Abstract
Summary
Trabecular bone scores (TBS) have recently been developed as a diagnostic tool to assess bone texture. We studied thyroid status and TBS in a population-based cohort and demonstrated that high-normal thyroxine levels are associated with low TBS in healthy euthyroid postmenopausal women.
Introduction
Increased thyroid hormone levels affect bone mineral density (BMD) and, if untreated, increase the risk of fracture. However, the relationship between thyroid function and bone microarchitecture has not yet been established. Trabecular bone scores (TBS) are gray-level textural measurements of dual energy X-ray absorptiometry (DXA) images. The TBS has been proposed as an indirect index of bone microarchitecture. The goal of this study was to characterize the relationship between thyroid function and TBS in euthyroid men and postmenopausal euthyroid women.
Methods
A total of 1376 euthyroid subjects (648 postmenopausal women and 728 men) were recruited from a community-based cohort in Korea. Free thyroxine (fT4) levels, thyroid stimulating hormone (TSH) levels, BMD, and TBS were measured and compared.
Results
There was no significant relationship between either fT4 or TSH levels and BMD in men and women. Multiple linear regression analysis showed that high-normal fT4 levels were negatively correlated with TBS (β = −0.111; P = 0.002, after adjusting for both age and body mass index [BMI]) in postmenopausal women. In men, however, there was no significant correlation between fT4 levels and TBS. TSH levels were not significantly associated with TBS in either men or women.
Conclusion
Higher fT4 levels within the normal reference range are associated with deterioration of trabecular microarchitecture in healthy euthyroid postmenopausal women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hyperthyroidism, which is characterized by elevated thyroid hormone levels and high metabolic state, is often accompanied by bone loss and increased risk of fracture [1]. When osteoporosis accompanies hyperthyroidism, increased thyroxine levels have been implicated as a culprit for the decreased bone density [2] through accelerated bone turnover [3] and shortening of the remodeling cycle [4]. In addition, in subclinical hyperthyroidism where the thyroxine level is normal but thyroid stimulating hormone (TSH) level is decreased, the reduced levels of TSH have been shown to be associated with the decreased bone mass [5–7], suggesting that TSH per se may have a direct effect on bone remodeling. This notion was also supported by in vivo studies that analyzed the effect of TSH on bone mass independent of thyroid hormones [8–10]. Furthermore, high-normal thyroxine or low-normal TSH levels are reportedly associated with low bone mineral density (BMD) in euthyroid subjects [11–13], indicating that bone mass is affected by both thyroid hormone and TSH levels, even when thyroid function is normal.
In addition to bone mass, bone quality, as measured by trabecular microarchitecture, is also influenced by thyroid status [14]. Low-dose TSH treatment has been reported to improve bone microarchitecture in ovariectomized rats [10], while trabecular thinning and reduced connectivity were identified in a mouse model of thyrotoxicosis [15]. However, the relationship between thyroid function and bone microarchitecture has not yet been studied in humans.
Osteoporosis is a progressive bone disease characterized by a decrease in bone mass and deterioration of bone microarchitecture. Measurement of BMD with dual energy X-ray absorptiometry (DXA) is a standard method both for diagnosis of osteoporosis and monitoring of treatment efficacy [16]. Although BMD is a strong predictor of subsequent fractures, it is not the only measure of bone strength and quality. Trabecular bone microarchitecture is a key factor that determines bone quality; bone turnover and mineralization are also important. However, none of these factors can be assessed by DXA. A new texture parameter, trabecular bone score (TBS), has recently been developed as an indirect measurement of trabecular microarchitecture [17]. TBS values are determined by quantifying pixel gray-level variations in two-dimensional DXA images. Low TBS values are related to altered bone microarchitecture and increased risk of fragility fractures, independent of BMD [18]. An international working group of TBS users has proposed TBS cut-off values for postmenopausal women: normal for TBS values over 1.350, partly degraded microarchitecture for values between 1.200 and 1.350, and degraded for values 1.200 or less [19] (http://www.medimapsgroup.com/upload/MEDIMAPS-UK-WEB.pdf).
In this study, we analyzed the results of thyroid function tests and TBS in a community-dwelling general population to assess the association between thyroid function and bone texture.
Subjects and methods
Study population
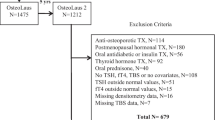
Study participants were recruited from among participants of the Ansung cohort study, a community-based cohort living in rural Korea. Details of the Ansung cohort study have been described elsewhere [20]. Briefly, the study started in 2001 and participants have undergone regular biennial examinations since that time. Thyroid function tests and DXA scans were performed as part of the subjects’ sixth biennial examination in 2011–2012. From this cohort, 2307 postmenopausal women and 2240 men were recruited. Individuals who had undergone thyroid surgery or had been diagnosed with thyroid disease were excluded, as were individuals taking steroids, treatments for osteoporosis, or anti-epilepsy drugs. No subject with a history of taking antiarrhythmic drugs reported use of amiodarone. In order to include only euthyroid subjects, subjects were excluded for abnormal thyroid function test results or for incomplete test data. The final data were based on 648 postmenopausal women and 728 men, all of whom had normal thyroid function (Fig. 1). The study was approved by the Institutional Review Board of the Korean National Institute of Health.
Measurements of thyroid function and skeletal parameters
BMD of the lumbar vertebrae (L1–L4), femoral neck, and total hip were evaluated using DXA scan images (Lunar Prodigy; GE Medical Systems) and analyzed (Encore Software version 11.0). The percent coefficient of variation of BMD (precision error) was 1.7 % for lumbar spine, 1.8 % for femoral neck, and 1.7 % for total hip measurements. Lumbar spine TBS measurements were generated from lumbar spine DXA files using TBS iNsight Software version 2.0.0.1 (Med-Imaps, Geneva, Switzerland). The precision of TBS was 1.5 %. TSH and free thyroxine (T4) levels were measured using a chemiluminescent immunoassay (CLIA; ADVIA centaur; Siemens, Berlin, Germany). Reference ranges for the thyroid function tests were 0.35–5.5 μU/mL for TSH and 0.89–1.76 ng/L for free T4. The intra- and inter-assay percent coefficients of variation were 2.7 and 2.9 % for free T4 and 2.0 and 1.6 % for TSH, respectively.
Statistics
Data are expressed as mean ± standard deviation. The correlations between thyroid function parameters and bone measurements were estimated by Pearson’s correlation analysis. Multiple linear regression models were applied to evaluate the association between thyroid function and TBS after adjusting for age, body mass index (BMI), and BMD. Subjects were divided into tertiles according to free T4 levels. Groups were compared with a χ 2 test based on the numbers of subjects with degraded microarchitecture. PASW Statistics for Windows, version 18.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis; P values <0.05 were considered statistically significant.
Results
The characteristics of the study subjects are shown in Table 1. The women and men were of similar age, 64.9 ± 8.0 and 64.0 ± 8.1 years, respectively. Mean TSH levels were significantly higher in women than in men (2.02 ± 1.04 μU/mL vs. 1.71 ± 0.89 μU/mL; P < 0.001) while mean fT4 levels were slightly but significantly lower in women (1.15 ± 0.14 ng/dL vs. 1.19 ± 0.15 ng/dL; P < 0.001). Mean TBS levels were significantly higher in women compared with men (1.343 ± 0.089 vs. 1.297 ± 0.092; P < 0.001). Mean BMD of lumbar spine (L1-4), femur neck, and total hip was significantly higher in men as expected.
There was a negative correlation between TSH and fT4 levels in both sexes, as expected: r = −0.204, P < 0.001 in women and r = −0.078, P = 0.035 in men. The TBS levels of L1-4 correlated positively with BMD of L1-4 in both sexes (r = 0.431, P < 0.001 in women and r = 0.263, P < 0.001 in men).
Multiple linear regression models used to determine the relationships between thyroid hormone levels and bone parameters revealed that TBS of L1-4 were negatively associated with fT4 levels in women (Table 2, Fig. 2). After adjusting for age and BMI, the values were β = −0.111 and P = 0.002; the association remained significant after additional adjustment for BMD of L1-4 (β = −0.098, P = 0.005; Table 2). However, there was no relationship between TSH and TBS in women (β = −0.043, P = 0.239; Fig 2, right panel). Neither TSH nor fT4 levels were correlated with TBS in men. BMDs of L1-4, the femur neck, and total hip did not correlate with TSH or fT4 levels in either men or women (Table 2). When we divided the subjects into tertiles according to fT4 levels, 3.4, 6.7, and 9.7 % of subjects in each tertile group had TBS values ≤1.200, the cut-off for “degraded microarchitecture [19]” (Fig. 2, left panel).
Discussion
Trabecular bone microarchitecture is an important determinant of bone strength [21]. It is usually assessed by high-resolution magnetic resonance imaging or multi-slice computed tomography [22, 23], but these techniques are expensive, time consuming, and hard to apply in the general population. The TBS has been recently developed to evaluate trabecular microarchitecture from DXA images. Relationships between TBS and three-dimensional trabecular microarchitecture parameters have been well documented in a human cadaver study using micro-computed tomography [24], which confirms the validity of the score. In addition, TBS combined with BMD improved the power to predict fracture risk in clinical studies [25, 26]. Hence, TBS is a promising tool for assessing trabecular microarchitecture and predicting fractures [27]. Decreased TBS have been shown to be associated with primary hyperparathyroidism [28], diabetes mellitus [29], glucocorticoid use [30], and subclinical hypercortisolism [31], even in the absence of obvious changes in lumbar spine BMD [28].
In this study, we observed that free T4 levels are negatively correlated with TBS in euthyroid postmenopausal women recruited from a community-dwelling cohort. This is a novel observation and extends the role of TBS in detecting subtle changes in bone microarchitecture in subclinical thyroid dysfunction. It has been well established that thyrotoxicosis is associated with increased risk of fracture through enhanced bone resorption and decreased bone mass [1, 5–7]. In addition, several lines of evidence indicate that high-normal thyroxine levels also may be harmful to trabecular bone microarchitecture and increase fracture risk in postmenopausal women [13, 32] Therefore, although we have not studied the fracture incidence in our cohort, the results of this study suggest that subtle changes in bone textures that occur in subclinical hyperthyroidism may contribute to increased fracture risk.
Unlike the TBS, we did not observe significant change in BMD according to fT4 or TSH levels within normal range. This result is inconsistent with previous studies that demonstrated decreased BMD in postmenopausal women with high-normal thyroxine and low-normal TSH levels. While we used fT4, TSH, and BMD levels as a continuum and analyzed whole subjects, previous studies have divided subjects into tertiles or quartiles and compared the highest fT4 quartile to the others [33] or the highest TSH tertile to the lowest [12] with respect to the BMD. Another study also divided the subjects based on the TSH level (high or low) and compared the proportion of participants with osteoporosis rather than comparing BMD values [11]. These different statistical methods may have contributed to the positive relationships reported in these studies, which might not have been evident if both parameters were used as continuous variables as in our study. One study, which used essentially the same method as ours, demonstrated significant correlation between fT4 levels and hip BMD levels, both used as continuous variables [13]. However, the β coefficient in that study was −0.051 with a P value of 0.040, which is very close to that in our study (β coefficient −0.048 and P value 0.054). Given the difference in the number of subjects (N = 1278 vs. N = 648 in our study), we speculate that our relatively small number of subjects may not have enough power to reveal an association between fT4 levels and BMD.
We have shown that fT4 but not TSH levels are associated with TBS of the lumbar spine in Korean postmenopausal women. The dominant effects of fT4 over TSH on skeletal phenotypes were also observed in a report by Murphy et al., who showed that upper normal thyroid hormone levels are associated with decreased hip BMD, while TSH levels are not [13]. Patients with isolated TSH deficiencies had normal BMD values following thyroxine treatment, also suggesting that TSH deficiency has only minor skeletal effects [34]. The predominant effects of thyroid hormone over TSH are also supported by a mouse model of thyroid hormone resistance (TRβ¯/¯). These mice had increased bone resorption and an osteoporotic phenotype accompanied by elevated TSH and thyroid hormone levels [15]. Our finding is consistent with these results, suggesting that elevated thyroid hormone levels, rather than the accompanying decreased TSH levels, predominate in thyroid regulation of bone health.
Interestingly, we were not able to identify a significant change in TBS according to fT4 levels in men. The reason for this discrepancy is not clear. It may result from a genuine lack of effects of fT4 on the skeletal microarchitecture in men through yet unidentified mechanisms. Alternatively, it may simply reflect the insufficient optimization or validation of the version of TBS software we used in this study for clinical use in men. TBS values are reportedly lower in men than in women due to thicker spine tissue, based on findings from a Caucasian study [35]. We have also found that TBS values in men are slightly lower than those in women (1.297 in men vs. 1.343 in women). As the TBS measurement includes an adjustment for soft tissue estimated from BMI, the increased spine tissue thickness in men results in greater X-ray absorption and less patterned images and therefore lower TBS values [35, 36]. Although we have not directly measured spine tissue thickness in this study, higher BMI values in men may have contributed to their lower TBS values. This inherent limitation of the TBS estimation in men may have contributed to our failure to observe subtle changes in microarchitecture among men with high-normal fT4 levels. Another limitation of TBS to be noted is the cut-off value for the degraded microarchitecture. Although we have observed that increasing proportion of subjects belong to the “degraded microarchitecture” category as fT4 levels increase in Fig. 2, the cut-off level we used was recommended by TBS working group to be applied for postmenopausal women only and a well-established cut-off level for “abnormal” TBS has yet to be defined. The definition of abnormal TBS should be extensively validated across age, gender, and ethnicity.
Our study has a number of limitations. As a cross-sectional design, the casual relationship between high-normal fT4 levels and TBS degradation cannot be definitely stated. Another limitation may be the measurement of TBS in men, which has not been sufficiently validated yet. Notwithstanding these limitations, this study is the first demonstration of association between thyroid function and TBS values, extending the utility of this new technology to one of the most common endocrine dysfunctions. The results of our study have clinical implications for management of subclinical hyperthyroidism; it is possible that even slight increases in fT4 levels within the upper normal range may be associated with deterioration of bone microarchitecture. This is especially important as TBS changes become evident before any obvious change in BMD. Further studies of the effects of subclinical hyper- and hypothyroidism on TBS should help to determine optimal level of thyroid hormone that does not jeopardize bone quality. Clinical studies of the effects of thyroxine on TBS and their relationship with the risk of fracture are also warranted.
References
Vestergaard P, Mosekilde L (2003) Hyperthyroidism, bone mineral, and fracture risk—a meta-analysis. Thyroid 13:585–593
Ross DS (1994) Hyperthyroidism, thyroid hormone therapy, and bone. Thyroid 4:319–326
Mosekilde L, Melsen F, Bagger JP, Myhre-Jensen O, Schwartz Sorensen N (1977) Bone changes in hyperthyroidism: interrelationships between bone morphometry, thyroid function and calcium-phosphorus metabolism. Acta Endocrinol (Copenh) 85:515–525
Eriksen EF, Mosekilde L, Melsen F (1985) Trabecular bone remodeling and bone balance in hyperthyroidism. Bone 6:421–428
Tauchmanova L, Nuzzo V, Del Puente A, Fonderico F, Esposito-Del Puente A, Padulla S, Rossi A, Bifulco G, Lupoli G, Lombardi G (2004) Reduced bone mass detected by bone quantitative ultrasonometry and DEXA in pre- and postmenopausal women with endogenous subclinical hyperthyroidism. Maturitas 48:299–306
Belaya ZE, Melnichenko GA, Rozhinskaya LY, Fadeev VV, Alekseeva TM, Dorofeeva OK, Sasonova NI, Kolesnikova GS (2007) Subclinical hyperthyroidism of variable etiology and its influence on bone in postmenopausal women. Hormones (Athens) 6:62–70
Lee WY, Oh KW, Rhee EJ et al (2006) Relationship between subclinical thyroid dysfunction and femoral neck bone mineral density in women. Arch Med Res 37:511–516
Galliford TM, Murphy E, Williams AJ, Bassett JH, Williams GR (2005) Effects of thyroid status on bone metabolism: a primary role for thyroid stimulating hormone or thyroid hormone? Minerva Endocrinol 30:237–246
Abe E, Marians RC, Yu W et al (2003) TSH is a negative regulator of skeletal remodeling. Cell 115:151–162
Sampath TK, Simic P, Sendak R, Draca N, Bowe AE, O’Brien S, Schiavi SC, McPherson JM, Vukicevic S (2007) Thyroid-stimulating hormone restores bone volume, microarchitecture, and strength in aged ovariectomized rats. J Bone Miner Res 22:849–859
Morris MS (2007) The association between serum thyroid-stimulating hormone in its reference range and bone status in postmenopausal American women. Bone 40:1128–1134
Kim DJ, Khang YH, Koh JM, Shong YK, Kim GS (2006) Low normal TSH levels are associated with low bone mineral density in healthy postmenopausal women. Clin Endocrinol (Oxf) 64:86–90
Murphy E, Gluer CC, Reid DM, Felsenberg D, Roux C, Eastell R, Williams GR (2010) Thyroid function within the upper normal range is associated with reduced bone mineral density and an increased risk of nonvertebral fractures in healthy euthyroid postmenopausal women. J Clin Endocrinol Metab 95:3173–3181
Brandi ML (2009) Microarchitecture, the key to bone quality. Rheumatology (Oxford) 48(Suppl 4):iv3–iv8
Bassett JH, O’Shea PJ, Sriskantharajah S et al (2007) Thyroid hormone excess rather than thyrotropin deficiency induces osteoporosis in hyperthyroidism. Mol Endocrinol 21:1095–1107
World Health Organization (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Organ Tech Rep Ser 843:1–129
Pothuaud L, Carceller P, Hans D (2008) Correlations between grey-level variations in 2D projection images (TBS) and 3D microarchitecture: applications in the study of human trabecular bone microarchitecture. Bone 42:775–787
Bousson V, Bergot C, Sutter B, Levitz P, Cortet B, Scientific Committee of the Groupe de Recherche et d’Information sur les O (2012) Trabecular bone score (TBS): available knowledge, clinical relevance, and future prospects. Osteoporos Int 23:1489–1501
Silva BC, Bilezikian JP (2014) Trabecular bone score: perspectives of an imaging technology coming of age. Arq Bras Endocrinol Metabol 58:493–503
Shin CS, Choi HJ, Kim MJ et al (2010) Prevalence and risk factors of osteoporosis in Korea: a community-based cohort study with lumbar spine and hip bone mineral density. Bone 47:378–387
Dalle Carbonare L, Giannini S (2004) Bone microarchitecture as an important determinant of bone strength. J Endocrinol Investig 27:99–105
Boutroy S, Bouxsein ML, Munoz F, Delmas PD (2005) In vivo assessment of trabecular bone microarchitecture by high-resolution peripheral quantitative computed tomography. J Clin Endocrinol Metab 90:6508–6515
Krug R, Banerjee S, Han ET, Newitt DC, Link TM, Majumdar S (2005) Feasibility of in vivo structural analysis of high-resolution magnetic resonance images of the proximal femur. Osteoporos Int 16:1307–1314
Hans D, Barthe N, Boutroy S, Pothuaud L, Winzenrieth R, Krieg MA (2011) Correlations between trabecular bone score, measured using anteroposterior dual-energy X-ray absorptiometry acquisition, and 3-dimensional parameters of bone microarchitecture: an experimental study on human cadaver vertebrae. J Clin Densitom 14:302–312
Hans D, Goertzen AL, Krieg MA, Leslie WD (2011) Bone microarchitecture assessed by TBS predicts osteoporotic fractures independent of bone density: the Manitoba study. J Bone Miner Res 26:2762–2769
Del Rio LM, Winzenrieth R, Cormier C, Di Gregorio S (2013) Is bone microarchitecture status of the lumbar spine assessed by TBS related to femoral neck fracture? A Spanish case-control study. Osteoporos Int 24:991–998
Silva BC, Leslie WD, Resch H, Lamy O, Lesnyak O, Binkley N, McCloskey EV, Kanis JA, Bilezikian JP (2014) Trabecular bone score: a noninvasive analytical method based upon the DXA image. J Bone Miner Res 29:518–530
Romagnoli E, Cipriani C, Nofroni I et al (2013) “Trabecular Bone Score” (TBS): an indirect measure of bone micro-architecture in postmenopausal patients with primary hyperparathyroidism. Bone 53:154–159
Leslie WD, Aubry-Rozier B, Lamy O, Hans D, Manitoba Bone Density P (2013) TBS (trabecular bone score) and diabetes-related fracture risk. J Clin Endocrinol Metab 98:602–609
Leslie WD, Krieg MA, Hans D, Manitoba Bone Density P (2013) Clinical factors associated with trabecular bone score. J Clin Densitom 16:374–379
Eller-Vainicher C, Morelli V, Ulivieri FM et al (2012) Bone quality, as measured by trabecular bone score in patients with adrenal incidentalomas with and without subclinical hypercortisolism. J Bone Miner Res 27:2223–2230
Roef G, Lapauw B, Goemaere S, Zmierczak H, Fiers T, Kaufman JM, Taes Y (2011) Thyroid hormone status within the physiological range affects bone mass and density in healthy men at the age of peak bone mass. Eur J Endocrinol 164:1027–1034
van Rijn LE, Pop VJ, Williams GR (2014) Low bone mineral density is related to high physiological levels of free thyroxine in peri-menopausal women. Eur J Endocrinol 170:461–468
Papadimitriou A, Papadimitriou DT, Papadopoulou A, Nicolaidou P, Fretzayas A (2007) Low TSH levels are not associated with osteoporosis in childhood. Eur J Endocrinol 157:221–223
Leslie WD, Lix L, Morin S, Majumdar S, Hans D (2014) Difference in spine TBS between men and women: real or technical? Osteoporos Int 25:S25–S26
Leslie WD, Aubry-Rozier B, Lix LM, Morin SN, Majumdar SR, Hans D (2014) Spine bone texture assessed by trabecular bone score (TBS) predicts osteoporotic fractures in men: The Manitoba Bone Density Program. Bone 67:10–14
Acknowledgments
This work was supported by the Research Program funded by the Korea Centers for Disease Control and Prevention (funds 2011-E71008-00 and 2012-E71008-00) and also supported by a grant from the Korean Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (HI12C1338). The funding source had no role in the collection of the data or in the decision to submit this manuscript for publication.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Hwangbo, Y., Kim, J.H., Kim, S.W. et al. High-normal free thyroxine levels are associated with low trabecular bone scores in euthyroid postmenopausal women. Osteoporos Int 27, 457–462 (2016). https://doi.org/10.1007/s00198-015-3270-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3270-3