Abstract
Summary
We performed a randomized clinical trial to evaluate the effect of a 12-month physical exercise program on quality of life, balance, and functional mobility in postmenopausal women with osteoporotic vertebral fractures. All three outcomes improved in the intervention group and were better than in the controls.
Introduction
Th aim of this study was to evaluate the effectiveness of a structured physical exercise intervention on quality of life, functional mobility, and balance in patients with osteoporotic vertebral fractures and back pain.
Methods
Seventy-eight postmenopausal women with vertebral fractures were randomized into an exercise group (n = 40) and a control group (n = 38). The mean age was 69.2 ± 7.7 years. All women had at least one osteoporotic vertebral fracture and suffered from chronic back pain. Patients with a history of vertebral and non-vertebral fracture within the past 6 months were excluded. The 40-min exercise program was conducted twice weekly for 1 year. Participants in the control group were instructed to continue their usual daily activities. Participants were assessed at baseline and at 12 months using the Quality of Life Questionnaire (QUALEFFO-41). Balance was measured with the Balance Master® System NeuroCom® and functional mobility was measured with the “timed up and go” test and “sit-to-stand” test.
Results
Total QUALEFFO-41 score after 12 months was significantly better in the exercise group (44.2 ± 7.5) compared to the control group (56.6 ± 9.4), p < 0.0001. Quality of life improved in domains: “Pain”, “Physical function: Jobs around the house”, “Physical function: Mobility”, “Social function”, “General health perception” in the exercise group as compared to the control group. After 12 months, balance as assessed by “Tandem Walk and Sway” became significantly better in the exercise group as compared to the control group (p = 0.02). A significant improvement in the “timed up and go” test (p = 0.02) and the “sit-to-stand” test (p = 0.01) was shown in the exercise group compared to the control group.
Conclusions
This is the first 12 month-randomized clinical trial of exercise in osteoporotic women with a vertebral fracture that demonstrates improvement of three key outcome measures: quality of life, functional mobility, and balance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a systemic disease of the skeleton characterized by low bone mineral density and microarchitectural deterioration of bone resulting in reduced strength and increased risk for fractures [1]. Vertebral fractures, widely recognized to be classic osteoporotic fractures, may occur during normal daily activities, such as stair climbing, bending forward etc. They typically occur without falling. In accordance with population studies conducted in Russia, the prevalence of morphometric vertebral fractures for patients aged 50 years and older ranges from 7.2 to 12 % in men and 7 to 16 % in women [2, 3]. Osteoporotic vertebral fractures lead to an increased risk for subsequent fractures, lower quality of life, disability, and higher mortality [4–6].
Patients with vertebral fractures often suffer from back pain caused by both the fractures themselves and secondary changes in the intervertebral joints and the neighboring muscular-ligament complex. The treatment of such patients should be comprehensive and include both pharmacological and non-pharmacological interventions. Anti-osteoporotic medications reduce fracture risk by influencing bone remodeling mechanisms. These drugs reduce vertebral fracture risk by 30–70 %, hip fractures by 20–40 %, and non-vertebral fractures by 15–20 % [7, 8]. Non-pharmacological interventions include physical exercise to improve muscle strength and balance, decrease pain, and improve quality of life [9]. Exercise is generally very straightforward, not requiring significant material costs or special equipment. It can be done at home. Patients with osteoporotic vertebral fractures are often advised to adhere to specially designed exercises for spinal stability and posture [10–12]. Only a few previous randomized studies on the effect of exercise on quality of life and physical activity in patients with osteoporotic vertebral fractures have been published. These studies were heterogeneous in methodology and yielded controversial results [13–20].
The objective of our study was to evaluate the effectiveness of a structured physical exercise intervention on quality of life, functional mobility, and balance in patients with osteoporotic vertebral fractures and back pain.
Materials and methods
Study participants were women aged 50 years and older with postmenopausal osteoporosis and at least one radiographically confirmed vertebral fracture and chronic back pain. Exclusion criteria were vertebral and non-vertebral fracture within the past 6 months, secondary osteoporosis, osteomalacia, inflammatory joint, or spine disease, diffuse connective tissue disease, history of malignancy in the last 5 years, significant functional abnormalities of the cardiovascular, respiratory, gastrointestinal, or nervous system, renal disease, and corticosteroid intake during the last year.
All patients gave written informed consent prior to being enrolled in the study and were informed, at that time, that they had an equal chance of being included in either the programmed exercise group or a control group without any active intervention.
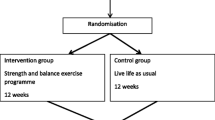
Patients were randomly assigned to the exercise and control groups in a 1:1 ratio. Randomization was performed using pre-generated randomization numbers in sealed opaque envelopes. An independent person not having any information about the patients opened the envelopes. Randomization number was reported to a researcher (LE) by telephone.
The study cohort was recruited from the Sverdlovsk Regional Hospital No. 1 and the Ural Institute of Traumatology and Orthopedics. Of the 135 women who were invited to participate, 78 subjects accepted.
Patients in the exercise group performed a specially designed 40-min program of physical exercises [21] in the exercise therapy gym twice weekly under the instructor’s supervision. The set of exercises consisted of three parts.
-
1.
Introductory Session (8 min). Subjects were prepared by being introduced to positions such as sitting, standing, supported standing position, standing with objects (sticks), and walking. In the introductory session, dynamic exercises for small, and medium-sized muscle groups and joints of the upper and lower extremities were performed. Movements were conducted at an average speed with the maximum possible amplitudes.
-
2.
Main Session (28 min). Special exercises were conducted. Initial positions were lying supine, sideways, prone, and knee-fist. Dynamic exercises for major muscle groups and joints were conducted for 10 min to strengthen the extensor muscles, increase mobility of the thoracic spine and improve posture. In addition, they performed isometric exercises for 14 min to strengthen the muscles of the lower extremities, abdomen, and back extensors. The exercises were interspersed with breathing techniques aimed to decrease a training load. The exercise program did not include spinal flexion and exercises with axial load bearing.
-
3.
Final session (4 min).The training load was gradually reduced. Breathing exercises combined with dynamic exercises for the upper extremities and diaphragm breathing were implemented. Exercises were conducted at a slow speed and maximum amplitude.
Relaxation techniques and autogenic training lasting for several minutes in the initial position lying supine followed the final part. The intensity of exercise increased with time.
When regular attendance of the sessions was impossible, patients were allowed to perform the structured exercise program at home provided that they had been properly trained previously by an instructor. Patients performing exercises on their own were given a booklet with the description of the whole structured program of exercises and a DVD-disk of these exercises.
Patients in the control group were asked to maintain their current level of physical activity. They could continue performing exercises at home on their own if they had performed the exercises prior to having been included in the study. The primary end-point of the study was change in quality of life over 12 months. The secondary end-points were changes in balance, functional mobility, severity of thoracic kyphosis, and subsequent fractures.
Quality of life was evaluated with the questionnaire QUALEFFO-41, which was especially designed and validated for patients with osteoporotic vertebral fractures and back pain [22]. Assessment of the questionnaire included both the total score and the score in the seven domains: pain, activities of daily living, jobs around the house, mobility, social function, general health perception, and mental function. Three domains of the aforementioned (activities of daily living, jobs around the house, and mobility) are supposed to reflect physical functioning. The lowest quality of life score in every domain corresponds to a total of 100 points; the highest quality of life is reflected by a total score equal to 0. Therefore, a lower score indicates a higher quality of life.
For assessment of balance, functional mobility, and its dynamics, stabilometry was used. The study was conducted with a computed posturographic system for diagnostics of balance and movement skills (Balance Master® System NeuroCom®) designed to objectively quantify balance and postural function of different origin [23–26]. To assess physical function and balance, possibly reflecting disorders of the musculoskeletal system, three tests were chosen.
-
1.
“Weight-bearing/squat” test to maintain static balance was performed to quantify the weight supported by each leg. The assessment is conducted in the upright position with extended legs. Weight distribution for each leg (as a percentage of body weight) is estimated and the difference between legs is calculated (normally, the allowable difference ranges from 5 to 15 % depending on the age of the patient). An increase in the asymmetry between legs may correspond to disorders of the musculoskeletal system or the presence of a neurological motor deficit.
-
2.
“Sit-to-stand” test provides an estimate of functional mobility assessed with the patient performing from a sitting position, without hands, the following tasks:
-
(a)
Weight transfer: time (in seconds) to shift the center of gravity from the moment the patient hears/sees a verbal or color command to the time when the patient completes the task the center of gravity is located over his feet;
-
(b)
Left/right weight symmetry: distribution of a support between the legs during lifting (percentage of body weight).
-
(a)
-
3.
Test “tandem walk and sway” performed as follows: a patient is asked to walk on a straight line moving the toe to the heel, to stop moving on command and to keep balance for 5 s. Oscillations of the center of gravity for 5 s after the command to stop motion (degrees per second) are assessed.
Patients with disorders of the musculoskeletal system, muscle weakness, or vestibular/motor deficit show asymmetry in distribution of support between their legs and high center of gravity fluctuation. In addition, they need more time to complete tests. To obtain clinically significant data, the design of the study included repetitive measures (×3) of the second and third tests. The computer program automatically calculated the parameters for each patient, taking into account age, and height.
Among these tests, tandem walk and sway test reflects balance to a greater extent than others, because it assesses fluctuations in center of gravity. Weight-bearing/squat and sit-to-stand tests mainly reflect muscular-skeletal abnormalities could show asymmetry for different reasons (osteoarthritis, joint deformities, muscle weakness, motor neural deficit). The second parameter of the sit-to-stand test (b.) reflects mainly functional mobility.
Functional mobility was also assessed with the test “timed up and go”. When performing this test, a patient is asked to stand up from a chair, walk three meters, then go back and sit down. The test was evaluated twice measuring the time in seconds. The best test result was included in the analysis.
The severity of thoracic kyphosis was evaluated by a predefined protocol measuring the distance between the wall and the occiput in standing position, leaning against the wall with the back, buttocks, and heels, keeping the head upright but trying to approximate the head against the wall. The line drawn through the lower edge of the eye socket and the upper edge of the tragus of the ear was on the horizontal line with the chin normally positioned, thus, ensuring that no cervical extension, rotation, flexion, or side flexion would occur. One investigator conducted the study for all patients at the first and last visits.
During the study, the patients in the exercise group kept specially designed diaries where they recorded the regularity of exercise sessions. In addition, the exercise instructor kept a log to register which patients participated in which session. To maintain regular exercises, patients in the exercise group were contacted by phone if they had missed a session and were asked to perform exercises at home. Patients of both groups continued to take their anti-osteoporosis medications.
Statistical analyses were performed using parametric (t test) and nonparametric criteria (Wilcoxon, Mann-Whitney, and chi-square tests), where appropriate, employing the Statistica 6.0 program. T test for independent samples and Mann-Whitney test were used to compare baseline values between groups and to compare values at 12-months registration between groups. Paired t test and Wilcoxon test were used to compare baseline values and values in 12 months in groups. To show that changes that occurred in the training groups were significantly different from the changes that occurred in the control group, we used an independent t test to analyze the changes in mean values from the measurement at baseline to 12 months. Results are presented as mean (M) and standard deviation (SD) for normally distributed variables and as median (Me) and 25–75 percentiles for variables with a skewed distribution. Data were analyzed following an intention-to-treat principle and missing data were managed using the last observation carried forward (LOCF) technique. The sample size was based on a mean change in total QUALEFFO-41 score of 5.0 for training groups. A total sample size of 68 subjects is required to find differences in changes between groups of this magnitude given a power of 80 % and α = 0.05. To account for potential dropouts, we enrolled 15 % more study subjects.
Blinded assessment of the parameters was conducted in the implementation and evaluation of stabilometry and quality of life questionnaire.
The Ethics Committee of the Sverdlovsk Regional Clinical Hospital No. 1 approved the study. This study is registered at the Center for Information Technologies and Systems of Executive Authorities, Ministry of Education and Science of Russian Federation, # 01201460156.
Results
Demographic and clinical variables
We recruited 78 participants with at least one osteoporotic vertebral fracture and chronic back pain (40 in the exercise group and 38 controls), mean age 69.2 ± 7.7 years. Demographic and clinical characteristics of the patients in both groups are shown in the Table 1.
Study parameters (quality of life, stabilometry, test timed up and go) did not differ between groups at baseline. Between-group differences were observed only in the thoracic kyphosis that was more pronounced in the exercise group: the distance between the wall and the occiput was greater in the exercised group (4.0 cm), compared with the control group (2.6 cm), p = 0.02. The data are presented in the Table 2.
Exercise
During the study, one patient in the exercise group and one in the control group dropped out (Fig. 1). The first one changed the place of residence, the second one refused to continue participation. Adverse events were not registered in both cases.
25 patients in the exercise group worked out in the exercise therapy gym under the instructor’s directions and 12 participants performed exercise at home according to the suggested program after a training course with an instructor. Overall, 37 patients performed exercises; two other patients did not perform exercise (Fig. 1). 21 subjects performed exercises two times a week during the whole year (13 participants in the exercise therapy gym and 8 participants at home), while 12 patients had gaps in the exercise schedule. However, the number of missed sessions did not exceed 20 % of the total number of sessions. Four patients did not perform their exercise regularly; they missed more than 20 % of sessions. Overall, 33 patients (89.2 %) were adherent because they missed less than 20 % of all sessions.
Among controls, 15 out of 18 subjects who were exercising before recruitment, continued to perform their exercises at home.
At the end of the study, the weekly duration of exercise significantly increased in the exercise group from 74.6 min. per week up to 138.6 min. per week (p = 0.0001).
In the control group, this parameter diminished slightly from 69.2 min. per week to 62.7 min. per week (p = 0.897).
Quality of life
Quality of life parameters are shown in the Table 3. At the end of the study, total QUALEFFO-41 score and scores on all domains, were significantly lower (better) in the exercise group compared to the control group. Based on average changes in the mean values occurring from baseline to the 12 month we found a significant difference between the exercise group and the control group in the measurements of “Pain”, “Physical function: Jobs around the house”, “Physical function: Mobility”, “Social function”, “General health perception,” and “Total QUALEFFO-41”.
Stabilometry and functional mobility
Both weight-bearing/squat test with extended legs and sit-to-stand: left/right weight symmetry test reflecting weight distribution to each leg did not show change either in the exercise group or in the controls. In contrast, the time of performing the sit-to-stand: weight transfer test and tandem walk and sway test demonstrated statistically a significant difference between groups with statistically significant worsening in the control group and non-significant improvement in the exercise group (Table 3).
Values in the timed up and go test at 12 months were not different between the exercise group and the control group. However, there was a significant improvement in the exercise group with a decrease in test performance time from 12.0 ± 3.8 to 11.4 ± 3.3 s (p = 0.02) while performance time remained unchanged in the control group (11.0 ± 3.3and 11.3 ± 2.9 s, respectively). Based on changes in mean values from baseline to the 12 months evaluation, we found a significant difference in change in mean between the intervention and the control group. The exercise group had better results than the control (p = 0.02).
Thoracic kyphosis
Severity of thoracic kyphosis, as measured with the occiput-wall distance, significantly decreased in the exercise group and did not change in the control group with no between-group differences at the end of the study. In the exercise group the occiput-wall distance decreased from 4.0 to 3.3 cm (p = 0.04), in controls from 2.6 to 2.5 cm (p = 0.46).
Fractures
During the one year of observation, 4 participants in the exercise group and 7 participants in the control group sustained clinical vertebral and non-vertebral fractures (p = 0.285). Although vertebral fractures were equally detected in the exercise (2 participants) and the control (2 participants) groups, non-vertebral fractures were found more frequently in the control group (5 patients) compared to the exercise group (2 patients). However, these differences were not statistically significant. No fracture occurred during the time of exercise performance. Adverse effect of exercising was observed only in one patient, who experienced an exacerbation of pain in the knee joint while performing exercise in the knee-wrist position. Later this initial position was excluded for that person, and the patient became pain free and was able to continue the exercise program.
Discussion
In the present study, we examined the effect of a 12-month exercise therapy program versus a control group in postmenopausal osteoporotic women with at least one vertebral fracture and chronic back pain. We found improvements in quality of life, balance, and physical functioning. Our positive results are related to the duration of the exercise program, the fact that the subjects were not elderly and, therefore, able to be rigorously trained, a sufficiently large number of patients in our study, and high adherence (89.2 %). Similar efforts to demonstrate an effect of exercise have been limited by their relatively short duration, usually less than 16 weeks [13, 15–17], and less than 50 % adherence [19].
At the end of the study, total QUALEFFO-41 score and scores in all domains were significantly better in the exercise group compared to the control group. We do realize that the QUALEFFO is a subjective self-rated measurement scale, but we also observed positive results in tests for balance and physical function which are objective measurements. Further, favorable QUALEFFO results were associated with improvements in pain, physical function, and balance. These results are also consistent with the impression that exercises have a positive impact on quality of life in older people with or without osteoporosis [9, 27]. Only few previously published studies have actually documented such an improvement. Bennel et al. demonstrated significantly greater improvement in the QUALEFFO physical function score compared with the control group, but no significant difference between groups in other QUALEFFO domains were shown [13]. In contrast to our study, that study evaluated the efficacy of a 10-week program with multi-modal physical therapy intervention including manual therapy, massage, taping, posture training, and exercise prescription. The additional interventions, therefore, may explain the positive results achieved in that study, despite the small sample size and its short duration [13]. Our results are comparable to the study of Bergland et al. who utilized the same length and frequency of training [14]. Positive effect on quality of life in both studies suggest that in order to demonstrate positive effects of exercise on quality of life, the studies have to be conducted for a longer period of time than has been traditionally employed [14]. In particular, the 12-month improvement in the Pain was noteworthy in both our study and Berglund’s. [14]. Improvement in other quality of life parameters might be secondary to pain relief.
In the study of Papaioannou et al. [19], all patients performed exercise at home 3 times a week over a 6-month period under monthly instructor supervision. Over the next 6 months, home exercises continued without supervision. A disease-specific questionnaire “Osteoporosis Quality of Life Questionnaire (OQLQ)” was used. After the first 6 months, a significant improvement in the intervention group versus the control group in symptoms (p = 0.003), emotions (p = 0.01), and leisure/social activities (p = 0.03) was shown. After 12 months, however, while the significant improvement in symptoms (p = 0.02) and activities daily living (p = 0.04) persisted, there was no longer significant between-group difference in emotions and leisure/social activities [19]. Differences between our study and that of Papaioannou et al. might be explained by better adherence at 12 month among our patients.
Malmros et al. used their own version of a QoL questionnaire to assess the efficacy of a 12-week exercise program with the same frequency training as our study. They demonstrated improvement in quality of life parameters within 5 (p = 0.01), 10 (p < 0.0001), and 12 weeks after the end of the group sessions (p = 0.0008) [15].
When studies have not distinguished subjects in those with and without vertebral fractures, results have failed to show an improvement of quality of life [28], and, in some cases, even deterioration in mental functioning has been reported [29]. Gold et al. [18] found in a study in 158 elderly women (mean age 81 years) significant between-group differences in the change in psychological symptoms only for Phase 1 of the crossover study, but no significance between-group difference was observed for pain in Phase 1 and Phase 2.
Stabilometry parameters assessing weight distribution between legs both in static position and in sit-to-stand: left/right weight symmetry test did not change significantly either in the exercise or in the control group. However, it should be noted that indicators for this test did not go beyond normal values both at baseline and at final visits. In contrast, statistically significant differences between the groups were noted in time of sit-to-stand:weight transfer test performance and tandem walk and sway test (oscillations of the center of gravity after movement was stopped). Between-group differences were due to stabilization and slight improvement in the exercise group and significant worsening in the control group. This improvement in oscillation of center of gravity in the intervention group might result from balance training in those who exercised. In other studies, Papaioannou et al. [19] and Smith et al. [28] showed statistically significant between-group differences in balance in patients with vertebral fractures. Bergland et al. [14] demonstrated balance improvement in the static position after 3 months of exercise, but no between-group statistical significance at 12 months. Parameters in the control group worsened both at 3 and 12 months, which is similar to our findings. Malmros et al. [15] reported a non-significant difference between groups. Positive effect of balance training exercise was also shown in elderly osteoporotic women without vertebral fractures [30, 31]. A large systematic review (94 studies, 9917 participants) obtained evidence that balance tests are improved by balance training exercise [32]. The effect was dependent upon the exact type of exercise: the statistically significant balance improvement was mentioned during the coordination and balance training exercises both in movement and in static positions. It should be emphasized that the effectiveness of the balance training exercise program might well be influenced by the presence of vertebral fractures if accompanied by kyphotic changes, back pain, and movement restrictions.
To assess functional mobility, we used the timed up and go test which showed a small but statistically significant improvement in the exercise group as well as statistically significant between-group difference in the average changes in mean values occurring in the exercise and control groups from baseline to 12 month. The other parameter assessing physical functioning in our study was the time of Sit-to-Stand: weight transfer test performance during stabilometry. At the time of the last visit, the groups differed significantly both in means and in change in means during the 12-month period. Other studies using the same test have reported conflicting results. Thus, in two studies [13, 19] no between-group difference was found, while two other studies [14, 16] reported an improvement in the exercise group compared to controls. The improvement in physical functioning shown by shortening the time of the timed up and go test performance was also demonstrated in 12-month [31] and 20-week [30] studies of exercises contained balance training in elderly osteoporotic women without vertebral fractures.
Our study also demonstrated a reduction of the occiput-to-wall distance in the exercise group. We do realize that this measurement of thoracic kyphosis is viewed by some as suboptimal because of a reliability and validity issues in comparison with non-invasive, skin-surface methods including the Debrunner kyphometer, the Spinal Mouse, the Flexicurve [33], as well as radiological measurements. However, given the fact that our program included exercises to train back extensors, and that the reduction of the occiput-wall distance from baseline to 12 month was observed only in the exercise group with predefined measurements that were performed by the same observer, we interpret our results as a trend to reduction of thoracic kyphosis after 12 months of exercise. In the study by Bennell et al. during 10 weeks of multi-modal physical therapy intervention including manual therapy, massage, taping, posture training, and exercise, the degree of kyphosis decrease in the training group by 3.2°, which was higher than in the control, but no statistically significant between-group and within-group differences were appreciated [13]. In the study by Bergstrom et al. including training focused on a back muscle extensor strengthening program twice weekly for 4 months [17], statistically significant differences in the reduction of thoracic kyphosis also were not shown. In our study, we failed to demonstrate between-group differences in thoracic kyphosis at the last visit. This might be related to an irreversible element of the deformities in some patients as well as to the large variability of parameters. Thus, subjects with both normal posture and hyperkyphosis were included, and occiput-wall distance ranged from 0 to 13 cm.
Since only a limited number of patients were enrolled in our study, it was not powered to detect a difference in vertebral or non-vertebral fractures between the groups. This is in line with other studies, in which lack of statistical power precluded significant conclusions to be drawn [20, 34]. Relatively few studies have shown a reduction in fracture risk. Kemmler et al. demonstrated statistically significant fracture risk reduction (0.51, 95 % CI 0.33; 0.97, p = 0.46) during a 12-year exercise program in the 16-year follow-up in the cohort of postmenopausal women without vertebral fractures who performed high-impact exercises with jumps and other types of exercises. While of interest, this kind of exercise program would not be recommended to patients who have sustained vertebral fractures [35]. The study by Sinaki et al. demonstrated the long-term effect of strengthened back muscles on the reduction of vertebral fractures in estrogen-deficient women [36].
Fracture risk during exercise is important indicator of the safety of the exercise program. Only one study demonstrated an increase in fracture risk during flexion exercise as compared to extension exercise [37]. This type of exercise is no longer utilized in more recent studies.
Adverse events during an exercise program in subjects with osteoporotic vertebral fractures (from muscle pain to ribs fractures) were found in 8.1 % of patients [34]. We noted worsening knee pain in one patient. In two other patients, new vertebral fractures developed but the events bore no relationship with the timing of exercises. Also, this did not differ from the control group.
Our study has confirmed the efficacy of exercise in relieving pain, improving quality of life, and physical functioning. Taking into account its efficacy and safety, exercise can be recommended to patients with osteoporosis complicated with vertebral fractures. Consultation with a physical therapist is suggested to ensure the safety and appropriateness of the exercise regimen. Osteoporotic patients should avoid push-ups, curl-ups, vertical jumps, and trunk forward flexion and exercises with axial load. Low-impact weight-bearing activities and resistance training combined with balance training are the best.
Our study has some limitations. Blinded assessment of the indices tracked was conducted only in stabilometry and the quality of life questionnaire. As in other studies, there was some crossover effect, and adherence to therapy in our study was 89.2 %. Not all patients in the exercise group performed physical exercises in the exercise therapy gym under the instructor’s control. Some who performed home exercises may not have executed them properly. Even other patients randomized to the exercise group did not perform all exercises. In contrast, some subjects from the control group continued their physical activity including home exercise. If both groups had been more clearly delineated with regard to compliance of exercise (test group) or no added exercise (control group), the differences between the two groups might have even been greater. Nevertheless, the differences are still most noteworthy.
Another limitation of the study is that validated, non-invasive thoracic kyphosis measurement techniques were not used. The results cannot be extended to those with cardiac or pulmonary comorbidity because there were exclusion criteria. Finally, our study does not define the optimal period of exercise. Presumably, more sustained exercise, exceeding the 12-month period of this study would continue to be beneficial.
Conclusion
The study demonstrates the effectiveness of a structured physical exercise program in reducing pain, improving quality of life, physical activity, and balance in postmenopausal women with osteoporotic vertebral fractures.
References
WHO (2003) WHO Scientific Group on the Prevention and Management of Osteoporosis. Prevention and management of osteoporosis: report of WHO scientific group. WHO Technical Report Series 2003: Vol. 921
Mikhailov E, Benevolenskaya LI, Mylov NM (1997) Incidence of vertebral fractures in population sample of individuals aged 50 years and older. Bull Traumatol Orthop NN Priorov 3:20–27, in Russian
Evstigneeva LP, Lesnyak OM, Piven AI (2001) Epidemiology of osteoporotic vertebral fractures according to X-ray and morphometric analysis among population sample of citizens of Ekaterinburg aged 50 years and older. Osteoporos Osteopathy 2:2–6 (in Russian)
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726–1733
Haczynski J, Jakimiuk A (2001) Vertebral fractures: a hidden problem of osteoporosis. Med Sci Monit 7:1108–1117
Lems WF (2007) Clinical relevance of vertebral fractures. Ann Rheum Dis 66(1):2–4
Body JJ, Bergmann P, Boonen S et al (2010) Evidence-based guidelines for the pharmacological treatment of postmenopausal osteoporosis: a consensus document by the Belgian Bone Club. Osteoporos Int 21:1657–1680
MacLean C, Newberry S, Maglione M et al (2008) Systematic review: comparative effectiveness of treatments to prevent fractures in men and women with low bone density or osteoporosis. Ann Intern Med 148:197–213
Liu-Ambrose TY, Khan KM, Eng JJ, Lord SR, Lentle B, McKay HA (2005) Both resistance and agility training reduce back pain and improve health-related quality of life in older women with low bone mass. Osteoporos Int 16:1321–1329
Burr J, Shephard R, Cornish S, Vatanparast H, Chilibeck P (2012) Arthritis, osteoporosis, and low back pain: evidence-based clinical risk assessment for physical activity and exercise clearance. Can Fam Physician 58(1):59–62
Sinaki M (2012) Exercise for patients with osteoporosis: management of vertebral compression fractures and trunk strengthening for fall prevention. PMR 4(11):882–888
Bonaiuti D, Arioli G, Diana G, Franchignoni F, Giustini A, Monticone M, Negrini S, Maini M (2005) SIMFER rehabilitation treatment guidelines in postmenopausal and senile osteoporosis. Eura Medicophys 41(4):315–337
Bennell KL, Matthews B, Greig A, Briggs A, Kelly A, Sherburn M, Larsen J, Wark J (2010) Effects of an exercise and manual therapy program on physical impairments, function and quality of-life in people with osteoporotic vertebral fracture: a randomised, single-blind controlled pilot trial. BMC Musculoskelet Disord 11:36
Bergland A, Thorsen H, Karesen R (2011) Effect of exercise on mobility, balance, and health-related quality of life in osteoporotic women with a history of vertebral fracture: a randomized, controlled trial. Osteoporos Int 22(6):1863–1871
Malmros B, Mortensen L, Jensen MB, Charles P (1998) Positive effects of physiotherapy on chronic pain and performance in osteoporosis. Osteoporos Int 8(3):215–221
Yang L, He C, Lei Z, Xie W, Lan Q (2007) Effect of pain-free exercises on female osteoporosis patients with spinal compressive fracture. J Clin Rehab Tis Eng Res 11:9108–9111
Bergstrom I, Bergstrom K, Kronhed A, Karlsson S, Brinck J (2011) Back extensor training increases muscle strength in postmenopausal women with osteoporosis, kyphosis and vertebral fractures. Adv Physiother 13(3):110–117
Gold DT, Shipp KM, Pieper CF, Duncan PW, Martinez S, Lyles KW (2004) Group treatment improves trunk strength and psychological status in older women with vertebral fractures: results of a randomized, clinical trial. J Am Geriatr Soc 52(9):1471–1478
Papaioannou A, Adachi JD, Winegard K, Ferko N, Parkinson W, Cook RJ, Webber C, McCartney N (2003) Efficacy of home-based exercise for improving quality of life among elderly women with symptomatic osteoporosis-related vertebral fractures. Osteoporos Int 14:677–682
Giangregorio LM, Macintyre NJ, Thabane L, Skidmore CJ, Papaioannou A (2013) Exercise for improving outcomes after osteoporotic vertebral fracture. Cochrane Database Syst Rev 1:CD008618
School of Health (2008) Osteoporosis. In: OМ L (ed) Guidelines for physicians. GEOTAR-Media, Russia, 64 p
Lips P, Cooper C, Agnusdei D, Caulin F, Egger P, Johnell O, Kanis JA, Kellingray S, Leplege A, Liberman UA, McCloskey E, Minne H, Reeve J, Reginster JY, Scholz M, Todd C, de Vernejoul MC, Wiklund I (1999) Quality of life in patients with vertebral fractures: validation of quality of life questionnaire of the European foundation for osteoporosis (QUALEFFO). Osteoporos Int 10(2):150–160
Di Fabio RP (1995) Sensitivity and specificity of platform posturography for identifying patients with vestibular dysfunction. Phys Ther 75(4):290–305
Usachev VI, Dotsenko VI, Kononov AF, Artemov VG (2009) New methodology for the stabilometric diagnosis of equilibrium dysfunction. Vestn Otorinolaringol 3:19–22
Nelson SR, Di Fabio RP, Anderson JH (1995) Vestibular and sensory interaction deficits assessed by dynamic platform posturography in patients with multiple sclerosis. Ann Otol Rhinol Laryngol 104(1):62–68
Di Nardo W, Ghirlanda G, Cercone S, Pitocco D, Soponara C, Cosenza A, Paludetti G, Di Leo MA, Galli I (1999) The use of dynamic posturography to detect neurosensorial disorder in IDDM without clinical neuropathy. J Diabetes Complicat 13(2):79–85
Langlois F, Vu TT, Chassé K, Dupuis G, Kergoat MJ, Bherer L (2013) Benefits of physical exercise training on cognition and quality of life in frail older adults. J Gerontol B Psychol Sci Soc Sci 68(3):400–404
Smith AA, Summers GD, Baxendale A, Butterly RJ (1998) A randomized controlled trial of the effects of weight-bearing exercise and resistance training on risk factors for fracture in women with osteoporosis. In: Ring EFJ, Elvins DM, Bhalla AK (eds) Current research in osteoporosis and bone mineral measurement. British Institute of Radiology, London, p 128
Bautmans I, Van Arken J, Van Mackelenberg M, Mets T (2010) Rehabilitation using manual mobilization for thoracic kyphosis in elderly postmenopausal patients with osteoporosis. J Rehabil Med 42:129–135
Carter ND, Khan KM, McKay HA, Petit MA, Waterman C, Heinonen A, Janssen PA, Donaldson MG, Mallinson A, Riddell L, Kruse K, Prior JC, Flicker L (2002) Community-based exercise program reduces risk factors for falls in 65- to 75-year-old women with osteoporosis: randomized controlled trial. CMAJ 167:997–1004
Madureira MM, Takayama L, Gallinaro AL, Caparbo VF, Costa RA, Pereira RMR (2007) Balance training program is highly effective in improving functional status and reducing the risk of falls in elderly women with osteoporosis: a randomized controlled trial. Osteoporos Int 18:419–425
Howe TE, Rochester L, Neil F, Skelton DA, Ballinger C (2011) Exercise for improving balance in older people. Cochrane Database Syst Rev 11:CD004963
Barrett E, McCreesh K, Lewis J (2014) Reliability and validity of non-radiographic methods of thoracic kyphosis measurement: a systematic review. Man Ther 19(1):10–17
Dusdal K, Grundmanis J, Luttin K, Ritchie P, Rompre C, Sidhu R, Harris SR (2011) Effects of therapeutic exercise for persons with osteoporotic vertebral fractures: a systematic review. Osteoporos Int 22(3):755–769
Kemmler W, Bebenek M, Kohl M, von Stengel S (2015) Exercise and fractures in postmenopausal women. Final results of the controlled Erlangen Fitness and Osteoporosis Prevention Study (EFOPS). Osteoporos Int 26(10):2491–2499. doi:10.1007/s00198-015-3165-3
Sinaki M, Itoi E, Wahner HW, Wollan P, Gelzcer R, Mullan BP, Collins DA, Hodgson SF (2002) Stronger back muscles reduce the incidence of vertebral fractures: a prospective 10-year follow-up of postmenopausal women. Bone 30(6):836–841
Sinaki M, Mikkelsen BA (1984) Postmenopausal spinal osteoporosis: flexion versus extension exercises. Arch Phys Med Rehabil 65:593–596
Acknowledgments
The authors would like to thank Professor John Bilezikian for his critical review of the manuscript and valuable comments.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethical approval
All procedures performed in studies involving human participants were conducted in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or compatible ethical standards.
Rights and permissions
About this article
Cite this article
Evstigneeva, L., Lesnyak, O., Bultink, I.E.M. et al. Effect of twelve-month physical exercise program on patients with osteoporotic vertebral fractures: a randomized, controlled trial. Osteoporos Int 27, 2515–2524 (2016). https://doi.org/10.1007/s00198-016-3560-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-016-3560-4