Abstract
Summary
Sickness absence is a risk marker for future health outcomes, but no previous studies have examined its association with osteoporotic fractures in old age. The results of this prospective population-based cohort study based on Swedish registers suggest that sickness absence is associated with higher risk of hip fracture.
Introduction
Number of sick leave days is a risk marker for future health outcomes, but few studies have examined its association with major public health concerns in old age, such as osteoporotic fractures. The aim of this prospective, nationwide, population-based cohort study based on Swedish registers was to investigate the association between number of sick leave days and future risk of hip fracture.
Methods
Participants included were all 983,244 individuals who were living in Sweden on 31 December 1995, aged 50 to 64 years, employed, and with no previous hip fracture. Those with sick leave days in 1995 were compared to those with no sickness absence. Incidence of hip fracture was followed from 1996 to 2010.
Results
According to Cox regression models adjusted for sociodemographic factors and morbidity, being on sick leave more than 3 months, irrespective of cause, was associated with a 2.0-fold (hazard ratio (HR) 1.96, 95 % confidence interval (CI) 1.74–2.20) and 1.4-fold (HR 1.40, 95 % CI 1.27–1.56) increased risk of hip fracture in men and women, respectively. Analyses repeated among those with previous non-hip fractures replicated the significant associations.
Conclusion
This nationwide cohort study suggests that sickness absence in working-age women and men is a risk marker of hip fracture at old ages.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Long-term sick leave is recognized as a useful measure of global health in studies of working populations [1, 2] as well as of social consequences of morbidity [3]. Several epidemiological studies have also shown that extended sick leave is a risk marker for a range of future health outcomes, such as sustained suboptimal health [4], disability pension [5–7], and all-cause and cause-specific mortality [8, 2, 9–11]. This suggests that sick leave is not only a marker of concurrent health status but can also be seen as a predictor of sustained suboptimal health over time. Moreover, long-term sick leave may entail unintended or unexpected negative “side effects” on physical or mental health, such as reduced psychological well-being, inactivity, isolation, and impaired sleep [12, 13]. Such adverse consequences of long-term sick leave may have long-lasting impact on health later in life.
In working populations, number of sick leave days has been shown to provide important prognostic information for conditions of major public health relevance [14]. However, most studies have used premature death as the outcome while specific types of morbidities have rarely been studied and we have found no studies on hip fractures as the outcome. It is of interest to examine whether sick leave could be an early prognostic marker of osteoporotic fractures, a major public health concern in the older population [15]. Of all osteoporosis-related fractures, hip fracture is the most adverse, both in terms of mortality [16–19] and economic expenditure [20, 21]. Hip fracture has also a great negative impact on older people’s lives because of pain, reduced functioning, and impaired quality of life [22–24].
To address this limitation, the aim of the present study was to examine, for the first time, the association between length of sick leave in working age and incidence of hip fracture at old ages accounting for previous non-hip fractures, which are among the main risk factors for subsequent hip fracture [25–27]. Since both the rates of sick leave [28, 29] and the incidence of hip fractures [30] differ between women and men, and the mechanism might vary with gender, we conducted analyses separately for men and women.
Methods
Study design and population
A prospective population-based cohort study with a 15-year follow-up was conducted. Included were all 1,408,011 individuals who were 50 to 64 years of age and registered as living in Sweden on 31 December 1994 and were working during the year 1995.
Data for definition of the cohort and on potential confounders (age, sex, country of birth, marital status, educational level, sick leave and disability pension in 1995, and on emigration up through 2010) was obtained from Statistics Sweden. For all cohort members, annual data from two nationwide, population-based registers were linked by using the unique ten-digit number assigned to all Swedish residents from the inpatient register regarding hospitalization in 1990–2010 and date of deaths in 1995–2010 from the Cause of Death register, both kept by the National Board of Health and Welfare. The study was approved by the Regional Ethical Board of Stockholm, Sweden.
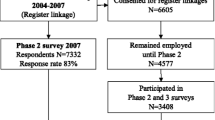
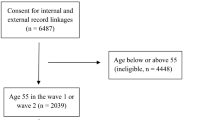
Figure 1 shows the flow of the participant selection. We excluded people not at risk for sickness absence in 1995, e.g., people on disability pension and people who in 1995 had an income below 10,000 SEK from work and/or benefits such as unemployment, sickness absence, student benefits, or parental leave, and people having had a previous hip fracture in the years 1964–1995. After these exclusions, the total cohort consisted of 983,246 individuals (514,901 men and 468,325 women).
Sick leave
In Sweden in 1995, people aged 16–65 with reduced work capacity due to disease or injury could be on sick leave with sickness benefits if having income from work or unemployment or other benefits exceeding 10,000 SEK. The sickness benefits covered up to 80 % of lost income. The first sick leave day was a qualifying day with no benefits. After the seventh sick leave day, a sickness certificate issued by a physician was required. The employer usually provided sick pay for the first 14 days of a sick leave spell. Thereafter, the Social Insurance Agency paid sickness benefits—in this study, information on the latter was used as exposure data. The number of days with sickness benefits from 1 January to 31 December 1995 was categorized as 0, 1–15, 16–75, 76–165, or 166–365.
Hip fracture
The follow-up information about hip fractures in 1996–2010 was drawn from the inpatient registry, using information on both primary and side diagnoses (ICD 10 codes S72.0-S72.2), that is excluding high-energy hip fractures according to the external cause codes (i.e., fractures following falls exceeding 1 m from one level to another or traffic accidents or casualties alike).
Covariates
Covariates, namely age, sex, educational level, marital status, and country of birth, were measured on 31 December 1995 and were categorized as indicated in Table 1. Information on inpatient care in 1990–1995 due to any disease (yes or no) was utilized to indicate morbidity before the exposure year 1996. Adjustment for inpatient care allows examining the independent association between number of sick leave days and hip fracture risk since sickness absence may convey additional knowledge that may not be completely captured by specific diseases, as it reflects, e.g., the work capacity in relation to the job-specific requirements and employees’ general health. Previous non-hip fractures in 1990–1995 were determined based on the inpatient care data.
Statistics
Study population characteristics at baseline for women and men according to the incident hip fracture status were calculated as mean values for continuous variables and as proportions for categorical variables. The Kaplan-Meier estimates of cumulative hazards were used to estimate the probability of hip fracture by number of sick leave days, taking the competing risk of death and emigration into account. Cox proportional hazards regression models were used to calculate hazard ratios (HR) and 95 % confidence intervals (CI) for incidence of hip fracture according to the number of sick leave days after assuring that the proportional hazard assumption was met. All contributed with person time until hip fracture, emigration, death, or end of follow-up, whichever came first. Analyses were stratified by gender, and models were adjusted in stages for age, education, marital status, birth country, and inpatient care in 1990–1995. In addition, subgroup analyses were conducted among those who received inpatient care in 1990–1995 due to non-hip fractures.
To address the possibility that the excess risk of hip fracture associated with sickness absence would be directly linked to the exposure (i.e., sickness absence), we repeated the main analysis, including only persons who had returned back to work after their sick leave and had income from work in 1996. The SAS 9.3 Statistical Package was used for all analyses (SAS Institute Inc., Cary, NC).
Results
Baseline characteristics of the cohort are shown in Table 1. During the 15-year register-based follow-up, 1.4 % (n = 7,148) men and 2.2 % (n = 10,457) women attained a hip fracture. At the baseline, the women and men with later incident hip fracture were older, were more often native Swedish, had lower levels of education, were less often married, had more sick leave days in 1995, and more often had had previous inpatient care than those without incident hip fracture (p for all <0.0001).
In Fig. 2, the Kaplan-Meier estimates show that there was a clear association with number of sick leave days and cumulative hazard of future hip fracture among both women and men. Basically, the patterns were alike, but women showed slightly less variation between categories of sick leave days and cumulative hazard of hip fracture than men.
Table 2 shows the HR for a hip fracture by number of sick leave days. In men, the HR of hip fracture was higher already with 1–15 sick leave days (HR 1.32, 95 % 1.19–1.47) and more than twofold (HR 2.27, 95 % CI 2.03–2.55, and HR 2.27, 95 % CI 2.04–2.52) among those with 3 to 12 months of sickness absence compared to those with no sickness absence. In women, the estimates were lower than in men and no excess risk of hip fracture emerged among those less than 3 months on sick leave. Adjustment for previous inpatient care attenuated the estimates in men and women, but all associations remained significant.
By utilizing information about previous fractures, it was found that previous non-hip fractures were strongly associated with future incidence of hip fracture in men (HR 3.59, 95 % 2.27–3.95) and in women (HR 2.94, 95 % 2.71–3.18). To examine the association between sick leave lengths with HR of hip fracture in this high-risk group for hip fractures, we repeated the analysis among those with previous non-hip fractures (Table 3). In men, a high number of sickness absence days (166–365) was associated with higher hip fracture risk after adjusting for previous inpatient care (HR 2.26, 95 % CI 1.68–3.03) and the risk estimate was slightly higher than in the entire male study population. In women with previous non-hip fractures, being sickness absent for 76–165 days or longer increased the risk 1.5-fold (HR 1.52, 95 % 1.16–1.99) compared to those with no sickness absence. The risk estimates were slightly higher than those in the entire cohort.
To address the possibility that the association between length of sick leave and incident hip fracture was directly linked to the baseline sickness absence, we conducted sensitivity analysis by repeating the main analysis, including only persons who had returned to work after their sick leave in 1996 (excluding 27,870 men and 25,634 women). The results were replicated and are shown in an online supplement (eTable 1).
Discussion
In this nationwide cohort study of almost one million people, we observed, for the first time, that long-term sick leave is associated with higher risk of hip fracture among women and men even after accounting for multiple confounders, including sociodemographic factors, morbidity, and previous non-hip fractures. Being on sick leave for more than 3 months showed in women a 1.4-fold and in men a 2.0-fold increase in hazard ratios of hip fracture in a 15-year follow-up compared with those with no sick leave days the same year.
Despite the longitudinal design, observational studies such as ours can only prove an association between the length of sick leave and hip fracture. Multiple epidemiological studies have identified several risk factors for hip fractures [31–33], including (but not limited to) cardiovascular factors (high diastolic blood pressure, resting heart rate), systemic diseases (diabetes, rheumatoid arthritis, Parkinson’s disease) [34, 35], several drugs (e.g., psychotropic drugs and opioids) [36, 37], and poor lifestyle (smoking and excessive alcohol use) [34], that can impact on both bone fragility and liability to falls. Most of these factors, especially chronic diseases and poor lifestyle, are also linked to higher prevalence and longer duration of sickness absence. Thus, number of sick leave days could be considered as a risk marker which summarizes information from these specific and more obvious predictors of hip fracture. Number of sick leave days could even be screened easily via electronic systems because they capture a wide range of illnesses that employees experience, allowing early identification of those people at increased hip fracture risk.
Moreover, we believe that long-term sick leave may convey additional information that may not be completely captured by specific diseases. The overall rate of medically certified sickness absence spells per year appears to be a good global measure of health [2] as it reflects day-to-day functioning in occupational settings and predicts mortality at least as well as more established indicators of health. In addition, previous research has shown that long-term sick leave independently predicts increased risk of sustained suboptimal health [4] and poor self-rated health increases the risk of hip fracture [34, 33]. Thus, data on sickness absence may provide useful information to identify groups with increased health risk and a need for targeted interventions. Future studies are needed to examine closer the association between cause-specific sickness absence and hip fracture risk as well as the mechanisms linking sickness absence with future hip fractures.
In theory, several plausible mechanisms link sick leave to higher risk of hip fracture. First, there are multiple diseases and related medication including cardiovascular diseases and mental disorders that are shown to be associated with increased hip fracture risk [35]. Results of this study showed that adjustment of previous inpatient care attenuated, but did not completely eliminate, the statistically significant association between length of sick leave and hip fractures. Second, sickness absence is also shown to be a strong prognostic indicator for multiple future health outcomes [5–8, 2, 9–11] probably because absence records provide day-to-day data on functioning in occupational settings and thus capture the presence of comorbidity, illness severity, and risk factors affecting work performance [14]. Moreover, long-term sick leave may also cause unintended or unexpected negative “side effects” on physical or mental health, such as inactivity, impaired health behavior, social isolation, lowered psychological well-being, and financial and work-related disturbances [12, 13], which may partly predispose to health and behavioral trajectories increasing fracture risk in the long run.
Since history of a previous fracture is one of the main risk factors for subsequent hip fracture [25–27], we conducted subgroup analysis among those with previous non-hip fractures to explore the association of length of sick leave and future hip fractures when major bone-related risk factor is accounted for. Our results suggest even among those with previous non-hip fracture, being sickness absent is associated with higher incidence of hip fracture compared with those with no sickness absence.
This study has major strengths. First, that the whole Swedish population of working age could be included, entailing very high statistical power, excluding selection bias, and allowing subgroup analyses. Second, the availability of register (i.e., not self-reported) data with no or very few missing data regarding exposures, outcomes, and confounders and the possibility to adjust for several potential confounders, including inpatient care because of different diseases [38, 39]. Third, that there was no loss to follow-up; and finally, the long followup and detection of hip fractures are almost complete because of the high-quality and nationwide coverage of the Swedish population-based registers used. We assume that any diagnosed hip fractures were treated at least 1 day at hospital. Nevertheless, we might have missed some hip fractures, for example among those patients in caring homes. However, as the participants in the cohort were relatively young, we do not assume we missed many—nevertheless, our results might imply a slight underestimation.
The limitations of the study also need to be acknowledged. First, sick leave spells shorter than 15 days were not included in the analyses because in Sweden the employer usually provides sick pay for the first 14 days of a sick leave spell. Second, it would have been an advantage if also information on the sick leave diagnoses could have been included; however, the Swedish Social Insurance Agency did not register those until 10 years later. Third, despite the long follow-up, covering transition from midle age into old age, the study population was relatively young and most of the subjects were only in their 70s by the end of the follow-up, which is still a relatively young age for hip fracture. Finally, data regarding adverse lifestyle factors, such as physical inactivity and smoking, which may be associated with exposure and outcome, were not available in the nationwide registers. However, such factors are associated with low SES and should partly be adjusted for by our adjustment for SES based on education.
In conclusion, the results of this prospective nationwide cohort study suggest that long-term sick leave is positively associated with incidence of hip fracture in working-age women and men after accounting for the effects of morbidity and previous fractures. Further studies are needed to explore the mechanisms underlying these associations.
References
Marmot M, Feeney A, Shipley M, North F, Syme SL (1995) Sickness absence as a measure of health status and functioning: from the UK Whitehall II study. J Epidemiol Community Health 49(2):124–130
Kivimäki M, Head J, Ferrie JE, Shipley MJ, Vahtera J, Marmot MG (2003) Sickness absence as a global measure of health: evidence from mortality in the Whitehall II prospective cohort study. BMJ 327((7411):364. doi:10.1136/bmj.327.7411.364
Alexanderson K, Norlund A (2004) Swedish Council on Technology Assessment in Health Care (SBU). Chapter 1. Aim, background, key concepts, regulations, and current statistics. . Scand J Public Health 32 (Supplement 63):12–30
Vahtera J, Westerlund H, Ferrie JE, Head J, Melchior M, Singh-Manoux A, Zins M, Goldberg M, Alexanderson K, Kivimäki M (2010) All-cause and diagnosis-specific sickness absence as a predictor of sustained suboptimal health: a 14-year follow-up in the GAZEL cohort. J Epidemiol Community Health 64(4):311–317. doi:10.1136/jech.2008.083923
Kivimaki M, Forma P, Wikstrom J, Halmeenmaki T, Pentti J, Elovainio M, Vahtera J (2004) Sickness absence as a risk marker of future disability pension: the 10-town study. J Epidemiol Community Health 58(8):710––711. doi:10.1136/jech.2003.015842
Lund T, Kivimaki M, Labriola M, Villadsen E, Christensen KB (2008) Using administrative sickness absence data as a marker of future disability pension: the prospective DREAM study of Danish private sector employees. Occup Environ Med 65(1):28–31
Labriola M, Lund T (2007) Self-reported sickness absence as a risk marker of future disability pension. Prospective findings from the DWECS/DREAM study 1990–2004. Int J Med Sci 4(3):153–158
Vahtera J, Pentti J, Kivimaki M (2004) Sickness absence as a predictor of mortality among male and female employees. J Epidemiol Community Health 58(4):321–326
Ferrie JE, Vahtera J, Kivimaki M, Westerlund H, Melchior M, Alexanderson K, Head J, Chevalier A, Leclerc A, Zins M, Goldberg M, Singh-Manoux A (2009) Diagnosis-specific sickness absence and all-cause mortality in the GAZEL study. J Epidemiol Community Health 63((1):50–55. doi:10.1136/jech.2008.074369
Head J, Ferrie JE, Alexanderson K, Westerlund H, Vahtera J, Kivimaki M (2008) Diagnosis-specific sickness absence as a predictor of mortality: the Whitehall II prospective cohort study. BMJ 337:a1469
Jansson C, Mittendorfer-Rutz E, Alexanderson K (2012) Sickness absence because of musculoskeletal diagnoses and risk of all-cause and cause-specific mortality: a nationwide Swedish cohort study. Pain 153(5):998–1005. doi:10.1016/j.pain.2012.01.028
Vingård E, Alexanderson K, Norlund A (2004) Swedish Council on Technology Assessment in Health Care (SBU). Chapter 9. Consequences of being on sick leave. Scandinavian Journal of Public Health 32(Supplemet 63, Review):207–215
Floderus B, Goransson S, Alexanderson K, Aronsson G (2005) Self-estimated life situation in patients on long-term sick leave. J Rehabil Med 37((5):291–299. doi:10.1080/16501970510034422
Kivimaki M, Head J, Ferrie JE, Singh-Manoux A, Westerlund H, Vahtera J, Leclerc A, Melchior M, Chevalier A, Alexanderson K, Zins M, Goldberg M (2008) Sickness absence as a prognostic marker for common chronic conditions: analysis of mortality in the GAZEL study. Occup Environ Med 65((12):820–826. doi:10.1136/oem.2007.038398
Compston J (2004) Action plan for the prevention of osteoporotic fractures in the European Community. Osteoporos Int 15(4):259–262
Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA (1999) Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet 353(9156):878–882
Omsland TK, Emaus N, Tell GS, Magnus JH, Ahmed LA, Holvik K, Center J, Forsmo S, Gjesdal CG, Schei B, Vestergaard P, Eisman JA, Falch JA, Tverdal A, Sogaard AJ, Meyer HE (2014) Mortality following the first hip fracture in Norwegian women and men (1999–2008). A NOREPOS study, Bone
Todd CJ, Palmer C, Camilleri-Ferrante C, Freeman CJ, Laxton CE, Parker MJ, Payne BV, Rushton N (1995) Differences in mortality after fracture of hip. BMJ 311(7011):1025
Johnell O, Kanis JA, Oden A, Sernbo I, Redlund-Johnell I, Petterson C, De Laet C, Jonsson B (2004) Mortality after osteoporotic fractures. Osteoporos Int 15(1):38–42
Haentjens P, Autier P, Barette M, Boonen S (2001) The economic cost of hip fractures among elderly women. A one-year, prospective, observational cohort study with matched-pair analysis. Belgian Hip Fracture Study Group J Bone Joint Surg Am 83-A(4):493–500
Haentjens P, Lamraski G, Boonen S (2005) Costs and consequences of hip fracture occurrence in old age: an economic perspective. Disabil Rehabil 27(18–19):1129–1141
Magaziner J, Fredman L, Hawkes W, Hebel JR, Zimmerman S, Orwig DL, Wehren L (2003) Changes in functional status attributable to hip fracture: a comparison of hip fracture patients to community-dwelling aged. Am J Epidemiol 157(11):1023–1031
Randell AG, Nguyen TV, Bhalerao N, Silverman SL, Sambrook PN, Eisman JA (2000) Deterioration in quality of life following hip fracture: a prospective study. Osteoporos Int 11(5):460–466
Boonen S, Autier P, Barette M, Vanderschueren D, Lips P, Haentjens P (2004) Functional outcome and quality of life following hip fracture in elderly women: a prospective controlled study. Osteoporos Int 15(2):87–94
Ismail AA, Cockerill W, Cooper C, Finn JD, Abendroth K, Parisi G, Banzer D, Benevolenskaya LI, Bhalla AK, Armas JB, Cannata JB, Delmas PD, Dequeker J, Dilsen G, Eastell R, Ershova O, Falch JA, Felsch B, Havelka S, Hoszowski K, Jajic I, Kragl U, Johnell O, Lopez Vaz A, Lorenc R, Lyritis G, Marchand F, Masaryk P, Matthis C, Miazgowski T, Pols HA, Poor G, Rapado A, Raspe HH, Reid DM, Reisinger W, Janott J, Scheidt-Nave C, Stepan J, Todd C, Weber K, Woolf AD, Ambrecht G, Gowin W, Felsenberg D, Lunt M, Kanis JA, Reeve J, Silman AJ, O′Neill TW (2001) Prevalent vertebral deformity predicts incident hip though not distal forearm fracture: results from the European Prospective Osteoporosis Study. Osteoporos Int 12(2):85–90
Mallmin H, Ljunghall S, Persson I, Naessen T, Krusemo UB, Bergstrom R (1993) Fracture of the distal forearm as a forecaster of subsequent hip fracture: a population-based cohort study with 24 years of follow-up. Calcif Tissue Int 52(4):269–272
Haentjens P, Autier P, Collins J, Velkeniers B, Vanderschueren D, Boonen S (2003) Colles fracture, spine fracture, and subsequent risk of hip fracture in men and women. A meta-analysis. J Bone Joint Surg Am 85-A(10):1936–1943
Feeney A, North F, Head J, Canner R, Marmot M (1998) Socioeconomic and sex differentials in reason for sickness absence from the Whitehall II Study. Occup Environ Med 55(2):91–98
Bekker MH, Rutte CG, van Rijswijk K (2009) Sickness absence: a gender-focused review. Psychol Health Med 14(4):405–418. doi:10.1080/13548500903012830
Requena G, Abbing-Karahagopian V, Huerta C, De Bruin ML, Alvarez Y, Miret M, Hesse U, Gardarsdottir H, Souverein PC, Slattery J, Schneider C, Rottenkolber M, Schmiedl S, Gil M, De Groot MC, Bate A, Ruigómez A, García Rodríguez LA, Johansson S, de Vries F, Montero D, Schlienger R, Reynolds R, Klungel OH, de Abajo FJ (2014) Incidence rates and trends of hip/femur fractures in five European countries: comparison using E-Healthcare records databases. Calcif Tissue Int 94(6):580–589. doi:10.1007/s00223-014-9850-y
Allolio B (1999) Risk factors for hip fracture not related to bone mass and their therapeutic implications. Osteoporos Int 9 Suppl 2(2):S9–S16
Marks R (2010) Hip fracture epidemiological trends, outcomes, and risk factors, 1970–2009. Int J Gen CXXMed 3:1–17
Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, Cauley J, Black D, Vogt TM (1995) Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med 332(12):767–773
Holmberg AH, Johnell O, Nilsson PM, Nilsson JA, Berglund G, Akesson K (2005) Risk factors for hip fractures in a middle-aged population: a study of 33,000 men and women. Osteoporos Int 16(12):2185–2194
Gerber Y, Melton LJ, McNallan SM, Jiang R, Weston SA, Roger VL (2013) Cardiovascular and noncardiovascular disease associations with hip fractures. Am J Med 26((2):169 e–119-126
Li L, Setoguchi S, Cabral H, Jick S (2013) Opioid use for noncancer pain and risk of fracture in adults: a nested case-control study using the general practice research database. Am J Epidemiol 178(4):559–569
Huang AR, Mallet L, Rochefort CM, Eguale T, Buckeridge DL, Tamblyn R (2012) Medication-related falls in the elderly: causative factors and preventive strategies. Drugs Aging 29(5):359–376
Causes of Death 2009 (2011). National Board of Health and Welfare Sweden, Stockholm
Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim JL, Reuterwall C, Heurgren M, Olausson PO (2011) External review and validation of the Swedish national inpatient register. BMC Public Health 11:450. doi:10.1186/1471-2458-11-450
Acknowledgments
This work was financially supported by the EU’s Era-Age 2 program (Academy of Finland (264944) and the Swedish Research Council for Health, Working Life and Welfare (Forte, 2007-1762). Sari Stenholm was also supported by the Academy of Finland (273850). Mika Kivimäki was also supported by the UK Medical Research Council (K013351), the National Heart, Lung and Blood Institute (HL36310), the National Institute of Aging (AG034454), and a professorial fellowship from the Economic and Social Research Council). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 15 kb)
Rights and permissions
About this article
Cite this article
Stenholm, S., Vahtera, J., Kjeldgård, L. et al. Length of sick leave as a risk marker of hip fracture: a nationwide cohort study from Sweden. Osteoporos Int 26, 943–949 (2015). https://doi.org/10.1007/s00198-014-2985-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-014-2985-x