Abstract
Summary
Adherence and persistence to oral bisphosphonates in women with postmenopausal osteoporosis is suboptimal. In this study, patients were treated with either oral or intravenous bisphosphonates. The increased adherence and persistence observed in patients receiving intravenous medication compared with those receiving oral medication may improve health outcomes.
Introduction
Poor adherence and persistence to oral medication are often observed in women with postmenopausal osteoporosis (PMO). The purpose of the non-interventional BonViva Intravenous Versus Alendronate (VIVA) study was to determine whether, in a real-world setting, (1) increased adherence and persistence to medication would be observed in women with PMO receiving intravenous (i.v.) ibandronate versus oral alendronate, (2) a correlation exists between adherence and persistence to medication and drug efficacy, and (3) any unexpected adverse events/serious adverse events (AEs/SAEs) may occur.
Methods
The study was conducted in 632 centers in Germany. A total of 6,064 females with PMO were enrolled and recruited into one of two treatment arms: quarterly i.v. administration of 3 mg ibandronate or weekly oral medication of 70 mg alendronate, for 12 months. At the end of the study, adherence and persistence to medication, new osteoporotic fractures, mobility, use of analgesics, and AEs/SAEs were determined.
Results
Greater adherence and persistence to medication were observed in the ibandronate treatment arm compared with the alendronate treatment arm. Although there was no significant difference in the number of patients with new vertebral, hip, or forearm fractures between treatment arms, a significantly greater increase in mobility and decrease in the use of analgesics were reported in the ibandronate treatment arm. No unexpected AEs/SAEs occurred in either arm.
Conclusions
Adherence and persistence to medication were greater in women with PMO receiving i.v. ibandronate compared with those receiving oral alendronate. This may have led to an increase in mobility and a decrease in pain in these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a disease characterized by defined risk factors which increase fracture probability. These include age, low bone density, and history of fragility fracture in a first-degree relative [1]. Osteoporosis-related fractures are associated with an increase in morbidity and mortality [2].
A recent study using German statutory health insurance claims data from 2006 to 2009 showed that the prevalence of osteoporosis in females aged 50 years or older was 24 % [3]. In German women in this age group, the lifetime probability of a major osteoporotic fracture is 31.4 % [4]. Furthermore, recent data obtained from the Global Longitudinal Study of Osteoporosis in Women (GLOW) [5] showed that women with postmenopausal osteoporosis (PMO) and osteoarthritis have an even higher risk of fracture [6].
Bisphosphonates are established as first-line therapy for osteoporosis, with nitrogen-containing bisphosphonates currently considered the first-line treatment for PMO [7]. The most important goal of PMO treatment is to reduce the risk of fracture [7].
Several clinical trials have shown that oral bisphosphonates can reduce the incidence of both vertebral and non-vertebral fractures [8, 9], but in order for bisphosphonate treatment to be clinically effective, patients must demonstrate adequate adherence and persistence to medication. Adherence to medication is one of several terms currently used in the literature to define deviations from a prescribed treatment. As described by Vrijens et al. [10], the first of these terms to be introduced was “patient compliance” and, together with “medication adherence,” has been the most widely used term to describe such deviations. However, these descriptors are often used inconsistently, and in order to enable the accurate interpretation of studies on medication-taking behavior, Vrijens et al. [10] have proposed new terminology, “adherence to medication,” described as the process whereby patients take their medication as prescribed. The term comprises three components: (1) initiation (when a patient takes the first dose of a prescribed medication), (2) implementation (the extent to which the prescribed dosing regimen is followed), and (3) discontinuation (indicates the end of therapy, when the patient stops taking the prescribed medication for whatever reason). Based on this description, the following can be classed as instances of nonadherence to medication: noninitiation of prescribed treatment, suboptimal implementation of the dosing regimen, and premature discontinuation of treatment. Persistence is interrelated to adherence and has been described as the length of time between initiation and the point in time when the patient took the last dose of medication in question [10].
Despite the proven efficacy of oral bisphosphonates in reducing the risk of fracture and the association between increased medication adherence/persistence and reduced risk of fracture [11–13], approximately 50 % of patients discontinue medication within the first year [14]. Therefore, there is a need to increase patient awareness with regard to the potential negative impact of drug discontinuation.
There are many possible reasons why patients may be nonadherent or nonpersistent to oral bisphosphonates [15]. These include strict dosing requirements associated with oral bisphosphonates [16], drug-related adverse events (AEs) occurring in the gastrointestinal tract [17], and inconvenient short dosing intervals [18].
Intravenous (i.v.) administration of bisphosphonates was introduced to address the unmet clinical need for a treatment that could be administered less frequently, was associated with fewer AEs, and involved a less rigorous mode of administration. After an initial study to assess the dose–response relationship with intermittent i.v. injections of ibandronate in women with PMO [19], the Intermittent Regimen intravenous Ibandronate Study (IRIS) [20] and the Dosing IntraVenous Administration (DIVA) study [21, 22] were conducted in order to determine the efficacy and tolerability of the injections. Based on the results of the DIVA study, quarterly i.v. injections of 3 mg ibandronate were approved for the treatment of PMO in the USA and Europe. Furthermore, 5-year data from the DIVA study long-term extension showed that the long-term i.v. administration of quarterly ibandronate is effective and well tolerated in women with PMO [23].
Although the efficacy and safety of i.v. ibandronate have been assessed in several clinical trials, to date, there have been no studies assessing the adherence and persistence of patients receiving the drug, specifically for PMO in a real-world setting. A study conducted by Feldstein and colleagues [24] highlighted the importance of assessing adherence and persistence to medication in such a setting. The authors reported a similar time to first fracture in patients treated with oral bisphosphonates and patients not on osteoporotic medication. Therefore, data obtained from randomized clinical trials are not necessarily mirrored in the real-world setting, because patients may not fill their prescription, may not take their medication as prescribed, and may show a lack of persistence.
The BonViva Intravenous Versus Alendronate (VIVA) study was a non-interventional, multicenter study conducted over 12 months. The primary aim of this study was to assess and compare the adherence and persistence of patients with PMO to either i.v. ibandronate 3 mg administered quarterly or oral alendronate 70 mg taken weekly, in a real-world setting. Weekly alendronate served as the reference because it currently represents the first-line treatment in Germany, due to reimbursement issues. The secondary aims of the VIVA study were to determine whether a correlation exists between adherence and persistence to medication and drug efficacy and to assess and compare the safety of the two drugs in a real-world setting.
Methods
Study design and participants
VIVA was a non-interventional German, multicenter study. The study was conducted in 632 centers consisting mainly of private practices representative of current German clinical practice. A number of institutions with specialized outpatient clinics for osteoporosis were also involved.
Over a period of 8 months, 6,064 females with PMO were enrolled in the study. Participants were recruited from the overall population of patients with PMO requiring medical treatment.
Patients were recruited into one of two treatment arms: i.v. injections of 3 mg ibandronate (BonViva, Roche Pharma AG, Grenzach-Wyhlen, Germany) administered quarterly for 12 months or oral 70 mg alendronate (Fosamax, MSD Sharp & Dohme GmbH, Lindenplatz 1, 85540 Haar, Germany) taken weekly for 12 months. Participating physicians decided which patient to assign to which treatment arm independently from and prior to the start of the study. Because patient characteristics in the two arms were expected to be different (e.g., patients with gastrointestinal problems, those who have difficulty swallowing, those with fractures, and those with more severe osteoporosis are all more likely to be represented in the i.v. ibandronate treatment arm), patients were enrolled in a ratio of 3:1 in favor of ibandronate in order to facilitate a comparative evaluation using a matched pair analysis. The criteria used to create the matched pair population were as follows: age, body mass index, history of fracture at the start of therapy, number of vertebral fractures prior to the study, pretreatment with bisphosphonates, number of comorbidities, and current therapy started ±31 days before/after the baseline visit.
All patients provided written informed consent prior to their inclusion in the study. Ethical approval was obtained from the ethics committee of the principle investigator following the recommendations for non-interventional study conduct of the competent German authority, the Federal Institute for Drugs and Medical Devices.
Assessments
The observation period was 12 months for each patient. Each participating center had online access to the documentation portal containing case report forms for up to 12 patients.
Documentation consisted of one inclusion/baseline visit as well as one final visit after 12 months of treatment. Additionally, the documentation of data on a maximum of three optional interim visits was permitted.
Data documented at intake examination included patient characteristics and mobility. Data documented at three optional interim visits included the use of analgesics for osteoporosis-related pain. Data documented at the end of the 12-month observation period included nonadherence to medication, persistence to medication, new osteoporotic fractures, mobility, use of analgesics for osteoporosis-related pain, and AEs/serious AEs (SAEs). Based on the description proposed by Vrijens et al. [10], nonadherence to medication was calculated by taking into account the number of patients who discontinued treatment, for whatever reason, before the end of the study. Persistence was calculated as the time between the initiation of medication and the point at which the patient took the last dose of medication. Mobility was evaluated by the physician, using a questionnaire. Patients were assigned to the following categories: full mobility, mild physical limitations, moderate physical limitations, severe physical limitations (partly dependent on outside help), and very severe physical limitations (always dependent on outside help). For each treatment arm, a comparison was made between the number of patients with full mobility at the start and end of the study. Reduction in analgesic use was also evaluated by the physician, again using a questionnaire. Patients were asked to respond “yes” or “no” when asked whether their analgesic intake was reduced at the end of the study as compared to baseline.
Statistical analyses
Sample size calculation
The sample size calculation was based on persistence. Assuming a 5 % difference in persistence between the two treatment arms and a power of 80 %, 360 patients would be required per group (alpha = 0.05, beta = 0.2, Program N of IDV Gauting, Munich).
The distribution of 3:1 (i.v. ibandronate/oral alendronate) should ensure that for 90 % of the alendronate patients, a suitable partner for the matched pair analysis would be found in the ibandronate group. Based on this consideration, and assuming a dropout rate of 20–25 %, 1,200 patients treated with alendronate and 4,500 treated with ibandronate were included in the study, for a total of 6,000 patients.
Analysis of study endpoints
Except for the AEs/SAEs, all primary and secondary endpoints of the study were assessed in the matched pair population.
Statistical differences in nonadherence to medication between the two treatment arms were evaluated using Fisher’s exact test. Statistical differences in persistence between the two treatment arms were evaluated using chi-squared tests.
With regard to the secondary endpoints, statistical differences in mobility between treatment arms were evaluated using Wilcoxon–Mann–Whitney U test. Differences between treatment arms with respect to the number of new osteoporosis-related fractures, use of analgesics for treatment of osteoporosis-related pain, and AEs/SAEs were all evaluated using Fisher’s exact test.
Results
Patient disposition and baseline characteristics
A total of 6,064 females with PMO were enrolled in the VIVA study. Figure 1 shows the patient disposition. Baseline demographic and clinical characteristics of the total patient population and the matched pairs are shown in Table 1. The statistical analyses accounted for any differences in variables between the two treatment arms.
Primary endpoints
Adherence to medication
In the overall matched pair population, 130 patients (14.4 %) in the ibandronate group and 229 patients (25.4 %) in the alendronate group ended treatment due to nonadherence to medication (p < 0.001).
Persistence to medication
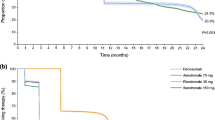
In the overall matched pair population, patients in the ibandronate group persisted on medication for a significantly greater number of days compared with patients in the alendronate group (Fig. 2a, mean number of days on ibandronate, 343; mean number of days on alendronate, 327, p < 0.001).
a Kaplan–Meier analysis showing persistence in patients receiving either ibandronate or alendronate over the 12-month study period in the overall matched pair population. b Kaplan–Meier analysis showing persistence in patients receiving either ibandronate or alendronate over the 12-month study period in the subpopulation of patients with prevalent osteoporosis-related fractures. c Kaplan–Meier analysis showing persistence in patients receiving either ibandronate or alendronate over the 12-month study period in the subpopulation of patients without prevalent osteoporosis-related fractures. i.v. intravenous
A similar pattern was observed when analyzing subpopulations of patients with and without prevalent osteoporosis-related fractures. In both subpopulations, patients in the ibandronate group persisted on medication for a significantly greater number of days compared with patients in the alendronate group (Fig. 2b, subpopulation of patients with prevalent osteoporosis-related fractures; mean number of days on ibandronate, 341; mean number of days on alendronate, 323, p = 0.002; Fig. 2c, subpopulation of patients without prevalent osteoporosis-related fractures; mean number of days on ibandronate, 345; mean number of days on alendronate, 329, p < 0.001).
Secondary endpoints
New osteoporosis-related fractures
In the bisphosphonate-naïve patients of the matched pair populations, there was no significant difference in the percentage of patients with new osteoporosis-related fractures of the vertebrae, hip, or forearm, between treatment arms at the end of the study period. However, there were a significantly greater number of patients with any fracture in the alendronate treatment arm (p < 0.05).
Mobility
At the end of the study, a significantly greater increase in mobility was observed in patients in the ibandronate treatment arm compared with those in the alendronate treatment arm, in both the subpopulation of patients with (Fig. 3a, p = 0.0042) and those without prevalent osteoporosis-related fractures (Fig. 3b, p < 0.0001).
Analgesic use
With regard to analgesic use at the end of observation, patients in the ibandronate treatment arm reported a significant decrease in the use of analgesics compared to patients in the alendronate treatment arm, both in the subpopulation of patients with and without prevalent osteoporosis-related fractures (Table 2, p < 0.001).
Adverse events/serious adverse events
Events from four different AE categories and one SAE category were reported in ≥1 % of the overall population, in either treatment arm, Table 3. There were significantly more gastrointestinal disorders in the alendronate treatment arm compared with the ibandronate treatment arm (p < 0.001), while a significantly greater number of general disorders and administration site conditions were reported in the ibandronate treatment arm (p = 0.002).
Discussion
The results of the VIVA study show that, in a real-world setting, patients treated with 3 mg i.v. quarterly ibandronate are significantly more adherent and persistent to medication than patients receiving 70 mg oral alendronate. This may lead to an improvement in pain relief and mobility in women with PMO, in the absence of any unexpected AEs or SAEs. In the large safety population, which included 4,476 patients treated with ibandronate, only 5.3 and 1.4 % of patients reported AEs or SAEs, respectively. Furthermore, no new safety signals were identified.
Poor adherence and persistence to medication are often observed in women with PMO [25]. There can be multiple reasons for this, including patient preference [26], intentional choice, and patient attitudes [27]. Data recently published in the Prospective Observational Scientific Study Investigating Bone Loss Experience (POSSIBLE US) [25] show that a lower treatment satisfaction is associated with an increased risk of discontinuation/switching of anti-osteoporosis medication in women with PMO.
Several studies have shown that persistence with oral bisphosphonates is particularly poor [13, 28], and the situation in Germany is no different. Recent data published from the German retrospective cohort analysis (GRAND) [29] showed inadequate adherence and persistence to oral bisphosphonates in women with osteoporosis. Although the results of the present study show that persistence with ibandronate was significantly greater than with alendronate, persistence was, nonetheless, high in the alendronate treatment arm compared with other studies reported in the literature [13, 28]. We have no explanation to account for this finding. The results of the present study are, however, in line with those published in a recent study which used a large-scale representative German database to analyze adherence and persistence to medication with regard to anti-osteoporotic medication. A greater degree of persistence was observed with i.v. bisphosphonate treatment compared with oral bisphosphonate treatment [30].
This is the first study specifically in patients with PMO to prospectively compare adherence and persistence to i.v. 3 mg ibandronate administered quarterly and oral 70 mg alendronate taken weekly. In addition, this study was conducted in a real-world setting, in the sense that patients were not specifically required to attend follow-up visits over the study period. This is important, because clinical studies sometimes involve patient support programs and physician–patient communication, which may act as contributing factors for increased persistence [31, 32].
With regard to the secondary study endpoints, there was a significant improvement in mobility and pain relief (as indicated by the reduction in analgesic use at the end of the study) in patients in the ibandronate treatment arm compared with patients in the alendronate treatment arm. In the large safety population, only 5.3 and 1.4 % of the 4,476 patients in the ibandronate treatment arm reported AEs or SAEs, respectively, while only 6.6 and 1.1 % of the 1,493 patients in the alendronate treatment arm reported AEs or SAEs, respectively. Furthermore, no new or unexpected safety signals were identified compared with the DIVA study [22] and with the Fracture Intervention Trial and other studies [33–35], with regard to ibandronate and alendronate, respectively.
This study has a number of potential limitations. With regard to the primary endpoints, not all aspects of adherence to medication were assessed, because there was no reliable record of whether the alendronate tablets were taken in accordance with the correct method of administration. Furthermore, in contrast to oral medication, i.v. administration ensures that a full dosage is administered, which may have a positive impact on adherence to medication. It is possible that there may have been a selection bias with respect to the significantly greater number of comorbidities in the ibandronate i.v. treatment arm. It has been reported that some comorbidities increase the severity of osteoporosis [36] and can also adversely affect the management of osteoporosis, because a greater burden of comorbidity has been associated with reduced adherence [37]. It is possible that participants in the ibandronate group may have been more motivated to continue therapy, due to the required interaction with the physician for drug administration. However, the fact that the number of interim visits was similar between both treatment arms reduces the likelihood of this. This study did not have a placebo treatment arm, which does not allow the effective evaluation of the secondary endpoints in terms of efficacy and safety of the two drugs. The non-interventional nature of this study did not allow for measurements of vitamin D levels, which would have revealed important information as to the response to antiresorptives. Finally, the results on pain and mobility may be confounded due to inter- and intraindividual perception of mobility and pain or uncertainty surrounding the type and amount of pain medication.
To date, the VIVA study is the largest non-interventional study performed in women with PMO. The results showed greater adherence and persistence to medication in patients on 3 mg i.v. quarterly ibandronate compared to those on 70 mg oral alendronate taken weekly. Future studies may seek to develop and integrate specific questionnaires, such as the self-reported ADherence Evaluation of OSteoporosis treatment (ADEOS) questionnaire [38] for osteoporotic postmenopausal women, as a tool to further evaluate persistence.
Increased adherence and persistence to medication may lead to a significant improvement in mobility and pain relief, as indicated by the results of this study. Furthermore, the burden [39] currently placed on the German healthcare system by osteoporosis may be lessened, because nonadherence has been associated with an increase in the number of hospitalizations [40] and in medical costs [41].
References
National Osteoporosis Foundation (2003) Physician’s guide to prevention and treatment of osteoporosis. Excerpta Medica, Belle Mead
Sambrook P, Cooper C (2006) Osteoporosis. Lancet 367:2010–2018
Hadji P, Klein S, Gothe H, Häussler B, Kless T, Schmidt T, Steinle T, Verheyen F, Linder R (2013) The epidemiology of osteoporosis—Bone Evaluation Study (BEST): an analysis of routine health insurance data. Dtsch Arztebl Int 110:52–57
Ström O, Borgström F, Kanis JA, Compston J, Cooper C, McCloskey EV, Jönsson B (2012) Osteoporosis: burden, health care provision and opportunities in the EU: a report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 6:59–155
Hooven FH, Adachi JD, Adami S, Boonen S, Compston J, Cooper C, Delmas P, Diez-Perez A, Gehlbach S, Greenspan SL, LaCroix A, Lindsay R, Netelenbos JC, Pfeilschifter J, Roux C, Saag KG, Sambrook P, Silverman S, Siris E, Watts NB, Anderson FA Jr (2009) The Global Longitudinal Study of Osteoporosis in Women (GLOW): rationale and study design. Osteoporos Int 20:1107–1116
Prieto-Alhambra D, Nogues X, Javaid MK, Wyman A, Arden NK, Azagra R, Cooper C, Adachi JD, Boonen S, Chapurlat RD, Compston JE, Gehlbach SH, Greenspan SL, Hooven FH, Netelenbos JC, Pfeilschifter J, Rossini M, Sambrook PN, Silverman S, Siris ES, Watts NB, Díez-Pérez A (2013) An increased rate of falling leads to a rise in fracture risk in postmenopausal women with self-reported osteoarthritis: a prospective multinational cohort study (GLOW). Ann Rheum Dis 72(6):911–7
Rizzoli R (2011) Bisphosphonates for post-menopausal osteoporosis: are they all the same? QJM 104:281–300
Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC, Bauer DC, Genant HK, Haskell WL, Marcus R, Ott SM, Torner JC, Quandt SA, Reiss TF, Ensrud KE (1996) Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet 348:1535–1541
Harris ST, Watts NB, Genant HK, McKeever CD, Hangartner T, Keller M, Chesnut CH 3rd, Brown J, Eriksen EF, Hoseyni MS, Axelrod DW, Miller PD (1999) Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial. Vertebral Efficacy with Risedronate Therapy (VERT) Study Group. JAMA 282:1344–1352
Vrijens B, De Geest S, Hughes DA, Przemyslaw K, Demonceau J, Ruppar T, Dobbels F, Fargher E, Morrison V, Lewek P, Matyjaszczyk M, Mshelia C, Clyne W, Aronson JK, Urquhart J, ABC Project Team (2012) A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol 73:691–705
Caro JJ, Ishak KJ, Huybrechts KF, Raggio G, Naujoks C (2004) The impact of compliance with osteoporosis therapy on fracture rates in actual practice. Osteoporos Int 15:1003–1008
Höer A, Seidlitz C, Gothe H, Schiffhorst G, Olson M, Hadji P, Häussler B (2009) Influence on persistence and adherence with oral bisphosphonates on fracture rates in osteoporosis. Patient Prefer Adherence 3:25–30
Penning-van Beest FJ, Erkens JA, Olson M, Herings RM (2008) Loss of treatment benefit due to low compliance with bisphosphonate therapy. Osteoporos Int 19:511–517
Siris ES, Selby PL, Saag KG, Borgström F, Herings RM, Silverman SL (2009) Impact of osteoporosis treatment adherence on fracture rates in North America and Europe. Am J Med 122(2 Suppl):S3–S13
Silverman SL, Schousboe JT, Gold DT (2011) Oral bisphosphonate compliance and persistence: a matter of choice? Osteoporos Int 22:21–26
Hamilton B, McCoy K, Taggart H (2003) Tolerability and compliance with risedronate in clinical practice. Osteoporos Int 14:259–262
Tosteson AN, Grove MR, Hammond CS, Moncur MM, Ray GT, Hebert GM, Pressman AR, Ettinger B (2003) Early discontinuation of treatment for osteoporosis. Am J Med 115:209–216
Simon JA, Lewiecki EM, Smith ME, Petruschke RA, Wang L, Palmisano JJ (2002) Patient preference for once-weekly alendronate 70 mg versus once-daily alendronate 10 mg: a multicenter, randomized, open-label, crossover study. Clin Ther 24:1871–1886
Thiébaud D, Burckhardt P, Kriegbaum H, Huss H, Mulder H, Juttmann JR, Schöter KH (1997) Three monthly intravenous injections of ibandronate in the treatment of postmenopausal osteoporosis. Am J Med 103:298–307
Adami S, Felsenberg D, Christiansen C, Robinson J, Lorenc RS, Mahoney P, Coutant K, Schimmer RC, Delmas PD (2004) Efficacy and safety of ibandronate given by intravenous injection once every 3 months. Bone 34:881–889
Delmas PD, Adami S, Strugala C, Stakkestad JA, Reginster JY, Felsenberg D, Christiansen C, Civitelli R, Drezner MK, Recker RR, Bolognese M, Hughes C, Masanauskaite D, Ward P, Sambrook P, Reid DM (2006) Intravenous ibandronate injections in postmenopausal women with osteoporosis: one-year results from the dosing intravenous administration study. Arthritis Rheum 54:1838–1846
Eisman JA, Civitelli R, Adami S, Czerwinski E, Recknor C, Prince R, Reginster JY, Zaidi M, Felsenberg D, Hughes C, Mairon N, Masanauskaite D, Reid DM, Delmas PD, Recker RR (2008) Efficacy and tolerability of intravenous ibandronate injections in postmenopausal osteoporosis: 2-year results from the DIVA study. J Rheumatol 35:488–497
Bianchi G, Czerwinski E, Kenwright A, Burdeska A, Recker RR, Felsenberg D (2012) Long-term administration of quarterly IV ibandronate is effective and well tolerated in postmenopausal osteoporosis: 5-year data from the DIVA study long-term extension. Osteoporos Int 23:1769–1778
Feldstein AC, Weycker D, Nichols GA, Oster G, Rosales G, Boardman DL, Perrin N (2009) Effectiveness of bisphosphonate therapy in a community setting. Bone 44:153–159
Barrett-Connor E, Wade SW, Do TP, Satram-Hoang S, Stewart R, Gao G, Macarios D (2012) Treatment satisfaction and persistence among postmenopausal women on osteoporosis medications: 12-month results from POSSIBLE US™. Osteoporos Int 23:733–741
Hadji P, Minne H, Pfeifer M, Bourgeois P, Fardellone P, Licata A, Devas V, Masanauskaite D, Barrett-Connor E (2008) Treatment preference for monthly oral ibandronate and weekly oral alendronate in women with postmenopausal osteoporosis: a randomized, crossover study (BALTO II). Joint Bone Spine 75:303–310
Silverman S, Gold DT (2010) Compliance and persistence with osteoporosis medications: a critical review of the literature. Rev Endocr Metab Disord 11:275–280
Gold DT, Martin BC, Frytak JR, Amonkar MM, Cosman F (2007) A claims database analysis of persistence with alendronate therapy and fracture risk in post-menopausal women with osteoporosis. Curr Med Res Opin 23:585–594
Hadji P, Claus V, Ziller V, Intorcia M, Kostev K, Steinle T (2012) GRAND: the German retrospective cohort analysis on compliance and persistence and the associated risk of fractures in osteoporotic women treated with oral bisphosphonates. Osteoporos Int 23:223–231
Ziller V, Kostev K, Kyvernitakis I, Boeckhoff J, Hadji P (2012) Persistence and compliance of medications used in the treatment of osteoporosis-analysis using a large-scale, representative, longitudinal German database. Int J Clin Pharmacol Ther 50:315–322
Seeman E, Compston J, Adachi J, Brandi ML, Cooper C, Dawson-Hughes B, Jönsson B, Pols H, Cramer JA (2007) Non-compliance: the Achilles’ heel of anti-fracture efficacy. Osteoporos Int 18:711–719
Sarrel PM (1999) Improving adherence to hormone replacement therapy with effective patient-physician communication. Am J Obstet Gynecol 180:S337–S340
Bauer DC, Black D, Ensrud K, Thompson D, Hochberg M, Nevitt M, Musliner T, Freedholm D (2000) Upper gastrointestinal tract safety profile of alendronate: the fracture intervention trial. Arch Intern Med 160:517–525
Greenspan S, Field-Munves E, Tonino R, Smith M, Petruschke R, Wang L, Yates J, de Papp AE, Palmisano J (2002) Tolerability of once-weekly alendronate in patients with osteoporosis: a randomized, double-blind, placebo-controlled study. Mayo Clin Proc 77:1044–1052
Eisman JA, Rizzoli R, Roman-Ivorra J, Lipschitz S, Verbruggen N, Gaines KA, Melton ME (2004) Upper gastrointestinal and overall tolerability of alendronate once weekly in patients with osteoporosis: results of a randomized, double-blind, placebo-controlled study. Curr Med Res Opin 20:699–705
Dennison EM, Compston JE, Flahive J, Siris ES, Gehlbach SH, Adachi JD, Boonen S, Chapurlat R, Díez-Pérez A, Anderson FA Jr, Hooven FH, LaCroix AZ, Lindsay R, Netelenbos JC, Pfeilschifter J, Rossini M, Roux C, Saag KG, Sambrook P, Silverman S, Watts NB, Greenspan SL, Premaor M, Cooper C, Investigators GLOW (2012) Effect of co-morbidities on fracture risk: findings from the Global Longitudinal Study of Osteoporosis in Women (GLOW). Bone 50:1288–1293
Curtis JR, Xi J, Westfall AO, Cheng H, Lyles K, Saag KG, Delzell E (2009) Improving the prediction of medication compliance: the example of bisphosphonates for osteoporosis. Med Care 47:334–341
Breuil V, Cortet B, Cotté FE, Arnould B, Dias-Barbosa C, Gaudin AF, Regnault A, Roborel de Climens A, Legrand E (2012) Validation of the adherence evaluation of osteoporosis treatment (ADEOS) questionnaire for osteoporotic post-menopausal women. Osteoporos Int 23:445–455
Häussler B, Gothe H, Göl D, Glaeske G, Pientka L, Felsenberg D (2007) Epidemiology, treatment and costs of osteoporosis in Germany—the BoneEVA Study. Osteoporos Int 18:77–84
Huybrechts KF, Ishak KJ, Caro JJ (2006) Assessment of compliance with osteoporosis treatment and its consequences in a managed care population. Bone 38:922–928
Sunyecz JA, Mucha L, Baser O, Barr CE, Amonkar MM (2008) Impact of compliance and persistence with bisphosphonate therapy on health care costs and utilization. Osteoporos Int 19:1421–1429
Acknowledgments
This study was funded by Roche Pharma AG, Grenzach-Wyhlen, Germany. The authors thank Dr. A. Defer, Dr. J. Pfeilschifter, and Dr. O. Gröschel for their participation in the study. The authors also thank Dr. M. Hoque from ACUMED for providing medical writing support, funded by Roche.
Conflicts of interest
Peyman Hadji: has received honoraria and research funding from Amgen, Roche, GlaxoSmithKline, Novartis, MSD, Daiichi Sankyo, Pfizer, Procter & Gamble, Eli Lilly, and Nycomed.
Lorenz Hofbauer receives honoraria for lectures and advisory board meetings from Amgen, Merck, and Novartis.
Dieter Felsenberg receives payment for consultancy/advisory boards from Amgen, Chugai Pharmaceutical Co. Ltd., GlaxoSmithKline, Lilly, MSD, Novartis, Nycomed, Roche, Servier, and Teva Pharmaceutical Industries Ltd.; lecture fees from Amgen, Chugai, GE Healthcare, GlaxoSmithKline, Lilly, MSD, Novartis, Nycomed, Roche, Servier, Teva Pharmaceutical Industries Ltd., and Warner Chilcott; and grant support from Amgen, Chugai, Lilly, MSD, Novartis, Nycomed, Roche, Teva Pharmaceutical Industries Ltd., and Servier.
Andreas Kurth is a speaker for Roche and an active member on the advisory board for BonViva; is a speaker for Biomet, DFine Europe, Medtronic, Servier, Novartis, Lilly, Amgen, BMS, GlaxoSmithKline, Baxter, Boehringer Ingelheim, and Anwerina; and is a consultant for DFine Europe, Biomet, Servier, Amgen, Boehringer Ingelheim, and BMS.
Michael Amling is a consultant and speaker for Roche, Novartis, Procter and Gamble, MSD, Servier, and Lilly. No royalties were received.
Julia Annabel Kandenwein is an employee of Roche Pharma Germany.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hadji, P., Felsenberg, D., Amling, M. et al. The non-interventional BonViva Intravenous Versus Alendronate (VIVA) study: real-world adherence and persistence to medication, efficacy, and safety, in patients with postmenopausal osteoporosis. Osteoporos Int 25, 339–347 (2014). https://doi.org/10.1007/s00198-013-2515-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-013-2515-2