledge, the number of included patients is one of the largest in the literature. However, weaknesses include the heterogeneity of BP indications, especially in the non-malignant bone disease group, including disorders of various severity. Moreover, this group was compared to healthy controls, which were perhaps not the best control, but we were unable to find some women with such diseases untreated. Also, for patients with systemic disorders, data on the activity of the underlying disease was not available, so we could not exclude a heterogeneity in disease severity among cases and control group. However, we had detailed information about the associated medications which was key for the evaluation of the risk of malformation and could also be considered as a surrogate marker of disease severity.
To conclude, this study provides some reassuring data on pregnancies exposed to BPs with no major teratogenic effects. However, we observed a higher rate of non-specific neonatal complications among women with systemic diseases and spontaneous abortion among those with bone diseases. Nevertheless, these complications were probably mainly due to the severity of the underlying diseases and other concomitant medications. Thus, even if BPs cannot be recommended in pregnant women, exposed women of childbearing age should be informed and reasonably reassured. Future studies, focusing on the outcome of children exposed in utero to such agents would be of great interest to analyze their long-term potential impact on growth and skeletal maturation.
References
Minisola S, Pepe J, Piemonte S, Cipriani C (2015) The diagnosis and management of hypercalcaemia. BMJ 350:h2723
Rizzoli R, Biver E (2014) Glucocorticoid-induced osteoporosis: who to treat with what agent? Nat Rev Rheumatol 11(2):98–109
Grossman JM, Gordon R, Ranganath VK, Deal C, Caplan L, Chen W, Curtis JR, Furst DE, McMahon M, Patkar NM, Volkmann E, Saag KG (2010) American College of Rheumatology 2010 recommendations for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Care Res 62(11):1515–1526
Mäkitie AA, Törnwall J, Mäkitie O (2008) Bisphosphonate treatment in craniofacial fibrous dysplasia—a case report and review of the literature. Clin Rheumatol 27(6):809–812
Drake MT, Clarke BL, Khosla S (2008) Bisphosphonates: mechanism of action and role in clinical practice. In: Mayo Clinic proceedings. Elsevier, pp 1032–1045
Lin JH, Duggan DE, Chen I-W, Ellsworth RL (1991) Physiological disposition of alendronate, a potent anti-osteolytic bisphosphonate, in laboratory animals. Drug Metab Dispos 19(5):926–932
Black DM, Delmas PD, Eastell R, Reid IR, Boonen S, Cauley JA, Cosman F, Lakatos P, Leung PC, Man Z, Mautalen C, Mesenbrink P, Hu H, Caminis J, Tong K, Rosario-Jansen T, Krasnow J, Hue TF, Sellmeyer D, Eriksen EF, Cummings SR, HORIZON Pivotal Fracture Trial (2007) Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med 356(18):1809–1822
Khan SA, Kanis JA, Vasikaran S, Kline WF, Matuszewski BK, McCloskey EV, Beneton MNC, Gertz BJ, Sciberras DG, Holland SD, Orgee J, Coombes GM, Rogers SR, Porras AG (1997) Elimination and biochemical responses to intravenous alendronate in postmenopausal osteoporosis. J Bone Miner Res 12(10):1700–1707
Papapoulos SE, Cremers SCLM (2007) Prolonged bisphosphonate release after treatment in children. N Engl J Med 356(10):1075–1076
Patlas N, Golomb G, Yaffe P, Pinto T, Breuer E, Ornoy A (1999) Transplacental effects of bisphosphonates on fetal skeletal ossification and mineralization in rats. Teratology 60(2):68–73
McKenzie AF, Budd RS, Yang C, Shapiro B, Hicks RJ (1994) Technetium-99m-methylene diphosphonate uptake in the fetal skeleton at 30 weeks gestation. J Nucl Med 35(8):1338–1341
Okazaki A, Matsuzawa T, Takeda M et al (1995) Intravenous reproductive and developmental toxicity studies of cimadronate (YM175), a novel bisphosphonate, in rats and rabbits. J Toxicol Sci 20(SupplementI):1–13
Minsker DH, Manson JM, Peter CP (1993) Effects of the bisphosphonate, alendronate, on parturition in the rat. Toxicol Appl Pharmacol 121(2):217–223
Levy S, Fayez I, Taguchi N, Han JY, Aiello J, Matsui D, Moretti M, Koren G, Ito S (2009) Pregnancy outcome following in utero exposure to bisphosphonates. Bone 44(3):428–430
Ornoy A, Wajnberg R, Diav-Citrin O (2006 Nov) The outcome of pregnancy following pre-pregnancy or early pregnancy alendronate treatment. Reprod Toxicol 22(4):578–579
Ioannis SP, Chrysoula LG, Aikaterini K, George T, George LP, Nikolaos PA, Symeon T (2011) The use of bisphosphonates in women prior to or during pregnancy and lactation. Hormones 10(4):280–291
Boocock GR, Todd PJ (1985) Inguinal hernias are common in preterm infants. Arch Dis Child 60(7):669–670
Wroblewska-Seniuk K, Chojnacka K, Pucher B, Szczapa J, Gadzinowski J, Grzegorowski M (2005) The results of newborn hearing screening by means of transient evoked otoacoustic emissions. Int J Pediatr Otorhinolaryngol 69(10):1351–1357
J Vettukattil J (2016) Pathophysiology of patent ductus arteriosus in the preterm infant. Curr Pediatr Rev 12(2):120–122
Perez-Aytes A, Marin-Reina P, Boso V, Ledo A, Carey JC, Vento M (2017) Mycophenolate mofetil embryopathy: a newly recognized teratogenic syndrome. Eur J Med Genet 60(1):16–21
Delabaere A, Huchon C, Deffieux X, Beucher G, Gallot V, Nedellec S, Vialard F, Carcopino X, Quibel T, Subtil D, Barasinski C, Gallot D, Vendittelli F, Laurichesse-Delmas H, Lémery D (2014) Epidemiology of loss pregnancy. J Gynecol Obstet Biol Reprod (Paris) 43(10):764–775
Losada I, Sartori L, Di Gianantonio E, Zen M, Clementi M, Doria A (2010) Bisphosphonates in patients with autoimmune rheumatic diseases: can they be used in women of childbearing age? Autoimmun Rev 9(8):547–552
Munns CF, Rauch F, Ward L, Glorieux FH (2004) Maternal and fetal outcome after long-term pamidronate treatment before conception: a report of two cases. J Bone Miner Res 19(10):1742–1745
Castillo H, Samson-Fang L (2009) Effects of bisphosphonates in children with osteogenesis imperfecta: an AACPDM systematic review. Dev Med Child Neurol 51(1):17–29
Chan B, Zacharin M (2006) Maternal and infant outcome after pamidronate treatment of polyostotic fibrous dysplasia and osteogenesis imperfecta before conception: a report of four cases. J Clin Endocrinol Metab 91(6):2017–2020
Hassen-Zrour S, Korbaa W, Béjia I, Saidani Z, Bergaoui N (2010) Maternal and fetal outcome after long-term bisphosphonate exposure before conception. Osteoporos Int 21(4):709–710
Dunlop DJ, Soukop M, McEwan HP (1990) Antenatal administration of aminopropylidene diphosphonate. Ann Rheum Dis 49(11):955
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Aurélien Sokal, Tifenn Leturcq, Delphine Beghin, and Xavier Mariette declare that they have no conflict of interest.
Raphaele Seror received consulting fees from Roche and Novartis.
Rights and permissions
About this article
Cite this article
Sokal, A., Elefant, E., Leturcq, T. et al. Pregnancy and newborn outcomes after exposure to bisphosphonates: a case-control study. Osteoporos Int 30, 221–229 (2019). https://doi.org/10.1007/s00198-018-4672-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-018-4672-9