Abstract
Summary
We evaluated the prevalence of osteoporosis using the osteoporosis diagnostic criteria developed by the National Bone Health Alliance (NBHA), which includes qualified fractures, FRAX score in addition to bone mineral density (BMD). The expanded definition increases the prevalence compared to BMD alone definitions; however, it may better identify those at elevated fracture risk.
Purpose
The purpose of this paper is to estimate the prevalence of osteoporosis in US adults ≥50 years using the NBHA osteoporosis diagnostic criteria.
Methods
Utilizing 2005–2008 data of the National Health and Nutrition Examination Survey (NHANES), we identified participants with osteoporosis with any one of the following: (1) femoral neck or lumbar spine T-score ≤ −2.5; (2) low trauma hip fracture irrespective of BMD or clinical vertebral, proximal humerus, pelvis, or distal forearm fracture with a T-score >−2.5 <−1.0; or (3) FRAX score at the National Osteoporosis Foundation intervention thresholds (≥3% for hip fracture or ≥20% for major osteoporotic fracture). We estimated the prevalence overall and by gender and age.
Results
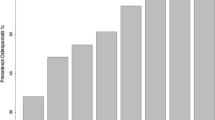
Our sample included 1948 (54.3%) men and 1639 (45.7%) women. Approximately 12% were 80+ years and 21% were from racial/ethnic minority groups. We estimated that 16.0% (0.8) of men and 29.9% (1.0) of women 50+ years have osteoporosis. The prevalence increases with age to 46.3% in men and 77.1% in women 80+ years. The combination of FRAX score and fractures was the largest contributing factor defining osteoporosis in men (70–79, 88.1%; 80+, 80.1%), whereas T-score was the largest contributing factor in women (70–79, 49.2%; 80+, 43.5%).
Conclusions
We found that 16% of men and 29.9% of women 50+ have osteoporosis based on the NBHA diagnostic criteria. Although the expanded definition increases the prevalence compared to BMD alone-based definitions, it may better identify those at elevated fracture risk in order to reduce the burden of fractures in older adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis has been defined as a skeletal disorder of reduced bone strength that leads to an increased risk for fracture, typically with a relatively low level of trauma such as a fall from standing height [1]. It has recently been estimated that 10.3% of adults 50 years and older in the USA have osteoporosis when the diagnosis is based upon measurements of bone mineral density (BMD) at the femur neck and/or lumbar spine with a T-score of ≤−2.5 [2]. However, certain low trauma fractures, particularly those of the hip and spine, are included in many national [3] and international [4] osteoporosis treatment guidelines since these types of fractures are recognized as indicative of osteoporosis in the absence of a BMD T-score meeting the diagnostic threshold. The exclusion of these and other fragility fractures from the diagnostic definitions would likely underestimate the true prevalence of osteoporosis. In addition, the role of clinical risk factors for low trauma fractures and their future fracture predictive ability has been clearly demonstrated with the creation and wide utilization of the FRAX algorithm [5]. FRAX has been incorporated into intervention guidelines, and in the USA, thresholds have been created to assist in treatment decisions for individuals age 40 and older who have low bone mass [3].
With these principles in mind, the National Bone Health Alliance (NBHA), a public-private partnership created in response the US Surgeon General’s Report on Bone Health and Osteoporosis [6] and led by the American Society for Bone and Mineral Research (ASBMR) and the National Osteoporosis Foundation (NOF), recently assigned a working group of 17 clinicians and clinical scientists to consider the possibility of an expansion of the criteria for the clinical diagnosis of osteoporosis for use in the USA. A position statement reflecting the consensus of the working group has been published [7]. The NBHA position states that in postmenopausal women and in men age 50 and older in the USA, osteoporosis may be diagnosed based on any one of three elements: traditional BMD based T-score of ≤−2.5 at the hip (total hip or femoral neck) or lumbar spine, a qualifying low trauma fracture, or a FRAX score meeting or exceeding the recommended treatment intervention cut points in persons with low BMD (T-score >−2.5 <−1.0) used in the USA. The qualifying low trauma fractures include hip, irrespective of BMD, and clinical vertebral, proximal humerus, pelvis, and in some cases distal forearm in individuals with low BMD (osteopenia). Morphometric vertebral fracture may be a qualifying fracture in someone with low bone mass if the clinician believes it to have been the result of reduced bone strength. The FRAX cut points chosen as diagnostic indicators of osteoporosis reflect the two being used as treatment intervention thresholds in the current NOF Clinician’s Guide, namely ≥3% 10 year absolute risk for hip fracture or ≥20% for major osteoporotic fracture in older US adults [3].
The new diagnostic criteria for osteoporosis recommended by NBHA have been endorsed by several national organizations including the NOF and the ASBMR as well as several professional societies whose members diagnose and treat osteoporosis, including the American Academy of Orthopaedic Surgeons, the US contingent of the International Society for Clinical Densitometry, and the Endocrine Society. However, it is not known how the expansion of the diagnostic criteria might affect prevalence estimates. The purpose of this paper is to estimate the proportion of the population of US postmenopausal women and men age 50 and older who would be identified as having a clinical diagnosis of osteoporosis based upon the expanded criteria recommended by the NBHA.
Methods
This study was performed using 2005–2008 data from the National Health and Nutrition Examination Survey (NHANES). The NHANES are conducted by the National Center for Health Statistics (NCHS), Centers for Disease Control and Prevention, to assess the health and nutritional status of large representative cross-sectional samples of the non-institutionalized, US civilian population. The analytic sample consisted of individuals 50 years and older, without missing information on any data element used in the NBHA definition.
Elements of NBHA definition
Bone mineral density
BMD testing was performed by every NHANES center on a sample of participants ≥8 years of age [8]. The anterior–posterior lumbar spine and femoral neck were measured with Hologic QDR 4500A fan-beam densitometers (Hologic, Inc., Bedford, MA) using Apex version 3.0 software (lumbar spine) or Discovery version 12.4 software (femur neck) as described elsewhere [9, 10]. The left hip was scanned unless there was a history of previous fracture or surgery, and scanning was done in the fast mode. Quality control (QC) programs included the use of anthropomorphic phantoms. Review of each QC and respondent scan were completed at a central site (Department of Radiology of the University of California, San Francisco), using standard radiologic techniques and study-specific protocols developed for the NHANES [11, 12]. Bone density T-scores were calculated as (respondent’s BMD − reference group mean BMD)/reference group standard deviation [SD]). The reference group for the femoral neck consisted of non-Hispanic White women aged 20–29 years from NHANES III, [13] while the reference group for the lumbar spine consisted of 30-year-old White females from the dual-energy X-ray absorptiometry (DXA) manufacturer reference database [14]. Using T-scores identified by the World Health Organization, [15] osteoporosis was defined as a T-score −2.5 or below at either the femoral neck or lumbar spine.
Qualifying low trauma fractures
NHANES participants self-reported hip, wrist (representing distal radius/ulna), and spine fractures based on the following question: “Has a physician ever told you that you had broken or fractured the specific site? [16]” If yes, participants were asked the number of times they broke each site, the age, and circumstances associated with each fracture. Circumstance categories consisted of “a fall from standing height or less (for example, tripped, slipped, fell out of bed); a hard fall (such as falling off a ladder or step stool, down stairs); or a car accident or other severe trauma” [16]. Other fracture sites were determined based on the question “Has a doctor ever told you that you had broken or fracture any other bones after 20 years of age?” If yes, respondents were first asked how much trauma was involved. Skeletal location and age at fracture were only asked for fractures that were due to “non-severe” trauma, i.e., those not resulting from car accidents or “hard falls” [16].
According to the NBHA criteria qualifying low trauma fractures include hip, clinical vertebral, proximal humerus, pelvis and some distal forearm in the presence of low BMD [7]. We did not have access to chest or lumbar radiographs to identify morphometric vertebral fractures and relied on self-report of spine fractures that the participant reported occurring after the age of 50 alone. We used patients reporting humerus and shoulder fractures occurring after the age of 50, who also had low BMD to represent qualifying proximal humerus fractures. It was previously suggested by the NBHA authors that there is potential for misclassification around the relationship of wrist fractures with osteoporosis in participants 50–59 [7], particularly given the circumstances around the fracture, e.g., trip and fall versus fall from skiing accident. Although trauma was reported by NHANES participants, to minimize misclassification and for purposes of these analyses to reduce overdiagnosing osteoporosis, we only considered those wrist fractures occurring in participants reporting fractures occurring at ≥60 years of age in the presence of low bone density as a qualifying fracture.
FRAX score
FRAX score is calculated based on BMD (or BMI when BMD is not available) and the following clinical factors: age, race/ethnicity, history of previous fracture, parental history of hip fracture, cigarette smoking, alcohol intake, use of systemic glucocorticoids, and rheumatoid arthritis. Since BMD measurements were available in this sample, other secondary causes of osteoporosis were not included, as per the FRAX algorithm. The operation of these variables in NHANES for calculation of FRAX scores has been previously summarized [17]. The 10-year probability for hip and major osteoporotic fractures was calculated using FRAX version 3.0. We identified those who met or exceeded the NOF intervention thresholds of a 10-year absolute risk of hip fracture of ≥3% or of major osteoporotic fracture ≥20% based upon the FRAX calculation.
Statistical analysis
We calculated the proportions meeting the qualifying elements of the NBHA diagnostic criteria overall, by gender and age. Each element was considered mutually exclusive, so participants were not counted twice. We estimated the prevalence of osteoporosis according to the NBHA diagnostic criteria overall and by gender and age. We used linear regression to test for trends in the prevalence of osteoporosis by age. We estimated the contributions of each element of the NBHA diagnostic criteria stratified by gender and age. We compared the proportions of each element of the criteria by gender using the chi-square test. All age-standardized estimates were calculated using the age distribution from the US Census 2000 population. All analyses used sample weights and took into account the complex design of the survey. All analyses were conducted with PC-SAS (version 9.2, SAS Institute, Cary, NC) and SUDAAN (version 10.0, Research Triangle Institute, NC).
Results
The 2005–2008 NHANES data included 7532 adults ≥50 years of age, of which 5288 (70.2%) were interviewed (Fig. 1). DXA examinations were performed on 5055 (95.6%) of the interviewed participants. Our study sample included 3587 adults with non-missing information on DXA, fracture, or any of the variables used for the FRAX score calculation (Fig. 1.) This represented 1948 (54.3%) men and 1639 (45.7%) postmenopausal women (Table 1). Approximately, a third of the sample was 50–59 years (30.6%) and 34.9% was between 60 and 69 years of age. The majority of the sample was non-Hispanic White (78.9%), with 8.7% representing non-Hispanic Blacks, 4.5% Mexican Americans, and 8.0% other races and ethnicities (Table 1).
Of the sample, 552 (15.4%) individuals reported having a fracture at ≥20 years of age (Fig. 1). However, only 153 (27.7%) of individuals reported that the fracture occurred ≥50 years of age, of which 88 (57.5%) were due to low trauma. Two participants reported two fractures at two different sites, so we only counted them once, leaving the final number of our sample reporting a fracture as 86 (2.4%).
The prevalence of each of the elements in the NHBA diagnostic categories is shown in Table 2. The prevalence and standard error (SE) of osteoporosis based on BMD at the femoral neck or the lumbar spine alone were 4.0% (0.45) in men and 15.5% (0.81) in women. The prevalence of osteoporosis at the femoral neck or lumbar spine was higher with increasing age (Table 2). For example in men, the prevalence was 3.3% in men 50–59 years of age and was 9.2% in men 80+. In women, the prevalence was 8.4% in women 50–59 years of age and was 33.6% in women 80+ years of age. This increasing trend with age was statistically significant in women only.
The prevalence of osteoporosis based on qualifying fractures in individuals with low BMD alone was statistically unreliable given the sample size overall and by age group, particularly in men. In women, 1.3% (0.37) had osteoporosis through qualifying fractures alone overall. When examining by age, the 70–79 age group was the only group with enough data to provide statistically reliable estimates, with 2.9% (0.78) having osteoporosis through qualifying fractures alone.
With respect to FRAX, overall, 11.6% (0.83) of men and 13.0% (0.97) of women 50+ years had osteoporosis based on a FRAX score at or above the NBHA diagnostic threshold (Table 2). Similar to the prevalence of osteoporosis based on DXA data alone, the prevalence of osteoporosis based on having a qualifying FRAX score increased with age. However, unlike the DXA data, this trend was statistically significant in both men and women, with the prevalence of osteoporosis based on having a qualifying FRAX score alone increasing from 2.0 to 34.0% in men 50–59 to 80+ years of age (p = 0.001) and from <1 to 41% in women 50–59 to 80+ years of age (p = 0.001), respectively (Table 2).
Patterns observed in non-Hispanic Whites were similar to those in the total study sample for the prevalence of osteoporosis based on each of the three elements both overall and by age (Table 2). Examinations in other racial and ethnic groups could not be performed due to small sample sizes.
Based upon the presence of any one of the three elements for diagnosis, overall 16.0% (0.78) of men and 29.9% (0.99) of women 50 years and older meet the NBHA diagnostic criteria for osteoporosis (Table 3). As anticipated, the prevalence of osteoporosis with the NBHA diagnostic criteria increases with age. In men, the estimated prevalence increased from 5.5 to 46.3% between the 50–59 and the 80+ age groups (Table 3). In women, the prevalence increased from 10.9% in the 50–59 age group to 77.1% in the 80+ age group. In both sexes, this trend is statistically significant (p = 0.001). We found similar patterns when evaluating non-Hispanic Whites alone, but the absolute prevalence of osteoporosis was higher in non-Hispanic Whites than the total study sample (Table 3).
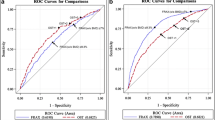
Given the low contribution of qualifying fractures alone to osteoporosis diagnosis, for purposes of analysis, we combined qualifying fractures with FRAX in our examination of the contributions of each criterion to those diagnosed with the NBHA criteria as having osteoporosis. Based on sample size, we also combined the 50–59 and 60–69 age groups. We observed statistical differences in the contributions of T-score and FRAX/qualifying fractures by sex and age (Fig. 2). FRAX/qualifying fracture score was the largest contributing factor defining osteoporosis in men 70–79 (men, 88.1% vs. women, 50.8%, p < 0.05) and 80+ (men, 80.1% vs. women, 56.5%, p < 0.05) than in women, whereas femoral neck and lumbar spine T-score was the largest contributing factor in women in those corresponding age groups (70–79, women 49.2% vs. men 11.9%, p < 0.05; 80+, women 43.5% vs. men 19.9%, p < 0.05) (Fig. 1). No statistical differences were observed in the youngest age group.
Discussion
We used NHANES 2005–2008 data to evaluate the prevalence of osteoporosis using the expanded osteoporosis diagnostic criteria recently recommended by the NBHA, which focused attention on the disease as one of elevated fracture risk in postmenopausal women and men over age 50 in the USA. The criteria include diagnosis based on BMD measurements as in the past and added as alternative means of diagnosis certain qualifying fractures and elevated risk for fracture as determined by FRAX as diagnostic for osteoporosis. We found that 16.0% of men age 50 and older and 29.9% of postmenopausal women would be classified as having osteoporosis in the USA. There was a statistically significant increasing trend in the prevalence with increasing age, underscoring the importance of advancing age as one of the primary risk factors for osteoporosis and fracture. In men and women 80 years and older, we estimated the prevalence to be 46.3 and 77.1%, respectively.
BMD, another potent risk factor for fracture, appears to be the driving component diagnosing women with osteoporosis, whereas FRAX appears to be more prominent in men, particularly older men. This finding may be in part a consequence of the current WHO guidelines for the calculation of T-scores for osteoporosis [15]. The young normal female referent group is used for the femoral neck T-score calculation for both men and women. If the male referent group is used to calculate T-scores in men, as is done by some clinical practitioners, a higher proportion of men would have been classified as having osteoporosis based on BMD T-scores at the spine or hip.
Previous national osteoporosis prevalence estimates using NHANES have been based only on BMD data [2, 18]. In the most recent national osteoporosis report, Wright and colleagues estimated that 4.3% of men and 15.4% of women 50 years and older have osteoporosis [2]. At face value, it appears that by using the expanded NBHA definition, the prevalence of osteoporosis increases by 3.7-fold in men and almost 2-fold in women.
One concern regarding increasing the numbers of individuals diagnosed with osteoporosis with the expanded criteria is that this would lead to an increase in the number of people being treated with prescription medication despite not having a T-score of −2.5 or lower [19]. Using the same NHANES data set, Dawson-Hughes and colleagues previously reported that 19.3% (1.2) of men and 30.8% (1.0) of women were eligible for osteoporosis treatment based on the current NOF treatment guidelines: T-score ≤−2.5 at spine or femoral neck, the presence of a vertebral or hip fracture, or meeting FRAX score thresholds of ≥3% risk for hip fracture or ≥20% risk for major osteoporotic fracture in those with low BMD [17]. Overall, we found 16% (0.8) of men and 29.9% (1.0) of women met the NHBA diagnostic criteria for osteoporosis. The proportions are nearly identically, suggesting that if all persons diagnosed with osteoporosis using the NBHA criteria were recommended for treatment by their doctors, the proportions would not increase if all clinicians were already following current NOF recommendations, which have been in place for several years.
In that same prevalence report, Wright and colleagues also estimated that approximately 44% of US adults 50+ years have low bone mass [2]. Several studies have shown that the majority of fractures occur in individuals with low bone mass [20–23]. The goal of the new NBHA criteria is to identify a population of people who have a high risk for fracture that previously was unrecognized and clinically manage and/or reduce that fracture risk. A formal diagnosis of osteoporosis may make the process easier.
Even if there is disagreement about the utility of prescription medication in patients diagnosed with osteoporosis using the NBHA criteria, particularly if that diagnosis is based solely on FRAX score, some management strategy is needed in all diagnosed patients to lower the elevated fracture risk that is present. In nearly all cases, especially in the oldest of the those diagnosed with osteoporosis with the expanded criteria, awareness by both clinicians and patients of the elevated fracture risk, correction of calcium and/or vitamin D deficiency, and a program to lessen the likelihood of falling are worthy and logical components of this strategy, and in those cases where medication to reduce fracture risk is appropriate, it should be used.
To our knowledge, this study is the first attempt to evaluate the impact of the NBHA osteoporosis diagnostic criteria; however, it is not without limitations. We were limited in the ascertainment of qualifying fractures due to data collection procedures in NHANES. Qualifying fractures only accounted for 1.3% of the NBHA classification in women and was statistically unreliable in men. Although this is a relatively small proportion, it could potentially represent over 467,000 women 50+ years of age based on the 2000 US census. The validity of the self-report of most fragility fractures is high [24], but misclassification is possible, particularly at fracture sites such as the spine. Due to the lack of radiographic information, we were also unable to incorporate morphometric fractures in our prevalence estimates. Radiographs can identify more spinal deformities that are indicative of fractures than waiting for patients to seek clinical attention. For example in analyses from the fracture interventions trial, 22.6% of the 446 radiographic deformities were clinically identified, whereas nearly 73% of the clinical identified vertebral fractures were morphometrically identified [25]. By excluding those individuals who would only be diagnosed with osteoporosis through the presence of a morphometric fracture and low BMD, we are biased towards lower prevalence. Another design decision that could have potentially biased our prevalence estimates lower was limiting our wrist fractures to those 60 years of age and older. This was done to be conservative as there is clinical equivocation on what is or is not a qualifying wrist fracture. As the 50–59 year olds represented a third of our study sample, we could have missed a number of wrist fractures that were truly attributable to osteoporosis in 50–59 year olds. Another conservative element of the NBHA criteria which may lead to underdiagnoses is related to the specific fracture sites included as qualifying fractures. Although the working group identified the top sites comprising almost two-thirds of osteoporosis-related fragility fractures, other fracture sites are also associated with increased risk for subsequent fracture [26]. Due to the overlap with DXA-defined osteoporosis, the number of people with qualifying fractures alone was small, making many estimates statistically unreliable. We could have also under diagnosed osteoporosis based by not having T-scores from other regions of the hip, such as total hip T-score, which is an appropriate measure by the NBHA criteria, but was not available in NHANES. Although it was useful to be able to compare our results with previously reported NHANES data, by standardizing our study sample to the 2000 Census did not allow us to capitalize on newer Census data that may better reflect the current demographics of the US population. Although, by design, NHANES provides national estimates of various conditions, such as osteoporosis, there could be selection bias among the participants, particularly among older and minority populations. However, NHANES strives to make each cycles participants as non-bias and as representative as possible to serve as a continual national data source for making national inferences.
In conclusion, the new expanded criteria for the clinical diagnosis of osteoporosis, intended to help to identify those older men and women at high risk for fracture, increases the prevalence of this condition beyond that found with BMD alone; however, based on the literature, the new diagnostic criteria will not alter the proportions of adults eligible for treatment. The expanded criteria were proposed for use in the USA, particularly in terms of FRAX calculations based on US specific estimates and intervention thresholds, but similar models could be developed in other countries if deemed appropriate. If there is to be an ongoing public health effort to reduce the burden of fractures in older women and men, the identification of those at elevated fracture risk and the development of management strategies to lower risk where it is found remains an important public health goal.
References
(2000) Osteoporosis prevention, diagnosis, and therapy. NIH Conses Statement 17(1):1–45
Wright NC, Looker AC, Saag KG, Curtis JR, Delzell ES, Randall S et al (2014) The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res 29(11):2520–2526. doi:10.1002/jbmr.2269
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S et al (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25(10):2359–2381. doi:10.1007/s00198-014-2794-2
Kanis JA, Burlet N, Cooper C, Delmas PD, Reginster JY, Borgstrom F et al (2008) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 19(4):399–428. doi:10.1007/s00198-008-0560-z
Kanis JA, WHOSG (2007) Assessment of osteoporosis at the primary health-care level. University of Sheffield, World Health Organization Collaborating Centre for Metabolic Bone Diseases
Office of the Surgeon General (U.S.) (2014) Department of Health and Human Services. Bone health and osteoporosis: a report of the Surgeon General. Rockville, MD. https://www.niams.nih.gov/Health_Info/Bone/SGR/SGRBoneHealthEnglish2015_022516.pdfhttps://www.niams.nih.gov/Health_Info/Bone/SGR/SGRBoneHealthEnglish2015_022516.pdf
Siris ES, Adler R, Bilezikian J, Bolognese M, Dawson-Hughes B, Favus MJ et al (2014) The clinical diagnosis of osteoporosis: a position statement from the National Bone Health Alliance Working Group. Osteoporos Int 25(5):1439–1443. doi:10.1007/s00198-014-2655-z
Zipf G CM, Porter KS, et al.. 2013 National Health and Nutrition Examination Survey: plan and operations, 1999–2010. National Center for Health Statistics. Vital Health Stat;1(56)
Baim S, Binkley N, Bilezikian JP, Kendler DL, Hans DB, Lewiecki EM et al (2008) Official positions of the International Society for Clinical Densitometry and executive summary of the 2007 ISCD Position Development Conference. J Clin Densitom 11(1):75–91. doi:10.1016/j.jocd.2007.12.007S1094-6950(07)00255-7
Prevention CfDCa (1999-2011) National Health and Nutrition Examination Survey (NHANES). Centers for Disease Control and Prevention, Hyattsville
NCHS CfDCaP (2006) National Health and Nutrition Survey: body composition procedure manual. US Department of Health and Human Services, Hyattsville
NCHS CfDCaP (2007) National Health and Nutrition Examination Survey: dual-energy X-ray absorptiometry (DXA) procedure manual. Hyattsville
Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP et al (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8(5):468–489
Kelly T (1990) Bone mineral density reference databases for American men and women. J Bone Miner Res 5(Suppl1):S249
Kanis JA, Melton LJ 3rd, Christiansen C, Johnston CC, Khaltaev N (1994) The diagnosis of osteoporosis. J Bone Miner Res 9(8):1137–1141. doi:10.1002/jbmr.5650090802
(2016) National Health and Nutrition Examination Survey 2007–2008 data documentation, codebook, and frequencies: osteoporosis 2009. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/2007-2008/OSQ_E.htm. Accessed 23 Nov 2016
Dawson-Hughes B, Looker AC, Tosteson AN, Johansson H, Kanis JA, Melton LJ 3rd (2012) The potential impact of the National Osteoporosis Foundation guidance on treatment eligibility in the USA: an update in NHANES 2005-2008. Osteoporos Int 23(3):811–820. doi:10.1007/s00198-011-1694-y
Looker AC, Melton LJ 3rd, Harris TB, Borrud LG, Shepherd JA (2010) Prevalence and trends in low femur bone density among older US adults: NHANES 2005-2006 compared with NHANES III. J Bone Miner Res 25(1):64–71. doi:10.1359/jbmr.090706
Schousboe JT, Ensrud KE (2015) Diagnostic criteria for osteoporosis should not be expanded. Lancet Diabetes Endocrinol 3(4):236–238. doi:10.1016/S2213-8587(15)00050-9S2213-8587(15)00050-9
Hillier TA, Cauley JA, Rizzo JH, Pedula KL, Ensrud KE, Bauer DC et al (2011) WHO absolute fracture risk models (FRAX): do clinical risk factors improve fracture prediction in older women without osteoporosis? J Bone Miner Res 26(8):1774–1782. doi:10.1002/jbmr.372
Schuit SC, van der Klift M, Weel AE, de Laet CE, Burger H, Seeman E et al (2004) Fracture incidence and association with bone mineral density in elderly men and women: the Rotterdam study. Bone 34(1):195–202
Siris ES, Chen YT, Abbott TA, Barrett-Connor E, Miller PD, Wehren LE et al (2004) Bone mineral density thresholds for pharmacological intervention to prevent fractures. Arch Intern Med 164(10):1108–1112. doi:10.1001/archinte.164.10.1108164/10/1108
Wainwright SA, Marshall LM, Ensrud KE, Cauley JA, Black DM, Hillier TA et al (2005) Hip fracture in women without osteoporosis. J Clin Endocrinol Metab 90(5):2787–2793
Chen Z, Kooperberg C, Pettinger MB, Bassford T, Cauley JA, LaCroix AZ et al (2004) Validity of self-report for fractures among a multiethnic cohort of postmenopausal women: results from the Women’s Health Initiative observational study and clinical trials. Menopause 11(3):264–274
Fink HA, Milavetz DL, Palermo L, Nevitt MC, Cauley JA, Genant HK et al (2005) What proportion of incident radiographic vertebral deformities is clinically diagnosed and vice versa? J Bone Miner Res 20(7):1216–1222. doi:10.1359/JBMR.050314
Gehlbach S, Saag KG, Adachi JD, Hooven FH, Flahive J, Boonen S et al (2012) Previous fractures at multiple sites increase the risk for subsequent fractures: the global longitudinal study of osteoporosis in women. J Bone Miner Res 27(3):645–653. doi:10.1002/jbmr.1476
Acknowledgements
We would like to thank Anne Looker, PhD, for her assistance with the provision and analysis of the NHANES data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial disclosures
NCW: research grants/contracts: Amgen.
KGS: consultant: Amgen, Lilly, Merck.
ESS: consultant: Amgen, Merck, Radius.
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Wright, N.C., Saag, K.G., Dawson-Hughes, B. et al. The impact of the new National Bone Health Alliance (NBHA) diagnostic criteria on the prevalence of osteoporosis in the USA. Osteoporos Int 28, 1225–1232 (2017). https://doi.org/10.1007/s00198-016-3865-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-016-3865-3