Abstract
Summary
Cadaver and phantom measurements and simulations confirmed that radiation exposure in 3D QCT of the spine can be reduced if 80 kV instead of 120 kV protocols are used; 120 mAs and slice thicknesses of 1–1.3 mm should be usable but obese patient will require higher milliampere-second settings.
Purpose
To develop a low-radiation exposure CT acquisition protocol for 3D QCT of the thoracolumbar spine.
Methods
Twenty-six cadavers were scanned with a standard protocol of 120 kV, 100 mAs and with a low-dose protocol using 90 kV, 150 mAs. The scan range included the vertebrae T6 to L4. Each vertebra was segmented and the integral volume and BMD of the total vertebral body were determined. Effective dose values were estimated. The impact of milliampere-second reduction on image quality was simulated by adding noise.
Results
One hundred ninety-six vertebrae were analyzed. Integral volume as well as integral BMD correlated significantly (p < 0.001) between standard and low-dose protocols (volume, r 2 = 0.991, residual root mean square (RMS) error, 0.77 cm3; BMD, r 2 = 0.985, RMS error, 4.21 mg/cm3). The slope significantly differed from 1 for integral BMD but not for volume hinting at residual field inhomogeneity differences between the two voltage settings that could be corrected by cross-calibration. Compared to the standard protocol, effective dose was reduced by over 50 % in the low-dose protocol. Adding noise in the 90 kV images to simulate a reduction from 150 to 100 mAs did not affect the results for integral volume or BMD.
Conclusions
For 3D QCT of the spine, depending on scanner type, 80 or 90 kV instead of 120 kV protocols may be considered as an important option to reduce radiation exposure; 120 mAs and slice thicknesses of 1–1.5 mm are usable if segmentation is robust to noise. In obese patients, higher milliampere-second settings will be required.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
3D quantitative computed tomography (QCT) is increasingly used to measure bone mineral density (BMD) and bone geometry in order to diagnose osteoporosis and to monitor age- and treatment-related changes [1]. While dual X-ray absorptiometry (DXA) remains the gold standard of osteodensitometry, integral, trabecular, and cortical bone compartments can be assessed separately with QCT. This is important to better understand the differential effects of interventions and one reason why QCT recently has been integrated into many pharmaceutical trials in osteoporosis [2–4]. QCT images can also provide the basis for finite element analysis (FEA) to determine bone strength.
However, compared to DXA, the radiation exposure in QCT is considerably higher, even for standard scan protocols that typically include L1 and L2 [1]. Recently, within the German research collaboration BioAsset (Biomechanically founded individualized osteoporosis Assessment and treatment) [5] a longer thoracolumbar spine segment of T6 to L4 was scanned that includes virtually all vertebrae susceptible to osteoporotic fracture. This research protocol in turn triggered the current study to address dose reduction in 3D QCT but of course the topic is independent of the number of vertebrae scanned.
Radiation exposure for QCT has been the focus of an earlier publication [6] but the results were obtained for single-slice imaging and do not apply to the newer spiral QCT protocols used nowadays for 3D imaging of complete spine segments. These use an X-ray tube voltage of 120 kV with around 100 mAs and a slice thickness of 1–3 mm. The easiest way to reduce radiation exposure is to lower the tube current–time product (mAs). One effect is an increase in noise which complicates the segmentation required for the BMD analysis. An increase in noise can principally be compensated by a larger slice thickness or a smoother tomographic reconstruction kernel; however, this reduces the spatial resolution of the CT data, which is an undesired effect in particular with respect to the assessment of cortical bone. Lowering the tube voltage is also effective to reduce radiation exposure [7–10] but has not been applied to 3D QCT although the early single-slice QCT protocols for assessment of BMD in the spine in fact used 80 kV [11, 12]. However, in these early studies, usually an elliptical trabecular volume of interest (VOI) has been analyzed, only and the slice thickness of 8 or 10 mm was much larger compared to the 1–1.25 mm used in state of the art 3D protocols. With 3D QCT techniques, additional VOIs such as the total vertebral body are also assessed which requires an accurate segmentation. Therefore, the effect of tube voltage reduction on VOI must also be examined.
In the present study with human cadavers, we investigated the effect of switching from a 120 kV to a 90 kV protocol on the quantification of BMD and volume of the vertebral bodies. We also simulated the effect of different milliampere-second settings on segmentation and analysis. The expected dose reduction was computed using Monte Carlo simulations.
Materials and methods
Sample data
Twenty-six cadavers, men and women of 65–90 years old were scanned within 7.3 ± 1.6 days after death and prior to autopsy. Informed consent was obtained from the family members after comprehensive information on relevant issues was given. Institutional approval for the study procedures had been obtained from the Ethics Committee of the Hamburg Chamber of Physicians (PV3486).
QCT acquisition and reconstruction
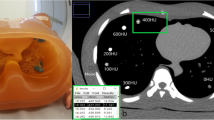
Two CT scans were performed on a clinical Philips MX8000 CT with a standard protocol using 120 kV and 100 mAs and a second low-dose protocol using 90 kV and 150 mAs. All other parameters were the same for both scans: table height, pitch of 1 and slice thickness of 1.3 mm, field of view of 15 cm and reconstruction kernel B. The scan range included vertebrae from T6 to L4 with adjacent endplates of T5 and L5. BMD calibration was performed using the QRM bone density calibration (BDC) phantom (QRM GmbH, Möhrendorf, Germany) scanned simultaneously with each cadaver. An example of the standard and the low-dose scan is presented in Fig. 1.
Axial and sagittal multiplanar reconstructions (MPR) from two CT datasets of the same cadaver under four different imaging conditions. Top left QCT standard protocol (120 kV, 100 mAs); top right low-dose protocol (90 kV, 150 mAs); bottom low-dose protocol with simulated 100 mAs (left) and with 50 mAs (right). Window/Center setting for all MPRs: 1000/-24 HU. The contours indicate integral VOIs for which volume and BMD were quantified
Image processing
The MIAF-Spine (MIAF: Medical Image Analysis Framework, version 3.1.5) developed at the IMP was used for analysis. Each vertebra was segmented individually. The spinal and dorsal processes and the ribs in the thoracic vertebrae were excluded. For the purpose of this study, only integral volume and BMD of the total vertebral body VOIs were determined. Fractured vertebrae, vertebrae filled with cement after vertebrae- or kyphoplasty and vertebrae with metal hardware were excluded from analysis. Two different analyses were performed: the scans obtained at 90 and 120 kV were analyzed independently, i.e., two different VOIs were obtained and compared (A1). In order to explore whether differences in bone-soft-tissue contrast between 90 and 120 kV had an impact on segmentation the VOIs obtained at 90 kV datasets were transferred to the 120 kV scans which were performed without repositioning the cadavers in-between (A2). Thus, for A2 analysis, VOIs were identical for 90 and 120 kV protocols.
Estimation of radiation exposure
The software package ImpactDose (CT Imaging GmbH, Erlangen) was used to estimate effective dose values [13]. It calculates organ dose and effective dose values for arbitrary scan parameters and anatomical ranges. Values for primary radiation are derived from measurements or manufacturer specifications; values for scattered radiation are derived from Monte Carlo calculations tabulated for standard anthropomorphic phantoms representing average and obese male and female subjects [14]. ImpactDose version 2.0 supports tissue weighting factors from ICRP 60 and ICRP 103 [15]. With respect to QCT of the spine the main difference between the two ICRP publications is an increase of the tissue weighting factor for the breast from 0.05 in ICRP 60 to 0.12 in ICRP 103.
Simulation of noise
In order to explore the possibility of further dose reduction, in four vertebrae (T9, T10, L1, and L2) from six cadavers (two fractured vertebrae were excluded, resulting in n = 22) a milliampere-second reduction was simulated by adding noise to the CT images. Specifically, datasets of six cadavers with large body sizes were selected so that their original noise levels were rather high already. Artificial noise was added under the assumption of independent Gaussian noise N(0; G) in every voxel as follows. Given that milliampere-second is proportional to the squared signal-to-noise ratio SNR 2 and thus to 1/G 2, we conclude that:
where G can be measured as standard deviation of the CT values in a given VOI in HU values. Thus G 2 denotes the variance. Consequently, in order to simulate Gaussian noise N(0;G 2) in an image with the noise level N(0;G 1), G 2 > G 1, we added Gaussian noise N(0, ∆G), where G 2 2 = G 2 1 + ∆G 2, so that
An example dataset with simulated noise is shown in Fig. 1. For the validation of the formula above, the European Spine Phantom (ESP, Fig. 2) was scanned on a Siemens SOMATOM Definition Flash using 120 kV with 100, 80, and 50 mAs and 80 kV with 150 and 100 mAs. Slice thickness was 1 mm, pitch 1, field of view 20 cm, and reconstruction kernel B40s.
Statistical analysis
Integral BMD and volume were compared between the standard and the low-dose protocols using Pearson correlation coefficients (r) and the Wilcoxon signed rank test for related samples because of non normal distribution (see “Results”). For the noise simulations, repeated measures ANOVA was used with one within-subject factor having three levels: standard protocol and two low-dose protocols with simulated 100 and 50 mAs. Matched pairs t tests were conducted post hoc for integral BMD and volume to compare the 150 mAs low-dose protocol with simulated 100 and 50 mAs protocols, using the Šidák correction as adjustment for multiple comparisons. The normality of all data was checked with the Kolmogorov–Smirnov test. All statistical procedures were performed with SPSS Statistics 20 (IBM Corp.).
Results
Dose estimates
Table 1 shows the estimated dose values for the QCT protocols used in this study. Effective dose estimates are given for four different Siemens CT scanners for 80 and 120 kV. Most scanners offer 80 and 120 kV instead of 90 and 120 kV as implemented on the Philips scanner which was used for the cadaver measurements. The Philips scanner is not included in ImpactDose. For all dose calculations, a scan length of 30 cm (Fig. 3) for the spine segment T6–L4 was assumed based on measurements in five cadavers with a total body height of 155.8 ± 7.05 cm that resulted in an average length of 29 ± 2.6 cm. Changing start and end points of the scan had little impact on effective dose estimates. For example, shifting the position by 6 cm (i.e., by approximately two vertebrae) in caudal direction changed the effective dose by less than 1 % (120 kV 100 mAs, female phantom, Somatom 64 scanner). In addition, dose values were estimated for a scan covering only L1 and L2, the configuration currently used in most spinal QCT studies [1]. The effective dose using the tissue weighing factors according to ICRP103 was approximately 14 % higher compared to ICRP60 in women due to the increase in the breast tissue weighing factors.
BMD and volume measurements
In the 26 cadavers, a total of 196 vertebrae were included in the analysis. For analysis A1, integral volume as well as integral BMD for T6 to L4 were highly correlated (Fig. 4) between standard and low-dose protocols (volume, r 2 = 0.991, residual root mean square (RMS) error = 0.77 cm3; BMD, r 2 = 0.985, RMS error = 4.21 mg/cm3). All correlation coefficients were significant (p < 0.001). For integral volume, no significant slope or offset were observed. The values were equal on average, with mean volumes of 25 ± 8 cm3 both in 120 and 90 kV, and pairwise equal according to the Wilcoxon signed rank test for related samples (p = 0.683). Both BMD and volume values at 120 and 90 kV were not normally distributed. At 120 kV, average BMD was 151 ± 35 mg/cm3 versus 141 ± 33 mg/cm3 at 90 kV. There was a slope of 1.034 (significantly different from 1 with p < 0.001) and an offset of 4.58 mg/cm3 (p = 0.001) in integral BMD between the 120 and 90 kV protocols after calibration with the BDC phantom, hinting at residual field inhomogeneity differences between the two voltage settings.
For A2, in which analysis VOIs were registered, there was a slope of 1.029 (significantly different from 1 with p < 0.001) and an offset of 3.75 mg/cm3 (p < 0.001). The residual RMS error was 2.74 mg/cm3, r 2 = 0.994. However, differences between A1 and A2 for slopes and offsets were not significant despite the fact that the two segmentations at 120 kV obtained for A1 and A2 were slightly different: at 120 kV average differences in BMD of 1.6 mg/cm3 between analyses A1 and A2 were small and significant (p < 0.001).
Noise
Noise was measured as standard deviation in HU in the cylindrical VOIs placed in the inserts of the BDC phantom. Although the noise level showed a slight tendency to increase with higher BMD values (Table 2), this dependence was not significant, i.e., noise levels were independent of the BMD values of the inserts (p >> 0.5 both in ANOVA and correlation analysis). The mean noise level in the datasets obtained with the standard 120 kV protocol was 18 HU, it increased to 23 HU in the low-dose 90 kV protocol.
Table 3 shows the noise measurements in the ESP in the VOIs shown in Fig. 2. Table 4 lists the corresponding variance ratios G 2 2/G 2 1, which are in good agreement with the corresponding milliampere-second ratios confirming Eqs. 1 and 2. In the ESP scan, the noise was higher than in comparable cadaver scans, as can be seen when comparing noise values for 120 kV and 100 mAs. This has a number of reasons: in the ESP, a slice thickness of 1 mm was used whereas in the cadavers a slice thickness of 1.3 mm was used. Also, 80 instead of 90 kV were used. Similar reconstructions kernels were used but kernels from different CT manufacturers have different noise and resolution characteristics. Finally, in order to compare the cadaver and the phantom scans, noise should be measured in a comparable location, i.e., in this case, in the calibration phantom. In the 200 mg/cm3 insert of the calibration phantom positioned under the ESP, at 120 kV/100 mAs, a standard deviation of 23 HU and at 80 kV/150 mAs, a standard deviation of 42 HU was measured. The 23 HU scales to 20.2 HU in a 1.3-mm-thick slice, which compares well with the 19 HU measured in the BDC of the cadaver scans, despite the remaining difference in kilovolts.
Table 5 shows the effect of the simulated decrease of exposure, 100 and 50 mAs, in six cadaver datasets in the 90 kV protocol. For this, larger cadavers resulting in higher image noise were selected. The noise in the 150 mAs column of Table 5 was higher than the average of 24 HU reported in Table 2. The added noise did not affect the results for integral volume as revealed by ANOVA with repeated measures for three noise levels (multivariate profile analysis). In contrast, integral BMD significantly changed (p = 0.015) as confirmed by four alternative statistical criteria, which produced equivalent results: Pillai’s trace, Wilks’ lambda, Hotelling’s trace, and Roy’s largest root. Post hoc analysis revealed that in the simulated 50 mAs datasets BMD values were significantly lower compared to 150 mAs (p = 0.022) and borderline lower compared to 100 mAs (p = 0.055) (Table 6). See also Fig. 5 for a graphical comparison of BMD values under various noise conditions.
Effect of increased noise: BMD comparison of 150 mAs with simulated 50 mAs (top left) and 100 mAs (top right) protocols, all using 90 kV. The comparison was performed in six selected datasets with a total of 22 vertebrae (for details, see text). In the bottom row, the same comparison is done with the help of Bland–Altman diagrams
Discussion
In this study, we revisited the use of a low-dose protocol for QCT of the spine. While pioneering work with single-slice QCT was already performed at 80 kV [11, 12], newer 3D spiral QCT protocols are based on 120 kV presumably to reduce noise. Two major reasons are the thinner slice thickness, which comes at a cost of higher noise: 1–3 versus 8–10 mm in the older single-slice approaches, and the sophisticated 3D image processing that is sensitive to noise, in particular, if not only the trabecular VOI but the complete vertebral body should be analyzed. Nevertheless, it is not fully clear why the earlier 80 kV protocols were abandoned in favor of 120 kV. Due to the decrease of Compton scatter and increase of the photoelectric absorption at 80 versus 120 kV the calcium contrast to noise ratio and as a consequence the calcium sensitivity increases at 80 kV [16, 17]. This was recently confirmed by extensive simulations using the dose weighted contrast to noise ratio (CNRD) [18]. An additional benefit of a lower tube voltage protocol is the significant reduction of the so called fat error, which describes the underestimation of trabecular BMD in the presence of marrow fat. A switch from 130 kV or above to 80 kV reduces the fat error by a factor of 1.5–2.5 [19, 20].
QCT has often been criticized as a high-dose technique. While radiation exposure in QCT is much lower than for most CT procedures performed in diagnostic radiology it is certainly higher than in DXA. Thus, reduction of radiation exposure in QCT is a continuing topic. If more than two vertebrae should be scanned such as in the BioAsset project, then obviously the radiation exposure is a major limiting factor of scan length because, for example for a 30-cm scan at 120 kV, an effective dose of 4–5 mSv for males and 5–6 mSv for females would be required (Table 1). Nevertheless, testing whether the reduction of 120 to 80 kV is favorable is independent of the number of vertebrae scanned. Interestingly, for 3D QCT, a comparison between voltage settings has not been published so far, although more broadly, for spinal CT low-dose protocols have been suggested before [21, 22]. Recent simulations supported by extensive phantom measurements proposed the use 80 kV for CT bone imaging in general [18].
We have analyzed possibilities of dose reduction by means of lower voltage and lower milliampere-second in cadavers. Specifically, we examined the effect of 90 versus 120 kV scan protocols. Most clinical whole-body CT scanners used for QCT offer an 80 kV instead of a 90 kV option. Therefore, for comparison we added scans of the European Spine Phantom (ESP) (QRM GmbH Möhrendorf, Germany), obtained from a Siemens scanner at 80 kV, while the cadavers were scanned on a Philips scanner. Major endpoints of the cadaver study were integral volume and integral BMD of the complete vertebral body.
As expected, noise measured as the standard deviation in HU values in the BDC phantom inserts was higher in the 90 kV compared to the 120 kV protocol (Table 2). However, the increased noise had no relevant effect on segmentation of the vertebral body. The paired volume and BMD measurements of the vertebrae were highly correlated (r 2 > 0.985). This means that the MIAF-Spine segmentation technique is not very sensitive to decreased image quality. The absolute difference in calibrated BMD values indicates differences in the scan field inhomogeneity at 90 and 120 kV requiring different corrections. However, as the correlation between BMD values at 90 and 120 kV was very high a linear correction approach, e.g., based on the scans of an appropriate phantom appears sufficient to obtain the same BMD results at 90 and 120 kV.
Moreover, the segmentation results were very stable with respect to noise, so that the radiation dose could likely be further reduced by decreasing the current-time product. The adopted simple simulation of low milliampere-second values by adding Gaussian noise is a coarse approximation value of the real changes in image quality, but it was in good agreement with phantom-based validation measurements. In our experiments, changes in volume and BMD were not significant for simulated 100 mAs compared to 150 mAs. The results for 50 mAs showed that changes in volume were still not significant but BMD values did differ slightly. From Fig. 5, it can be seen that the correlation coefficients decreased for 100 and 50 mAs when compared to Fig. 4. Thus, segmentation with 50 mAs is less stable and more error prone, and although the measured volume values remain unchanged on average, within a given patient variations increase. The reason that BMD but not volume differences at 50 mAs became significant can be explained by fact that a small volume change may cause a much higher BMD change because at the periosteal surface BMD values change rapidly between soft tissue and cortical bone. In the reported ANOVA analysis, we pooled all vertebral levels, but using the level as a between-subjects factor for otherwise the same repeated measures ANOVA didn’t change the conclusion.
The data in Table 5 indicate that in our cadaver dataset noise levels of around 40 HU measured in the BDC phantoms are a reasonable upper limit for acceptable image quality. This is comparable with a standard deviation of 42 HU at 80 kV/150 mAs obtained in the ESP measurements; 80 kV/120 mAs and a slice thickness of 1.3 mm would result in almost the same noise level. According to Table 1, even at 80 kV/150 mAs the dose reduction is larger than 50 % compared to the standard 120 kV/100 mAs protocol, which compares well with the reduction of up to 56.8 % in weighted CT dose index for abdominal examinations [23] performed with tube voltages of 120 and 90 kV and constant 300 mAs. An 80 kV protocol in standard scans of two vertebrae will limit the radiation exposure below 1 mSv.
Our study has a number of limitations. First, no cadavers with obese stature were included in the study, the average BMI was 22 kg/m2. Even those cadavers which were used for the simulation study and in which noise levels were highest had an average BMI of 25 kg/m2, only. The suggested 120 to 150 mAs protocol may not work in obese patients. In particular, higher milliampere-second values will be required to compensate the increased X-ray absorption, but of course this is partly true for the 120 kV protocol as well. Second, the cadaver scans had been performed on an older Philips scanner only providing 90 kV, while the ESP scans used for comparison were obtained at 80 kV on a Siemens scanner. Thus, settings were not immediately comparable; also, slice thicknesses and reconstruction kernels were different. But this is the standard scenario at least in multi center studies, where equipment from different manufactures is used. On the positive side, our study demonstrates that differences can be adjusted with adequate phantoms.
We have measured the cadavers with two different protocols only and have not tried to achieve identical contrast to noise ratios in the scans although the difference was small (Table 2). Of course, radiation exposure can be reduced by lower tube voltages but also by lowering the milliampere-second settings at a given kilovolt value. For example, the noise in the 120 kV 100 mAs protocol was still lower than in the 90 kV 150 mAs protocol (Table 2), thus the differences in exposure shown in Table 1 between 120 and 80 kV also reflect higher noise at 80 kV. However, a systematic investigation of the CNRD based on phantoms has shown that the use of 80 kV indeed is advantageous, i.e., lowering the kV setting is more effective than lowering milliampere-second settings [18]. At 80 kV the CNRD was 10 to 20 % higher, i.e., a given contrast to noise ratio could be obtained at a 10 to 20 % lower radiation exposure than at 120 kV. The advantage of 80 kV was smaller for larger phantoms and smaller in the lumbar than in the thoracic region. Adding the reduced fat error, these data together with the results of the current study underscore the advantages of an 80 kV protocol.
We did not consider automatic exposure control (AEC) options available on all modern whole-body CT scanners or advanced iterative reconstruction methods to further reduce radiation exposure. Second, the noise simulations were just based on random Gaussian noise, whereas in CT images structured noise as seen in Fig. 1 is more realistic because the X-ray attenuation in non circular objects varies with the angle between X-ray beam and object, or in other words varies among the tomographic projections used to reconstruct the image. Also all dose calculations using ImpactDose have to be interpreted within the limitations of the implemented dose estimation approach: it is based on geometrically defined phantoms and human anatomy may considerably deviate from phantoms. Also, the definition of the exact scan range is somewhat arbitrary although a slight shift within the phantoms had little effect on dose. Effective dose values depend on tissue weighing factors and the change from ICRP 60 to ICRP 103, which was based on new data and a new interpretation of existing data, nicely demonstrates the impact of changing their values. Also, differences in organ sizes and locations between patient and phantom and differences in geometry, spectrum, or filtration among CT scanners may significantly influence dose values. Therefore, the estimated effective dose values should be interpreted cautiously; however, the dose differences reported here between the two scanners and CT protocols will be largely accurate.
Finally, we acknowledge potential reservations against including thoracic vertebrae in spinal QCT and indeed it is not suggested that the current practice of scanning two (or sometimes three) lumbar vertebrae should be changed in particular as scanning larger segments results in a larger radiation exposure. The BioAsset research project, in which a longer segment of the spine is scanned, triggered this study but the result that an 80-kV scan protocol is advantageous for QCT of the spine and can be used without major impact on BMD results is independent of scan length. Using 80 kV instead of 120 kV for QCT of the spine is the most effective way to optimize radiation exposure. Other measures can have similar though somewhat inferior effects such as the use of patient size and location specific milliampere-second settings as realized by many AEC systems. Also, reducing the milliampere-seconds to allow for higher noise or combined with the use of thicker slices are means to reduce dose.
Almost all QCT studies of the spine recently reported in the literature were performed at 120 kV. This is most likely also true for most clinical measurements; perhaps with the exception of those using the older single-slice Osteo protocol still installed on various Siemens CT units. Of course, it is not advisable to change tube voltage in current studies or ongoing clinical programs in which data are compared with earlier visits. Also, abdominal or thoracic CT scans performed for various diagnostic tasks, which may be used for a later BMD analysis to address additional clinical questions, are usually taken at 120 kV. Nevertheless, as radiation exposure in CT is a topic of increasing public interest, dose reduction is a major focus of innovation in CT technology and one important recent insight is that besides AEC and iterative reconstruction algorithms lower kV settings would contribute to lower radiation exposure for many CT protocols and not just in osteodensitometry [18]. Thus, new programs using QCT of the spine should consider the advantages of an 80 kV protocol.
In summary, this study confirmed that radiation exposure in 3D QCT can be reduced if 80 kV instead of 120 kV protocols are used; 120 mAs and slice thicknesses of 1–1.3 mm should be usable if the applied segmentation is robust to noise. In obese patients, higher milliampere-second settings will be required. In new QCT spine projects, the use of 80 kV may be considered as an important option to reduce radiation exposure, unless existing data acquired at 120 kV should be used for comparisons.
References
Engelke K, Adams JE, Armbrecht G, Augat P, Bogado CE, Bouxsein ML, Felsenberg D, Ito M, Prevrhal S, Hans DB, Lewiecki EM (2008) Clinical use of quantitative computed tomography and peripheral quantitative computed tomography in the management of osteoporosis in adults: the 2007 ISCD official positions. J Clin Densitom 11(1):123–162
Lewiecki EM, Keaveny TM, Kopperdahl DL, Genant HK, Engelke K, Fuerst T, Kivitz A, Davies RY, Fitzpatrick LA (2009) Once-monthly oral ibandronate improves biomechanical determinants of bone strength in women with postmenopausal osteoporosis. J Clin Endocrinol Metab 94(1):171–180
Brixen, K., R. Chapurlat, A.M. Cheung, T.M. Keaveny, T. Fuerst, K. Engelke, R. Recker, B. Dardzinski, N. Verbruggen, S. Ather, E. Rosenberg, and A.E. de Papp (2013) Bone density, turnover, and estimated strength in postmenopausal women treated with odanacatib: a randomized trial. J Clin Endocrinol Metab, 2013/01/23
Yang L, Sycheva AV, Black DM, Eastell R (2013) Site-specific differential effects of once-yearly zoledronic acid on the hip assessed with quantitative computed tomography: results from the HORIZON Pivotal Fracture Trial. Osteoporos Int 24(1):329–338, 2012/11/07
Glüer, C.-C., M. Krause, O. Museyko, B. Wulff, G. Campbell, T. Damm, M. Daugshies, G. Huber, Y. Lu, J. Pena, S. Waldhausen, J. Bastgen, K. Rohde, I. Steinebach, F. Thomsen, M. Amling, R. Barkmann, K. Engelke, M. Morlock, J. Pfeilschifter, and K. Püschel, New horizons for the in vivo assessment of major aspects of bone quality: microstructure and material properties assessed by Quantitative Computed Tomography and Quantitative Ultrasound methods developed by the BioAsset consortium. Osteologie, submitted
Kalender WA (1992) Effective dose values in bone mineral measurements by photon absorptiometry and computed tomography. Osteoporos Int 2:82–87
Funama Y, Awai K, Nakayama Y, Kakei K, Nagasue N, Shimamura M, Sato N, Sultana S, Morishita S, Yamashita Y (2005) Radiation dose reduction without degradation of low-contrast detectability at abdominal multisection CT with a low-tube voltage technique: phantom study. Radiology 237(3):905–910, 2005/10/21
Karmazyn B, Liang Y, Klahr P, Jennings SG (2013) AJR Am J Roentgenol 200(5):1001–1005, 2013/04/27
Tang K, Wang L, Li R, Lin J, Zheng X, Cao G (2012) Effect of low tube voltage on image quality, radiation dose, and low-contrast detectability at abdominal multidetector CT: phantom study. J Biomed Biotechnol 2012:130169, 2012/05/24
Murakami Y, Kakeda S, Kamada K, Ohnari N, Nishimura J, Ogawa M, Otsubo K, Morishita Y, Korogi Y (2010) Effect of tube voltage on image quality in 64-section multidetector 3D CT angiography: Evaluation with a vascular phantom with superimposed bone skull structures. AJNR Am J Neuroradiol 31(4):620–625, 2009/11/28
Kalender WA, Klotz E, Suess C (1987) Vertebral bone mineral analysis: an integrated approach with CT. Radiology 164(2):419–423, 1987/08/01
Genant HK, Cann CE, Ettinger B, Gordan GS (1982) Quantitative computed tomography of vertebral spongiosa: a sensitive method for detecting early bone loss after oophorectomy. Ann Intern Med 97(5):699–705
Kalender WA, Schmidt B, Zankl M, Schmidt M (1999) A PC program for estimating organ dose and effective dose values in computed tomography. Eur Radiol 9(3):555–562, 1999/03/23
Zankl, M., W. Panzer, and G. Drexler (1991) The calculation of dose from external photon exposures using reference human phantoms and Monte Carlo methods. Part VI: Organ doses from computed tomographic examinations, Munich
ICRP, The 2007 Recommendations of the International Commission on Radiological Protection, ICRP 103. Ann ICRP, 2007. 37(2–4)
Genant HK, Boyd D (1977) Quantitative bone mineral analysis using dual energy computed tomography. Invest Radiol 12(6):545–551
Cann CE (1988) Quantitative CT for determination of bone mineral density: a review. Radiology 166:509–522
Kalender WA, Deak P, Kellermeier M, van Straten M, Vollmar SV (2009) Application- and patient size-dependent optimization of X-ray spectra for CT. Med Phys 36(3):993–1007, 2009/04/22
Glüer CC, Genant HK (1989) Impact of marrow fat on accuracy of quantitative CT. J Comput Assist Tomogr 13(6):1023–1035
Laval-Jeantet AM, Roger B, Bouysee S, Bergot C, Mazess RB (1986) Influence of vertebral fat content on quantitative CT density. Radiology 159(2):463–466, 1986/05/01
Abul-Kasim K (2010) Low-dose spine CT: optimisation and clinical implementation. Radiat Prot Dosim 139(1–3):169–172
Mulkens TH, Marchal P, Daineffe S, Salgado R, Bellinck P, te Rijdt B, Kegelaers B, Termote JL (2007) Comparison of low-dose with standard-dose multidetector CT in cervical spine trauma. AJNR Am J Neuroradiol 28(8):1444–1450, 2007/09/12
Nakayama Y, Awai K, Funama Y, Hatemura M, Imuta M, Nakaura T, Ryu D, Morishita S, Sultana S, Sato N, Yamashita Y (2005) Abdominal CT with low tube voltage: preliminary observations about radiation dose, contrast enhancement, image quality, and noise. Radiology 237(3):945–951, 2005/10/21
Acknowledgments
This project was supported by the German Federal Ministry of Education and Research (BMBF, BioAsset 01EC1005D).
Conflicts of Interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Museyko, O., Heinemann, A., Krause, M. et al. A low-radiation exposure protocol for 3D QCT of the spine. Osteoporos Int 25, 983–992 (2014). https://doi.org/10.1007/s00198-013-2544-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-013-2544-x