Abstract
Summary
This study evaluated changes in spinal alignment and quality of life (QOL) after corrective spinal surgery for patients with postmenopausal osteoporosis and spinal kyphosis. Spinal global alignment and QOL were significantly improved after corrective spinal surgery but did not reach the level of non-operated controls.
Introduction
With the increased aging of society, the demand for corrective spinal instrumentation for spinal kyphosis in osteoporotic patients is increasing. However, previous studies have not focused on the improvement of quality of life (QOL) after corrective spinal surgery in patients with osteoporosis, compared to non-operated control patients. The purposes of this study were thus to evaluate changes in spinal alignment and QOL after corrective spinal instrumentation for patients with osteoporosis and spinal kyphosis and to compare these results with non-operated patients.
Methods
Participants comprised 39 patients with postmenopausal osteoporosis ≥50 years old who underwent corrective spinal surgery using multilevel posterior lumbar interbody fusion (PLIF) for symptomatic thoracolumbar or lumbar kyphosis, and 82 age-matched patients with postmenopausal osteoporosis without prevalent vertebral fractures. Spinopelvic parameters were evaluated with standing lateral spine radiography, and QOL was evaluated with the Japanese Osteoporosis QOL Questionnaire (JOQOL), SF-36, and Roland-Morris Disability Questionnaire (RDQ).
Results
Lumbar kyphosis angle, sagittal vertical axis, and pelvic tilt were significantly improved postoperatively. QOL evaluated with all three questionnaires also significantly improved after 6 months postoperatively, particularly in domain and subscale scores for pain and general/mental health. However, these radiographic parameters, total JOQOL score, SF-36 physical component summary score, and RDQ score were significantly inferior compared with non-operated controls.
Conclusions
The results indicate that spinal global alignment and QOL were significantly improved after corrective spinal surgery using multilevel PLIF for patients with osteoporosis and spinal kyphosis but did not reach the level of non-operated controls.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a disorder that generally affects the biomechanical competence of bone and leads to an increased risk of fractures, with older female patients as the most severely affected population. Osteoporotic patients frequently suffer spinal kyphosis; this often results from vertebral fractures, the most common clinical manifestation of the disease, but is also related to weakness of the back extensor muscles [1, 2] and intervertebral disc degeneration. Spinal kyphosis in patients with osteoporosis causes chronic back pain and significant functional impairments in activities of daily living (ADL) [3–6]. These functional impairments by spinal kyphosis also influence the quality of life (QOL) in patients with osteoporosis [5–8].
With the increased aging of society worldwide, the demand for corrective spinal instrumentation for spinal kyphosis is increasing even for osteoporotic elderly patients. In cases of adult spinal deformity, recent studies have shown that positive sagittal plane imbalance is directly associated with decreased QOL outcome scores [9–11], and postoperative improvement in sagittal plane alignment has been shown to significantly improve patient outcomes [10, 12]. However, no studies specifically focusing on the improvement of QOL after corrective spinal surgery in patients with osteoporosis and spinal kyphosis have been reported. In addition, we have been unable to determine whether the postoperative improvement of QOL is comparable with common osteoporosis patients without prevalent vertebral fractures, because no studies have reported the comparison of surgical results with non-operated control patients with osteoporosis. The purposes of this study were thus to evaluate changes in spinal alignment and QOL after corrective spinal instrumentation for patients with postmenopausal osteoporosis and thoracolumbar or lumbar kyphosis and to compare these results with non-operated patients with postmenopausal osteoporosis without prevalent vertebral fractures.
Materials and methods
Patients
Subjects comprised 39 consecutive patients with postmenopausal osteoporosis ≥50 years old who underwent corrective spinal surgery for symptomatic thoracolumbar or lumbar kyphosis (surgery group), and 82 consecutive age-matched patients with postmenopausal osteoporosis without prevalent vertebral fractures who had visited our outpatient clinics for the treatment of osteoporosis as non-operated controls (control group). The recruitment period was the same for patients in both groups, from January 2011 to December 2013. In the surgery group, 7 patients (18 %) showed vertebral fractures (4 patients had one fracture, and 3 patients had 2 fractures). Osteoporosis was diagnosed according to the criteria proposed by the Japanese Society for Bone and Mineral Research, as described in the Japanese 2011 guidelines for the prevention and treatment of osteoporosis [13]. Briefly, osteoporosis was diagnosed in patients with (1) any fragility fractures or (2) bone mineral density (BMD) level less than 70 % of the young adult mean or radiographic osteopenia of the spine. All patients had been prescribed oral bisphosphonates (35 mg/week of alendronate or 17.5 mg/week of risedronate) for the treatment of osteoporosis.
Lateral spine radiographs to evaluate global spinal sagittal alignment and questionnaires for QOL were obtained from each patient. Patients undergoing surgery were examined before surgery and after 6 months postoperatively, and control patients without surgery were examined at the time of enrollment. Patients undergoing surgery were followed up prospectively, and none dropped out during follow-up.
Exclusion criteria were as follows: (1) history of metabolic bone disease other than primary osteoporosis or history of malignancy; (2) history of spinal surgery before inclusion; (3) spinal scoliosis; (4) chronic glucocorticoid use; or (5) documented fresh fractures (in vertebrae and extremities) within the last 6 months. An informed consent was obtained from all patients at the time of enrollment.
Corrective spinal surgery
The indications for corrective spinal surgery were osteoporosis with rigid thoracolumbar or lumbar kyphosis and impaired QOL caused mainly by intolerable back and/or low back pain due to spinal imbalance that was not adequately controlled by comprehensive conservative treatment (i.e., pharmacotherapy, physiotherapy, braces, and trigger point block). However, because of the high invasiveness of the surgery, in principle, we applied corrective spinal surgery for healthy osteoporotic individuals without serious comorbidities. The majority of operated patients in this study were agriculturists who had a history of hard manual labor before retirement.
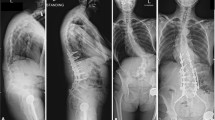
All operated patients underwent posterior-approach corrective fusion using a posterior lumbar interbody fusion (PLIF) technique for multiple levels (Fig. 1). The upper end of the fusion ranged from T4 to L2, and the lower end was L5 or S1 based on the level of kyphosis and the magnitude of spinal curvature in the individual. For all 39 operated patients, the mean number of fused levels was 6.6 (range, 3–13). The multilevel PLIF technique provides sufficient spinal correction [14]. Because PLIF can be applied even if the patient has mild vertebral deformity, most cases in this study underwent spinal correction using this technique alone. However, in some patients with severely collapsed vertebrae, the vertebrae were partially resected and replaced with large, rectangular, parallelepiped cages (REC cages) and autograft bone. This technique is a modification of the PLIF technique and was termed “posterior-approach vertebral replacement with REC cages” (PAVREC) [15]. PAVREC was applied as a part of spinal correction combined with multilevel PLIF.
Preoperative (a) and postoperative (b) standing lateral radiographs of a 73-year-old woman with prevalent L3 osteoporotic vertebral fracture and lumbar kyphosis who underwent multilevel posterior lumbar interbody fusion (PLIF) combined with posterior instrumentation. Spinal alignment was improved after surgery
Because the present study did not aim to discuss surgical invasiveness and complications, parameters regarding surgical invasiveness and complications were not included. Operative invasiveness (i.e., surgical time and blood loss) and perioperative complications of multilevel PLIF have been described elsewhere [16]. Although these surgeries seemed highly invasive, we did not encounter any critical complications [16].
Radiologic measurements
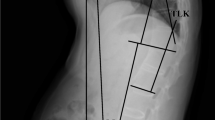
On standing lateral total spine x-ray, the following spinopelvic parameters for global spinal sagittal alignment were measured: thoracic kyphosis angle (TKA), angle between the upper endplate of T4 and the lower endplate of T12; lumbar lordosis angle (LLA), angle between the upper endplate of L1 and the upper endplate of S1; sagittal vertical axis (SVA); pelvic tilt (PT); and pelvic incidence (PI).
TKA and LLA were measured using the Cobb angle method. SVA is defined as the horizontal offset from the postero-superior corner of S1 to the vertebral midbody of C7 [12]. Increased SVA means the trunk is inclined anteriorly (stooped trunk). PT is defined as the angle between the vertical and the line through the midpoint of the sacral plate to the femoral head axis [12]. It has commonly been recognized as a compensatory mechanism that when the trunk is inclined anteriorly (e.g., increased kyphosis), a subject will try his/her best to maintain an economic posture and keep the spine balanced (i.e., bring the spine over the pelvis) [12]. One way to maintain this spinopelvic alignment is to retrovert the pelvis (increase of PT) [12]. PI is defined as the angle between the perpendicular to the upper sacral endplate at its midpoint and the line connecting this point to the femoral head axis [12]. PI is a morphological parameter of primary importance commonly used to define spinopelvic morphotypes [12].
In all patients, BMD of the proximal femur was measured with dual-energy x-ray absorptiometry (QDR 4500A; Hologic, Waltham, MA, USA) at the time of enrollment.
QOL evaluation
QOL was evaluated with the Japanese Osteoporosis QOL Questionnaire (JOQOL) [17, 18], the Medical Outcomes Study Short Form 36 (SF-36) [19, 20], and the Roland-Morris Disability Questionnaire (RDQ) [21, 22]. JOQOL was developed based on the Osteoporosis Assessment Questionnaire (OPAQ) [23] and Qualeffo-41 [24], with modification according to the Japanese lifestyle. JOQOL contains 38 items in six domains: pain (back/low back pain) (5 items, 20 points); ADL (16 items, 64 points); leisure and social activities (5 items, 20 points); general health perception (3 items, 12 points); posture and figure (4 items, 16 points); and fear of falling and mental factors (5 items, 20 points). Scores for each item range from 0 to 4, with a maximum possible score of 152. In JOQOL and SF-36, a higher score indicates a higher level of QOL. Conversely, a higher RDQ score indicates a lower QOL.
Statistical analyses
All data are expressed as mean ± standard deviation (SD). All statistical analyses were performed using StatView statistical software (SAS Institute, Cary, NC, USA). Differences between pre- and postoperative values were evaluated using repeated-measures one-way analysis of variance and Fisher’s protected least-significant difference as a post-hoc test. Differences between operated and non-operated groups were evaluated with the unpaired t test. Values of p < 0.05 were considered statistically significant.
Results
Baseline characteristics
Baseline characteristics of patients are presented in Table 1. No significant difference was seen between operated and non-operated groups at baseline in terms of age and height. However, weight, body mass index (BMI), and BMD were significantly higher in the operated group than in the non-operated group.
Spinal sagittal alignment
Preoperative TKA and LLA were significantly lower in the operated group than in the non-operated controls without prevalent vertebral fractures (Table 2). In the operated group, postoperative TKA was significantly higher than preoperative TKA, and postoperative TKA was also significantly higher than in the non-operated control group. LLA was also significantly increased after surgery but remained significantly lower than in non-operated controls.
Preoperative SVA and PT were significantly higher in the operated group than in non-operated controls. SVA and PT were significantly decreased (improved) after surgery but were still significantly higher than in non-operated controls. PI showed no significant differences between groups with and without surgery or between pre- and postoperatively.
QOL
All JOQOL domain scores and total score before surgery were significantly less than in non-operated controls (Table 3). Postoperatively, pain, general health perception, posture and figure, fear of falling and mental factors, and total JOQOL score were significantly improved but did not reach the levels seen in non-operated controls, with the exception of pain and general health perception. Pain domain score improved after surgery to a comparable level with non-operated controls, and general health perception was significantly improved after surgery compared to non-operated controls. However, no significant differences were observed between before and after surgery in terms of ADL or leisure and social activities.
In SF-36, all subscale scores and summary scores before surgery were significantly lower than in non-operated controls (Table 4). Subscale scores other than role physical (RP) and role emotional (RE) were significantly improved after surgery. Among these, bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), and mental health (MH) after surgery were comparable with and showed no significant differences from non-operated controls, but physical functioning (PF) did not reach the level of non-operated controls. Mental component summary (MCS) score improved significantly after surgery and was comparable with the score for non-operated control patients. Physical component summary (PCS) score did not improve significantly after surgery.
Preoperative RDQ score was significantly higher than in non-operated controls (Fig. 2). Postoperatively, RDQ score decreased significantly but remained significantly higher than in non-operated controls.
Discussion
The most frequent form of spinal deformity in patients with osteoporosis is spinal kyphosis. However, elderly patients sometimes show spinal scoliosis combined with kyphosis (kyphoscoliosis). The presence of apparent spinal scoliosis must also represent an important issue for QOL in the elderly. Lumbar scoliosis in the elderly sometimes causes lumbar foraminal stenosis resulting in nerve root compression, often requiring surgical decompression and instrumented fusion. However, because this study was focused on the impact of sagittal malalignment and realignment on QOL in patients with postmenopausal osteoporosis, spinal scoliosis (typically showing unilateral lumbar nerve root pain) was considered an exclusion criterion in this investigation.
In our study, although patients in the different groups were age-matched, BMI and BMD were both significantly higher in the surgery group than in the control group. This difference might be attributable to differences in occupation before retirement. The majority of patients in the surgery group were agriculturists who had been engaged in hard manual labor, while many of the patients in the control group had been housewives or non-agriculturists. Hard manual labor might be related to higher BMI and protective effects in terms of loss of BMD but is also considered to be associated with the development of lumbar spine lesions.
Back pain is a major source of morbidity among patients with osteoporosis and kyphosis. The literature suggests a prevalence of clinically relevant chronic back pain among patients with osteoporosis within the range of 28–91.4 % [25–28], with differences attributable to a lack of concordance in terms of patient background, including age stratification, pain definition, and methodology. However, the main cause of chronic back pain in patients with osteoporosis seemed highly related to increased spinal kyphosis. Increased spinal kyphosis is likely to induce abnormal stress on the supporting structures of the spinal column and may cause chronic back pain that usually develops while standing, walking, or doing other normal daily activities [29].
Conservative management is the first-line treatment for symptomatic spinal kyphosis, but corrective spinal surgery can be considered if the kyphosis is rigid and comprehensive conservative treatment proves ineffective. Fixed sagittal malalignment often requires complex reconstructive procedures that include osteotomies to adequately correct and restore global sagittal balance [30]. However, the incidence of complications after deformity surgery is relatively high [31–33]. Operative management of spinal deformity in osteoporotic elderly individuals is challenging, as perioperative complications may be associated with the overall medical condition with advancing age, and postoperative instrumentation failure may occur due to bone fragility. Indications for such surgery for osteoporosis in elderly individuals should thus be considered with great care.
The present results indicate that corrective spinal surgery for patients with osteoporosis and spinal kyphosis can significantly improve spinal alignment and QOL after surgery. Preoperative spinal alignment in the study subjects clearly showed that osteoporotic patients requiring corrective spinal surgery achieved significant decreases in lumbar lordosis (increased lumbar kyphosis) compared to non-operated controls. Increased lumbar kyphosis is known to represent an important causative factor for stooped trunk (increased SVA) and to exert a more significant negative impact on back or low back pain and QOL than increased thoracic kyphosis [6, 34].
PI showed no significant difference between operated and non-operated groups in this study. Because PI is an inherent parameter of spinopelvic alignment [12], original global spinal alignment, including spinopelvic alignment, is likely to be comparable between operated and non-operated patients at younger ages. Lower preoperative TKA compared to non-operated controls in this study seemed to represent a compensatory mechanism for decreased LLA to maintain sagittal balance.
In this study, however, postoperatively improved LLA, SVA, and PT did not reach the levels of non-operated controls, still showing under-correction after surgery. The present study used the multilevel PLIF technique for spinal column correction and fused the lower end at L5 or S1. Our indication for multilevel PLIF was rigid or ankylosing spinal deformity. If we had applied this technique for cases of milder kyphosis with greater flexibility, we probably could have accomplished complete correction comparable to normal spinal alignment. However, such cases are typically treated conservatively, and surgery is usually unnecessary. In addition, even for rigid cases, fusion including the ilium and/or other techniques including vertebral column resection, pedicle subtraction osteotomy [35], or a combination of these techniques may allow for more significant correction. However, the optimal degree of correction and tolerable level of invasiveness in elderly patients with osteoporosis remain unclear.
QOL as evaluated with JOQOL, SF-36, and RDQ were significantly improved after surgery, but total JOQOL score, PCS score of SF-36, and RDQ score did not reach the level of non-operated controls without prevalent vertebral fractures. Considering the results of domain scores in JOQOL and subscale and MCS scores in SF-36, although corrective spinal surgery was not particularly effective in improving ADL or RP, significant efficacy in reducing back pain and improving general and mental health was seen. In patients with osteoporosis, spinal mobility (particularly of the lumbar spine) is generally a very important factor for QOL as well as to maintain lumbar lordosis [5, 6]. Corrective fusion surgery restores lumbar lordosis but sacrifices spinal mobility, and this immobility may affect the results for ADL and RP. Conversely, significantly reduced back pain and improved posture after surgery are likely to positively impact the mental health of patients.
Although this study offered the first comparison of QOL after corrective spinal surgery for thoracolumbar or lumbar kyphosis in patients with osteoporosis with non-operated controls, various limitations need to be addressed. Since we wanted to determine the direct operative effects on QOL, postoperative results were evaluated only 6 months after surgery, as possible late complications related to surgery might influence QOL results. Postoperative effectiveness in terms of QOL may vary in the long-term after surgery, because postoperative complications regarding spinal instrumentation (i.e., proximal junctional kyphosis) are known to occur in osteoporotic patients and increase over time [36, 37] and may impact long-term results. However, long-term results for QOL are also important for patient care. Future studies thus need to include a longer follow-up after corrective spinal surgery for osteoporotic patients.
Conclusions
In conclusion, this study evaluated changes in global spinal alignment and QOL after corrective spinal surgery for patients with postmenopausal osteoporosis and spinal kyphosis and compared the results with corresponding non-operated patients without vertebral fractures. The results indicated that corrective spinal surgery using a multilevel PLIF technique significantly improved global spinal alignment and QOL (especially in terms of pain reduction and general/mental health) at 6 months after surgery, but neither radiographic parameters nor QOL scores (especially in physical activities) for surgical treatment reached the levels of non-operated controls.
References
Sinaki M, Itoi E, Rogers JW, Bergstralh EJ, Wahner HW (1996) Correlation of back extensor strength with thoracic kyphosis and lumbar lordosis in estrogen-deficient women. Am J Phys Med Rehabil 75:370–374
Mika A, Unnithan VB, Mika P (2005) Differences in thoracic kyphosis and in back muscle strength in women with bone loss due to osteoporosis. Spine (Phila Pa 1976) 30:241–246
Ryan SD, Fried LP (1997) The impact of kyphosis on daily functioning. J Am Geriatr Soc 45:1479–1486
Martin AR, Sornay-Rendu E, Chandler JM, Duboeuf F, Girman CJ, Delmas PD (2002) The impact of osteoporosis on quality-of-life: the OFELY cohort. Bone 31:32–36
Miyakoshi N, Itoi E, Kobayashi M, Kodama H (2003) Impact of postural deformities and spinal mobility on quality of life in postmenopausal osteoporosis. Osteoporos Int 14:1007–1012
Miyakoshi N, Hongo M, Maekawa S, Ishikawa Y, Shimada Y, Itoi E (2007) Back extensor strength and lumbar spinal mobility are predictors of quality of life in patients with postmenopausal osteoporosis. Osteoporos Int 18:1397–1403
Roux C, Fechtenbaum J, Kolta S, Said-Nahal R, Briot K, Benhamou CL (2010) Prospective assessment of thoracic kyphosis in postmenopausal women with osteoporosis. J Bone Miner Res 25:362–368. doi:10.1359/jbmr.090727
Hongo M, Miyakoshi N, Shimada Y, Sinaki M (2012) Association of spinal curve deformity and back extensor strength in elderly women with osteoporosis in Japan and the United States. Osteoporos Int 23:1029–1034. doi:10.1007/s00198-011-1624-z
Schwab FJ, Smith VA, Biserni M, Gamez L, Farcy JP, Pagala M (2002) Adult scoliosis: a quantitative radiographic and clinical analysis. Spine (Phila Pa 1976) 27:387–392
Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F (2005) The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 30:2024–2029
Lafage V, Schwab F, Patel A, Hawkinson N, Farcy JP (2009) Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976) 34:E599–E606. doi:10.1097/BRS.0b013e3181aad219
Schwab F, Patel A, Ungar B, Farcy JP, Lafage V (2010) Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976) 35:2224–2231. doi:10.1097/BRS.0b013e3181ee6bd4
Orimo H, Nakamura T, Hosoi T, Iki M, Uenishi K, Endo N, Ohta H, Shiraki M, Sugimoto T, Suzuki T, Soen S, Nishizawa Y, Hagino H, Fukunaga M, Fujiwara S (2012) Japanese 2011 guidelines for prevention and treatment of osteoporosis—executive summary. Arch Osteoporos 7:3–20
Miyakoshi N, Abe E, Kobayashi T, Abe T, Shimada Y (2012) Spinal corrective fusion using multilevel PLIF technique for lumbar spinal deformities: comparison of the surgical outcomes between the elderly and the non-elderly patients. J East Jpn Orthop Traumatology 24:62–65 (in Japanese)
Suzuki T, Abe E, Miyakoshi N, Murai H, Kobayashi T, Abe T, Kikuchi K, Shimada Y (2013) Posterior-approach vertebral replacement with rectangular parallelepiped cages (PAVREC) for the treatment of osteoporotic vertebral collapse with neurological deficits. J Spinal Disord Tech 26:E170–E176. doi:10.1097/BSD.0b013e318286fc18
Miyakoshi N, Abe E, Kobayashi T, Suzuki T, Abe T, Hongo M, Kasukawa Y, Murai H, Shimada Y (2011) Perioperative complications of instrumented corrective surgery for spinal deformity in the healthy elderly. J Spine Res 2:337–340
Takahashi H, Iwaya C, Iba K, Gorai I, Suzuki T, Hayashi Y, Fujinawa T, Yamazaki K, Endo N (2001) The Japanese osteoporosis QOL questionnaire (JOQOL): 2000 edition. J Jpn Soc Bone Miner Res 18:85–101 (in Japanese)
Kumamoto K, Nakamura T, Suzuki T, Gorai I, Fujinawa O, Ohta H, Shiraki M, Yoh K, Fujiwara S, Endo N, Matsumoto T (2010) Validation of the Japanese osteoporosis quality of life questionnaire. J Bone Miner Metab 28:1–7. doi:10.1007/s00774-009-0125-z
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30:473–483
Patel AA, Donegan D, Albert T (2007) The 36-item short form. J Am Acad Orthop Surg 15:126–134
Roland M, Morris R (1983) A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine (Phila Pa 1976) 8:141–144
Roland M, Morris R (1983) A study of the natural history of low-back pain. Part II: development of guidelines for trials of treatment in primary care. Spine (Phila Pa 1976) 8:145–150
Randell AG, Bhalerao N, Nguyen TV, Sambrook PN, Eisman JA, Silverman SL (1998) Quality of life in osteoporosis: reliability, consistency, and validity of the osteoporosis assessment questionnaire. J Rheumatol 25:1171–1179
Lips P, Cooper C, Agnusdei D, Caulin F, Egger P, Johnell O, Kanis JA, Liberman U, Minne H, Reeve J, Reginster JY, de Vernejoul MC, Wiklund I (1997) Quality of life as outcome in the treatment of osteoporosis: the development of a questionnaire for quality of life by the European foundation for osteoporosis. Osteoporos Int 7:36–38
Cockerill W, Ismail AA, Cooper C, Matthis C, Raspe H, Silman AJ, O’Neill TW (2000) Does location of vertebral deformity within the spine influence back pain and disability? European Vertebral Osteoporosis Study (EVOS) Group. Ann Rheum Dis 59:368–371
Jacobs JM, Hammerman-Rozenberg R, Cohen A, Stessman J (2006) Chronic back pain among the elderly: prevalence, associations, and predictors. Spine (Phila Pa 1976) 31:E203–E207
Kuroda T, Shiraki M, Tanaka S, Shiraki Y, Narusawa K, Nakamura T (2009) The relationship between back pain and future vertebral fracture in postmenopausal women. Spine (Phila Pa 1976) 34:1984–1989. doi:10.1097/BRS.0b013e3181b0c97a
Miyakoshi N, Hongo M, Shimada Y (2012) Prevalence of back pain in postmenopausal osteoporosis and associations with multiple spinal factors. In: Dionyssiotis Y (ed) Osteoporosis. InTech, Rijeka, pp 103–114
Satoh K, Kasama F, Itoi E, Tanuma S, Wakamatsu E (1988) Clinical features of spinal osteoporosis: spinal deformity and pertinent back pain. Contemp Orthop 16:23–30
Savage JW, Patel AA (2014) Fixed sagittal plane imbalance. Glob Spine J 4:287–296. doi:10.1055/s-0034-1394126
Baron EM, Albert TJ (2006) Medical complications of surgical treatment of adult spinal deformity and how to avoid them. Spine (Phila Pa 1976) 31(19 Suppl):S106–S118
DeWald CJ, Stanley T (2006) Instrumentation-related complications of multilevel fusions for adult spinal deformity patients over age 65: surgical considerations and treatment options in patients with poor bone quality. Spine (Phila Pa 1976) 31(19 Suppl):S144–S151
Pekmezci M, Berven SH, Hu SS, Deviren V (2009) The factors that play a role in the decision-making process of adult deformity patients. Spine (Phila Pa 1976) 34:813–817. doi:10.1097/BRS.0b013e3181851ba6
Miyakoshi N, Kasukawa Y, Ishikawa Y, Nozaka K, Shimada Y (2010) Spinal alignment and mobility in subjects with chronic low back pain with walking disturbance: a community-dwelling study. Tohoku J Exp Med 221:53–59
Joseph SA Jr, Moreno AP, Brandoff J, Casden AC, Kuflik P, Neuwirth MG (2009) Sagittal plane deformity in the adult patient. J Am Acad Orthop Surg 17:378–388
Cho SK, Shin JI, Kim YJ (2014) Proximal junctional kyphosis following adult spinal deformity surgery. Eur Spine J 23:2726–2736. doi:10.1007/s00586-014-3531-4
Lau D, Clark AJ, Scheer JK, Daubs MD, Coe JD, Paonessa KJ, LaGrone MO, Kasten MD, Amaral RA, Trobisch PD, Lee JH, Fabris-Monterumici D, Anand N, Cree AK, Hart RA, Hey LA, Ames CP (2014) Proximal junctional kyphosis and failure after spinal deformity surgery: a systematic review of the literature as a background to classification development. Spine (Phila Pa 1976) 39:2093–2102. doi:10.1097/BRS.0000000000000627
Conflicts of interest
None.
Ethical approval
All procedures in studies involving human participants were performed in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miyakoshi, N., Hongo, M., Kobayashi, T. et al. Improvement of spinal alignment and quality of life after corrective surgery for spinal kyphosis in patients with osteoporosis: a comparative study with non-operated patients. Osteoporos Int 26, 2657–2664 (2015). https://doi.org/10.1007/s00198-015-3163-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3163-5