Abstract
Summary
The rate of change in bone density was not different between peri- and post-menopausal women. Differences in rate of change were observed in bone microarchitecture, specifically cortical porosity (Ct.Po), where peri-menopausal women increased +9% per year compared with the +6% per year for post-menopausal women.
Introduction
The purpose of this study was to compare changes in bone density and microarchitecture in peri- and post-menopausal women over 6 years.
Methods
Peri- (n = 26) and post- (n = 65) menopausal women were selected from the Canadian Multicenter Osteoporosis Study. Caucasian women were scanned on dual x-ray absorptiometry (DXA) and high-resolution peripheral quantitative computed tomography (HR-pQCT) at baseline and follow-up, an average 6 years later. To compare repeat scans, automated 3D image registration was conducted. At the radius and tibia, total volumetric BMD (Tt.BMD), total bone area (Tt.Ar) and cortical porosity (Ct.Po) were assessed, and finite element analysis estimated apparent bone strength.
Results
At the tibia, the rate of change for Ct.Po and Tt.Ar was different between groups. Peri-menopausal women had a + 9% per year increase in Ct.Po, but this increase was slower for post-menopausal women at +6% per year (p = 0.049). In addition, post-menopausal women had an increase in Tt.Ar of +0.13% per year compared with a slower increase of +0.06% per year for peri-menopausal women (p = 0.017). The rate of change of density between groups was not significantly different and was approximately −1% per year at the hip by DXA, and −1% per year at the radius and −0.5% per year tibia by HR-pQCT.
Conclusion
This is a 6-year prospective HR-pQCT study exploring rate of change in Caucasian peri- and post-menopausal women. The microarchitectural features represented by Ct.Po and Tt.Ar changed at a significantly different rate between groups, but group differences were not detected by density measures.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Menopause is the cessation of the menstrual period, which occurs on average at 51 years of age [1]. During the transition period, ovarian function changes and has been associated with symptoms such as hot flashes, tiredness, and mood swings [2] as well as loss of bone mineral density (BMD) [3]. Currently, menopause-related bone density changes have primarily been characterized by dual x-ray absorptiometry (DXA) [3–8]. While DXA is the clinical standard used to assess BMD [9], this methodology is two dimensional and is limited in its ability to differentiate trabecular and cortical bone or quantify bone microarchitecture, which influences bone strength [10].
High-resolution peripheral quantitative computed tomography (HR-pQCT) offers additional information on bone changes around menopause by measuring volumetric density and bone microarchitecture. In previous studies of pre- and post-menopausal women using HR-pQCT, it was shown that decreasing bone density is accompanied by decreasing cortical thickness, trabecular number, and trabecular thickness (Ct.Th, Tb.N, Tb.Th) [11] and increasing cortical porosity (Ct.Po) [12]. However, these changes in bone microarchitecture during menopause have been derived from cross-sectional data. Longitudinal HR-pQCT studies may provide more accurate data by accounting for secular differences such as lifestyle.
The purpose of this study was to use a longitudinal study design to compare changes in bone density and microarchitecture in peri- and post-menopausal women. Specifically, we will establish rate of change within and between these two groups of women.
Materials and methods
Participants
Participants (n = 91) were selected from a larger cohort of individuals participating in the Canadian Multicenter Osteoporosis Study (CaMos) in Calgary. The CaMos study is a nation-wide, prospective population-based study. Participants in the Calgary cohort (n > 460 at follow-up) are healthy men and women above the age of 16 years. Individuals whose bone metabolism may be affected by medications or other medical conditions were not included in the study. Based on questionnaire information provided at baseline [10], Caucasian women undergoing menopause at the time of the study comprised the peri-menopausal group (n = 26), and Caucasian women who had completed menopause comprised the post-menopausal group (n = 65) (Fig. 1). Informed consent was obtained from all individual participants included in the study, and the University of Calgary’s Conjoint Health Research Ethics Board approved all protocols. Details of the CaMos study protocols [13, 14] and Calgary cohort [10, 15] have been published previously.
Clinical assessments and questionnaire
An interview administered questionnaire provided information on the participant’s sociodemographic and medical information. This includes fracture history, family history, dietary information, and lifestyle habits. Weight and height were recorded to the nearest 0.1 kg and 0.1 cm. Menopause stage was assessed at baseline using a scale of 1 to 5. Women in stage 1 had no signs of starting menopause. The peri-menopausal group was defined as women in stages 2–4: just beginning, in the middle, or near the end of menopause, respectively. Stage 5 women had completed the midlife process (no menses for >12 months) and were included in the post-menopausal group.
Dual x-ray absorptiometry
DXA (Discovery W, Hologic, Bedford, MA) scans calculated areal bone mineral density (aBMD; g/cm2) of the left hip (total hip: TH), left femoral neck (FN), and lumbar spine (LS). Trained technologists conducted scanning and analysis. Daily and weekly calibrations and quality assurance assessments were performed following guidelines provided by the manufacturer. Technologists met acceptable precision scores according to the International Society for Clinical Densitometry 2015 position statement of 1.9% for the lumbar spine, 1.8% for the total hip, and 2.5% for the femoral neck (www.ISCD.org).
Image registration
In order to compare common regions between baseline and follow-up scans, image registration was performed for all parameters with the exception of finite element analysis (Image Processing Language, v5.42), rather than the standard slice-matching method provided by the manufacturer. The gray scale images were registered using a 3D rigid body transformation derived from a mutual information metric and linear interpolation. Registration allowed for common regions of interest to be determined and periosteal, trabecular, and cortical masks to be created for further analysis. Baseline contours were used at baseline and follow-up contours were used at follow-up. Scans were included in this study if the common region between baseline and follow-up was 75% or greater.
High-resolution peripheral quantitative computed tomography
HR-pQCT (XtremeCT, Scanco Medical, Brüttisellen, Switzerland) scans of the radius and tibia were performed at baseline and follow-up, following our previously published method [10, 15]. Scans at 81-μm nominal isotropic resolutions were performed at a standard location below reference lines, determined using a scout image. For radius scans, the reference line was placed at the mid-inclination tuberosity and the scan taken 9.5 mm proximal to this location. For tibia scans, the scan was done 22.5 mm proximal to the reference line, placed at the plateau of the tibia endplate. Each scan consists of 110 slices, or a 9.02 mm length, taken with a standard human in vivo protocol (60 kVp, 1000 μA, 100 ms integration time). The patient’s left tibia and non-dominant radius were scanned, unless they had experienced a previous fracture. In the case of a fracture, the opposite limb was scanned.
Trained technologists conducted all HR-pQCT scans. CVs range from <1% for density measures to 4% for microarchitecture parameters in our laboratory [16], although a different image registration method was used for this study. During analysis, motion artifacts were recorded: a score of 5 corresponds to distortion and severe blurring while a score of 1 corresponds to no motion. Only scans with low motion score of 1–3 were used in analysis [17]. A standard morphological analysis was done following the manufacturer’s method to determine primary morphological parameters. This includes total and trabecular volumetric bone mineral density (Tt.BMD and Tb.BMD; mg HA/cm3), trabecular number (Tb.N; mm−1), and trabecular thickness, (Tb.Th; mm) [11], described in detail elsewhere [10]. An automated segmentation method which distinguishes periosteal and endosteal cortex of the cortical shell [12] was used to determine cortical parameters. This includes total cross-sectional area (Tt.Ar; mm), cortical volumetric BMD (Ct.BMD; mg HA/cm3), cortical thickness (Ct.Th; mm) and cortical porosity (Ct.Po; %) [18, 19].
Finite element analysis
Radius and tibia scans were analyzed using custom finite element analysis (FEA) software (FAIM, version 6.0, Numerics88 Solutions, Calgary, Canada) to estimate failure load (N) [20]. Scans were segmented and filtered using a Laplace-Hamming filter to generate a linear homogeneous mesh [21]. Young’s modulus of 6829 MPa, Poisson’s ratio of 0.3, and a uniaxial strain of 1% were used [21, 22]. FEA was performed on unregistered images due to image registration causing non-parallel surfaces.
Statistical analysis
The changes within each group over time and differences in rate of change between groups were investigated (R, version 0.99.489). To compare the change from baseline to follow-up within each group, paired T-tests compared the baseline value to the follow-up value for each parameter. To assess rates of change between groups, the percent change per year for each parameter was calculated and then compared using independent sample t-tests. Chi-square was used for categorical variables.
Linear regression was used to determine if age, the number of years past final menstrual period and osteoporotic medication influence rate of change between groups. Sub-analyses were performed on women with and without hysterectomy and oophorectomy. Results are reported as mean values with 95% confidence interval. A p value <0.05 was considered to be significant.
Results
Descriptive characteristics at baseline are shown in Table 1. Eleven of the peri-menopausal women were in stage 2, four were in stage 3, and eleven were in stage 4. Our post-menopausal group was 15 years past final menstrual period and was older and more likely to be taking osteoporosis-based medication than the peri-menopausal group. All women taking osteoporotic medication were on bisphosphates, irrespective of group. Height, weight, and BMI did not change significantly during the study; however, there was a non-significant trend for weight to increase in peri-menopausal women, and height to decrease in post-menopausal women.
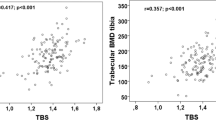
Baseline scan data are presented in Table 2. One woman did not complete DXA scans. Furthermore, one LS scan was excluded, as unreliable, due to degenerative changes (osteophytes) in the spine. There were no differences between groups for DXA aBMD at baseline. For HR-pQCT scans, seven radius and two tibia scans were removed due to motion scores exceeding our criteria. In addition, two radius and three tibia scans were removed from analysis due to scan abnormality (large holes in the trabecular bone region) or artifact. There was no between-group difference in the percent overlap of baseline and follow-up scan regions (radius 90% overlap; tibia 94% overlap). At the radius, baseline results show post-menopausal women had lower BMD (Tt.BMD and Ct.BMD), Tb.N, Ct.Th, Ct.Ar and failure load than peri-menopausal women, with higher Ct.Po. At the tibia, post-menopausal women had lower BMD (Tt.BMD and Ct.BMD) and higher Ct.Po than peri-menopausal women.
Change data were normalized as percent change per year and results are shown for between and within groups in Table 3. The time between scans was 5.8 ± 0.7 years for the peri-menopausal women and 5.4 ± 0.4 years for the post-menopausal women.
Rate of change within groups
Over the duration of the study, BMD (DXA and HR-pQCT) decreased by −0.4 to −1.2% per year for both groups. Ct.Th decreased (<1%) while Ct.Po increased (+6 to +11%). Ct.Ar decreased (radius only) and Tb.Ar increased. Failure load decreased over the duration of the study for post-menopausal women at the radius (−0.6% per year), but did not significantly change at the tibia.
Rate of change between groups
At the tibia, there were significant differences in the rate of change between groups for Ct.Po and Tt.Ar. Peri-menopausal women had a + 9% per year increase in Ct.Po compared with +6% per year for post-menopausal women. In addition, post-menopausal women had an increase in Tt.Ar of +0.13% per year compared with +0.06% per year for peri-menopausal women. The rate of change between groups was not significantly different for any other microarchitecture, density, geometry, or strength measures at all skeletal sites measured. Other than menopause status, age, the number of years past final menstrual period, and osteoporotic medication did not contribute to rate of change differences between groups.
After performing sub-analyses on women with and without hysterectomy and oophorectomy, differences between groups emerged at the radius. Post-menopausal women with a hysterectomy lost Tb.BMD at a larger rate than peri-menopausal women with hysterectomy (−0.6% per year, p < 0.05). The same result was observed for women following hysterectomy or oophorectomy (−0.5% per year, p < 0.05). In addition, post-menopausal women with hysterectomy lost Tb.Th at a higher rate than peri-menopausal women with hysterectomy (−1.2% per year, p < 0.05). Again, the same result was observed for women following hysterectomy or oophorectomy (−1.1% per year, p < 0.05). At the tibia, post-menopausal women without hysterectomy had larger increases in Tt.Ar than peri-menopausal women without hysterectomy (+0.1% per year, p < 0.05). Post-menopausal women with hysterectomy or oophorectomy lost Tb.BMD and Tb.Th faster than peri-menopausal women at the radius and do not gain bone size at the tibia.
Discussion
This study estimated the average annual percent change in bone density and microarchitecture parameters for peri- and post-menopausal women over 6 years. While many bone parameters changed over the duration of this study, differences in rate of change were statistically different between the peri- and post-menopausal women for two microarchitectural parameters at the tibia. Specifically, cortical porosity increased at a higher rate in peri- compared with post-menopausal women, and total area increased at a higher rate in post- compared with peri-menopausal women. There were no differences in rate of change at the hip and spine using DXA.
Changes in BMD throughout the menopause transition from DXA-based studies are inconsistent due to the methodological variances in study design—cross-sectional [4] compared with longitudinal [3, 8, 23–25] studies—and different group comparisons: pre- to post- menopausal [4, 23], pre- to peri-menopausal [7, 24], and peri- to post-menopausal [3, 8, 26]. Using DXA, we found that both groups lost BMD at the hip at a rate of approximately 1% per year, and at the spine, post-menopausal women reported a slight increase in BMD. This increase in lumbar spine BMD may be attributed to the degenerative changes known to occur during the aging process [27]. We did not observe differences in rate of change between peri- and post-menopausal groups, which may be due to the limitation of using a 2D projection method such as DXA.
There were significant differences in microarchitectural parameters at the tibia that may be indicative of accelerated remodeling during the menopause transition. Using HR-pQCT, we found an increased rate of cortical porosity in peri- compared with post-menopausal women, whereas we failed to observe differences in rate of change of trabecular microarchitecture within groups at the tibia. These data suggest that within the age range of our participants, cortical bone changes occur at a higher rate than trabecular bone changes. Similar results have previously been observed following menopause [28, 29]. The increased rate of change in Ct.Po observed in peri-menopausal women is consistent with data showing increased bone remodeling due to estrogen deficiency [30], and is thought to be associated with cortical bone loss [31]. The fact that the trabecular area increased and the cortical area decreased during the transition, coupled with the increased cortical porosity, suggests that endocortical remodeling likely underpins the cortical bone loss.
All the women in our study displayed increased cortical porosity coupled with decreased cortical thickness, both of which have been linked to fracture risk in post-menopausal women [12]. As noted, these women had increased trabecular area and an overall increase in total bone size at the tibia. The fact that we did not find a significant change in bone strength over time may be because the increase in bone size helped maintain bone strength [32].
The differences we observed at the tibia are statistically relevant with respect to the detection limits of the scanning protocol. Remembering that the percent change values we presented are representative of annual changes, over the duration of the study, which was approximately 6 years, the changes we observed were larger than the precision error of the scanner. Previously reported root mean square coefficient of variation (RMSCV) values were 0.1% at the radius and tibia for total area whereas cortical porosity RMSCV were 11.7% at the radius and 3.9% at the tibia for an elderly population [19]. In addition, our absolute change was also greater than the least significant change (LSC) [19]. It appears that cortical porosity is a useful parameter that is sensitive to bone remodeling activity.
Although the tibia showed between-group differences in the rate of change, it is important to note that an overall larger annual change was observed at the radius than tibia (e.g. Tt.BMD radius −1%, tibia −0.5%), and has been shown elsewhere [29]. The larger overall change at the radius accompanied by maintained bone size and decreased bone strength suggests a link to elevated fracture risk at the radius over the tibia. It is possible that this non-weight-bearing bone has higher sensitivity to the effect of estrogen and hormonal influences leading to greater bone changes surrounding menopause. Such effects may be blunted at the tibia due to daily mechanical loading.
Few studies have used HR-pQCT to explore skeletal changes longitudinally [29, 33]. The annual rates of change we report in post-menopausal women are similar for density measures [29] but differ for trabecular microarchitecture [29, 33]. While other studies reported changes in trabecular number [29, 33], thickness and separation [33] at the radius in post-menopausal women, we only observe changes in trabecular microarchitecture following sub-analyses for hysterectomy or oophorectomy. Furthermore, compared with one study [29], the annual change in cortical porosity was higher in our study (radius +7 vs. +10%, tibia +3 vs. +6%) and failure load was slightly lower (radius −0.9 vs. −0.6%, tibia −0.5 vs. −0.3%). The differences in trabecular thickness and separation between studies may arise due to the fact that these parameters are derived in first generation HR-pQCT scanners. In addition, sample size, duration of follow-up, age of participants, and years since final menstrual period were different between studies and may account for deviating findings. Participants in our study had a 6-year follow-up whereas others had a 3-year [29] or 1-year [33] follow-up. The post-menopausal participants in our study were younger than previously reported [33] and therefore might have been closer in time to final menstrual period and less likely to report hysterectomy or oophorectomy, although such information was not provided [29, 33]. All three studies report very different post-menopausal changes in trabecular number at the radius: −6.4% per year [33], −0.82% per year [29], and +0.1% per year in this study. Interestingly, the largest change was observed in the 1-year study and the smallest changes in the 6-year study. The effect of anti-resorptive medication, hysterectomy and/or oophorectomy cannot be ruled out as causes for these differences.
The advantage of a longer follow-up time is that precision errors are minimized; however, it can also span periods of time that include fast as well as slower changes. We know that differences in rates of bone loss may occur up to 10 years after final menstrual period, with the greatest bone loss reported 2–4 years following final menstrual period [8, 28], around 50–54 years [34]. We did not observe differences in rate of change since final menstrual period in our study; however, with the majority of our participants being 5 to 15 years post-menopausal, we may have been underpowered to report differences outside this range. As trabecular bone is known to react to hormonal changes faster than cortical bone [35], it is possible the timeframe of our measurements may have been too late to detect changes in trabecular bone. It is possibly a limitation of our study that we did not focus on post-menopausal women that were closer in time (<5 years) to their final menstrual period, which may have led to additional and greater differences in rate of changes between groups.
Biochemical monitoring of bone metabolism and hormonal activity fell outside the scope of this study and are therefore noted as a limitation of the current study. Menopause stage was determined by a research-nurse following an interview administered questionnaire. We acknowledge the subjective nature of this assessment and for this reason chose not to stratify data by menopause stage. While we performed sub-analyses for women with hysterectomy and hysterectomy or oophorectomy, we did not have a large enough sample to look at women with oophorectomy without hysterectomy (two women). In addition, the small sample size of the peri-menopausal group is a limiting factor. Finally, although this study spans 6 years, we were unable to capture the entire menopause transition as women passed from pre- through to post-menopausal. Future studies should aim to encompass the entire menopause transition, explore differences between ethnicities, consider having a post-menopausal group within 5 years of the final menstrual period, and capture changes to both cortical and trabecular bone at weight-bearing and non-weight-bearing skeletal sites.
In conclusion, this study compared changes in bone density and microarchitecture parameters in peri- and post-menopausal Caucasian women over 6 years. We found that cortical porosity increased at a higher rate in peri- compared with post-menopausal women, and total area increased at a higher rate in post- compared with peri-menopausal women. Over the duration of the study, bone quality declined for both peri- and post-menopausal women at the hip, radius, and tibia, which is consistent with cross-sectional study findings. It appears that cortical porosity is a sensitive microarchitectural parameter to the bone changes that occur during the menopause transition and may be a useful marker for prevention and treatment of bone quality during aging.
References
Greendale GA, Lee NP, Arriola ER (1999) The menopause. Lancet 353:571–580. doi:10.1016/S0140-6736(98)05352-5
Xu J, Bartoces M, Neale AV et al (2005) Natural history of menopause symptoms in primary care patients: a MetroNet study. J Am Board Fam Pract 18:374–382. doi:10.3122/jabfm.18.5.374
Finkelstein JS, Brockwell SE, Mehta V et al (2008) Bone mineral density changes during the menopause transition in a multiethnic cohort of women. J Clin Endocrinol Metab 93:861–868. doi:10.1210/jc.2007-1876
Arlot ME, Sornay-Rendu E, Garnero P et al (1997) Apparent pre-and postmenopausal bone loss evaluated by DXA at different skeletal sites in women: the OFELY cohort. J Bone Miner Res 12:683–690. doi:10.1359/jbmr.1997.12.4.683
Soda M-Y, Mizunuma H, Honjo S-I et al (1993) Pre- and postmenopausal bone mineral density of the spine and proximal femur in Japanese women assessed by dual-energy X-ray absorptiometry: a cross-sectional study. J Bone Miner Res 8:183–189. doi:10.1002/jbmr.5650080209
Warming L, Hassager C, Christiansen C (2002) Changes in bone mineral density with age in men and women: a longitudinal study. Osteoporos Int 13:105–112. doi:10.1007/s001980200001
Chapurlat RD, Garnero P, Sornay-Rendu E et al (2000) Longitudinal study of bone loss in pre- and perimenopausal women: evidence for bone loss in perimenopausal women. Osteoporos Int 11:493–498. doi:10.1007/s001980070091
Guthrie JR, Ebeling PR, Hopper JL et al (1998) A prospective study of bone loss in menopausal Australian-born women. Osteoporos Int 8:282–290. doi:10.1007/s001980050066
Kanis JA (2002) Diagnosis of osteoporosis and assessment of fracture risk. Lancet 359:1929–1936. doi:10.1016/S0140-6736(02)08761-5
Macdonald HM, Nishiyama KK, Kang J et al (2011) Age-related patterns of trabecular and cortical bone loss differ between sexes and skeletal sites: a population-based HR-pQCT study. J Bone Miner Res 26:50–62. doi:10.1002/jbmr.171
Boutroy S, Bouxsein ML, Munoz F, Delmas PD (2005) In vivo assessment of trabecular bone microarchitecture by high-resolution peripheral quantitative computed tomography. J Clin Endocrinol Metab 90:6508–6515. doi:10.1210/jc.2005-1258
Nishiyama KK, Macdonald HM, Buie HR et al (2010) Postmenopausal women with osteopenia have higher cortical porosity and thinner cortices at the distal radius and tibia than women with normal aBMD: an in vivo HR-pQCT study. J Bone Miner Res 25:882–890. doi:10.1359/jbmr.091020
Kreiger N, Tenenhouse A, Joseph L et al (1999) The Canadian multicentre osteoporosis study (CaMos): background, rationale, methods. Can J Aging 18:376–387
Tenenhouse A, Kreiger N, Hanley D (2000) Canadian multicentre osteoporosis study (CaMos). Drug Develop Res 49:201–205. doi:10.1002/(SICI)1098-2299(200003)49:3<201::AID-DDR10>3.0.CO;2-O
Burt LA, Macdonald HM, Hanley DA, Boyd SK (2014) Bone microarchitecture and strength of the radius and tibia in a reference population of young adults: an HR-pQCT study. Arch Osteoporos 9:183–189. doi:10.1007/s11657-014-0183-2
MacNeil JA, Boyd SK (2008) Improved reproducibility of high-resolution peripheral quantitative computed tomography for measurement of bone quality. Med Eng Phys 30:792–799. doi:10.1016/j.medengphy.2007.11.003
Pauchard Y, Liphardt A-M, Macdonald HM et al (2012) Quality control for bone quality parameters affected by subject motion in high-resolution peripheral quantitative computed tomography. Bone 50:1304–1310. doi:10.1016/j.bone.2012.03.003
Buie HR, Campbell GM, Klinck RJ et al (2007) Automatic segmentation of cortical and trabecular compartments based on a dual threshold technique for in vivo micro-CT bone analysis. Bone 41:505–515. doi:10.1016/j.bone.2007.07.007
Burghardt AJ, Buie HR, Laib A et al (2010) Reproducibility of direct quantitative measures of cortical bone microarchitecture of the distal radius and tibia by HR-pQCT. Bone 47:519–528. doi:10.1016/j.bone.2010.05.034
Pistoia W, van Rietbergen B, Laib A, Rüegsegger P (2001) High-resolution three-dimensional-pQCT images can be an adequate basis for in-vivo μFE analysis of bone. J Biomech Eng 123:176–183. doi:10.1115/1.1352734
MacNeil JA, Boyd SK (2008) Bone strength at the distal radius can be estimated from high-resolution peripheral quantitative computed tomography and the finite element method. Bone 42:1203–1213. doi:10.1016/j.bone.2008.01.017
Pistoia W, van Rietbergen B, Lochmüller EM et al (2002) Estimation of distal radius failure load with micro-finite element analysis models based on three-dimensional peripheral quantitative computed tomography images. Bone 30:842–848. doi:10.1016/S8756-3282(02)00736-6
Ahlborg HG, Johnell O, Nilsson BE et al (2001) Bone loss in relation to menopause: a prospective study during 16 years. Bone 28:327–331. doi:10.1016/S8756-3282(00)00451-8
Sowers M, Crutchfield M, Bandekar R et al (1998) Bone mineral density and its change in pre- and perimenopausal white women: the Michigan bone health study. J Bone Miner Res 13:1134–1140. doi:10.1359/jbmr.1998.13.7.1134
Greendale GA, Sowers M, Han W et al (2012) Bone mineral density loss in relation to the final menstrual period in a multiethnic cohort: results from the Study of Women’s Health Across the Nation (SWAN). J Bone Miner Res 27:111–118. doi:10.1002/jbmr.534
Guthrie JR, Dennerstein L, Taffe JR et al (2010) The menopausal transition: a 9-year prospective population-based study. The Melbourne Women's Midlife Health Project Climacteric 7:375–389. doi:10.1080/13697130400012163
Tenne M, McGuigan F, Besjakov J et al (2013) Degenerative changes at the lumbar spine—implications for bone mineral density measurement in elderly women. Osteoporos Int 24:1419–1428. doi:10.1007/s00198-012-2048-0
Recker R, Lappe J, Davies K, Heaney R (2000) Characterization of perimenopausal bone loss: a prospective study. J Bone Miner Res 15:1965–1973. doi:10.1359/jbmr.2000.15.10.1965
Shanbhogue VV, Brixen K, Hansen S (2016) Age- and sex-related changes in bone microarchitecture and estimated strength. A three-year prospective study using HRpQCT. J Bone Miner Res 31:n/a–n/a. doi: 10.1002/jbmr.2817
Recker R, Lappe J, Davies KM, Heaney R (2004) Bone remodeling increases substantially in the years after menopause and remains increased in older osteoporosis patients. J Bone Miner Res 19:1628–1633. doi:10.1359/JBMR.040710
Riggs BL, Melton LJ, Robb RA et al (2008) A population-based assessment of rates of bone loss at multiple skeletal sites: evidence for substantial trabecular bone loss in young adult women and men. J Bone Miner Res 23:205–214. doi:10.1359/jbmr.071020
Ahlborg HG, Johnell O, Turner CH et al (2003) Bone loss and bone size after menopause. N Engl J Med 349:327–334. doi:10.1056/NEJMoa022464
Kawalilak CE, Johnston JD, Olszynski WP, Kontulainen SA (2014) Characterizing microarchitectural changes at the distal radius and tibia in postmenopausal women using HR-pQCT. Osteoporos Int 25:2057–2066. doi:10.1007/s00198-014-2719-0
Berger C, Langsetmo L, Joseph L et al (2008) Change in bone mineral density as a function of age in women and men and association with the use of antiresorptive agents. Can Med Assoc J 178:1660–1668. doi:10.1503/cmaj.071416
Seifert-Klauss V, Fillenberg S, Schneider H et al (2012) Bone loss in premenopausal, perimenopausal and postmenopausal women: results of a prospective observational study over 9 years. Climacteric 15:433–440. doi:10.3109/13697137.2012.658110
Acknowledgements
The authors would like to thank all the participants who graciously devoted time to participate in the study, Anne Cooke and Taryn Harris for the scan acquisition, Duncan Raymond for recruitment and scan analysis, and Jane Allan and Bernice Love for their assistance in participant recruitment and administering the extensive interview-based questionnaire.
This study was funded by the Canadian Institutes of Health Research (CIHR) MOP-106611.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed consent was obtained from all individual participants included in the study, and the University of Calgary’s Conjoint Health Research Ethics Board approved all protocols.
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Burt, L.A., Bhatla, J.L., Hanley, D.A. et al. Cortical porosity exhibits accelerated rate of change in peri- compared with post-menopausal women. Osteoporos Int 28, 1423–1431 (2017). https://doi.org/10.1007/s00198-016-3900-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-016-3900-4