Abstract
Summary
We report on second fracture occurrence in the year following a hip, shoulder or wrist fracture using insurance claims. Among 273,330 people, 4.3 % had a second fracture; risk did not differ by first fracture type. Estimated adjusted second fracture probabilities may facilitate population-based evaluation of secondary fracture prevention strategies.
Introduction
The purpose of this study was estimate second fracture risk for the older US population in the year following a hip, shoulder, or wrist fracture.
Methods
Observational cohort study of Medicare fee-for-service beneficiaries with an index hip, shoulder, or wrist fragility fracture in 2009. Time-to-event analyses using Cox proportional hazards models to characterize the relationship between index fracture type (hip, shoulder, wrist) and patient factors (age, gender, and comorbidity) on second fracture risk in the year following the index fracture.
Results
Among 273,330 individuals with fracture, 11,885 (4.3 %) sustained a second hip, shoulder or wrist fracture within one year. Hip fracture was most common, regardless of the index fracture type. Comparing adjusted second fracture risks across index fracture types reveals that the magnitude of second fracture risk within each age-comorbidity group is similar regardless of the index fracture. Men and women face similar risks with frequently overlapping confidence intervals, except among women aged 85 years or older who are at greater risk.
Conclusions
Regardless of index fracture type, second fractures are common in the year following hip, shoulder or wrist fracture. Secondary fracture prevention strategies that take a population perspective should be informed by these estimates which take competing mortality risks into account.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An estimated 323 million people suffer from osteoporosis worldwide and that number is projected to reach 1.55 billion by the year 2050 [1]. Although osteoporosis places individuals at increased risk for fracture, the best predictor of sustaining a fragility fracture is having had a prior fracture [2]. The risk of subsequent fracture associated with history of osteoporotic fracture has been studied in several cohorts across the world with results summarized in meta-analyses which report estimated relative risks between 1.5 and 2.3 following a wrist, shoulder, or hip fracture [3, 4]. The incident osteoporotic fracture population presents an opportunity for targeted fracture reduction interventions because they have known increased risk of fracture and are easily identified.
To capitalize on this opportunity, the clinical community needs more granular information about in whom the increased risk occurs and how other factors may affect the risk of subsequent fracture. Specifically, most prior studies have not addressed the competing risk of mortality among older adults or have done so in a limited fashion [5]. In addition, most prior studies are based on self-report of prior fracture without attention to how soon or late the risk of subsequent fracture occurs after an index fracture. Whether medications to improve bone strength (which requires significant time) or fall prevention interventions (with impact in the short term) would be more effective for any given patient depends, in part, on competing mortality risks and temporal aspects of increased fracture risk. In this paper, we report the incidence of a subsequent fracture in the US population of men and women ages 66 and older who sustained a hip, shoulder or wrist fracture in 2009. We then use time-to-event analyses to evaluate the relationship between type of index fracture (hip, shoulder, wrist) and patient factors (age, gender, race, and comorbidity) on risk of a subsequent fracture.
Methods
Patient population
We developed an observational cohort study of fee-for-service Medicare beneficiaries aged 66–99 years old who sustained a hip, shoulder, or wrist fragility fracture. Beneficiaries had to be aged 66 by Jan 1, 2009 and be enrolled in Parts A and B without managed care enrollment for one year before and one year after the index fracture or until death. Index fractures were identified using Medpar, Carrier, and Outpatient Hospital files in 2009 and utilization data from the prior year (2008) was used to confirm that no similar fracture occurred within that time frame and to calculate comorbidity.
Fracture identification
We developed an algorithm to identify index fractures among elderly beneficiaries that were most likely related to osteoporosis. The general approach to identifying an index fracture was to require a claim with an appropriate diagnosis and treatment code without a similar fracture in the prior year. We also applied additional rules when necessary to assure that the event indicated a new fracture rather than follow-up care of a previous fracture. The Methodological Appendix in the supplementary materials provides details of all of the specific diagnostic and procedural codes used to develop the cohort referenced in the following section.
Hip fractures were identified by an acute care hospitalization with an appropriate ICD-9 diagnostic and a diagnosis-related group (DRG) or ICD-9 procedure code indicating surgical repair. For wrist and humerus fractures treated as inpatients, we required both a diagnosis code and a relevant indication of treatment, which could include non-surgical treatments. Unlike hip fracture, shoulder and wrist fractures can also be treated in outpatient settings.
When treated as an outpatient without surgery to avoid including a patient who was merely having after-care for a previous fracture, we required a claim with the appropriate diagnosis and treatment codes along with a claim for appropriate imaging within seven days before or after the treatment claim. The same diagnostic codes were used for outpatient and inpatient cases. Treatment and imaging were indicated by presence of specific Common Procedural and Treatment (CPT) codes listed in the methodological appendix. Imaging of the appropriate region with plain X-ray, CT scan, or MRI was accepted. Some individuals had multiple index fractures on the same day (ex. a hip and wrist fracture from the same fall). In these cases, we attributed the person to the fracture of greatest functional impact (hip > shoulder > wrist).
We applied exclusions to remove people who were receiving treatments that suggested the event was not an osteoporosis-related fracture, such as a cancer diagnosis, multitrauma, or complications of a prior fracture (mal- or non-union, infection, revision, or hardware removal). In the case of fractures due to cancer, we excluded fractures with a diagnostic code indicating “pathologic” and the presence of cancer in the year before or one month after the fracture (to account for cases when the fracture is the initial presentation of the cancer). We included in our list of cancers only those known to be primary to bone or to metastasize commonly to bone. We did not exclude all fractures indicated as “pathologic” because some clinicians refer to fractures due to any bone disease, including osteoporosis, as pathologic.
Main outcome measure
After the index fracture that allowed cohort entry, individuals were followed for up to one year or until occurrence of another fracture or death. The occurrence of a new hip, shoulder, or wrist fracture was determined using the same approach as for index fracture with adaptations to distinguish follow-up care for the index fracture because claims do not indicate laterality of fracture. When a fracture is treated in the hospital with surgery, we have high confidence that the fracture is new once we apply the exclusion criteria for complications from prior fractures. We also have high confidence when a fracture affects a different site than the index fracture (for example, a wrist fracture after a hip fracture).
For upper extremity fractures that are managed non-surgically, it can be challenging to distinguish a follow-up visit from the occurrence of a new fracture in the same location. As a result, when a wrist fracture is followed by another wrist fracture or shoulder by shoulder, we applied a period when no claims for the same fracture occurs (a “clean period”). This allows us to be more confident that the new episode of claims represents a subsequent fracture rather than recurring care for an earlier one. We tested the sensitivity of our fracture rate results to the length of clean period and present those results as a sensitivity analysis in the online supplementary material Table 1. Based on the sensitivity analysis and clinical judgment, we applied a 90-day clean period when the index fracture is wrist or shoulder followed by a subsequent fracture of the same type.
Secondary outcome measure
We were also interested in a more broad assessment of the burden of subsequent fractures—one that incorporates other types of fracture that may be associated with osteoporosis. To do so, we also looked for the occurrence of other upper and lower extremity fractures. We applied a similar approach requiring no fracture of the same type one year prior to exclude a visit simply for follow-up care and selected claims with an appropriate diagnosis and treatment indicator. We did not include vertebral fractures because many are asymptomatically detected on imaging precluding identification of a reliable date of onset [6].
Covariates
We describe the age-, race-, and gender-specific rates of each fracture type then determine the rate and type of subsequent fracture occurring in the year following the index fracture. Date of birth, date of death, race, and gender were obtained from the Medicare enrollment file. Age was calculated at the date of the index fracture. Race was categorized as white, black, Hispanic and other. Comorbidity was measured with the Charlson Comorbidity Score calculated based on diagnoses identified in the year prior to index fracture and it was categorized as a score of 0, 1, 2, or 3 or more [7, 8].
Statistical analysis
We calculated the rate of second fracture per 100,000 person-years by type of incident fracture, age and gender of beneficiary, where the person-year was defined starting from the date of the index fracture and ending at the date of the second fracture, death, or one year from the index fracture, whichever is earliest. We analyzed the time to the second fracture, treating death as a censoring event, and estimated the percent with second fracture at one year based on a Kaplan-Meier curve, stratified by location of the index fracture. This statistical approach explicitly takes into account the competing risk of death which is substantial among older adults who experience a fragility fracture. We used Cox proportional hazards regression models to estimate the predicted probability and 95 % CIs of a second fracture within one year of the index fracture, including type of index fracture, age, gender, and comorbidity and all interactions among these four covariates. This model also adjusted for race.
Results
Cohort description
In 2009, there were 273,330 fee-for-service Medicare beneficiaries who suffered either a hip, shoulder or wrist fracture related to osteoporosis in the USA. Figure 1 describes the identification algorithm, the numbers of people excluded, and our final study population. The population of patients with an index fracture was composed of 161,072 (59 %) with a hip fracture, 37,716 (14 %) with a shoulder fracture, and 74, 542 (27 %) with wrist fracture.
Differences between the three index fracture types
The characteristics of the people having each type of index fracture were quite different as shown in Table 1. Hip fracture patients, as expected, were on average older, had higher comorbidity, and were more likely to die within a year of the index fracture. Shoulder fracture patients were intermediate between hip and wrist fracture patients in their mean age, level of comorbidity, and percentage dying in one year. While women were more likely to have any fracture, the gender imbalance was higher for wrist (14 % male) and shoulder (19 % male) compared with hip fracture (26 % male). Survival to the end of the observation period was highly variable across the three index fracture types (73 % for hip, 87 % for shoulder, and 93 % for wrist).
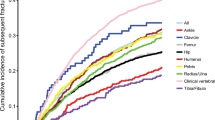
Second fracture
A total of 11,885, or 4.2 % of the fracture cohort sustained a subsequent hip, shoulder, or wrist fracture within a year. The most common second fracture type was hip, regardless of the type of index fracture. When we included other types of upper or lower extremity fractures in the count of subsequent fractures, 14,326 (5.2 %) of patients had a second fracture. Figure 2 shows that the distribution of fracture type for the subsequent fracture is similar regardless of the type of index fracture. The overall rate of second fracture per 100,000 person-years was 7386 (S.E. 79) per 100,000 for hip, 5871 (S.E. 135) per 100,000 for shoulder, and 5499 (S.E. 90) per 100,000 for wrist. The Kaplan-Meier plot (Online Supplementary Figure 1) confirmed the difference between fracture rates in hip compared to shoulder and wrist but does not show a clear pattern of early versus late second fracture occurrence over one year following index fracture.
Stratified crude analysis—age and gender
Several notable findings emerge in Table 2, which shows crude rate of second fracture per 100,000 person-years stratified by index fracture and subsequent fracture location as well as gender and age. Though the second fracture rate after wrist (5433 per 100,000) or shoulder (5871 per 100,000) was significantly less than after hip fracture (7386 per 100,000) (p value <0.0001), the magnitude of these differences was less than expected. In addition, some factors that are strongly related with first fracture incidence appear to have relatively smaller effects in second fracture occurrence. Women have generally, but not universally, higher rates than men and the relative differences appear smaller. Finally, the association of age with second fracture seems lower among people whose index fracture was a wrist or shoulder fracture compared to hip. None of these crude results, however, take into account the potential interactions between age, comorbidity, gender or type of index fracture.
Predicted probability of second fracture
We estimated the predicted probability of second fracture, expressed as the percentage of people who fracture in one year (Fig. 3). This fully adjusted model of subsequent fracture includes interaction terms between index type of fracture, gender, and comorbidity (Table 3 for point estimates and Online Supplementary Table 3 for model coefficients). Men and women face similar risks with frequently overlapping confidence intervals except among those over age 85 years. A similar rise in risk is seen with both age and comorbidity, the exception being that the oldest men with an index hip or shoulder fracture do not see the same stepwise increase in risk with comorbidity as in other age groups. The results were unchanged when we used the fracture outcome at 6 versus 12 months.
Discussion
Using a large, national cohort of older adults who sustained an osteoporosis-related hip, shoulder, or wrist fracture, we report the rate of second fracture at one year taking into account the competing risk of death and the independent effects of age, gender, comorbidity and type of first fracture. Importantly, our study is inclusive of a broadly representative older population including the entire USA and people across all fee-for-service care settings. Our main finding is that while age and comorbidity have strong effects on risk of second fracture, the risk does not differ markedly based on whether an individual has an index wrist, shoulder or hip fracture or on gender. This finding highlights the importance of attention to fracture prevention following osteoporotic fractures at any site among both men and women.
The opportunity to identify and intervene on a population of people who have substantially elevated risk of fracture by targeting older adults who have already sustained an osteoporotic fracture has received attention as a means for improving health outcomes in those with established osteoporosis [9]. This is evidenced by initiatives of specialty groups such as the American Orthopedics Association “Own the Bone” campaign [10] and by the fact that attention to osteoporosis following a fragility fracture in older women is a HEDIS quality of care measure [11]. While the current literature provides evidence on the magnitude of subsequent fracture risk [3, 4, 12, 13], data sources and limited sample sizes have hampered studies in delving more deeply at the individual level to understand particular population sub-groups. Thus, we have been limited in identifying where there may be inadequate preventive interventions undertaken.
Two prior meta-analyses have summarized results across many studies which similarly find that risk of second fracture is elevated after hip or wrist fracture with a relative risk between 1.5–2.0 [3, 4]. Our results reinforce this finding and go further by adjusting for age, comorbidity, and censoring for death. These factors are important because there are differences in the type of people who have an incident wrist or shoulder fracture from those who have hip fracture. For example, wrist fractures tend to occur more often in younger elderly that may confound analyses of secondary fracture risk [3]. Our findings suggests that while hip fractures draw great attention in research and policy, if the interest is in reducing the risk of subsequent fracture, individuals sustaining wrist and shoulder fractures warrant a similar level of focused attention.
Furthermore, the differences in risk of second fracture are related more to the personal characteristics, particularly age and comorbidity, than to type of index fracture (Table 3). While a younger person may have a longer exposure time to have a subsequent fracture, in the immediate period up to one year from index fracture, older persons are at twice the risk of fracture. Unlike our study, Kanis showed a non-significant declining risk of subsequent fracture with age, however there was no accounting for time between the index and subsequent fracture and it is unclear how competing risk of death was handled [3]. Another single institution study reported that the risk of second fracture was greatest in young adults in a study over 12 years following people aged 45 years and older [5]. Their result was based on calculated re-fracture as a proportion of total fractures using a person-year analysis censoring for death. Their result may reflect that the underlying fracture rate in older adults is much higher than younger adults such that the fraction re-fracturing appears lower, whereas young people who sustain a fragility fracture are at exceptionally high risk or alternatively remain more active and at risk to fall and fracture.
Lastly, the difference between men and women in incidence of osteoporotic fracture, a forty percent higher age-adjusted rate of incident fracture in women [14], is less prominent when examining second fracture. Yet the number of women who sustain a second fracture (N = 11808 or 82 % of second fractures) still dwarfs the number of men (N = 2518 or 18 % of second fractures); a difference driven by the number women who have a first fracture—not the risk of second fracture. The salience of this finding is that in clinical practice, the dominance of women fracturing may influence whether clinicians address the future risk in men as rigorously as in women. Other studies have shown that men who fracture warrant assessment for treatment with bisphosphonates [15], yet men have less knowledge about their osteoporosis risk [16] and are less likely to be treated with antiresorptive medications [17].
Our approach to assessing subsequent fracture risk draws on a national database large enough to estimate the risk of second fracture while incorporating detailed information about patient characteristics. This may be important for planning population strategies for secondary fracture prevention to minimize further impairment and costs of subsequent fracture. Importantly, using our claims-based approach makes it possible to evaluate clinical outcomes across health care environments and in smaller sub-groups of at-risk people.
Limitations
Our methodological approach using a large administrative database and analytic methods that account for competing risk of death and other factors on risk of second fracture is not without limitations. While administrative data from a large population provide detailed information about health care use and long term outcomes, there is an absence of detailed information about behavioral or biological measures. One of the specific measures we do not have is baseline bone mineral density (BMD) or whether people are on medications that alter their BMD. Kanis shows, however, that adjusting for BMD had only a small effect on risk of second fracture in women and no statistically significant effect in men [3]. In addition, the osteoporosis treatment guidelines generally recommend treatment for osteoporosis when a person sustains a fragility fracture without regard for BMD when they are older than 50.
A second limitation is that our estimates of second fracture rate are dependent on the ability within claims to identify onset of new fractures as distinct events. For this reason, we did not include vertebral fractures in our analysis. We also developed a strategy to assure that we do not include follow-up care as a new event for fractures managed in the outpatient setting. We did so by using a 90-day clean period, chosen because beyond 90 days the fracture rates were fairly stable. However, the limitation imposed by this methodological barrier is that any same location new fracture to the upper extremity that occurs within 90 days will not be captured. The impact on overall fracture rates, however, will be low as same location upper extremity fractures are infrequent (less than 1 % of total observed fractures).
Implications
From this large national study of the second fracture occurrence after an incident osteoporotic fracture in the USA, we provide estimates of subsequent fracture rates that take into account gender, age, comorbidity and type of index fracture as well as the competing risk of death. Defining the populations at risk is an essential first step toward understanding how delivery of care can be improved to reduce secondary fracture risk. Effort to identify areas where interventions may improve care and reduce the burden of osteoporotic fractures the most will benefit from these estimates of risk in the population of elders who sustain fractures in the USA.
References
Dennison E, Cole Z, Cooper C (2005) Diagnosis and epidemiology of osteoporosis. Curr Opin Rheumatol 17(4):456–461
Kanis JA (2002) Diagnosis of osteoporosis and assessment of fracture risk. Lancet 359(9321):1929–1936
Kanis JA, Johnell O, De Laet C et al (2004) A meta-analysis of previous fracture and subsequent fracture risk. Bone 35(2):375–382
Klotzbuecher CM, Ross PD, Landsman PB et al (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res Off J Am Soc Bone Miner Res 15(4):721–739
Robinson CM, Royds M, Abraham A et al (2002) Refractures in patients at least forty-five years old. a prospective analysis of twenty-two thousand and sixty patients. J Bone Joint Surg Am Vol 84-A(9):1528–1533
Cooper C, Atkinson EJ, O’Fallon WM et al (1992) Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985–1989. J Bone Miner Res Off J Am Soc Bone Miner Res 7(2):221–227
Radley DC, Gottlieb DJ, Fisher ES et al (2008) Comorbidity risk-adjustment strategies are comparable among persons with hip fracture. J Clin Epidemiol 61(6):580–587
Romano PS, Roos LL, Jollis JG (1993) Adapting a clinical comorbidity index for use with ICD-9-CM administrative data: differing perspectives. J Clin Epidemiol 46(10):1075–1079, discussion 81-90
Eisman JA, Bogoch ER, Dell R et al (2012) Making the first fracture the last fracture: ASBMR task force report on secondary fracture prevention. J Bone Miner Res Off J Am Soc Bone Miner Res 27(10):2039–2046
American Orthopaedic Association. Own the Bone. Secondary Own the Bone. http://www.ownthebone.org/about-own-the-bone.aspx
National Committee for Quality Assurance. Osteoporosis testing and management in older women. Secondary osteoporosis testing and management in older women 2014. http://www.ncqa.org/ReportCards/HealthPlans/StateofHealthCareQuality/2014TableofContents/Osteoporosis.aspx
Lee YK, Ha YC, Yoon BH et al (2013) Incidence of second hip fracture and compliant use of bisphosphonate. Osteoporos Int: J Established Result Cooperation Between Eur Foundation Osteoporos Nat Osteoporos Foundation USA 24(7):2099–2104
Melton LJ 3rd, Kearns AE, Atkinson EJ et al (2009) Secular trends in hip fracture incidence and recurrence. Osteoporos Int: J Established Result Cooperation Between Eur Foundation Osteoporos Nat Osteoporos Foundation USA 20(5):687–694
Melton LJ 3rd, Crowson CS, O'Fallon WM (1999) Fracture incidence in Olmsted County, Minnesota: comparison of urban with rural rates and changes in urban rates over time. Osteoporos Int: J Established Result Cooperation Between Eur Foundation Osteoporos Nat Osteoporos Foundation USA 9(1):29–37
Schousboe JT, Taylor BC, Fink HA et al (2007) Cost-effectiveness of bone densitometry followed by treatment of osteoporosis in older men. JAMA: J Am Med Assoc 298(6):629–637. doi:10.1001/jama.298.6.629
Gaines JM, Marx KA, Caudill J et al (2010) Older men’s knowledge of osteoporosis and the prevalence of risk factors. J Clin Densitometry: Off J Int Soc Clin Densitometry 13(2):204–209
Kiebzak GM, Beinart GA, Perser K et al (2002) Undertreatment of osteoporosis in men with hip fracture. Arch Intern Med 162(19):2217–2222
Acknowledgments
This study was supported by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (#P60 AR062799).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interests.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 120 kb)
Supplementary Figure 1
(GIF 52 kb)
Online Supplementary Table 1
(DOCX 31 kb)
Online Supplementary Table 3
(DOCX 39 kb)
Rights and permissions
About this article
Cite this article
Bynum, J.P.W., Bell, JE., Cantu, R.V. et al. Second fractures among older adults in the year following hip, shoulder, or wrist fracture. Osteoporos Int 27, 2207–2215 (2016). https://doi.org/10.1007/s00198-016-3542-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-016-3542-6