Abstract
Summary
Tooth extraction in patients receiving bisphosphonates is thought to be a risk factor for osteonecrosis of the jaw (ONJ); however, ONJ did not develop, even when tooth extraction was performed with continued oral bisphosphonate therapy. A drug holiday from bisphosphonates before tooth extraction may not be necessary.
Introduction
It is controversial whether bisphosphonate withdrawal is necessary prior to invasive procedures such as tooth extraction in order to prevent bisphosphonate-related osteonecrosis of the jaw (BRONJ). This study aimed to evaluate the clinical safety of continuing oral bisphosphonate therapy in patients undergoing tooth extraction.
Methods
We prospectively enrolled 132 patients (20 men, 112 women) who were receiving oral bisphosphonates for the prevention or treatment of osteoporosis and required tooth extraction. All patients were managed using an identical protocol, which included preoperative antibiotic prophylaxis and did not necessarily require complete wound closure. The patients were classified into groups according to the duration of bisphosphonate administration: < 2 years (n = 51), 2–5 years (n = 41), 5–10 years (n = 28), and > 10 years (n = 12). The groups were compared regarding the time taken for the extraction socket to heal, and the occurrence of BRONJ. Follow-up duration was at least 3 months.
Results
A total of 274 teeth were removed. Long-term oral bisphosphonate therapy for > 5 years significantly delayed the healing of the extraction socket in comparison with administration for < 5 years; however, BRONJ did not develop in any group. There was no prolongation of wound healing due to systemic risk factors such as glucocorticoid administration and diabetes mellitus. There were no adverse skeletal events such as bone fracture.
Conclusions
Patients who underwent tooth extraction with continued oral bisphosphonate therapy showed delayed healing of the extraction socket as the cumulative administration period prolonged, but BRONJ did not develop.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is characterized by low bone mass, deterioration of bone tissue, and resultant bone fragility [1]. In Japan, osteoporosis affects more than 13 million people [2]. Osteoporosis is the most common cause of fracture in older adults and leads to an increased risk of hip fractures [3]. Hip fractures markedly increase the mortality rate, reduce independence, and impair the ability to walk and perform activities of daily living, seriously reducing the health-related quality of life [4, 5]. Hence, it is important to prevent hip fractures, and the key drugs used to accomplish this are bisphosphonates (BP). BP inhibit bone resorption through induction of osteoclast apoptosis and are used for the treatment of many bone diseases, including osteoporosis, bone metastasis of malignant tumors, and multiple myeloma [6,7,8].
One serious complication associated with BP administration is osteonecrosis of the jaw (ONJ). The first case reports that described the relationship between high-dose intravenous BP and the incidence of ONJ in cancer patients were published in 2003 [9]. In 2004, Ruggiero et al. reported the relationship between oral BP in osteoporotic patients and the incidence of refractory osteomyelitis [10]. These two conditions (ONJ and refractory osteomyelitis) were considered to be the same BP-associated disease, which was termed bisphosphonate-related ONJ (BRONJ). Newer approaches to dental issues and treatment of BRONJ showed reduced incidence and severity, but BRONJ may still adversely affects quality of life and produces substantial morbidity [11]. The incidence of BRONJ in osteoporotic patients reportedly ranges from 0.001–0.15% [12]. In particular, the risk of BRONJ may be higher in Asia than in other regions [13]. Although gradual progress has been made toward the elucidation of the etiopathology and associated risk factors for BRONJ, definite preventive strategies have not yet been established.
One factor generally considered to increase the risk of BRONJ development is dentoalveolar surgery such as tooth extraction [14, 15]. The relative risk of BRONJ after tooth extraction in patients with cancer who are receiving BP is reportedly 16–50 times higher than in patients receiving BP who have not undergone tooth extraction [14, 16, 17]. Although the incidence of BRONJ in patients receiving oral BP following tooth extraction was reportedly only 0.5% in 2009 [18], this incidence has increased during the past 5 years; recent studies have reported higher incidences, including 2.27% in 2013 [19], 2.5% in 2013 [20], and 3.44% in 2017 [21]. In Japan, a retrospective study published in 2017 reported that the incidence of BRONJ after tooth extraction was 3.0% (35 of 1175 cases, 41 of 2458 teeth) [22].
A drug holiday before tooth extraction is often performed as a precautionary measure to minimize the influence of BP on the development of BRONJ [11, 23]. However, Taguchi et al. suggested that discontinuation of BP therapy may not prevent BRONJ, and may increase adverse events and lead to interruption of osteoporosis treatment [24]. When a drug holiday is discussed, patients may refuse BP administration due to the fear of BRONJ. If a drug holiday is not necessary, continued BP therapy is desirable to prevent adverse skeletal events such as bone fracture. It is also greatly beneficial to treat any dental infection that may have occurred during the drug holiday period.
Most previous studies investigating the relationship between tooth extraction and development of BRONJ are retrospective [22, 25]. Mozzati et al. performed a prospective study of tooth extraction in osteoporotic patients, but did not specify whether BP therapy was continued at the time of tooth extraction [26]. Therefore, the present study prospectively examined the clinical course after tooth extraction with continued BP therapy before and after the procedure in patients receiving oral BP. We hypothesized that BRONJ would not develop after tooth extraction in patients receiving oral BP before and after the procedure.
Methods
The present study was approved by the Independent Ethics Committee of the Hyogo College of Medicine (approval number: 1702) and was performed in accordance with the standards of the Declaration of Helsinki. All patients provided written informed consent before study commencement.
Between September 2014 and May 2017, 132 patients receiving oral BP were prospectively enrolled in the present study. Inclusion criteria were men or women aged over 40 years who were currently receiving BP therapy for the prevention or treatment of osteoporosis, oral BP therapy had been administered for at least 1 month, dental assessment determined that one or more teeth required extraction, consent provided for tooth extraction with continued BP therapy, and follow-up observation for 3 months or longer at our department or at a local dental clinic where we could confirm the clinical course. Exclusion criteria were cancer, intravenous BP administration, patients previously treated with BP (including those who were withdrawn by switching to other osteoporosis drugs not classified as antiresorptive agents such as teriparatide), BRONJ already developing at the time of tooth extraction, previous head and neck radiotherapy, and obvious metastatic disease of the jaw. The patients were divided into four groups in accordance with the duration of oral BP administration: group I had received BP for less than 2 years (n = 51 patients), group II had received BP for more than 2 years and less than 5 years (n = 41), group III had received BP for more than 5 years and less than 10 years (n = 28), and group IV had received BP for more than 10 years (n = 12).
All patients were managed using an identical protocol, which did not include a pre-extraction drug holiday from BP. Our protocol included (1) preoperative oral management consisting of patient education, maintenance of good oral hygiene (via cooperation with dental hygienists), treatment of caries and periodontitis, and denture adjustment if necessary; (2) oral antibiotics (at least 250 mg amoxicillin or 200 mg clarithromycin) administered prophylactically 60 min before the surgical extraction in accordance with the guidelines for the prevention of surgical site infection; (3) performance of atraumatic tooth extraction as much as possible, even in cases with gingival incision, alveolar bone removal, and/or tooth splitting (without extended bone scraping in principle); (4) tension-free wound closure without relief incision to avoid interruption of the blood supply (i.e., complete closure was not necessarily performed); (5) postoperative administration of oral antibiotics for up to 2 days with the same drugs that were used prophylactically (total daily dose was 1000 mg amoxicillin or 400 mg clarithromycin); (6) follow-up observation and post-extraction socket irrigation in our outpatient department at 1–2 days postoperatively, and then every week until complete epithelialization of the socket was obtained.
The following factors were investigated in all patients: sex, age, medical background, type of administered oral BP, total duration of BP administration, tooth extraction site, type of dental disease that was the reason for tooth extraction, length of follow-up observation until wound healing, and conclusive surgical outcome. Wound healing was defined as epithelial continuity obtained by granulation of the extraction socket, with no fistulae that connected to bone; healing was assessed by one or two dentists who specialized in oral surgery. In cases in which the initial BP was switched to another type of BP, the longest administered drug was regarded as the administered oral BP. BRONJ was diagnosed in accordance with the 2014 criteria of the American Association of Oral and Maxillofacial Surgeons [11]. Patients with systemic risk factors such as glucocorticoid/immunosuppressant administration, diabetes mellitus, rheumatoid arthritis, systemic lupus erythematosus, and/or renal dialysis were regarded as having a much greater risk of BRONJ. We investigated the healing period of the extraction socket and the occurrence of BRONJ. The investigators assessing the outcome were blinded to information about the duration of BP administration. Statistical differences were tested using the Mann-Whitney U test. Differences with p values less than 5% were considered statistically significant.
Results
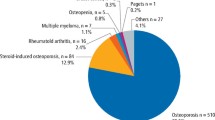
The patient information is summarized in Table 1. There were 20 men (15.2%) and 112 women (84.8%). The mean age was 71.9 ± 11.4 years (range 40–94 years). The reason for BP therapy was primary osteoporosis or osteoporosis prevention; primary osteoporosis was caused by aging or menopause in 77 cases (58.3%), and osteoporosis prevention was required due to long-term administration of glucocorticoids in 55 cases (41.7%). The diseases that necessitated the glucocorticoid administration were rheumatoid arthritis, Sjögren’s syndrome, nephrotic syndrome, interstitial pneumonia, pemphigus, systemic lupus erythematosus, subacute thyroiditis, Behçet’s disease, polymyositis/dermatomyositis, and others. Most patients with autoimmune diseases were referred from the Division of Rheumatology in the Department of Internal Medicine at our institution with many patients. Administered oral BP were alendronate in 59 patients (44.7%), risedronate in 37 patients (28.0%), minodronate in 31 patients (23.5%), and ibandronate in five patients (3.8%). Figure 1 shows the number of cases in each group and the number of cases within each group that had systemic risk factors (Fig. 1). Combined systemic risk factors were glucocorticoid administration in 55 patients (41.7%), diabetes mellitus in 28 patients (21.2%), rheumatoid arthritis in 23 patients (17.4%), systemic lupus erythematosus in four patients (3.0%), and renal dialysis in three patients (2.3%) (overlapping distribution).
Patient distribution by total duration of bisphosphonate (BP) administration and presence (+) or absence (−) of systemic risk factors. In most groups, more than half of the patients had at least one risk factor for the development of BP-related osteonecrosis of the jaw. Group I, those who had received BP therapy for < 2 years (n = 51); group II, received BP for 2–5 years (n = 41); group III, received BP for 5–10 years (n = 28); group IV, received BP for > 10 years (n = 12)
The characteristics of the teeth that were extracted are summarized in Table 2. We removed 274 teeth, of which 101 (36.9%) were maxillary premolars and molars including third molars, 76 (27.7%) were mandibular premolars and molars including third molars, 64 (23.4%) were maxillary anterior teeth, and 33 (12.0%) were mandibular anterior teeth. The dental disease that was the reason for tooth extraction was residual tooth root in 91 teeth (33.2%), chronic marginal periodontitis in 86 teeth (31.4%), periapical periodontitis in 67 teeth (24.5%), root fracture in 18 teeth (6.6%), and pericoronitis of a third molar in 12 teeth (4.3%).
The duration of healing in groups III and IV (BP administration for > 5 years) was significantly longer than that in the groups that had received BP administration for periods of < 5 years. There was no significant difference in the time taken for healing to occur between group III and group IV (Fig. 2). The duration of wound healing exceeded 8 weeks in two cases from group III and two cases from group IV. However, epithelialization was observed at 8 weeks, although it was not yet complete. Therefore, these four cases were judged to have not developed BRONJ and were eventually completely healed without the development of BRONJ. There was no BRONJ in any case, regardless of the BP administration period. In all groups, there was no significant prolongation of wound healing due to systemic risk factors such as glucocorticoid administration and diabetes mellitus.
The relationship between bisphosphonate (BP) administration period and duration of wound healing after tooth extraction. The duration of healing in groups III and IV (BP administration for > 5 years) was significantly longer than that in the groups that received BP therapy for < 5 years. There was no significant prolongation of wound healing due to the presence of systemic risk factors in any group. Group I, those who had received BP therapy for < 2 years; group II, received BP for 2–5 years; group III, received BP for 5–10 years; group IV, received BP for > 10 years. Error bars show the standard error of the mean; n.s., not significant; *p < 0.01; the plus sign indicates patients with systemic risk factors, while the minus sign indicates those without systemic risk factors
Discussion
In the present study, we removed 274 teeth in 132 patients with continued oral BP therapy. Long-term oral BP therapy for > 5 years significantly delayed the healing of the extraction socket; however, BRONJ did not develop, regardless of the administration period.
There is a strong tendency to avoid invasive dental treatment such as tooth extraction in those receiving BP, as this is considered a major risk factor for BRONJ. However, the risk of BRONJ is lower in osteoporotic patients receiving low-dose BP than in patients with cancer receiving high-dose BP, and elective dentoalveolar surgery does not appear to be contraindicated in patients receiving low-dose BP for osteoporosis [11]. Additionally, several studies reported that existing infectious conditions, such as periodontitis/periapical lesions and baseline osteomyelitis, were much greater risk factors for BRONJ development than tooth extraction [27,28,29]. Furthermore, avoiding tooth extraction and leaving the chronic inflammatory state unattended may actually cause BRONJ, so tooth extraction may be required to remove the cause of inflammation.
Some previous studies have investigated the effects of a drug holiday for the prevention of BRONJ [11, 12, 30, 31], but there is no unified consensus. The American Association of Oral and Maxillofacial Surgeons guidelines (revised in 2014) suggest that clinicians should consider instigating a 2-month drug-free period prior to an invasive procedure [11]. In 2011, the American Dental Association Council on Scientific Affairs revised their prior recommendation of a drug holiday and suggested that patients receiving lower cumulative doses of BP (< 2 years) may continue antiresorptive therapy during invasive dental treatment [30]. The International ONJ Task Force recommends a drug holiday until the site has healed in patients at greater risk of developing ONJ, including those with greater cumulative BP exposure (> 4 years) [12]. A 2011 document published by the Food and Drug Administration on the long-term safety of BP therapy for osteoporosis stated that there was “no substantial data available to guide decisions regarding the initiation or duration of a drug holiday” [31]. However, these recommendations are mostly based on observational studies and case reports that have little definitive evidence [24, 32]. Additionally, they are focused solely on BRONJ, while not considering adverse skeletal events. Considering the potential outcome of fracture caused by adverse skeletal events, caution is required when deciding whether to initiate a drug holiday from BP.
Regarding strategies for the prevention of BRONJ after tooth extraction, there are controversies about antibiotic administration methods and the necessity of complete wound closure. With no definite consensus on the antibiotic administration method [33], we took into consideration the risk of antibiotic-resistant bacteria development due to long-term antibiotic administration and administered the minimum dosage required from just before tooth extraction. Antibiotic administration for 6 days from the evening before surgery is reportedly useful [26], but our study showed that there was no problem with using the minimum dosage in accordance with the guidelines for prevention of surgical site infection.
Regarding closure of the extraction socket wound, good progress can reportedly be obtained by performing complete closure [34], but some cases result in wound dehiscence even after complete closure at the time of tooth extraction. Healing of the extraction socket may be hindered by invasive procedures such as grinding of the alveolar bone and creating a gingival flap relief incision, and these procedures may increase the risk of BRONJ. More noninvasive tooth extraction is preferred, as atraumatic surgery is more comfortable and beneficial for patients [26]. Therefore, we considered it preferable to close the wound only to the extent possible using noninvasive methods rather than closing the wound forcibly, and did not necessarily perform complete closure in all cases.
Tooth extraction via our protocol resulted in no occurrence of BRONJ. We did not perform any special procedures, but avoided the development of BRONJ even after tooth extraction with continued BP therapy by performing atraumatic procedures and strict infection control.
The reference value for “2-year periods” of cumulative BP exposure was based on previous evaluations by multiple organizations of the risk of BRONJ [12, 30, 35]. The higher values (“5-year periods” and “10-year periods”) used in the present study were determined with reference to the recommendations of a Task Force of the American Society for Bone and Mineral Research (ASBMR) [13]. The ASBMR recommends reassessment after 5 years of oral BP; lower-risk patients should then be offered a drug holiday, while BP should be continued for up to 10 years in higher-risk patients [13]. Previous studies have reported systemic factors such as glucocorticoid administration and diabetes mellitus as risk factors for BRONJ [11, 12], but the existence of these risk factors within the same BP administration period group did not significantly delay healing after tooth extraction in our study. Although the duration of healing was significantly prolonged in groups III and IV (BP administration for > 5 years) in comparison with the groups who had received BP for periods of < 5 years, BRONJ did not occur. Our treatment strategy is based on a protocol that allows tooth extraction without hesitation even by dentists who do not specialize in oral surgery, and is highly versatile. The present results suggest that our method is not inferior to the treatment strategy that includes a pre-extraction drug holiday from BP and is a viable treatment option.
It is necessary to identify the cases that have already developed BRONJ (i.e., latent BRONJ) at the time of tooth extraction. If we had performed tooth extraction in these cases, it may have been incorrectly concluded that BRONJ had developed due to tooth extraction. One such case that could have been misdiagnosed as BRONJ development after tooth extraction was excluded from the present study after BRONJ was diagnosed because of the presence of Vincent’s symptom. If latent BRONJ is suspected, a biopsy should be taken from the extraction socket to enable definitive diagnosis.
Care must be taken when performing tooth extraction in patients receiving long-term oral BP therapy and in those with a high cumulative dosage despite a low daily dose. The present results suggest that the effect of BP administration for “more than 5 years” should be considered; this is also the time at which reassessment of oral BP administration is recommended by the Task Force of the ASBMR [13]. Although it is uncertain how effective a short-term BP drug holiday would be considering bone physiology and the pharmacokinetics of BP, it may be valuable to consider a drug holiday in high-risk patients, such as those who have taken oral BP for more than 5 years.
The present study had some limitations. Our study was prospective, but did not include a non-BP-treated control group. As BRONJ is associated with various systemic and local risk factors, we cannot make definitive conclusions about BRONJ development from the present results alone due to the relatively small sample size; however, there were no occurrences of BRONJ using our treatment strategy. Furthermore, the occurrence of ONJ is not related solely to BP administration and has been reported in patients receiving denosumab, leading to the recent introduction of the terms “medication-related osteonecrosis of the jaw” and “antiresorptive agent-related osteonecrosis of the jaw” [11, 12, 30, 36]. We plan to conduct a similar study on tooth extraction with continuous administration of denosumab.
Conclusion
In patients who underwent tooth extraction with continued oral BP therapy, the healing of the extraction socket was delayed as the cumulative administration period prolonged, but BRONJ did not develop.
References
Kanis JA, Melton LJ 3rd, Christiansen C, Johnston CC, Khaltaev N (1994) The diagnosis of osteoporosis. J Bone Miner Res 9:1137–1141
Orimo H, Nakamura T, Hosoi T, Iki M, Uenishi K, Endo N, Ohta H, Shiraki M, Sugimoto T, Suzuki T, Soen S, Nishizawa Y, Hagino H, Fukunaga M, Fujiwara S (2012) Japanese 2011 guidelines for prevention and treatment of osteoporosis—executive summary. Arch Osteoporos 7:3–20
Kanis JA (2002) Diagnosis of osteoporosis and assessment of fracture risk. Lancet 359:1929–1936
Kitamura S, Hasegawa Y, Suzuki S, Sasaki R, Iwata H, Wingstrand H, Thorngren KG (1998) Functional outcome after hip fracture in Japan. Clin Orthop Relat Res 348:29-36
Willig R, Keinanen-Kiukaaniemi S, Jalovaara P (2001) Mortality and quality of life after trochanteric hip fracture. Public Health 115:323–327
Russell RG, Watts NB, Ebetino FH, Rogers MJ (2008) Mechanisms of action of bisphosphonates: similarities and differences and their potential influence on clinical efficacy. Osteoporos Int 19:733–759
Bilezikian JP (2009) Efficacy of bisphosphonates in reducing fracture risk in postmenopausal osteoporosis. Am J Med 122:S14–S21
Body JJ, Coleman R, Clezardin P, Ripamonti C, Rizzoli R, Aapro M (2007) International Society of Geriatric Oncology (SIOG) clinical practice recommendations for the use of bisphosphonates in elderly patients. Eur J Cancer 43:852–858
Marx RE (2003) Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg 61:1115–1117
Ruggiero SL, Mehrotra B, Rosenberg TJ, Engroff SL (2004) Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg 62:527–534
Ruggiero SL, Dodson TB, Fantasia J, Goodday R, Aghaloo T, Mehrotra B, O’Ryan F (2014) American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw—2014 update. J Oral Maxillofac Surg 72:1938–1956
Khan AA, Morrison A, Hanley DA, Felsenberg D, McCauley LK, O’Ryan F, Reid IR, Ruggiero SL, Taguchi A, Tetradis S, Watts NB, Brandi ML, Peters E, Guise T, Eastell R, Cheung AM, Morin SN, Masri B, Cooper C, Morgan SL, Obermayer-Pietsch B, Langdahl BL, al Dabagh R, Davison KS, Kendler DL, Sándor GK, Josse RG, Bhandari M, el Rabbany M, Pierroz DD, Sulimani R, Saunders DP, Brown JP, Compston J, on behalf of the International Task Force on Osteonecrosis of the Jaw (2015) Diagnosis and management of osteonecrosis of the jaw: a systematic review and international consensus. J Bone Miner Res 30:3–23
Adler RA, El-Hajj Fuleihan G, Bauer DC et al (2016) Managing osteoporosis in patients on long-term bisphosphonate treatment: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 31:16–35
Vahtsevanos K, Kyrgidis A, Verrou E, Katodritou E, Triaridis S, Andreadis CG, Boukovinas I, Koloutsos GE, Teleioudis Z, Kitikidou K, Paraskevopoulos P, Zervas K, Antoniades K (2009) Longitudinal cohort study of risk factors in cancer patients of bisphosphonate-related osteonecrosis of the jaw. J Clin Oncol 27:5356–5362
Saad F, Brown JE, Van Poznak C et al (2012) Incidence, risk factors, and outcomes of osteonecrosis of the jaw: integrated analysis from three blinded active-controlled phase III trials in cancer patients with bone metastases. Ann Oncol 23:1341–1347
Kyrgidis A, Vahtsevanos K, Koloutsos G, Andreadis C, Boukovinas I, Teleioudis Z, Patrikidou A, Triaridis S (2008) Bisphosphonate-related osteonecrosis of the jaws: a case-control study of risk factors in breast cancer patients. J Clin Oncol 26:4634–4638
Hoff AO, Toth BB, Altundag K, Johnson MM, Warneke CL, Hu M, Nooka A, Sayegh G, Guarneri V, Desrouleaux K, Cui J, Adamus A, Gagel RF, Hortobagyi GN (2008) Frequency and risk factors associated with osteonecrosis of the jaw in cancer patients treated with intravenous bisphosphonates. J Bone Miner Res 23:826–836
Kunchur R, Need A, Hughes T, Goss A (2009) Clinical investigation of C-terminal cross-linking telopeptide test in prevention and management of bisphosphonate-associated osteonecrosis of the jaws. J Oral Maxillofac Surg 67:1167–1173
Hansen PJ, Knitschke M, Draenert FG, Irle S, Neff A (2013) Incidence of bisphosphonate-related osteonecrosis of the jaws (BRONJ) in patients taking bisphosphonates for osteoporosis treatment—a grossly underestimated risk? Clin Oral Investig 17:1829–1837
Taylor T, Bryant C, Popat S (2013) A study of 225 patients on bisphosphonates presenting to the bisphosphonate clinic at King’s College Hospital. Br Dent J 214:E18
Jeong HG, Hwang JJ, Lee JH, Kim YH, Na JY, Han SS (2017) Risk factors of osteonecrosis of the jaw after tooth extraction in osteoporotic patients on oral bisphosphonates. Imaging Sci Dent 47:45–50
Hasegawa T, Kawakita A, Ueda N et al (2017) A multicenter retrospective study of the risk factors associated with medication-related osteonecrosis of the jaw after tooth extraction in patients receiving oral bisphosphonate therapy: can primary wound closure and a drug holiday really prevent MRONJ? Osteoporos Int 28:2465–2473
Damm DD, Jones DM (2013) Bisphosphonate-related osteonecrosis of the jaws: a potential alternative to drug holidays. Gen Dent 61:33–38
Taguchi A, Shiraki M, Tsukiyama M, Miyazaki T, Soen S, Ohta H, Nakamura T, Orimo H (2015) Impact of osteonecrosis of the jaw on osteoporosis treatment in Japan: results of a questionnaire-based survey by the adequate treatment of osteoporosis (A-TOP) research group. Calcif Tissue Int 97:542–550
Huang YF, Chang CT, Muo CH, Tsai CH, Shen YF, Wu CZ (2015) Impact of bisphosphonate-related osteonecrosis of the jaw on osteoporotic patients after dental extraction: a population-based cohort study. PLoS One 10:e0120756
Mozzati M, Arata V, Gallesio G (2013) Tooth extraction in osteoporotic patients taking oral bisphosphonates. Osteoporos Int 24:1707–1712
Yamazaki T, Yamori M, Ishizaki T, Asai K, Goto K, Takahashi K, Nakayama T, Bessho K (2012) Increased incidence of osteonecrosis of the jaw after tooth extraction in patients treated with bisphosphonates: a cohort study. Int J Oral Maxillofac Surg 41:1397–1403
Tsao C, Darby I, Ebeling PR, Walsh K, O’Brien-Simpson N, Reynolds E, Borromeo G (2013) Oral health risk factors for bisphosphonate-associated jaw osteonecrosis. J Oral Maxillofac Surg 71:1360–1366
Saia G, Blandamura S, Bettini G, Tronchet A, Totola A, Bedogni G, Ferronato G, Nocini PF, Bedogni A (2010) Occurrence of bisphosphonate-related osteonecrosis of the jaw after surgical tooth extraction. J Oral Maxillofac Surg 68:797–804
Hellstein JW, Adler RA, Edwards B, Jacobsen PL, Kalmar JR, Koka S, Migliorati CA, Ristic H, American Dental Association Council on Scientific Affairs Expert Panel on Antiresorptive Agents (2011) Managing the care of patients receiving antiresorptive therapy for prevention and treatment of osteoporosis: executive summary of recommendations from the American Dental Association Council on Scientific Affairs. J Am Dent Assoc 142:1243–1251
Food and Drug Administration (2011) Background Document for Meeting of Advisory Committee for Reproductive Health Drugs and Drug Safety and Risk Management Advisory Committee http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/drugs/DrugSafetyandRiskManagementAdvisoryCommittee/ucm270958
Yoneda T, Hagino H, Sugimoto T, Ohta H, Takahashi S, Soen S, Taguchi A, Toyosawa S, Nagata T, Urade M (2010) Bisphosphonate-related osteonecrosis of the jaw: position paper from the allied task force committee of Japanese society for bone and mineral research, Japan Osteoporosis Society, Japanese Society of Periodontology, Japanese Society for Oral and Maxillofacial Radiology, and Japanese Society of Oral and Maxillofacial Surgeons. J Bone Miner Metab 28:365–383
American Dental Association Council on Scientific Affairs (2006) Dental management of patients receiving oral bisphosphonate therapy: expert panel recommendations. J Am Dent Assoc 137:1144–1150
Heufelder MJ, Hendricks J, Remmerbach T, Frerich B, Hemprich A, Wilde F (2014) Principles of oral surgery for prevention of bisphosphonate-related osteonecrosis of the jaw. Oral Surg Oral Med Oral Pathol Oral Radiol 117:e429–e435
Barasch A, Cunha-Cruz J, Curro FAA et al (2011) Risk factors for osteonecrosis of the jaws: a case-control study from the CONDOR dental PBRN. J Dent Res 90:439–444
Yoneda T, Hagino H, Sugimoto T et al (2017) Antiresorptive agent-related osteonecrosis of the jaw: Position Paper 2017 of the Japanese Allied Committee on Osteonecrosis of the Jaw. J Bone Miner Metab 35:6–19
Acknowledgments
We thank Kelly Zammit, BVSc, from Edanz Group (www.edanzediting.com/ac), for editing a draft of this manuscript.
Funding
This study was supported, in part, by the Ministry of Education, Culture, Sports, Science and Technology (MEXT) Supported Program for the Strategic Research Foundation at Private Universities, 2014–2018.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflicts of interest
The authors received a research grant from MEXT 2014–2018 (no grant number). Hiromitsu Kishimoto has received a lecture fee from Asahi Kasei Pharma, Daiichi-Sankyo, Chugai Pharmaceutical, Teijin Pharma.
Informed consent
Informed consent was obtained from all individual participants included in this study.
Rights and permissions
About this article
Cite this article
Shudo, A., Kishimoto, H., Takaoka, K. et al. Long-term oral bisphosphonates delay healing after tooth extraction: a single institutional prospective study. Osteoporos Int 29, 2315–2321 (2018). https://doi.org/10.1007/s00198-018-4621-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-018-4621-7