Abstract
Summary
The relationship between change in body weight and risk of fractures is inconsistent in epidemiologic studies. In this cohort of middle-aged to elderly Chinese in Singapore, compared to stable weight, weight loss ≥10 % over an average of 6 years is associated with nearly 40 % increase in risk of hip fracture.
Introduction
Findings on the relationship between change in body weight and risk of hip fracture are inconsistent. In this study, we examined this association among middle-aged and elderly Chinese in Singapore.
Methods
We used prospective data from the Singapore Chinese Health Study, a population-based cohort of 63,257 Chinese men and women aged 45–74 years at recruitment in 1993–1998. Body weight and height were self-reported at recruitment and reassessed during follow-up interview in 1999–2004. Percent in weight change was computed based on the weight difference over an average of 6 years, and categorized as loss ≥10 %, loss 5 to <10 %, loss or gain <5 % (stable weight), gain 5 to <10 %, and gain ≥10 %. Multivariable Cox proportional hazards regression model was applied with adjustment for risk factors for hip fracture and body mass index (BMI) reported at follow-up interview.
Results
About 12 % experienced weight loss ≥10 %, and another 12 % had weight gain ≥10 %. After a mean follow-up of 9.0 years, we identified 775 incident hip fractures among 42,149 eligible participants. Compared to stable weight, weight loss ≥10 % was associated with 39 % increased risk (hazard ratio 1.39; 95 % confidence interval 1.14, 1.69). Such elevated risk with weight loss ≥10 % was observed in both genders and age groups at follow-up (≤65 and >65 years) and in those with baseline BMI ≥20 kg/m2.There was no significant association with weight gain.
Conclusions
Our findings provide evidence that substantial weight loss is an important risk factor for osteoporotic hip fractures among the middle-aged to elderly Chinese.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Weight loss due to reduced lean mass during aging is common among elderly [1–3]. Previous studies conducted in Western populations suggested that weight loss was significantly associated with bone loss in women [4, 5] and increased fracture risk among middle-aged to elderly men and women [6–13]. However, results on weight gain were inconclusive. While most of the studies did not show statistically significant association between weight gain and bone health outcomes, one study among Norwegian men and women reported that weight gain over 5.6 kg significantly increased hip fracture risk in women [10], while another study showed weight loss ≥10 % reduced risk of hip fracture of borderline statistical significance among Caucasian men in the USA [9].
Leanness is an established independent risk factor of hip fracture in a previous meta-analysis [14]. We have also reported that low body mass index (BMI) increased the risk of hip fracture among men in our cohort of middle-aged and elderly Chinese in Singapore [15]. Asian populations have lower BMI and possibly different weight change patterns during aging as compared to their Western counterparts. In the present study, we used prospective data from the same cohort to examine the association between body weight changes over an average of 6 years with risk of hip fracture.
Methods
Study population
The present study was conducted in the Singapore Chinese Health Study, a population-based cohort prospective study established to investigate dietary and lifestyle factors in relation to risk of chronic diseases. We recruited 63,257 aged 45–74 years men (n = 27,959) and women (n = 35,298) between April 1993 and December 1998. The study participants were restricted to two dialect groups of Hokkiens and Cantonese who originated from Fujian and Guangdong provinces in southern China. During the enrollment period, all of our study participants were residents of government housing estates, where 86 % of the Singapore population was residing at the time of recruitment [16]. Participants were recontacted for a telephone interview between July 1999 and October 2004 [17]. After excluding those who had died, were noncontactable, or who were no longer able to participate in the follow-up interview due to disability, a total of 52,322 participants (82.7 % of the original cohort) were reinterviewed. The Institutional Review Board at the National University of Singapore approved this study. All study participants gave written informed consent.
Exposure assessment
Baseline assessment was conducted between 1993 and 1998 through a face-to-face interview with a trained interviewer using a structured questionnaire, which included demographics, medical history, cigarette smoking, alcohol consumption, physical activity, detailed menstrual and reproductive history (women only), and habitual diet recorded by a validated semi-quantitative food frequency questionnaire. History of cancer prior to the follow-up interview was self-reported and also assessed via linkage with the national cancer registry. At the follow-up interview from 1999 to 2004, smoking and drinking behavior, medical and health history, and menstrual and reproductive history (women only) were reassessed. Current body weight and height were self-reported at both of the baseline and the follow-up assessments with an average of 5.7 years apart. BMI is calculated as weight in kilograms divided by height in meters squared (kg/m2). We excluded participants with missing body weight and height at both baseline and follow-up interviews (n = 9994). We further excluded 41 participants who developed hip fracture prior to baseline and 138 participants who developed hip fracture prior to the follow-up interview, thus leaving 42,149 participants in this study for the final analysis. Compared to the participants included in this study, the 9994 participants excluded from this study were older, had a higher proportion of women and were less educated. They were also more likely to be current smokers, and had higher prevalence of diabetes mellitus, stroke, and cancer.
Weight change
Percent weight change was computed as weight difference divided by baseline body weight [(weight at follow-up − weight at baseline) / weight at baseline] × 100 %]. Weight change was then categorized as follows: loss ≥10 %, loss 5 to <10 %, stable weight (loss or gain <5 %), gain 5 to <10 %, and gain ≥10 %. These categories of weight change were suggested to be clinically relevant and meaningful comparison among participants with wide range of weight variation in previous studies [7, 18].
Case ascertainment
Incident cases of hip fracture were identified through December 31, 2010, via the record linkage with the national hospital discharge database, which captures inpatient discharge information from all public and private hospitals in Singapore. All hip fracture cases were verified by surgical or medical records. Only 47 participants from this cohort (0.07 %) were known to be lost to follow-up due to migration out of Singapore or for other reasons. The survival status of all cohort participants was ascertained via the record linkage with the population-based Singapore Registry of Births and Deaths.
Statistical analysis
Differences in characteristics among weight change groups were tested for statistical significance using chi-squared tests for categorical variables and ANOVA for continuous variables. For each study subject, person-years were counted from the date of the follow-up interview to the date of diagnosis of hip fracture, death, migration or December 31, 2010, whichever occurred first. Multivariable Cox proportional hazards regression model was applied to assess the association between weight change and risk of hip fracture for the whole cohort and for subgroup analyses. The strength of the association between weight change and hip fracture risk was estimated by hazard ratios (HRs) and their corresponding 95 % confidence intervals (CI), using participants with stable weight (loss or gain <5 %) as the reference group. We did not identify any violation of the proportional hazard assumption or multicollinearity among the covariates that were included in the models.
We examined the association between weight change and risk of hip fracture using three models. Model 1 was adjusted for the following covariates: age at follow-up interview (years), time interval between baseline and follow-up assessments (years), dialect group (Hokkien, Cantonese), level of education (no formal education, primary school, secondary school or higher), smoking status at follow-up interview (never smokers, ex-smokers, current smokers), current use of hormone replacement at follow-up interview (women only; yes, no), and gender (for the whole cohort). The time interval between baseline and follow-up defined the period when weight change occurred, since weight and height were assessed at these two occasions. The mean (standard deviation (SD)) time interval was 5.7 years (1.4), and the interquartile range was 4.5 to 8.8 years. This variable was included as a covariate in the regression model because the duration of the time interval could influence the degree of weight change and thus confound the relationship between weight change and the risk of hip fracture. Model 2 was adjusted for the abovementioned covariates plus self-reported physician-diagnosed history of diabetes mellitus (yes, no), stroke (yes, no), coronary heart disease (yes, no), cancer (yes, no), and other fractures (yes, no) prior to baseline or the follow-up interview. Model 3 was further adjusted for BMI (<20, 20–23.9, 24–27.9, ≥28 kg/m2) reported at the follow-up interview. We also conducted stratified analysis by gender (men and women), age group at follow-up (≤65 and >65 years) and baseline BMI category (BMI <20, 20 to <25, and ≥25 kg/m2). Finally, we tested interactions between weight change categories and gender, age groups, or baseline BMI categories using the likelihood ratio test. The test was done by including five product terms in the model between these two sets of variables.
All statistical analysis was conducted using SAS version 9.2 (SAS Institute, Inc., Cary, NC). A P value <0.05 is considered to be statistically significant. All reported P values are two-sided.
Results
We identified 775 incident cases of hip fracture among 42,149 eligible cohort participants during a mean survival time of 9.0 years (SD 2.1). The time interval between the two assessments of body weight at baseline and follow-up interviews was 5.7 years (SD 1.4). Among the incident cases of hip fracture, the mean age at fracture was 75.3 years (SD 7.3). Women accounted for 69.2 % of all hip fracture cases. The incidence rate of hip fractures in women standardized to the age structure of the whole cohort was 256 per 100,000 person-years, which was nearly two times that in men (143 per 100,000 person-years).
The characteristics of participants according to weight change are shown in Table 1. About half of the cohort participants had weight change less than 5 %, and the mean of the absolute weight change was −0.08 kg (SD 6.36). For the other half of participants, the proportion of weight loss and weight gain was distributed similarly, with 11.6 % of the cohort reporting extreme weight loss and 12.2 % reporting extreme weight gain ≥10 %. The mean (SD) for extreme weight change was −10.7 kg (7.4) for weight loss ≥10 % and 9.8 kg (5.1) for weight gain ≥10 %, respectively. Compared to those with stable weight, participants with weight loss ≥10 % were older at follow-up interview, more likely to be men, had higher weight and BMI at baseline; they also had lower education level, were more likely to be current smokers, and had a higher prevalence of diabetes, stroke, coronary heart disease, and cancer. Among the women, they were more likely to be postmenopausal and less likely to use hormone replacement therapy. By contrast, relative to those with stable weight, participants who had weight gain ≥10 % were more likely to be women, slightly older at follow-up interview, and had lower weight and BMI at baseline; they were also less educated and had a higher proportion of current smokers. Among the women, they were also more likely to be postmenopausal and less likely to use hormone replacement therapy (Table 1).
The association between body weight change and risk of hip fracture is shown in Table 2. Compared to stable weight (loss or gain <5 %), individuals with weight loss ≥10 % experienced a statistically significant 56 % increase in risk of hip fracture after adjustment for demographic and lifestyle factors (model 1). Further adjustment for comorbidities including history of diabetes, stroke, coronary heart disease, cancer, and other bone fractures (model 2) and BMI reported at the follow-up assessment (model 3) did not materially alter the results. In the final model, compared to stable weight, weight loss ≥10 % was associated with 39 % increased risk of hip fracture (HR 1.39; 95 % CI 1.14, 1.69). Conversely, no association was found between weight gain and hip fracture risk. The results were materially the same in a simpler model that included only age, gender, and BMI at follow-up as covariates (Supplemental Table S1). In this simpler model, the HR (95 % CI) associated with weight loss ≥10 % was 1.55 (1.28, 1.88) and that with weight gain ≥10 % was 1.00 (0.78, 1.26). The association between weight change and risk of hip fractures did not differ by gender (all P for interaction >0.30).
We further analyzed the data after excluding participants with history of diabetes, stroke, coronary heart disease, and cancer reported at the follow-up interview, because they would be more likely to experience greater weight loss than those without such diseases. Among the 31,875 participants without the abovementioned comorbidities, there were 468 incident cases of hip fracture. Compared to stable weight, weight loss ≥10 % was significantly associated with a statistically significant 55 % increase in risk of hip fracture (HR 1.55; 95 % CI 1.20, 2.01), whereas no apparent association was found for those with weight gain ≥10 % (HR 1.14; 95 % CI 0.85, 1.53).
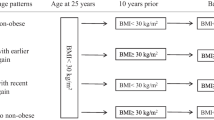
Table 3 shows the association between weight change and risk of hip fracture stratified by baseline BMI in three categories (<20, 20 to <25, and ≥25 kg/m2) and age group at follow-up (≤65 and >65 years). We used BMI <20 kg/m2 as the cutoff for leanness, because it was a significant risk factor for hip fracture in this cohort [15] as well as in a meta-analysis that examined BMI and fracture risk [14]. We used the current recommendation by the World Health Organization of BMI ≥25 kg/m2 as the cutoff for the overweight category [19]. In the stratification by baseline BMI, there was a marginal significant difference in the risk estimates associated with weight loss ≥10 % between the BMI <20 kg/m2 and BMI 20 to <25 kg/m2 categories (P = 0.09), and also between the BMI <20 kg/m2 and BMI ≥25 kg/m2 categories (P = 0.06).Weight loss ≥10 % was not significantly associated with hip fracture risk in participants with baseline BMI <20 kg/m2. Conversely, among those with baseline BMI ≥20 kg/m2, there was a 48 % increase in hip fracture risk (HR 1.48; 95 % CI 1.18, 1.84). The highest risk was observed among those who were overweight (BMI ≥25 kg/m2) at baseline (HR 1.55; 95 % CI 1.02, 2.37). The risk estimates for hip fracture associated with weight gain ≥10 % between the three baseline BMI categories were not statistically different (all Ps for interaction >0.18). Compared to stable weight, weight loss ≥10 % was associated with increased risk of hip fracture similarly in both age groups. There was no apparent difference in the relationship between weight change and risk of hip fracture by age group (all Ps for interaction >0.59).
Furthermore, in the stratum of participants with baseline BMI <20 kg/m2, we excluded those who died before the cutoff date of December 31, 2010 (n = 1036), leaving 6513 surviving participants with 148 hip fracture incident cases and 6365 non-cases. Although those who remained alive before the cutoff date were likely to be healthier than those who had died, the risk estimates for the 6513 surviving participants remained materially the same. Neither weight loss ≥10 % (HR 1.01; 95 % CI 0.56, 1.82) nor weight gain ≥10 % (HR 0.81; 95 % CI 0.52, 1.25) was associated with risk of hip fracture.
Discussion
In this study, we observed a significant increase in risk of hip fracture among those who sustained a weight loss of 10 % and above. Conversely, no significant association was found between weight gain and risk of hip fracture. Results were similar in both men and women.
Weight loss has been documented to be related to bone loss [4, 5] and increased fracture risk [6–9, 12] in previous studies among Western populations. Findings from the present study are generally consistent with the results reported earlier, where extreme weight loss was associated with increased fracture risk in both men and women [6–9, 12]. Similar to the findings in a community-dwelling prospective cohort study among US Caucasian men [9] and women [7], whose weight change was measured between age of 50 years and older, weight loss >10 % compared to stable weight significantly increased risk of hip fracture by nearly threefold in men (HR 2.79; 95 % CI 1.62, 4.79) [9] and in women (HR 2.9; 95 % CI 2.0, 4.1) [7]. Another longitudinal study among Norwegian men and women also showed that weight loss of more than 3 kg was associated with a significant twofold increase in risk of hip fracture as compared to those who had body weight gain of 1.3–5.5 kg [10]. Furthermore, in this study, the significantly elevated risk with weight loss ≥10 % persisted in men and women combined, in elderly aged >65 years, in those whose baseline BMI ≥20 kg/m2, and among participants without medical history of diabetes, stroke, cancer, and coronary heart disease. Thus, our data demonstrated the independent role of weight change in relation to risk of hip fracture. On the other hand, weight gain ≥10 % was not statistically significantly associated with hip fracture risk in this cohort, which is similar to the previous findings among Caucasian men [20] and women [12]. In line with these studies [6, 7, 9, 12], we did not find differences regarding weight change and hip fracture risk by gender or age group (≤65 and >65 years). Compared to the weight change pattern in previous studies, the absolute change in weight among the participants in the extreme weight change category (≥10 %) in our study was about 4–5 kg less than that in the same category in two Caucasian studies [7, 9]. However, it should be noted that age, lifestyle factors, health conditions, and the time interval of weight change vary from one study to another.
This study is the first to examine weight change in relation to risk of hip fracture in lean participants with BMI <20 kg/m2, which is an independent risk factor for hip fracture [14, 15]. We found that weight loss ≥10 % did not further affect the risk of hip fracture among these lean individuals whose baseline BMI was already <20 kg/m2. Furthermore, after excluding who died between the follow-up assessment and December 31, 2010, in this subgroup, our results did not appear to bias toward to the healthier survivors. This suggested, at least in part, that in lean individuals who were already at risk of hip fracture due to their low BMI, extreme weight loss did not confer additional risk for hip fracture. Nevertheless, this could be an observation by chance in our study due to the small numbers of participants and hip fracture cases in this group. In the previous studies among Caucasian populations, the lowest cutoff for baseline BMI was <23 kg/m2 among women in the USA [7] and was ≤22.6 kg/m2 among men in Norway [20]. Hence, we are not able to compare our results for those with baseline BMI <20 kg/m2 with other populations. In the study among white women in the USA, weight loss ≥10 % was consistently associated with elevated risk of hip fracture in all strata of baseline BMI at 50 years of age. However, weight gain ≥10 % appeared to be associated with increased risk among those with baseline BMI <23 kg/m2, yet it was associated with reduced risk among those with baseline BMI ≥23 kg/m2, although the relationship between weight gain ≥10 % and hip fracture risk did not reach statistical significance [7]. Conversely, in the study among Norwegian white men, compared to stable weight, weight loss ≤5 % decreased bone mineral density (BMD) and weight gain ≥5 % increased BMD across all baseline BMI strata [20]. Further studies are needed to validate our finding of the null association between extreme weight loss and fracture risk in lean individuals with baseline BMI <20 kg/m2.
The potential mechanisms between weight loss and osteoporotic fractures have been proposed previously. Weight loss among elderly was suggested to decrease more lean mass, especially muscle mass [3, 21], resulting in weakened muscle strength and increased frailty [22]. This is particularly the case among elderly men [23], because men have more muscle mass than women [24]. In line with this, studies have shown that lean mass was an independent contributor to hip bone mineral density [25, 26], especially in men [26, 27]. Furthermore, decreased lean mass may reduce testosterone level [28, 29], which has been shown to be positively associated with muscle strength and bone mineral density [28]. In contrast, loss of fat mass following weight loss may play a more predominant role in bone mass among postmenopausal women [26, 27], possibly due to more fat tissue in women as compared to men [3]. Thus, loss of fat mass could contribute to a further decline of estrogen in postmenopausal women [30, 31], and reduced estrogen could have a negative impact on osteoblasts [32] and osteoclasts [33] through the expression of the pro-inflammatory cytokines, such as interleukin (IL)-1, IL-6, and TNF-α [34]. Other mechanisms underlying weight loss and hip fracture include decreased mechanical loading and weight bearing, and loss of fat around the hip, which in turn increase the risk of fractures during falls [35, 36]. Taken together, weight loss among elderly men and women may thus impair bone health and increase risk of fracture.
On the other hand, the benefit of weight gain in reducing risk of hip fracture is less certain. Although weight gain increased weight bearing, mechanical loading and padding around the hip [35, 36], all of which may protect against falls and fractures, there is generally little lean mass conservation with weight gain among elderly men and women [23, 37]. In the present study, although weight gain ≥10 % in those who were not overweight at baseline (BMI <25 kg/m2) was associated with lower risk of hip fracture, it did not reach statistical significance. In contrast, weight gain ≥10 % in those who were overweight (BMI ≥25 kg/m2) at baseline was associated with a non-significant increase in risk. We speculate that extreme weight gain among overweight middle-aged to elderly may be associated with increased risk of other chronic diseases, such as cardiovascular disease and type 2 diabetes [38, 39], which are risk factors for hip fracture [40, 41]. In addition, body fat may redistribute with increased visceral fat in elderly [3], which in turn could impair insulin sensitivity and increase the expression of other pro-inflammatory cytokines [39]. Furthermore, serum vitamin D status was inversely related to adiposity [42], thus extreme weight gain may in turn decrease the circulation of vitamin D [43] and affect dietary calcium absorption [44]. All of these are plausible explanations why weight gain may not protect against hip fracture among overweight participants in our study population.
The strength of this study is the large number of incident cases of hip fracture identified from a population-based prospective cohort with a long follow-up time. Another strength is the presumed lack of recall bias in body weight, height, and other potential confounding variables since they were reported by participants prior to hip fracture. Singapore is a small city-state with a system for easy access to specialized medical care. Since practically all hip fracture cases would seek medical attention immediately and be hospitalized, as well as a negligible proportion (0.07 %) of original cohort participants who migrated out of Singapore, our case ascertainment through the linkage with the comprehensive, nationwide hospital database can be considered complete. A limitation of our study is the lack of information on diet and physical activity at the follow-up interview, which did not allow us to further examine whether changes in these lifestyle factors may confound the association between weight change and risk of hip fracture. The use of self-reported body weight and height could be prone to non-differential misclassification, and thus, it would lead to underestimation of the association between weight change and risk of hip fracture. A systematic review of 64 studies [45] and a study among middle-aged and elderly Australian adults [46] suggested trends of underestimation for self-reported weight and overestimation for self-reported height. Furthermore, the systematic review also showed that the difference between the self-reported and objectively measured BMI was relatively small for those with BMI less than 30 kg/m2 [45]. In line with this, there was a very high correlation between self-reported and measured height, weight, and BMI among the middle-aged and elderly Australians (r ≥ 0.95), and those with higher measured BMI tend to have greater underestimation [46]. Nevertheless, self-report of body weight has been shown to be valid across many populations and specifically in Asians [47], and 96 % of our study population had BMI <30 kg/m2. We therefore speculated that the underestimation of self-reported weight and height was relatively small in our study population. Another limitation is that change of body composition, such as that of lean and fat mass, was not investigated in the current study. Therefore we were unable to evaluate whether the effect of weight change could be mediated by the variation of body composition in the development of osteoporosis. Finally, our study excluded those who could not report weight and/or height at either interview, and they were different in mean age and in the distribution of gender, education level, and prevalence of comorbidities from those included in this study. Nevertheless, all of our statistical models had included these factors as covariates to minimize possible confounding bias by these factors. Hence, even though differences between the participants included in the study and those who were excluded may affect the generalizability of the results, we feel that the conclusions of the present study should be valid.
In conclusion, data from the present study demonstrate that weight loss of 10 % or more was associated with significant increased risk of hip fracture among middle-aged to elderly Chinese men and women in Singapore. Our findings highlight the importance of identifying risk of osteoporotic hip fracture in middle-aged to elderly with substantial weight loss in addition to low BMI.
References
Chapman IM (2011) Weight loss in older persons. Med Clin North Am 95(3):579–593, xi
McMinn J, Steel C, Bowman A (2011) Investigation and management of unintentional weight loss in older adults. BMJ 342:d1732
Seidell JC, Visscher TL (2000) Body weight and weight change and their health implications for the elderly. Eur J Clin Nutr 54(Suppl 3):S33–S39
Ensrud KE, Ewing SK, Stone KL, Cauley JA, Bowman PJ, Cummings SR (2003) Intentional and unintentional weight loss increase bone loss and hip fracture risk in older women. J Am Geriatr Soc 51(12):1740–1747
Nguyen TV, Sambrook PN, Eisman JA (1998) Bone loss, physical activity, and weight change in elderly women: the Dubbo Osteoporosis Epidemiology Study. J Bone Miner Res 13(9):1458–1467
Ensrud KE, Cauley J, Lipschutz R, Cummings SR (1997) Weight change and fractures in older women. Study of Osteoporotic Fractures Research Group. Arch Intern Med 157(8):857–863
Langlois JA, Harris T, Looker AC, Madans J (1996) Weight change between age 50 years and old age is associated with risk of hip fracture in white women aged 67 years and older. Arch Intern Med 156(9):989–994
Langlois JA, Mussolino ME, Visser M, Looker AC, Harris T, Madans J (2001) Weight loss from maximum body weight among middle-aged and older white women and the risk of hip fracture: the NHANES I epidemiologic follow-up study. Osteoporos Int 12(9):763–768
Langlois JA, Visser M, Davidovic LS, Maggi S, Li G, Harris TB (1998) Hip fracture risk in older white men is associated with change in body weight from age 50 years to old age. Arch Intern Med 158(9):990–996
Meyer HE, Tverdal A, Falch JA (1995) Changes in body weight and incidence of hip fracture among middle aged Norwegians. BMJ 311(6997):91–92
Meyer HE, Tverdal A, Selmer R (1998) Weight variability, weight change and the incidence of hip fracture: a prospective study of 39,000 middle-aged Norwegians. Osteoporos Int 8(4):373–378
Omsland TK, Schei B, Gronskag AB, Langhammer A, Forsen L, Gjesdal CG, Meyer HE (2009) Weight loss and distal forearm fractures in postmenopausal women: the Nord-Trondelag health study, Norway. Osteoporos Int 20(12):2009–2016
Wilsgaard T, Jacobsen BK, Ahmed LA, Joakimsen RM, Stormer J, Jorgensen L (2011) BMI change is associated with fracture incidence, but only in non-smokers. The Tromso Study. Osteoporos Int 22(4):1237–1245
De Laet C, Kanis JA, Oden A, Johanson H, Johnell O, Delmas P, Eisman JA, Kroger H, Fujiwara S, Garnero P, McCloskey EV, Mellstrom D, Melton LJ 3rd, Meunier PJ, Pols HA, Reeve J, Silman A, Tenenhouse A (2005) Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int 16(11):1330–1338
Dai Z, Wang R, Ang LW, Low YL, Yuan JM, Koh WP (2014) Protective effects of dietary carotenoids on risk of hip fracture in men: the Singapore Chinese Health Study. J Bone Miner Res 29(2):408–417
Hankin JH, Stram DO, Arakawa K, Park S, Low SH, Lee HP, Yu MC (2001) Singapore Chinese Health Study: development, validation, and calibration of the quantitative food frequency questionnaire. Nutr Cancer 39(2):187–195
Lim SH, Tai BC, Yuan JM, Yu MC, Koh WP (2013) Smoking cessation and mortality among middle-aged and elderly Chinese in Singapore: the Singapore Chinese Health Study. Tob Control 22(4):235–240
Christian JG, Tsai AG, Bessesen DH (2010) Interpreting weight losses from lifestyle modification trials: using categorical data. Int J Obes 34(1):207–209
World Health Organization (1997) Preventing and managing the global epidemic. Report on a WHO Consultation on Obesity. WHO, Geneva
Meyer HE, Sogaard AJ, Falch JA, Jorgensen L, Emaus N (2008) Weight change over three decades and the risk of osteoporosis in men: the Norwegian Epidemiological Osteoporosis Studies (NOREPOS). Am J Epidemiol 168(4):454–460
Lindle RS, Metter EJ, Lynch NA, Fleg JL, Fozard JL, Tobin J, Roy TA, Hurley BF (1997) Age and gender comparisons of muscle strength in 654 women and men aged 20-93 yr. J Appl Physiol 83(5):1581–1587
Pocock N, Eisman J, Gwinn T, Sambrook P, Kelly P, Freund J, Yeates M (1989) Muscle strength, physical fitness, and weight but not age predict femoral neck bone mass. J Bone Miner Res 4(3):441–448
Newman AB, Lee JS, Visser M, Goodpaster BH, Kritchevsky SB, Tylavsky FA, Nevitt M, Harris TB (2005) Weight change and the conservation of lean mass in old age: the Health, Aging and Body Composition Study. Am J Clin Nutr 82(4):872–878
Kyle UG, Genton L, Hans D, Karsegard VL, Michel JP, Slosman DO, Pichard C (2001) Total body mass, fat mass, fat-free mass, and skeletal muscle in older people: cross-sectional differences in 60-year-old persons. J Am Geriatr Soc 49(12):1633–1640
Segal NA, Torner JC, Yang M, Curtis JR, Felson DT, Nevitt MC (2008) Muscle mass is more strongly related to hip bone mineral density than is quadriceps strength or lower activity level in adults over age 50 year. J Clin Densitom 11(4):503–510
Taaffe DR, Cauley JA, Danielson M, Nevitt MC, Lang TF, Bauer DC, Harris TB (2001) Race and sex effects on the association between muscle strength, soft tissue, and bone mineral density in healthy elders: the Health, Aging, and Body Composition Study. J Bone Miner Res 16(7):1343–1352
Baumgartner RN, Stauber PM, Koehler KM, Romero L, Garry PJ (1996) Associations of fat and muscle masses with bone mineral in elderly men and women. Am J Clin Nutr 63(3):365–372
van den Beld AW, de Jong FH, Grobbee DE, Pols HA, Lamberts SW (2000) Measures of bioavailable serum testosterone and estradiol and their relationships with muscle strength, bone density, and body composition in elderly men. J Clin Endocrinol Metab 85(9):3276–3282
Gates MA, Mekary RA, Chiu GR, Ding EL, Wittert GA, Araujo AB (2013) Sex steroid hormone levels and body composition in men. J Clin Endocrinol Metab 98(6):2442–2450
Hui SL, Perkins AJ, Zhou L, Longcope C, Econs MJ, Peacock M, McClintock C, Johnston CC Jr (2002) Bone loss at the femoral neck in premenopausal white women: effects of weight change and sex-hormone levels. J Clin Endocrinol Metab 87(4):1539–1543
O'Dea JP, Wieland RG, Hallberg MC, Llerena LA, Zorn EM, Genuth SM (1979) Effect of dietery weight loss on sex steroid binding sex steroids, and gonadotropins in obese postmenopausal women. J Lab Clin Med 93(6):1004–1008
Eriksen EF, Colvard DS, Berg NJ, Graham ML, Mann KG, Spelsberg TC, Riggs BL (1988) Evidence of estrogen receptors in normal human osteoblast-like cells. Science (New York, NY) 241(4861):84–86
Chen FP, Wang KC, Huang JD (2009) Effect of estrogen on the activity and growth of human osteoclasts in vitro. Taiwan J Obstet Gynecol 48(4):350–355
Zallone A (2006) Direct and indirect estrogen actions on osteoblasts and osteoclasts. Ann N Y Acad Sci 1068:173–179
Dawson-Hughes B, Shipp C, Sadowski L, Dallal G (1987) Bone density of the radius, spine, and hip in relation to percent of ideal body weight in postmenopausal women. Calcif Tissue Int 40(6):310–314
Wei TS, Hu CH, Wang SH, Hwang KL (2001) Fall characteristics, functional mobility and bone mineral density as risk factors of hip fracture in the community-dwelling ambulatory elderly. Osteoporos Int 12(12):1050–1055
Lee JS, Visser M, Tylavsky FA, Kritchevsky SB, Schwartz AV, Sahyoun N, Harris TB, Newman AB (2010) Weight loss and regain and effects on body composition: the Health, Aging, and Body Composition Study. J Gerontol A Biol Sci Med Sci 65(1):78–83
Lebovitz HE (2006) Insulin resistance—a common link between type 2 diabetes and cardiovascular disease. Diabetes Obes Metab 8(3):237–249
Lebovitz HE (2001) Insulin resistance: definition and consequences. Exp Clin Endocrinol Diabetes 109(Suppl 2):S135–S148
Sennerby U, Melhus H, Gedeborg R, Byberg L, Garmo H, Ahlbom A, Pedersen NL, Michaelsson K (2009) Cardiovascular diseases and risk of hip fracture. JAMA 302(15):1666–1673
Koh WP, Wang R, Ang LW, Heng D, Yuan JM, Yu MC (2010) Diabetes and risk of hip fracture in the Singapore Chinese Health Study. Diabetes Care 33(8):1766–1770
Cheng S, Massaro JM, Fox CS, Larson MG, Keyes MJ, McCabe EL, Robins SJ, O’Donnell CJ, Hoffmann U, Jacques PF, Booth SL, Vasan RS, Wolf M, Wang TJ (2010) Adiposity, cardiometabolic risk, and vitamin D status: the Framingham Heart Study. Diabetes 59(1):242–248
Mason C, Xiao L, Imayama I, Duggan CR, Bain C, Foster-Schubert KE, Kong A, Campbell KL, Wang CY, Neuhouser ML, Li L, Jeffery RW, Robien K, Alfano CM, Blackburn GL, McTiernan A (2011) Effects of weight loss on serum vitamin D in postmenopausal women. Am J Clin Nutr 94(1):95–103
Cifuentes M, Riedt CS, Brolin RE, Field MP, Sherrell RM, Shapses SA (2004) Weight loss and calcium intake influence calcium absorption in overweight postmenopausal women. Am J Clin Nutr 80(1):123–130
Connor Gorber S, Tremblay M, Moher D, Gorber B (2007) A comparison of direct vs. self-report measures for assessing height, weight and body mass index: a systematic review. Obes Rev 8(4):307–326
Ng SP, Korda R, Clements M, Latz I, Bauman A, Bambrick H, Liu B, Rogers K, Herbert N, Banks E (2011) Validity of self-reported height and weight and derived body mass index in middle-aged and elderly individuals in Australia. Aust N Z J Public Health 35(6):557–563
Hu FB (2008) Obesity epidemiology, vol 1. Oxford University Press, New York
Acknowledgments
We thank Siew-Hong Low of the National University of Singapore for supervising the fieldwork and Renwei Wang for the maintenance of the database in the Singapore Chinese Health Study. We also thank the Ministry of Health in Singapore for assistance with the identification of hip fracture cases and mortality via database linkages. Finally, we acknowledge the founding Principal Investigator of the Singapore Chinese Health Study, Mimi C. Yu.
Funding
This study was supported by the National Medical Research Council, Singapore (NMRC/EDG/0011/2007) and National Institutes of Health, USA (RO1 CA144034 and UM1 CA182876).
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM
(DOCX 16.7 kb)
Rights and permissions
About this article
Cite this article
Dai, Z., Ang, LW., Yuan, JM. et al. Association between change in body weight after midlife and risk of hip fracture—the Singapore Chinese Health Study. Osteoporos Int 26, 1939–1947 (2015). https://doi.org/10.1007/s00198-015-3099-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3099-9