Abstract
Summary
Deprivation predicts increased hip fracture risk. Over 14 years, hip fracture incidence increased among men with persisting inequalities. Among women, inequalities in incidence were less pronounced; whilst incidence decreased overall, this improvement was seen marginally less in women from the most deprived areas. Hip fracture prevention programmes have not reduced inequalities.
Purpose
Deprivation is associated with increased hip fracture risk. We examined the effect of area-level deprivation on hip fracture incidence in England over 14 years to determine whether inequalities have changed over time.
Methods
We used English Hospital Episodes Statistics (2001/2002–2014/2015) to identify hip fractures in adults aged 50+ years and mid-year population estimates (2001–2014) from the Office for National Statistics. The Index of Multiple Deprivation measured local area deprivation. We calculated age-adjusted incidence rate ratios (IRR) for hip fracture, stratified by gender and deprivation quintiles.
Results
Over 14 years, we identified 747,369 hospital admissions with an index hip fracture; the number increased from 50,640 in 2001 to 55,092 in 2014; the proportion of men increased from 22.2% to 29.6%. Whereas incidence rates decreased in women (annual reduction 1.1%), they increased in men (annual increase 0.6%) (interaction p < 0.001). Incidence was higher in more deprived areas, particularly among men: IRR most vs. least deprived quintile 1.50 [95% CI 1.48, 1.52] in men, 1.17 [1.16, 1.18] in women. Age-standardised incidence increased for men across all deprivation quintiles from 2001 to 2014. Among women, incidence fell more among those least compared to most deprived (year by deprivation interaction p < 0.001).
Conclusions
Deprivation is a stronger relative predictor of hip fracture incidence in men than in women. However, given their higher hip fracture incidence, the absolute burden of deprivation on hip fractures is greater in women. Despite public health efforts to prevent hip fractures, the health inequality gap for hip fracture incidence has not narrowed for men, and marginally widened among women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fractures are common with a substantial public health impact. There were approximately 65,000 hip fractures in England, Wales and Northern Ireland in 2015 [1]; this number is projected to increase as our population ages. Hip fractures are associated with significant morbidity and mortality [2,3,4], and have a considerable financial impact upon healthcare systems. Annual hospital costs associated with incident hip fractures have been estimated at £1.1 billion for the UK [5].
Greater deprivation is associated with an increased hip fracture incidence in many countries including Australia [6], Canada [7], Portugal [8], Sweden [9] and the USA [10, 11]. In contrast, the reverse relationship has been reported in Spain where hip fracture risk was higher in the least deprived compared to most deprived areas, possibly explained by the protective effects of obesity for the hip [12]. In the UK, a number of studies have identified an association between worsening deprivation and higher hip fracture incidence [13,14,15,16], but this has not been consistently demonstrated albeit by studies of varying lengths [17, 18]. In addition, recent evidence suggests that the relationship between deprivation and hip fracture risk may be stronger in men than in women [16], potentially explained by differing predispositions in men and women towards lifestyle habits that increase fracture risk, such as tobacco and heavy alcohol consumption [19, 20].
Over the last two decades, efforts have been made to prevent hip fractures, through development of fracture liaison services that prioritise secondary fracture prevention [21]. Over this period, hip fracture incidence has plateaued or declined in high-income countries; age-standardised hip fracture incidence declined in Australia [22], Canada [23] and the USA [24], and rates have plateaued in England [13, 15, 25]. However, contrasting gender-specific trends in England have been reported, with hip fracture incidence rising among older men, but declining among the larger older female population (between 2003 and 2013) [26]. In support of this, analysis of the Clinical Practice Research Datalink (CPRD) showed that hip fracture incidence had remained unchanged in women between 1990–1994 and 2008–2012, but had increased in men over the same period [27].
What is not known is how the relationship between deprivation and hip fracture incidence has changed over recent years in men and women. We hypothesised that secular changes in hip fracture incidence in men and women have not been the same across all levels of deprivation; we hypothesised that greater declines in hip fracture incidence would be observed among women living in less deprived areas, given a greater awareness of osteoporosis risk among women, and that individuals living in less deprived areas are more likely to engage with preventative healthcare services [28]. We used English Hospital Episodes Statistics (HES) and Office for National Statistics (ONS) mid-year population estimates for the period 2001 to 2015, to identify if secular trends differed by levels of deprivation among men and women in England over this 14-year period.
Methods
Data sources
We used anonymised patient-level data from the routinely collected HES Admitted Patient Care database that included admissions to all English hospitals within the National Health Service (NHS) (i.e. excluding privately financed healthcare) for the period 1st April 2001 to 31st March 2015. Each entry, or episode, in HES relates to a period of care under a single hospital consultant; there are one or more hospital episodes during a hospital admission. Each HES episode includes information on patient demographics and up to 20 clinical diagnoses using International Classification of Diseases, Tenth Revision (ICD-10) disease codes [29].
We obtained mid-year population estimates for England for each year from 2001 to 2014 from the ONS. We received population denominator data stratified by age categories (birth to 90+ years in 5-yearly intervals), gender and Index of Multiple Deprivation (IMD) 2015 quintiles.
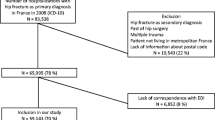
Study population
We identified hip fracture admissions using ICD-10 disease codes for fracture of neck of femur (S72.0), pertrochanteric fracture (S72.1) and subtrochanteric fracture (S72.2). Our study population consisted of index cases of hip fracture, that is, the first occurrence of hip fracture, among male and female English residents aged 50 years and older who were admitted to the hospital with a hip fracture or who sustained a hip fracture during a hospital admission. We excluded second hip fractures in order to avoid double-counting, since we were not able to distinguish reliably between two separate hip fracture events in HES. We excluded patients under the age of 50 years as hip fractures in this age group are primarily due to high-impact trauma. We also excluded patients with missing data for age, gender, IMD and geographic region of residence (n = 4667).
Study variables
We used the IMD to measure socio-economic deprivation. The IMD is a relative measure of deprivation for small areas, termed lower super output areas (LSOAs), which are defined as geographical areas of a similar population size with an average of 1500 residents [30]. The IMD is composed of seven measures of deprivation: income deprivation; employment deprivation; education, skills and training deprivation; health deprivation and disability; crime; barriers to housing and services; and living environment deprivation. There are 32,482 LSOAs in England, and each LSOA is assigned a score and a rank for the individual domains of deprivation. A weighted sum of the ranks for each domain is used to calculate an overall IMD score based upon which LSOAs are then ranked nationally. The IMD 2004 version was used for financial years 2001/2002 to 2006/2007 in HES; the IMD 2007 version was used for financial years 2007/2008 to 2009/2010; and the IMD 2010 version was used for financial years 2010/2011 to 2014/2015 [29]. We used the IMD rank for a patient’s LSOA and categorised patients into quintiles based upon the national ranking of local areas, with quintile 1 being the least deprived group and quintile 5 being the most deprived group.
We derived further variables to describe patient characteristics, including 5-yearly age groupings from 50 years to 90+ years, gender and comorbidity. We used the Royal College of Surgeons Charlson Score to measure comorbidity [31]. This is based upon several chronic conditions identified using ICD-10 diagnosis codes for the index hip fracture admission and admissions in the preceding 3 years. In our HES extract, comorbidity data were only available for the most recent 10 financial years (2005/2006 to 2014/2015) so we restricted our comorbidity analyses to the most recent 7 years (2008/2009 to 2014/2015) to allow a 3-year retrospective period. We categorised the comorbidity score into a four-level ordinal variable (0, 1, 2 or 3 or more comorbid conditions).
Research approvals
We obtained NHS Research Ethics Committee approval for this study (REC reference: 15/LO/1056).
Statistical analyses
We summarised key demographic statistics, and used the chi-squared (χ 2) test to assess the association between categorical variables and linear regression to assess trends in log-transformed age and IMD score. We calculated annual incidence rates of hip fracture per 100,000 population as the number of index hip fractures divided by the population count for each year, gender and IMD quintile. To assess time trends, we used direct standardisation to calculate age-standardised rates using the population of England in 2001 as our reference year and grouping age into nine bands.
Separately for women and men, we used Poisson regression modelling to determine the association between IMD and hip fracture incidence and calculated incidence rate ratios (IRRs), using quintile 1, the least deprived quintile, as the reference category and adjusting for age. We then included year as a linear term to test for time trends, and tested for differences in time trends by deprivation by including interaction terms. All statistical analyses were conducted using Stata, version 14 MP.
As a secondary analysis, we explored time trends among hip fracture patients with comorbidities and examined differences by levels of deprivation. We were unable to determine differences in hip fracture incidence by comorbidity because we lacked comorbidity data for the English population as a whole. Instead, we used direct standardisation to calculate the age-standardised proportion of hip fracture admissions with low (≤1 comorbid condition) and high (≥2 comorbid conditions) comorbidity by gender and IMD quintiles using the hip fracture population in 2008 as the reference year.
Results
We identified 752,036 hospital admissions with an index hip fracture among English residents aged 50 years and older from 2001 to 2014. We excluded 4667 (0.6%) patients with missing data for age, sex, IMD and/or geographic region of residence. Of the remaining 747,369 cases of hip fracture, 74.2% occurred in women and 37.7% had two or more coded comorbid conditions (Table 1). The median (inter-quartile range) age of our study population was 83 years (77–88): 81 (74–87) in men and 84 (78–89) in women. Hip fracture patients in the most deprived quintile were more likely to be younger, male and have a higher burden of comorbidity when compared to patients in the least deprived quintile (Table 1). Over time, the proportion of women decreased and the burden of comorbidity increased within our hip fracture population (Table 2).
Hip fracture incidence
Whilst the number of hip fracture admissions increased over the 14 years examined, from 50,640 in 2001 to 55,092 in 2014, overall age-standardised hip fracture incidence rates decreased from 308 to 271 per 100,000 population between 2001 and 2014.
Trends in age-standardised incidence differed markedly by gender with a decline observed for women at an average rate of 1.1% per year, whilst rates increased for men at an average rate of 0.6% per year (gender by time interaction p < 0.001). As expected, considerably higher rates of hip fracture were observed among older people (80+ vs. <80 years: IRR 12.64 [95% CI 12.58, 12.70], p < 0.001), but the rate among women was approximately 80% higher than that for men even after adjusting for age (IRR 1.78 [95% CI 1.77, 1.79], p < 0.001).
Hip fracture incidence by levels of deprivation in men
Age-adjusted incidence was substantially higher for men in the most deprived compared with the least deprived quintile (IRR 1.50 [95% CI 1.48, 1.52], p < 0.001) with a dose-response pattern (Fig. 1).
From 2001 to 2014, age-standardised hip fracture incidence rates increased similarly for men across all strata of deprivation and this rate of increase did not differ by levels of deprivation (deprivation by time interaction, p = 0.11) (Fig. 2).
Hip fracture incidence by levels of deprivation in women
In women, there was a less marked association between levels of deprivation and hip fracture incidence with a dose-response pattern (Fig. 1). Age-adjusted hip fracture incidence was 17% higher in the most deprived vs. the least deprived quintile (IRR 1.17 [95% CI 1.16, 1.18], p < 0.001).
Whereas age-standardised incidence declined in women across all strata of deprivation from 2001 to 2014, more marked declines in hip fracture incidence were observed among women in the least deprived quintile as compared to the most deprived quintile (deprivation by time interaction, p < 0.001). For example, among the least deprived quintile, hip fracture incidence decreased by 60 hip fractures per 100,000 women between 2001 and 2014 equating to an average decline of 1.41% per year, whilst among the most deprived quintile a more modest decline of 31 hip fractures per 100,000 women was seen, equating to an average decline of 0.59% per year (Fig. 2).
Hip fracture admissions among those with high levels of comorbidity
Over the period 2008 to 2014, 46.2% of men and 34.5% of women with a hip fracture admission had high levels of comorbidity. After standardising for age, the proportion of hip fracture admissions rose by 14.2% among men and 12.7% among women between 2008 and 2014. The age-standardised proportion was higher in the most deprived compared with the least deprived quintile in both men and women, and this proportion increased similarly across all strata of deprivation (Fig. 3).
Discussion
This study examined the relationship between area-based deprivation and hip fracture incidence in men and women aged 50 years and older in England over a 14-year period, confirming that whilst age-standardised hip fracture incidence is declining in women, there has been an increase among men. Among men, social deprivation is associated with substantially higher hip fracture rates, and these inequalities have not improved over more than a decade, so that men who are most deprived are 50% more likely to fracture their hip than those who are least deprived. Across England, when averaged over 14 years, this equates to approximately 8546 excess hip fractures per year occurring among men with greater deprivation (quintiles 2 to 5 vs. 1). Among women, the effect of deprivation on hip fracture incidence is weaker: however, owing to the higher incidence of hip fractures in women, the absolute burden of deprivation on hip fractures is greater in women than in men. Differences in hip fracture incidence have become more overt over time, with women who are most deprived benefiting the least from improved secular trends in hip fracture incidence. Comorbidity levels have increased within the hip fracture population over time, and these increases have occurred in women and men across all deprivation strata.
Ours is only the second study in the UK to examine the association between deprivation and hip fracture incidence over time; a previous analysis (1998–2008) did not identify the clear relationships we have done [13]; however, their analyses were not gender stratified and were based upon the Carstairs deprivation index, an area-based measure of relative material deprivation calculated at the ward level using four census indicators (male unemployment, overcrowding, car ownership and low social class) [32]. We used the IMD which, in contrast, is based on a broader range of deprivation measures across seven domains of deprivation, and therefore is considered to provide a more comprehensive assessment of deprivation at the small-area level. We also measured at a smaller and more homogenous area (LSOAs), which should have reduced exposure misclassification.
Few studies have examined the relationship between deprivation and hip fracture incidence by gender. Our findings suggest a stronger association between deprivation and hip fracture incidence in men than in women and are consistent with those of a recent UK study, in men and women aged over 18 years, using general practitioner (CPRD) records from 1988 to 2012 [16]; our findings, with the advantage of a larger sample size, confirm a clear association between deprivation and hip fracture risk in men, and determine a previously unidentified association between deprivation and hip fracture risk in women. This association between deprivation and increased hip fracture incidence in both men and women may partly be explained by the social gradient of lifestyle-associated risk factors for fracture. The prevalence of tobacco [33] and heavy alcohol consumption [34] is higher among more deprived populations, with men rather than women having a greater propensity towards these lifestyle habits [19, 20]. Alcohol consumption and tobacco use are associated with an increased risk of hip fracture in men [35]. Similarly, the prevalence of obesity, physical inactivity and poor nutrition increases with greater levels of deprivation [36]. The less marked relationship between deprivation and hip fracture incidence in women may in part be explained by the stronger relationship between deprivation and obesity in women [37], as adiposity over the greater trochanter is thought to protect against hip fracture [38]. Interestingly, a regional study in an urban population in Spain (2009–2012) demonstrated that age- and sex-adjusted hip fracture risk was 10% lower in the most deprived as compared to the least deprived areas [12]. However, this association was attenuated after adjustment for body mass index (BMI), suggesting that a higher prevalence of obesity in more deprived areas may have accounted for the inverse relationship observed. We were unable to adjust for obesity in our analyses due to lack of BMI data in HES; similarly, tobacco use and alcohol consumption data were not available for analysis.
Studies investigating the relationship between deprivation and hip fracture incidence have mostly demonstrated a social gradient with greater levels of deprivation being associated with a higher hip fracture incidence across many high-income countries [6,7,8,9,10,11], including the UK [14,15,16]. Despite efforts made over the last decade by the UK Government to reduce health inequalities in England, it is concerning that our findings suggest that disparities in fracture prevention persist and, in some groups, have worsened. The ‘Choosing Health: making healthy choices easier’ (2004) and ‘Healthy Lives, Healthy People’ (2010) white papers highlighted the Government’s strategy for addressing public health challenges [39, 40], and the ‘Marmot Review’ (2010) provided evidence-based policy recommendations for addressing health inequalities in England [41]. These efforts coincided with a growing emphasis towards the improved management of individuals at risk of fragility fractures; in 2012, NICE issued guidance on targeted assessment of fracture risk among ‘at risk’ populations (such as those with comorbidities) using validated tools, namely FRAX and QFracture [42], as well as treatment recommendations to protect bone [43]. Hip fractures commonly follow another index fragility fracture, hence the importance of Fracture Liaison Services (FLS) to promptly identify such fractures and instigate management to reduce future fracture risk (21). Despite this, a significant gap in care for secondary fracture prevention has been reported in several countries [44] as well as in the UK [45]. Several large-scale initiatives aiming to narrow this care gap have been implemented nationally [21, 42, 46] and internationally [47]. Encouragingly, over the last two decades, we have made considerable gains in reducing hip fracture incidence among women in England; however, our findings suggest that greater focus needs to be placed upon addressing the rising hip fracture incidence in men, as well as the inequities in hip fracture incidence observed in those who are most deprived.
The decline in hip fracture incidence rates among women that we report are consistent with studies conducted in Australia [22], Canada [23] and the USA [24]. However, these also reported, albeit to a lesser degree, declining rates in men. Our contrasting observation of increasing hip fracture incidence among men is consistent with an analysis of UK general practitioner (CPRD) records, which showed that hip fracture incidence increased from 108 to 134 hip fractures per 100,000 person-years between 1990-1994 and 2008–2012 [27]; although hip fracture incidence was reported as stable in women, the analyses were not age adjusted. Early HES analyses reported stable age-standardised hospital admission rates for hip fractures in men and women in England between 1989 and 1998 [25], and gender-specific trends similar to those we report were seen in older adults between 2003 and 2013 [26]. Gender differences in secular trends in hip fracture incidence may be partly explained by an under-appreciation of osteoporosis as a disease that affects men. Despite a third of all hip fractures worldwide occurring in men [48], and their higher associated mortality [49], men are less likely to receive osteoporosis treatment than women [24, 45, 50]. A UK study found that women were 50% more likely than men to be initiated on an anti-osteoporosis drug within the year following an incident hip fracture over the period 2000 to 2010 [45]. The use of androgen deprivation therapy to treat prostate cancer has risen in England since the 1980s from 33,000 prescriptions in 1987 to 470,000 prescriptions in 2004 and is a well-established risk factor for fracture [51, 52]. Whilst the frequency of alcohol consumption has decreased considerably from 2005 to 2014, in men alcohol consumption more than three times the daily recommended limit has only marginally decreased from 12% in 2005 to 10% in 2014 [53].
Our findings that the proportion of age-standardised hip fracture admissions in both men and women who have comorbidity has risen from 2008 to 2014 further highlights the importance of hip fracture prevention in those with comorbid conditions; a similar trend has been observed in the USA using Medicare claims data from 1985 to 2005 [24]. Nationally the burden of comorbidity is growing; the number of people with multiple comorbidities is predicted to rise from 1.9 million in 2008 to 2.9 million in 2018 in the UK [54]. Furthermore, deprivation is associated with higher rates of comorbidity [55, 56]. The increasing burden of comorbid disease amidst our growing ageing population is likely to have a significant impact on future hip fracture incidence.
Limitations
We calculated hip fracture incidence rates based on individuals, and therefore, we limited our analyses to the first occurrence of hip fracture for each patient, which is likely to lead to an underestimation of hip fracture incidence (8.7% of hip fractures are thought to be second hip fractures [57]). The vast majority of hip fractures are expected to be managed in an NHS hospital; however, a small proportion may have been admitted directly to privately financed healthcare facilities and hence were not captured in HES, again leading to an underestimation of hip fracture incidence, particularly among those least deprived. The quality of clinical coding in HES is liable to have changed over time in response to changes in health care tariff systems, influencing the recording of comorbidities over our study period and potentially contributing to the apparent increasing burden of comorbid disease. Hence, we may have underestimated the proportion of hip fracture admissions with comorbidity during the earlier years of our analyses. Finally, we used an area-based measure of deprivation as a proxy for an individual’s level of deprivation, so this ecological measure will in some cases misclassify individuals.
Conclusion
Our study is the largest UK population-based study of incident hip fracture admissions assessed by levels of deprivation in both men and women for more than a decade. The availability of patient-level data for all hip fracture admissions to English NHS hospitals over a 14-year period allowed us to undertake detailed examination of secular trends in hip fracture incidence, stratified by IMD quintiles and gender, using a valid measure of deprivation specific to the English context. We have demonstrated firstly that, after accounting for age, hip fracture incidence is declining in women, but is rising in men; secondly, deprivation predicts increased hip fracture incidence in both women and men, with a stronger relative impact among men. However, owing to the overall higher incidence of hip fractures in women, deprivation has a greater impact on the number of hip fractures among women. Thirdly, despite UK Government and public health initiatives to both address health inequalities and prevent hip fractures, absolute inequalities in hip fracture incidence have persisted among both men and women over the 14 years studied, with the health inequality gap marginally widening among women. Our findings stress the need for reassessment of current national public health strategies to prevent hip fractures. Particular focus is needed on the development of health policies that address persisting social and gender inequalities.
References
Royal College of Physicians (2016) National Hip Fracture Database annual report 2016. RCP, London
Keene GS, Parker MJ, Pryor GA (1993) Mortality and morbidity after hip fractures. BMJ 307(6914):1248–1250
Katsoulis M, Benetou V, Karapetyan T, Feskanich D, Grodstein F, Pettersson-Kymmer U et al (2017) Excess mortality after hip fracture in elderly persons from Europe and the USA: the CHANCES project. J Intern Med 281(3):300–310
Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA (1999) Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet 353(9156):878–882
Leal J, Gray AM, Prieto-Alhambra D, Arden NK, Cooper C, Javaid MK et al (2016) Impact of hip fracture on hospital care costs: a population-based study. Osteoporos Int 27(2):549–558
Brennan SL, Henry MJ, Kotowicz MA, Nicholson GC, Zhang Y, Pasco JA (2011) Incident hip fracture and social disadvantage in an Australian population aged 50 years or greater. Bone 48(3):607–610
Brennan SL, Yan L, Lix LM, Morin SN, Majumdar SR, Leslie WD (2015) Sex- and age-specific associations between income and incident major osteoporotic fractures in Canadian men and women: a population-based analysis. Osteoporos Int 26(1):59–65
Oliveira CM, Economou T, Bailey T, Mendonca D, Pina MF (2015) The interactions between municipal socioeconomic status and age on hip fracture risk. Osteoporos Int 26(2):489–498
Farahmand BY, Persson PG, Michaelsson K, Baron JA, Parker MG, Ljunghall S (2000) Socioeconomic status, marital status and hip fracture risk: a population-based case-control study. Osteoporos Int 11(9):803–808
Bacon WE, Hadden WC (2000) Occurrence of hip fractures and socioeconomic position. J Aging Health 12(2):193–203
Zingmond DS, Soohoo NF, Silverman SL (2006) The role of socioeconomic status on hip fracture. Osteoporos Int 17(10):1562–1568
Reyes C, Garcia-Gil M, Elorza JM, Fina-Aviles F, Mendez-Boo L, Hermosilla E et al (2015) Socioeconomic status and its association with the risk of developing hip fractures: a region-wide ecological study. Bone 73:127–131
Wu TY, Jen MH, Bottle A, Liaw CK, Aylin P, Majeed A (2011) Admission rates and in-hospital mortality for hip fractures in England 1998 to 2009: time trends study. J Public Health 33(2):284–291
Quah C, Boulton C, Moran C (2011) The influence of socioeconomic status on the incidence, outcome and mortality of fractures of the hip. J Bone Joint Surg 93(6):801–805
Smith P, Ariti C, Bardsley M (2013) Focus on hip fracture: trends in emergency admissions for fractured neck of femur, 2001 to 2011. The Health Foundation and Nuffield Trust
Curtis EM, van der Velde R, Moon RJ, van den Bergh JP, Geusens P, de Vries F et al (2016) Epidemiology of fractures in the United Kingdom 1988-2012: variation with age, sex, geography, ethnicity and socioeconomic status. Bone 87:19–26
Court-Brown CM, Aitken SA, Ralston SH, McQueen MM (2011) The relationship of fall-related fractures to social deprivation. Osteoporos Int 22(4):1211–1218
West J, Hippisley-Cox J, Coupland CA, Price GM, Groom LM, Kendrick D et al (2004) Do rates of hospital admission for falls and hip fracture in elderly people vary by socio-economic status? Public Health 118(8):576–581
Peters SA, Huxley RR, Woodward M (2014) Do smoking habits differ between women and men in contemporary Western populations? Evidence from half a million people in the UK Biobank study. BMJ Open 4(12):e005663
Wilsnack RW, Wilsnack SC, Kristjanson AF, Vogeltanz-Holm ND, Gmel G (2009) Gender and alcohol consumption: patterns from the multinational GENACIS project. Addiction 104(9):1487–1500
National Osteoporosis Society (2015) Effective secondary prevention of fragility fractures: clinical standards for fracture liaison services. National OsteoporosisSociety, Camerton.
Crisp A, Dixon T, Jones G, Cumming RG, Laslett LL, Bhatia K et al (2012) Declining incidence of osteoporotic hip fracture in Australia. Arch Osteoporos 7:179–185
Leslie WD, O'Donnell S, Jean S, Lagace C, Walsh P, Bancej C et al (2009) Trends in hip fracture rates in Canada. JAMA 302(8):883–889
Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB (2009) Incidence and mortality of hip fractures in the United States. JAMA 302(14):1573–1579
Balasegaram S, Majeed A, Fitz-Clarence H (2001) Trends in hospital admissions for fractures of the hip and femur in England, 1989-1990 to 1997-1998. J Public Health Med 23(1):11–17
Neuburger J, Wakeman R (2016) Is the incidence of hip fracture increasing among older men in England? J Epidemiol Community Health 70(10):1049–1050
van der Velde RY, Wyers CE, Curtis EM, Geusens PP, van den Bergh JP, de Vries F et al (2016) Secular trends in fracture incidence in the UK between 1990 and 2012. Osteoporos Int 27(11):3197–3206
Bender AM, Kawachi I, Jorgensen T, Pisinger C (2015) Neighborhood deprivation is strongly associated with participation in a population-based health check. PLoS One 10(6):e0129819
Health and Social Care Information Centre (2017) Hospital episodes statistics data dictionary: admitted patient care. http://content.digital.nhs.uk/media/25188/DD-APC-V10/pdf/DD-APC-V10.pdf.Accessed 17 March 2017
Department for Communities and Local Government (2011) The English indices of deprivation 2010. Department for Communities and Local Government, London
Armitage JN, van der Meulen JH (2010) Identifying co-morbidity in surgical patients using administrative data with the Royal College of Surgeons Charlson Score. Br J Surg 97(5):772–781
Carstairs V, Morris R (1989) Deprivation and mortality: an alternative to social class? Community Med 11(3):210–219
Hiscock R, Bauld L, Amos A, Fidler JA, Munafo M (2012) Socioeconomic status and smoking: a review. Ann N Y Acad Sci 1248:107–123
Huckle T, You RQ, Casswell S (2010) Socio-economic status predicts drinking patterns but not alcohol-related consequences independently. Addiction 105(7):1192–1202
Kanis J, Johnell O, Gullberg B, Allander E, Elffors L, Ranstam J et al (1999) Risk factors for hip fracture in men from southern Europe: the MEDOS study. Mediterranean Osteoporosis Study. Osteoporos Int 9(1):45–54
Public Health England (2013) Social and economic inequalities in diet and physical activity. Public Health England, London
Zhang Q, Wang Y (2004) Socioeconomic inequality of obesity in the United States: do gender, age, and ethnicity matter? Soc Sci Med 58(6):1171–1180
Tang X, Liu G, Kang J, Hou Y, Jiang F, Yuan W et al (2013) Obesity and risk of hip fracture in adults: a meta-analysis of prospective cohort studies. PLoS One 8(4):e55077
Department of Health (2004) Choosing Health: making healthier choices easier. Her Majesty's Stationery Office, London
Department of Health (2010) Healthy lives, healthy people: our strategy for public health in England
Marmot M (2010) Fair society, healthy lives: strategic review of health inequalities in England post-2010. University College London, London
National Institute for Health and Care Excellence (2012) Osteoporosis: assessing the risk of fragility fracture (Clinical Guideline 146). https://www.nice.org.uk/guidance/cg146. Accessed 17 March 2017
National Institute for Health and Care Excellence. Clinical knowledge summaries: osteoporosis—prevention of fragility fractures. https://cks.nice.org.uk/osteoporosis-prevention-of-fragility-fractures. Accessed 17 March 2017
Kanis JA, Svedbom A, Harvey N, McCloskey EV (2014) The osteoporosis treatment gap. J Bone Miner Res 29(9):1926–1928
Klop C, Gibson-Smith D, Elders PJ, Welsing PM, Leufkens HG, Harvey NC et al (2015) Anti-osteoporosis drug prescribing after hip fracture in the UK: 2000-2010. Osteoporos Int 26(7):1919–1928
Royal College of Physicians. The Falls and Fragility Fracture Audit Programme (FFFAP). http://www.fffap.org/FFFAP/landing.nsf/index.html. Accessed 17 March 2017
Åkesson K, Marsh D, Mitchell PJ, McLellan AR, Stenmark J, Pierroz DD, Kyer C, Cooper C, IOF Fracture Working Group (2013) Capture the fracture: a best practice framework and global campaign to break the fragility fracture cycle. Osteoporosis Int 24(8):2135–2152.
Gullberg B, Johnell O, Kanis JA (1997) World-wide projections for hip fracture. Osteoporos Int 7(5):407–413
Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR (2009) Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA 301(5):513–521
Jennings LA, Auerbach AD, Maselli J, Pekow PS, Lindenauer PK, Lee SJ (2010) Missed opportunities for osteoporosis treatment in patients hospitalized for hip fracture. J Am Geriatr Soc 58(4):650–657
Hussain S, Gunnell D, Donovan J, McPhail S, Hamdy F, Neal D et al (2008) Secular trends in prostate cancer mortality, incidence and treatment: England and Wales, 1975-2004. BJU Int 101(5):547–555
Shahinian VB, Kuo YF, Freeman JL, Goodwin JS (2005) Risk of fracture after androgen deprivation for prostate cancer. N Engl J Med 352(2):154–164
Office for National Statistics. Adult drinking habits in Great Britain (2014) https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/drugusealcoholandsmoking/datasets/adultdrinkinghabits. Accessed 8 March 2017
Department for Health (2012) Long term conditions compendium of information: Third Edition https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/216528/dh_134486.pdf.Accessed 18 March 2017
Schafer I, Hansen H, Schon G, Hofels S, Altiner A, Dahlhaus A et al (2012) The influence of age, gender and socio-economic status on multimorbidity patterns in primary care. First results from the multicare cohort study. BMC Health Serv Res 12:89
Li J, Green M, Kearns B, Holding E, Smith C, Haywood A et al (2016) Patterns of multimorbidity and their association with health outcomes within Yorkshire, England: baseline results from the Yorkshire Health Study. BMC Public Health 16:649
Nymark T, Lauritsen JM, Ovesen O, Rock ND, Jeune B (2006) Short time-frame from first to second hip fracture in the Funen County Hip Fracture Study. Osteoporos Int 17(9):1353–1357
Acknowledgements
The authors acknowledge Susan Charman for access to the Stata code that she developed for calculating the Royal College of Surgeons Charlson score. AB is supported by the Linda Edwards Memorial PhD studentship funded by the National Osteoporosis Society. CLG is funded by Arthritis Research UK (grant ref. 20000). YBS’s and TJ’s time is supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care West (CLAHRC West) at University Hospitals Bristol NHS Foundation Trust. JN is funded by an NIHR post-doctoral Fellowship (PDF-2013-06-078). The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
We obtained NHS Research Ethics Committee approval for this study (REC reference: 15/LO/1056).
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Bhimjiyani, A., Neuburger, J., Jones, T. et al. The effect of social deprivation on hip fracture incidence in England has not changed over 14 years: an analysis of the English Hospital Episodes Statistics (2001–2015). Osteoporos Int 29, 115–124 (2018). https://doi.org/10.1007/s00198-017-4238-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-017-4238-2