Abstract
Summary
Because kidney dysfunction reduces the ability to excrete dietary acid excess, we hypothesized that underlying kidney function may have confounded the mixed studies linking dietary acid load with the risk of osteoporosis and fractures in the community. In a relatively large survey of elderly men and women, we report that dietary acid load did neither associate with DEXA-estimated bone mineral density nor with fracture risk. Underlying kidney function did not modify these null findings. Our results do not support the dietary acid-base hypothesis of bone loss.
Introduction
Impaired renal function reduces the ability to excrete dietary acid excess. We here investigate the association between dietary acid load and bone mineral density (BMD), osteoporosis, and fracture risk by renal function status.
Methods
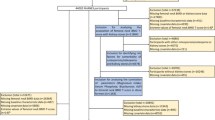
An observational study was conducted in 861 community-dwelling 70-year-old men and women (49 % men) with complete dietary data from the Prospective Investigation of the Vasculature in Uppsala Seniors (PIVUS). The exposure was dietary acid load as estimated from 7-day food records by the net endogenous acid production (NEAP) and potential renal acid load (PRAL) algorithms. Renal function assessed by cystatin C estimated glomerular filtration rate was reduced in 21 % of the individuals. Study outcomes were BMD and osteoporosis state (assessed by DEXA) and time to fracture (median follow-up of 9.2 years).
Results
In cross-section, dietary acid load had no significant associations with BMD or with the diagnosis of osteoporosis. During follow-up, 131 fractures were validated. Neither NEAP (adjusted hazard ratios (HR) (95 % confidence interval (CI)), 1.01 (0.85–1.21), per 1 SD increment) nor PRAL (adjusted HR (95 % CI), 1.07 (0.88–1.30), per 1 SD increment) associated with fracture risk. Further multivariate adjustment for kidney function or stratification by the presence of kidney disease did not modify these null associations.
Conclusions
The hypothesis that dietary acid load associates with reduced BMD or increased fracture risk was not supported by this study in community-dwelling elderly individuals. Renal function did not influence on this null finding.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis and its complications, in particular osteoporosis-related fractures, represent major public health problems among elderly [1, 2]. Apart from aging, osteoporosis is also affected by comorbidities, hormonal changes, lifestyle, and dietary factors. The acid-base theory postulates that bone acts as a primary buffer system for basic components in foods such as calcium, phosphate, potassium, and magnesium while acid ions in foods act as proton (H+) donors [3, 4], and that bone loss and osteoporosis may ensue due to release of alkaline salts from bone to maintain acid-base balance [5]. Acid-producing foods include meats, fish, hard cheeses, cereal grains, salted foods, and legumes, whereas alkaline, base-producing foods are fruits and vegetables [6, 7]. Thus, long-term exposure to an acidic environment may induce calcium loss [7], leading to the decline of bone mineral density (BMD) and subsequently to osteoporosis-related fractures.
Adherence to a Western diet, characterized by high consumption of animal protein, has been associated with chronic metabolic acidosis [8, 9], and diets rich in meat and low in vegetables lead to both increased dietary net acid load [10] and hip fracture risk in postmenopausal women [11]. In vivo, metabolic acidosis has been suggested to suppress the activity of the bone-forming osteoblasts [12]. Metabolic acidosis associates also with negative calcium balance, attributed to the mobilization of calcium carbonate from the skeleton [4, 13]. Correcting metabolic acidosis by administration of NaHCO3 may lead to modest improvement in the negative calcium balance in patients with severe renal insufficiency [14].
In nutritional epidemiology, the net endogenous acid production (NEAP) and the potential renal acid load (PRAL) calculated from dietary recalls are often used to estimate the dietary acid load [15]. Several large population studies have used NEAP and potential renal acid load (PRAL) to investigate the association of dietary acid load and BMD, but the results are mixed and inconsistent [15–19]. The same inconsistency is seen in the fewer studies addressing the association between dietary acid load and fracture risk [20, 21]. A potential limitation of previous studies is the lack of consideration of underlying kidney function, as the consequences of dietary acid load in the community may depend on the ability of the body to excrete acids and calcium into the urine [22]. This may be of particular relevance given that previous studies included eminently elderly individuals [15–21, 23]. Indeed, kidney function declines with age, and as many as 50–60 % of individuals above 65 years of age are considered to have moderate to advanced kidney disease in national screening programs [24]. In this study, we examined the association between dietary acid load, BMD, and fracture risk in a population-based cohort of elderly men and women, taking underlying kidney function into account as a potential confounder and/or modifying cofactor.
Subjects and methods
Subjects
This is an ancillary analysis from the population-based Swedish cohort Prospective Investigation of the Vasculature in Uppsala Seniors (PIVUS), involving 1061 women and men aged 70 years, whose recruitment and clinical assessment took place between 2001 and 2004 [25]. The primary aim of PIVUS was to investigate vascular risk factors among the elderly. For this specific analysis, 200 individuals were a priori excluded due to the lack of dietary data, leaving 861 eligible subjects (49 % males). The study was approved by the Ethics Committee of Uppsala University, and informed consent was obtained from all participants.
Dietary assessment
Dietary assessment was made with a 7-day food-frequency questionnaire which has been validated by pre-coded menu book from Swedish National Food Administration (NFA) [26]. The dietary intake of energy and nutrients was calculated using a database from the NFA. The macro- and micronutrients in this study were corrected for total energy intake by normalizing all intakes to a diet of 8.29 MJ (or 1982 kcal) by regression analysis of the residual method [27]. PRAL was calculated with the algorithm of Remer et al. [28]: PRAL (mEq/day) = 0.49 × protein intake (g/d) + 0.037 × phosphorus (mg/day) − 0.021 × potassium (mg/day) − 0.013 × calcium (mg/day) − 0.026 × magnesium (mg/day). Estimation of the NEAP was calculated according to the equation of Frassetto et al. [29]: NEAP (mEq/day) = (54.4 × protein intake (g/day) / potassium (mEq/day)) − 10.2.
Bone mineral density assessment
BMD of total body, lumbar spine (LS) (L1-L4), femoral neck (FN), and total hip were measured by DEXA (DPX, Lunar Prodigy, Lunar Corp., Madison, WI, USA). The BMD of the femoral neck and total hip were measured on both sides. Osteoporosis was clinically diagnosed using BMD measurements at multiple sites (lumbar spine, total hip, or femoral neck) and defined as a T-score ≤−2.5 standard deviation (SD) from the National Health and Nutrition Examination Survey (NHANES) III reference database in Caucasian women aged 20–29 years [30]. The precision error of DEXA measurements of BMD was between 0.8 and 1.5 % by a triple measurement performed in 15 subjects.
Identification of fractures during follow-up
As the main outcome, fractures occurring in study participants after enrollment through 31 December 2011 were identified by matching to the Patient Register of the Uppsala County. Complete linkage is enabled by use of the individual personal identification number provided to all Swedish citizens. Fractures considered were those from the neck down, as specified by the International Classification of Diseases (ICD) 10 codes S12, S22, S32, S42, S52, S62, S72, S82, and S92. The first registered fracture for each individual was used.
Other covariates
Body mass index was calculated as weight (kg) at baseline divided by the square of height (m2). Smoking status was recorded as current smoker or not. Education levels were grouped at least college level or below. Physical activity was categorized into low and high based on a calculation of both light and heavy physical activity. Venous blood samples were drawn in the morning after an overnight fast and then stored at −70 °C pending analysis. Serum cystatin C was measured by latex-enhanced reagent (N Latex Cystatin C, Dade Behring, Deerfield, IL, USA) with a Behring BN ProSpec analyzer (Dade Behring). The total analytical imprecision of the method was 4.8 % at 0.56 mg/L and 3.7 % at 2.85 mg/L. Parathyroid hormone (PTH) levels were analyzed using the Immulite 2000 intact PTH assay (Diagnostic Products Corporation, Los Angeles, CA, USA). All analysis of other biomarkers was performed at the Swedish Board for Accreditation and Conformity Assessment (SWEDAC) accredited laboratory of Department of Chemistry, University Hospital, Uppsala. Estimated glomerular filtration rate (eGFR) was calculated by serum cystatin C concentrations (mg/L) by the following formula: eGFR = 77.24 × Cystatin C −1.2623, which has been validated to be closely correlated with iohexol clearance [31]. As a sensitivity/confirmatory analysis, we also estimated GFR with the recent international, assay-independent estimated, cystatin C-based GFR (CAPA-eGFR) equation: NCC-eGFR = 130 × Cystatin C −1.069 × age−0.117 − 7 [32].
Statistical analysis
Variables are reported as means ± SD, median (interquartile range) or percentages, respectively, unless otherwise specified. Participants were divided into four groups according to quartiles of NEAP distribution. The linearity of variables among groups was tested with Jonckheere-Terpstra (F) test. Person-years at risk were calculated from the date of entry at the cohort to the date of the first fracture event, date of death, or the end of the follow-up period (31 December 2011), whichever came first. Multiple linear regression analysis was used to determine whether NEAP and PRAL were independent predictors of BMD. Cox proportional hazards models were used to estimate the hazard ratios (HRs) with 95 % confidence intervals (CIs) for fractures. Both per SD increment as well as per quartiles of PRAL and NEAP were tested as exposures. In multivariate analyses, the following serial adjustments were performed: (1) minimal adjustment for sex and energy intake; (2) further adjustment for BMI and confounding lifestyle factors (alcohol intake, smoking, physical activity) and education level; (3) further adjustment for eGFR. The association between dietary acid load and osteoporosis was investigated with multivariable logistic regression model using quartiles of diet acid load and the same multivariable adjustments as above. Cox regression models also included threshold models (highest quartile versus the rest) and stratification by the presence/absence of CKD (defined as eGFR <60 ml/min/1.73 m2). Finally, a power calculation for our fracture risk analysis was performed to assess the robustness of our null findings. P < 0.05 was considered as statistically significant. All statistical analyses were performed by using Stata version 12.0 (Stata Corporation, College Station, TX, USA).
Results
Baseline characteristics
The median NEAP and PRAL of the study population were 40.1 mEq/day (interquartile range (IQR) 35.6 to 45.0; range 16.7–78.2) and 1.05 mEq/day (IQR −4.40 to 6.9; range −32.7–43.4), respectively. NEAP closely correlated with PRAL (Rho = 0.95, p < 0.001). Median eGFR was 74.2 ml/min/1.73 m2, and 182 individuals (21 %) were considered to have CKD defined as eGFR <60 ml/min/1.73 m2 with moderate (n = 181, eGFR 30.9–58.9 ml/min/1.73 m2) or, in one individual, severe (eGFR = 21.8 ml/min/1.73 m2) impairment of renal function. Baseline characteristics of study subjects stratified by quartiles of NEAP are shown in Table 1. Along with increasing NEAP, the proportion of men increased, whereas no differences were observed as regards to the proportion of diabetes, CVD, or levels of BMI and eGFR. Alcohol intake, energy intake, and lean body mass increased across increasing NEAP quartiles.
Dietary acid load and bone mineral density
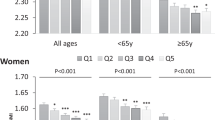
Along with increasing NEAP quartiles, T-scores for total body BMD, and BMD for the femoral neck, spine, and hip were rather similar for Q1–Q3 but higher for Q4 (Table 2). The multivariate regression analysis (Table 2) failed, however, to show any statistically significant association between dietary acid load and DEXA measures when confounders were considered. Null associations were also observed when including T-scores serving as the dependent variable (data not shown). Osteoporosis was clinically identified in 18 % (157 cases) of individuals. The proportion of individuals with osteoporosis decreased with increasing quartiles of dietary acid load: 27 % in Q1, 21 % in Q2, 19 % in Q3, and 14 % in Q4, respectively, based on NEAP. Nevertheless, the risk of osteoporosis did not associate with dietary acid load (Fig. 1). Adjustment for renal function did not modify this null association. We identified 182 individuals with manifest CKD (eGFR <60 ml/min/1.73 m2). Stratification by the presence of CKD yielded similar results in each stratum (Fig. 2).
Odds ratios (and 95 % CI) for the presence of osteoporosis across quartiles of the distribution of dietary acid load calculated by net endogenous acid production (NEAP) and potential renal acid load (PRAL) algorithms, respectively. The percentages of osteoporosis across dietary acid load quartiles of distribution were 27 % in Q1, 21 % in Q2, 19 % in Q3, and 14 % in Q4, respectively; model A was adjusted by sex and energy intake; model B was adjusted by sex, energy intake, body mass index, lifestyle factors (alcohol intake, smoking, physical exercise, education), and eGFR
Odds ratios (and 95 % CI) for the presence of osteoporosis (a, b) and hazard ratios (and 95 % CI) for the risk of fractures (c, d) associated to dietary acid load and after stratification by the presence of CKD (<60 ml/min/1.73 m2). Models are fully adjusted by sex, energy intake, body mass index, and lifestyle factors (alcohol intake, smoking, physical exercise, education)
Dietary acid load and the risk of fractures
The men and women in PIVUS were assessed after a follow-up time of 9.2 ± 2.4 years (IQR 8.8–10.8 years, range 0.1–11.8 years). During the follow-up, 131 cases of fractures were validated. In Cox regression models, neither PRAL nor NEAP associated with fracture risk (Table 3). Additional adjustment for possible confounders including eGFR did not modify these null associations. Stratification by the presence of CKD did not modify the results (Fig. 2).
Because lean body mass increased across the categories of NEAP likely due to a higher proportion of men, we further tested, as a sensitivity analysis, lean body mass as an additional confounder in Cox regression models. Resulting hazards were largely unaffected (data not shown). Consideration of the CAPA-eGFR equation to estimate kidney function yielded similar results (Supplemental figure and table). In the setting of a HR equal to 1.22 (95 % CI 0.86–1.17) (high NEAP group versus low NEAP group divided by median value of NEAP) including 861 subjects and 131 events (overall events ratio = 0.123), the power of our study is 0.82, which we take as reasonably good to support our statements.
Discussion
The dietary acid load (estimated both by PRAL and NEAP) did not associate with BMD, osteoporosis, or fracture risk among elderly Swedish individuals. Taking kidney function into consideration did not modify these null findings.
A Western diet contains typically a NEAP score of about 50 mEq/day [29]. This fits well with NEAP estimates from nationally representative US populations reporting an average dietary acid load of 48 mEq/day [6] and 45 mEq/day [33]. The estimated dietary acid load in the current study was, however, slightly lower (40 mEq/day), which may reflect different dietary habits in the Nordic countries or a selection bias of more health-oriented individuals accepting to participate in our survey. Thus, the putative negative effect of acid load on bone could have been concealed since the body could correct the acid-base imbalance in the low range of acid load intake. Furthermore, the calculation of NEAP and PRAL uses protein intake as a surrogate of sulfur amino acid production; this is an inherent limitation of the applied algorithms as one cannot separate the potentially harmful effects of acid production from the anabolic effects of protein intake which should have a favorable impact on bone health. In our study, the daily protein intakes had a similar range (1.0 ± 0.3 g/kg/day) as that reported for individuals in their 70s, or above, from the USA [34]. Metabolic acidosis, to which an increased protein intake could contribute, stimulates protein degradation and leads to muscle loss [35]. On the other hand, it is likely that any negative association between dietary acid load and bone health-related parameters may be neutralized by positive anabolic effects of an increased dietary intake of protein or calcium [36], as well as by an increased alkalinogenic impact from sufficient intake of fruits and vegetables [37]. This could perhaps additionally contribute to explain our null findings. The observation that lean body mass was higher in individuals with increased dietary acid load in our study is in line with these individuals having a higher protein intake, and complements a very recent study reporting that a higher alkaline dietary load is associated with greater indexes of skeletal muscle mass in women [38]. Thus, a protective effect on bone of increased weight loading and muscle strength associated with higher lean body mass linked to higher protein intake could have masked the putative negative effect of acid load on the investigated parameters.
We did not observe an association between dietary acid load and risk of fractures, adding to previous prospective observational studies and meta-analyses [15, 23, 39] refuting the dietary acid load hypothesis of bone loss. One possible explanation is that in nutritional epidemiology, we assume that dietary intake remains constant over time, but changes in acid intake can possibly vary throughout seasons (higher intake of fruits and vegetables during summer/spring) and throughout life. However, the effect of fruit and vegetables on bone resorption seems, at least in rats, to be independent of the acid-base balance [40]. It has been proposed [41] that age-related metabolic acidosis due to renal function deterioration could be pathophysiologically implicated in the increase of osteoporosis prevalence with aging. However, and for the sake of completeness, other studies do not support this relationship [42, 43]. In our study, we hypothesized that age-related deterioration in kidney function could confound and amplify the effect of dietary acid load on bone and fractures by virtue or impaired ability to excrete excess acid. Our hypothesis proved negative in this study, but we must acknowledge that the design of the cohort, with individuals of same age, ethnicity, and geographical location may provide a too narrow range of both dietary acid load and kidney function to fully capture this effect.
The present study has several strengths including the use of 7-day food records which provides reasonably reproducible measurements of dietary intake [44]. We were also able to assess associations with bone density and fracture risk in the same individuals and benefited from a richness of data usually not available in large population cohorts. The validation of cases in registers with limited loss to follow-up and high validity also offers a strength compared with self-reports. Also, both adjustments for kidney function and stratification by kidney disease further strengthens our considerations of confounders. However, several limitations should be recognized: Although the subjects in our study had similar age, ethnicity, and geographical distribution, which may be a strength towards population homogeneity, this limits the generalizability of our statements. Overall, the range of kidney function in this population was narrow, and CKD individuals were mostly in the range of moderate impairment. We cannot therefore not exclude that an effect would be seen in individuals with more advanced disease stages. However, those individuals would have received dietary counselling to reduce protein intake and acidic load as a disease prevention strategy. Bicarbonate levels were unfortunately not available in our cohort in order to test if an increased dietary acid load associated with metabolic acidosis. However, community screenings from the USA have suggested that this is the case [9]. Furthermore, the relatively small number of cases of fractures could influence the statistical power and, to some extent, induce a type II error, thus, further explorations in larger sample size cohorts are warranted. Moreover, although efforts were made to adjust for confounders, residual confounding of other potential factors is a limitation of this or any observational study. In particular, we acknowledge the lack of other bone turnover markers, serum vitamin D, and urinary calcium excretion.
Conclusions
Dietary acid load did not associate with BMD, osteoporosis, or fracture risk in Swedish community-dwelling elderly men and women. Our results add to previous evidence challenging the acid-base hypothesis of bone loss.
References
Chrischilles EA, Butler CD, Davis CS, Wallace RB (1991) A model of lifetime osteoporosis impact. Arch Intern Med 151:2026–2032
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res 22:465–475
Tucker KL, Hannan MT, Kiel DP (2001) The acid-base hypothesis: diet and bone in the Framingham Osteoporosis Study. Eur J Nutr 40:231–237
Fenton TR, Lyon AW, Eliasziw M, Tough SC, Hanley DA (2009) Meta-analysis of the effect of the acid-ash hypothesis of osteoporosis on calcium balance. J Bone Miner Res 24:1835–1840
Hanley DA, Whiting SJ (2013) Does a high dietary acid content cause bone loss, and can bone loss be prevented with an alkaline diet? J Clin Densitom 16:420–425
Sebastian A, Frassetto LA, Sellmeyer DE, Merriam RL, Morris RC Jr (2002) Estimation of the net acid load of the diet of ancestral preagricultural Homo sapiens and their hominid ancestors. Am J Clin Nutr 76:1308–1316
Remer T, Manz F (1995) Potential renal acid load of foods and its influence on urine pH. J Am Diet Assoc 95:791–797
Kurtz I, Maher T, Hulter HN, Schambelan M, Sebastian A (1983) Effect of diet on plasma acid-base composition in normal humans. Kidney Int 24:670–680
Amodu A, Abramowitz MK (2013) Dietary acid, age, and serum bicarbonate levels among adults in the United States. Clin J Am Soc Nephrol 8:2034–2042
Sebastian A, Harris ST, Ottaway JH, Todd KM, Morris RC (1994) Improved mineral balance and skeletal metabolism in postmenopausal women treated with potassium bicarbonate. N Engl J Med 330:1776–1781
Sellmeyer DE, Stone KL, Sebastian A, Cummings SR, G SOFR (2001) A high ratio of dietary animal to vegetable protein increases the rate of bone loss and the risk of fracture in postmenopausal women. Am J Clin Nutr 73:118–122
Krieger NS, Frick KK, Bushinsky DA (2004) Mechanism of acid-induced bone resorption. Curr Opin Nephrol Hypertens 13:423–436
Fenton TR, Eliasziw M, Tough SC, Lyon AW, Brown JP, Hanley DA (2010) Low urine pH and acid excretion do not predict bone fractures or the loss of bone mineral density: a prospective cohort study. BMC Musculoskelet Dis 11:88
Litzow JR, Lemann J Jr, Lennon EJ (1967) The effect of treatment of acidosis on calcium balance in patients with chronic azotemic renal disease. J Clin Invest 46:280–286
Welch AA, Bingham SA, Reeve J, Khaw KT (2007) More acidic dietary acid-base load is associated with reduced calcaneal broadband ultrasound attenuation in women but not in men: results from the EPIC-Norfolk cohort study. Am J Clin Nutr 85:1134–1141
New SA, MacDonald HM, Campbell MK, Martin JC, Garton MJ, Robins SP, Reid DM (2004) Lower estimates of net endogenous non-carbonic acid production are positively associated with indexes of bone health in premenopausal and perimenopausal women. Am J Clin Nutr 79:131–138
Wynn E, Lanham-New SA, Krieg MA, Whittamore DR, Burckhardt P (2008) Low estimates of dietary acid load are positively associated with bone ultrasound in women older than 75 years of age with a lifetime fracture. J Nutr 138:1349–1354
Rahbar A, Larijani B, Nabipour I, Mohamadi MM, Mirzaee K, Amiri Z (2009) Relationship among dietary estimates of net endogenous acid production, bone mineral density and biochemical markers of bone turnover in an Iranian general population. Bone 45:876–881
Macdonald HM, New SA, Fraser WD, Campbell MK, Reid DM (2005) Low dietary potassium intakes and high dietary estimates of net endogenous acid production are associated with low bone mineral density in premenopausal women and increased markers of bone resorption in postmenopausal women. Am J Clin Nutr 81:923–933
Feskanich D, Willett WC, Stampfer MJ, Colditz GA (1996) Protein consumption and bone fractures in women. Am J Epidemiol 143:472–479
Dargent-Molina P, Sabia S, Touvier M, Kesse E, Breart G, Clavel-Chapelon F, Boutron-Ruault MC (2008) Proteins, dietary acid load, and calcium and risk of postmenopausal fractures in the E3N French women prospective study. J Bone Miner Res 23:1915–1922
Bonjour JP (2013) Nutritional disturbance in acid–base balance and osteoporosis: a hypothesis that disregards the essential homeostatic role of the kidney. Br J Nutr 110:1168–1177
Munger RG, Cerhan JR, Chiu BC (1999) Prospective study of dietary protein intake and risk of hip fracture in postmenopausal women. Am J Clin Nutr 69:147–152
Hallan SI, Dahl K, Oien CM, Grootendorst DC, Aasberg A, Holmen J, Dekker FW (2006) Screening strategies for chronic kidney disease in the general population: follow-up of cross sectional health survey. BMJ 333:1047
Lind L, Andersson J, Ronn M, Gustavsson T, Holdfelt P, Hulthe J, Elmgren A, Zilmer K, Zilmer M (2008) Brachial artery intima-media thickness and echogenicity in relation to lipids and markers of oxidative stress in elderly subjects:–the Prospective Investigation of the Vasculature in Uppsala Seniors (PIVUS) study. Lipids 43:133–141
Becker W (1999) Dietary guidelines and patterns of food and nutrient intake in Sweden. Br J Nutr 81(Suppl 2):S113–S117
Willett W, Stampfer MJ (1986) Total energy intake: implications for epidemiologic analyses. Am J Epidemiol 124:17–27
Remer T, Dimitriou T, Manz F (2003) Dietary potential renal acid load and renal net acid excretion in healthy, free-living children and adolescents. Am J Clin Nutr 77:1255–1260
Frassetto LA, Todd KM, Morris RC Jr, Sebastian A (1998) Estimation of net endogenous noncarbonic acid production in humans from diet potassium and protein contents. Am J Clin Nutr 68:576–583
Kanis JA, Adachi JD, Cooper C et al (2013) Standardising the descriptive epidemiology of osteoporosis: recommendations from the Epidemiology and Quality of Life Working Group of IOF. Osteoporos Int 24:2763–2764
Larsson A, Malm J, Grubb A, Hansson LO (2004) Calculation of glomerular filtration rate expressed in mL/min from plasma cystatin C values in mg/L. Scand J Clin Lab Invest 64:25–30
Grubb A, Horio M, Hansson LO et al (2014) Generation of a new cystatin C-based estimating equation for glomerular filtration rate by use of 7 assays standardized to the international calibrator. Clin Chem 60:974–986
McLean RR, McLennan CE, Qiao N, Broe KE, Tucker KL, Cupples LA, Hannan MT (2007) Net endogenous acid production (NEAP) and bone mineral density in men and women: the Framingham Offspring Study. J Bone Miner Res 22:S307
Fulgoni VL 3rd (2008) Current protein intake in America: analysis of the National Health and Nutrition Examination Survey, 2003–2004. Am J Clin Nutr 87:1554S–1557S
May RC, Kelly RA, Mitch WE (1986) Metabolic acidosis stimulates protein degradation in rat muscle by a glucocorticoid-dependent mechanism. J Clin Invest 77:614–621
McLean RR, Qiao N, Broe KE, Tucker KL, Casey V, Cupples LA, Kiel DP, Hannan MT (2011) Dietary acid load is not associated with lower bone mineral density except in older men. J Nutr 141:588–594
New SA (2003) Intake of fruit and vegetables: implications for bone health. Proc Nutr Soc 62:889–899
Welch AA, MacGregor AJ, Skinner J, Spector TD, Moayyeri A, Cassidy A (2013) A higher alkaline dietary load is associated with greater indexes of skeletal muscle mass in women. Osteoporos Int 24:1899–1908
Thorpe DL, Knutsen SF, Beeson WL, Rajaram S, Fraser GE (2008) Effects of meat consumption and vegetarian diet on risk of wrist fracture over 25 years in a cohort of peri- and postmenopausal women. Public Health Nutr 11:564–572
Muhlbauer RC, Lozano A, Reinli A (2002) Onion and a mixture of vegetables, salads, and herbs affect bone resorption in the rat by a mechanism independent of their base excess. J Bone Miner Res 17:1230–1236
Frassetto LA, Morris RC Jr, Sebastian A (1996) Effect of age on blood acid-base composition in adult humans: role of age-related renal functional decline. Am J Physiol 271:F1114–F1122
Hsu CY, Cummings SR, McCulloch CE, Chertow GM (2002) Bone mineral density is not diminished by mild to moderate chronic renal insufficiency. Kidney Int 61:1814–1820
Eustace JA, Astor B, Muntner PM, Ikizler TA, Coresh J (2004) Prevalence of acidosis and inflammation and their association with low serum albumin in chronic kidney disease. Kidney Int 65:1031–1040
Schatzkin A, Kipnis V, Carroll RJ, Midthune D, Subar AF, Bingham S, Schoeller DA, Troiano RP, Freedman LS (2003) A comparison of a food frequency questionnaire with a 24-hour recall for use in an epidemiological cohort study: results from the biomarker-based Observing Protein and Energy Nutrition (OPEN) study. Int J Epidemiol 32:1054–1062
Acknowledgments
This work was supported by the grants from the Swedish Research Council. Baxter Novum is the result of a grant from Baxter Healthcare Corporation to Karolinska Institutet.
Conflicts of interest
BL is affiliated with Baxter Healthcare Corporation. TEL is an employee of Astellas. Ting Jia, Liisa Byberg, Lars Lind, Karl Michaëlsson, and Juan Jesus Carrero declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplemental figure
(DOCX 56 kb)
Supplemental table
(DOCX 18 kb)
Rights and permissions
About this article
Cite this article
Jia, T., Byberg, L., Lindholm, B. et al. Dietary acid load, kidney function, osteoporosis, and risk of fractures in elderly men and women. Osteoporos Int 26, 563–570 (2015). https://doi.org/10.1007/s00198-014-2888-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-014-2888-x