Abstract
Summary
Fractures are common in chronic kidney disease (CKD). We determined if bone mineral density testing by dual energy X-ray absorptiometry (DXA) and high resolution peripheral quantitative computed tomography (HR pQCT) could discriminate fracture status in CKD patients. Both tests were able to discriminate fracture status. Further, the addition of HR pQCT measurements to DXA measurements did not improve fracture discrimination.
Introduction
The optimal method to identify individuals with CKD at high fracture risk is unknown.
Methods
We determined if bone mineral density (BMD) by DXA and HR pQCT could discriminate fracture status in 211 adult men and women with stages 3 to 5 CKD, attending predialysis clinics in Toronto Canada, using logistic regression. Results are expressed as the odds ratio (OR) of fracture (prevalent vertebral and/or low trauma since age 40 years) per standard deviation decrease in the predictor adjusted for age, weight, sex, and CKD stage. We constructed receiver operating characteristic curves to examine the discriminative ability of BMD measures for fracture.
Results
Most participants were Caucasian men with a mean age of 63.3 ± 15.5 years. There were 77 fractures in 74 participants. Decreases in BMD were associated with increased fracture risk: OR = 1.56 (95% confidence interval (CI), 1.41 to 1.71) for BMD by DXA at the ultradistal radius, and OR = 1.24 (95% CI, 1.12 to 1.36) for cortical area by HR pQCT. Further, while both tests were able to discriminate fracture status, the addition of HR pQCT measures to BMD by DXA did not improve fracture discrimination ability.
Conclusions
Among CKD patients not yet requiring renal replacement therapy, BMD by DXA is able to discriminate fracture status.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fractures are common in patients with chronic kidney disease (CKD) and associated with substantial morbidity and mortality [1]. One way to decrease the adverse outcomes associated with fractures in patients with CKD is to identify those at high risk and target treatments to this group.
To date, studies have focused on the association between fracture and bone mineral density (BMD) by dual energy X-ray absorptiometry (DXA) and peripheral quantitative computed tomography (pQCT) in patients with stage 5 CKD on dialysis (5D CKD) largely due to the substantial fracture burden in this population. Overall, these studies suggest that BMD by DXA, while slightly lower in those with fracture than those without, is not able to discriminate fracture status in patients with stage 5D CKD. In contrast, cortical—but not trabecular bone—measures by conventional and high resolution (HR) pQCT are strongly associated with fractures in these patients [2–13].
It is important to note that fractures are not limited to patients with stage 5D CKD. Data obtained as part of the Third National Health and Nutrition Examination Survey (NHANES) reported an approximate twofold increase risk of hip fracture among those with an estimated glomerular filtration rate (eGFR) <60 ml/min, compared to those with an eGFR ≥ 60 ml/min [14]. Data from the Study of Osteoporotic Fractures found that fracture risk increased with worsening of renal function such that compared to women with an eGFR ≥ 60 ml/min, hip fracture risk was increased by 1.5-fold among those with an eGFR between 45 to 50 ml/min and was doubled among women with an eGFR < 45 ml/min [15]. Further, 26 million North Americans (13% of the population) are affected by CKD [16]. As such, the burden of illness due to fractures is largely a result of the fractures that occur before stage 5 CKD. Only one study has reported on fracture risk assessment in patients with early stages of CKD [10]. A positive association was found between fractures and HR pQCT (radius and tibia) and DXA (hip, spine, and radius). However, the relative contributions of DXA and HR pQCT to fracture was not examined—a clinically important point as very few health care facilities have access to HR pQCT. Further, the generalizability of this study is limited by the small sample size (32 with fractures and 59 without).
The purpose of our study was to assess the relative contributions of DXA and HR pQCT measurements to fracture risk among patients with stages 3 to 5 CKD. We hypothesized that both DXA and HR pQCT would be associated with fracture and that the addition of HR pQCT measurements to DXA would not improve the discriminative ability of DXA.
Methods
Study participants
We enrolled 211 subjects over 30 months from three predialysis clinics in Toronto, Canada. These tertiary care clinics aim to provide multidisciplinary care to optimize patient health while progressing through the stages of CKD.
We included men and women 18 years of age and older with a Modification of Diet in Renal Disease short formula-derived eGFR of <60 ml/min and classified subjects by stage of CKD according to the National Kidney Foundation Guidelines [17]. Specifically: stage 3 CKD (mild): eGFR = 30–59 ml/min, stage 4 CKD (severe): eGFR = 15–29 ml/min, and stage 5 CKD (kidney failure): eGFR < 15 ml/min. We excluded dialysis patients, patients with prior renal transplants, those taking bisphosphonate therapy or calcitonin, and women taking hormone replacement therapy and/or the oral contraceptive pill. Radiographs, BMD measurements by DXA and HR pQCT were obtained at a single study site. All participants gave written informed consent. The study was approved by the appropriate institutional review boards.
Interviewer-administered questionnaire
Participants were interviewed by a research coordinator about age, race, current alcohol and caffeine consumption, current smoking, physical activity, and family history of osteoporosis (fractures in a first-degree relative). We inquired about a history of fractures since age 40, falls in the past 12 months, and the presence of diabetes. The questionnaire has been used in several populations, including patients with stage 5 CKD [4, 12].
Chart review
We confirmed the cause and duration of CKD by chart review. Patients attending the predialysis clinics have blood taken for serum calcium, phosphate, creatinine, alkaline phosphatase, 25-hydroxy-vitamin D (25(OH) D3), and intact parathyroid hormone (PTH) on a regular basis; timing of the blood work required by the study protocol was designed to align with that obtained for clinical purposes. All tests were performed by a single, central laboratory using standardized methods and reference ranges were determined from this laboratory’s data (The University Health Network). We analyzed values obtained within 1 month before or after the BMD measurements.
Low-trauma fractures
We inquired about fractures since age 40 and classified fractures as low-trauma or traumatic according to the World Health Organization definition [18]. We included only low-trauma fractures defined as fractures that occur from minimal trauma, such as a fall from a standing height or less, in our analyses. We excluded fractures of the fingers, toes, patella, and skull. We confirmed all self-reported low-trauma fractures by review of radiographs or radiology reports.
Prevalent vertebral fractures
We obtained anteroposterior and lateral radiographs of the thoracic and lumbar spine and identified fractures by quantitative morphometry. Our primary definition of a prevalent fracture was defined as a decrease of at least 20% and 4 mm or greater in any vertical dimension compared with the vertebra above or below one or more thoracic and lumbar vertebrae [19]. We also examined fracture severity using a previously described semiquantitative grading scale—where mild deformity is classified as a 20–25% height loss (anterior, middle, and/or posterior relative to adjacent vertebrae); moderate a 25–40% height loss, and severe >40% height loss [20]. Films were interpreted by two experienced radiologists, blinded to the clinical history and results of BMD testing. Differences in fracture classification were resolved by consensus.
HR pQCT measurements
We obtained HR pQCT measurements at the non-dominant distal radius (non-weight bearing site) using the Xtreme CT device (Scanco Medical AG, Basserdorf, Switzerland) at the University of Toronto Centre of Excellence in Skeletal Health Assessment. Measurements were performed by trained technologists who were blinded to the study hypotheses and were not involved in patient care. Distal radial measurements were obtained according to manufacturer's standard protocol. Briefly, to obtain distal radial measurements, a reference line was set manually at the endplate of the radius on an anteroposterior scout view. The region of interest (a 9-mm stack of 110 slices) was identified automatically at a set distance from this reference line. Measurements obtained from HR pQCT include: total volumetric bone mineral density, total area, cortical area and trabecular area, cortical volumetric bone mineral density, trabecular volumetric bone mineral density, cortical thickness, trabecular separation, and trabecular thickness. The reproducibility (root-mean-square coefficient of variation) for density measurements at the distal radius are from 0.46% to 0.70%. To calculate this, 31 individuals (25 women, 6 men; mean age 44.2 years, range 20–69) with various densities were scanned at the distal radius according to standard protocol by one operator. They were repositioned and rescanned by the same operator later the same day.
BMD by DXA
We assessed BMD at the lumbar spine (L1–L4), total hip, and the non-dominant ultradistal and 1/3 radius using one Hologic Discovery A densitometer (Hologic Inc, Waltham, MA, USA). Tests were performed by one of two International Society of Clinical Densitometry certified technologists not involved in the care of study participants, and blinded to our study hypotheses. The short-term in vivo precision (root-mean-square coefficient of variation) is: 1.01% at the total lumbar spine (L1 to L4), 1.08% at the total hip, and 1.5% for the distal radius.
Outcomes
Fractures were classified as follows: (1) prevalent vertebral fractures by spinal radiographs and/or a clinical spine fracture; (2) a history of a nonspine fracture since age 40 years; and (3) either of the first two classifications.
Statistical analyses
We used bivariate analyses (t test, chi-squared or Fisher's exact test, as appropriate) to examine differences in demographic and lifestyle factors, medical history, cause of CKD, serum markers of mineral metabolism, and duration of CKD by fracture. We used logistic regression to examine the associations between fractures and radiographic measurements: BMD at the lumbar spine (L1–L4), total hip, 1/3 and ultradistal radius, and HR pQCT measures (total volumetric BMD, total area, cortical density, cortical area, cortical thickness, trabecular area, trabecular density, trabecular separation, and trabecular thickness). We considered HR pQCT measures that have been previously reported to be associated with fractures in patients with and without CKD [10, 12, 21, 22]. We considered each predictor as a continuous variable and adjusted our analyses for age, weight, sex, and stage of CKD. Results are expressed as the odds ratio of fracture per standard deviation decrease in the predictor.
To examine the discriminative ability of these tests by fracture status, we constructed receiver operating characteristic (ROC) curves for each predictor variable. We compared the area under the ROC curves (AUC) for each DXA and HR pQCT measurement using a chi-squared test [23, 24]. To compare the predictive value of DXA alone to the predictive value of DXA and HR pQCT to discriminate fracture status, we considered the fact that BMD by DXA is a composite measure reflecting both projected area and bone mineral content and that a similar comparator for HR pQCT would be total volumetric BMD and cortical thickness. We then derived a logistic model using BMD by DXA at the ultradistal radius, total volumetric BMD, and cortical thickness by HR pQCT at the radius and compared the linear predictor from this model to the logistic model derived from using BMD by DXA at the ultradistal radius alone. Analyses were performed with STATA Version 11.0 (STATA Corp., College Station, TX, USA). Statistical tests were considered significant at a two-tailed level of 0.05 and were not adjusted for multiple comparisons.
Results
Characteristics of study population
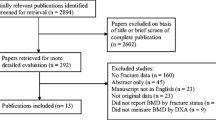
We identified 432 eligible patients by chart review. Of these, 221 did not wish to participate (the most common reasons being that they were “too busy” or had difficulty obtaining transportation). Of those who declined, 200 (90%) allowed us to conduct a chart review to compare demographic characteristics of nonparticipants and participants. Patients who declined to participate were more often women (120 of 200; 60%), than those who agreed (86 of 211; 40%; p < 0.001), but there were no other significant differences. Most of our 211 consented participants were Caucasian men with a mean age of 63.3 ± 15.5 years, a mean duration of CKD of 96.7 ± 125.3 months, and roughly one third had CKD attributed to diabetic nephropathy. The proportions of participants were approximately equally divided between CKD stages 3, 4, and 5. Compared to participants without fractures, those with fractures were older (61 vs. 68 years; p = 0.03), weighed less (81 vs. 75 kg; p = 0.05), had a higher level of serum PTH (22 vs. 40 pmol/L; p = 0.002), were less likely to be in stage 3 CKD (39% vs. 16%; p < 0.0001), and reported falling more frequently in the past year (22% vs. 54%; p < 0.001) (Table 1). In all participants, serum calcium was in the normal range (normal range 2.20 to 2.62 mmol/L), as was alkaline phosphatase (normal range ≤ 110 U/L), phosphate was slightly elevated (normal range 0.8 to 1.35 mmol/L), 25(OH) D3 was in the suboptimal range (defined as 25 to 75 nmol/L), and serum PTH was elevated (normal range 1.6 to 6.9 pmol/L).
When we examined markers of mineral metabolism by stage of CKD and fracture status, we found that serum calcium and alkaline phosphatase were in the normal range regardless of CKD stage and/or fracture status. Phosphate was in the normal range in stage 3 CKD and in stage 4 CKD without fractures. Phosphate was above the normal range in stage 4 CKD with fractures and in stage 5 CKD regardless of fracture status. Further, phosphate was higher in stage 5 CKD with fractures compared to those without (p = 0.04). Vitamin D was in the suboptimal range for all subjects except those with stage 3 CKD without fractures. Further, vitamin D decreased with increasing stage of CKD (test for trend = 0.05). Serum PTH was elevated in all stages of CKD regardless of fracture status—higher in patients with fractures compared to those without in each stage of CKD (p < 0.01 for all comparisons), and increased with declining renal function (test for trend p = 0.02) (Table 2).
There were 77 fractures in 74 participants: 41 participants had prevalent spine fractures and 2 had clinical spine fractures; 34 self-reported low-trauma fractures (15 wrist, 5 rib, 3 humerus, 2 hip, 1 clavicle, 1 sacrum, 1 pelvis, and 6 ankle) since age 40 years and 3 participants had both a prevalent spine fracture and another low-trauma fracture. Of the 41 prevalent spine fractures, 21 were classified as mild, 19 moderate, and 1 severe.
Association between HR pQCT measures, DXA, and fractures
All measures of BMD by DXA were statistically significantly higher in patients without fractures compared to those with fractures. With regards to HR pQCT: trabecular separation was statistically significantly lower in those without fractures (by self report and/or prevalent vertebral fractures) compared to those with fractures; trabecular thickness, total and trabecular area were not statistically significantly different by fracture status; the remainder of the HR pQCT measures were statistically significantly higher in those without fractures compared to those with fractures. Serum PTH was inversely correlated with all cortical measures by HR pQCT (r ranged from 0.4 to 0.67) and not correlated with trabecular measures (r ranged from 0.1 to 0.23). Results were similar and statistical significance was unchanged when we considered prevalent vertebral fractures and self-reported fractures separately (Table 3).
After adjusting for age, weight, sex and stage of CKD, we found that each standard deviation decrease in BMD by DXA at the total hip, lumbar spine, ultradistal, and 1/3 radius was associated with an increased risk of fracture (by self report and/or prevalent vertebral fracture). Similarly, decreases in total volumetric BMD, total area, cortical area, cortical density, trabecular density, trabecular thickness, and cortical thickness by HR pQCT were associated with an increased fracture risk while an increase in trabecular separation was associated with an increase in fracture risk. Trabecular area by HR pQCT was not significantly associated with fracture risk. Results were similar and statistical significance remained unchanged when we considered prevalent vertebral fractures and self-reported fractures separately for all measures except cortical density, cortical thickness, and trabecular thickness which did not reach statistical significance (Table 4).
ROC curves confirmed that BMD testing by DXA and HR pQCT measures (except trabecular area) at all sites was able to discriminate among participants with and without fractures (Table 4). The greatest area under the ROC curve was obtained for BMD by DXA at the ultradistal radius (AUC: 0.80; 95% confidence interval 0.74 to 0.87) which was statistically significantly greater than all other measures (p < 0.001 for all comparisons). Among HR pQCT measures, with the exception of trabecular thickness, cortical measures were associated with statistically significantly greater AUC’s compared with trabecular measures (p < 0.003 for all comparisons).
We also examined the effect of combining BMD by DXA at the ultradistal radius measure together with a composite measure of HR pQCT, specifically total volumetric BMD and cortical thickness, to determine if the addition of HR pQCT to BMD by DXA could improve fracture discrimination. When the composite HR pQCT measure was added to the BMD by DXA at the ultradistal radius, the AUC was 0.81 (95% CI 0.74 to 0.88). However, this AUC was not significantly different than BMD by DXA at ultradistal radius alone (AUC 0.80; 95%CI 0.74 to 0.87; p = 0.37) (Fig. 1).
Discussion
We found that both BMD by DXA and HR pQCT parameters are associated with fractures among men and women with stages 3 to 5 CKD. In our study population, the measure that was best able to discriminate between fractured and nonfractured patients was BMD by DXA at the ultradistal radius with an AUC of 0.80. This measure was better than any HR pQCT measures and the addition of any of the HR pQCT measures to BMD by DXA at the ultradistal radius did not improve fracture discrimination. This has important clinical implications—the 26 million North Americans with stages 3 to 5 CKD not on dialysis and at high fracture risk can be identified by BMD testing with DXA; the ultradistal radius being the preferred site.
The performance test characteristics of both DXA and HR pQCT measures in our study are similar to those previously reported by a single smaller study of CKD patients not on dialysis [10]. That study, which enrolled 32 patients with fractures and 59 without, also reported that areal BMD by DXA and total volumetric BMD by HR pQCT were both associated with fracture; however, they did not formally compare DXA measures to HR pQCT measures. Of note, both in this small CKD study and in our current study, DXA and HR pQCT were associated with fracture even when bone mass measurements were obtained after the fracture occurred.
The fact that BMD testing with DXA can be used in stages 3 to 5 CKD to assess fracture risk is consistent with what has been reported in an analysis using data from the Study of Osteoporotic Fractures which demonstrated that among women with moderate to severe CKD, femoral neck BMD independently contributed to the risk of hip and spine fracture [15]. In addition, randomized trials of alendronate, risedronate, raloxifene, denosumab, and teriparatide for the prevention of osteoporotic fractures enrolled some patients who had markers of mineral metabolism and serum creatinine in the normal range but estimated creatinine clearances in the range of 15 to 60 ml/min (stages 3 and 4 CKD) and BMD by DXA was able to predict fracture risk in these patients [25–28].
With the exception of trabecular thickness, compared to cortical measures, the AUC’s for trabecular measures by HR pQCT were lower indicating poorer discriminative ability. Indeed, the AUC for trabecular area was 0.52 (95% CI 0.38 to 0.59). One potential explanation for this finding is that in early stages of CKD, before dialysis, the adverse bone effects are primarily due to excess PTH [29]. Histomorphometric studies demonstrate that hyperparathyroidism preferentially affects cortical bone, resulting in subperiosteal resorption (reflected by a decrease in cortical area) and intracortical porosity (reflected by a decrease in cortical density) [30]. In keeping with these findings, we found that serum PTH was weakly correlated with all our cortical measures.
Our findings are different than what we and others have reported in stage 5D CKD. In the dialysis population, cortical pQCT measures are strongly associated with fractures but there is no association between BMD by DXA or trabecular measures by HR pQCT and fractures [4, 6, 12]. These divergent findings are consistent with the concept that the type of bone disease differs by stage of CKD. In early stages (stages 3, 4, and early stage 5-predialysis), the predominant form of bone disease is hyperparathyroid bone disease which is associated with decreases in BMD preferentially at cortical sites, while in later stages (late stage 5 and dialysis), adynamic bone disease, osteomalacia and mixed renal osteodystrophy become more prevalent [29, 31]. These latter forms of renal osteodystrophy, which increase fracture risk, may or may not be associated with alterations in BMD by DXA, limiting the diagnostic utility of this test in dialysis patients.
Our study had some limitations. Our data were cross-sectional and as such we cannot comment on the ability of BMD testing by DXA or HR pQCT parameters to prospectively identify patients with CKD who will have fracture. Also, due to the cross-sectional design, we could not evaluate the influence that progression of renal disease has on these bone measures. We did not perform bone biopsies and as such are unable to directly determine the effects of PTH on cortical and trabecular bone parameters. While this is the largest cross-sectional study of bone mass measures in CKD stages 3 to 5, there were only 77 fractures limiting our ability to perform subanalyses by stage and type of fracture and/or by severity of vertebral fracture. Most of our subjects were Caucasian men which limits the application of our findings to women and other races. Finally and perhaps most importantly, the participants in our study were active, with very minimal abnormalities of serum calcium, phosphate, PTH, and 25(OH) D3 limiting the generalizability of our findings to patients that are less active and have greater disturbances of mineral metabolism.
It is important to note that the paucity of mineral abnormalities in our participants likely means that for the most part they did not have CKD-MBD. Our findings, specifically that BMD testing might be meaningful in these patients, is not out of keeping with the 2009 Kidney Disease Improving Global Outcomes Clinical Practice Guideline for the Diagnosis, Evaluation, and Treatment of CKD–Mineral and Bone Disorder (CKD-MBD) which indicate that BMD testing should not be performed in patients with stages 3-5D with evidence of CKD-MBD [32].
In summary, we found that in patients with stages 3 to 5 CKD, BMD testing by DXA is able to discriminate well among those with or without fractures. Further, the addition of HR pQCT measures to BMD by DXA does not improve fracture discrimination.
References
Lindberg JS, Moe SM (1999) Osteoporosis in end-state renal disease. Semin Nephrol 19:115–122
Yamaguchi T, Kanno E, Tsubota J, Shiomi T, Nakai M, Hattori S (1996) Retrospective study on the usefulness of radius and lumbar bone density in the separation of hemodialysis patients with fractures from those without fractures. Bone 19:549–555
Fontaine MA, Albert A, Dubois B, Saint-Remy A, Rorive G (2000) Fracture and bone mineral density in hemodialysis patients. Clin Nephrol 54:218–226
Jamal S, Chase C, Goh Y, Richardson R, Hawker G (2002) Bone density and heel ultrasound testing do not identify patients with dialysis-dependent renal failure who have had fractures. Am J Kidney Dis 39:843–849
Kaji H, Suzuki M, Yano S, Sugimoto T, Chihara K, Hattori S, Sekita K (2002) Risk factors for hip fracture in hemodialysis patients. Am J Nephrol 22:325–331
Jamal SA, Hayden JA, Beyene J (2007) Low bone mineral density and fractures in long-term hemodialysis patients: a meta-analysis. Am J Kidney Dis 49:674–681
Dolgos S, Hartmann A, Bonsnes S, Ueland T, Isaksen GA, Godang K, Pfeffer P, Bollerslev J (2008) Determinants of bone mass in end-stage renal failure patients at the time of kidney transplantation. Clin Transplant 22:462–468
Elder GJ, Mackun K (2006) 25-Hydroxyvitamin D deficiency and diabetes predict reduced BMD in patients with chronic kidney disease. J Bone Miner Res 21:1778–1784
Ersoy FF, Passadakis SP, Tam P, Memmos ED, Katopodis PK, Ozener C, Akcicek F, Camsari T, Ates K, Ataman R, Vlachojannis JG, Dombros AN, Utas C, Akpolat T, Bozfakioglu S, Wu G, Karayaylali I, Arinsoy T, Stathakis PC, Yavuz M, Tsakiris JD, Dimitriades CA, Yilmaz ME, Gultekin M, Karayalcin B, Yardimsever M, Oreopoulos DG (2006) Bone mineral density and its correlation with clinical and laboratory factors in chronic peritoneal dialysis patients. J Bone Miner Metab 24:79–86
Nickolas TL, Stein E, Cohen A, Thomas V, Staron RB, McMahon DJ, Leonard MB, Shane E (2010) Bone mass and microarchitecture in CKD patients with fracture. J Am Soc Nephrol 21:1371-1380.
Russo CR, Taccetti G, Caneva P, Mannarino A, Maranghi P, Ricca M (1998) Volumetric bone density and geometry assessed by peripheral quantitative computed tomography in uremic patients on maintenance hemodialysis. Osteoporos Int 8:443–448
Jamal SA, Gilbert J, Gordon C, Bauer DC (2006) Cortical PQCT measures are associated with fractures in dialysis patients. J Bone Miner Res 21:543–548
Hasegawa K, Hasegawa Y, Nagano A (2004) Estimation of bone mineral density and architectural parameters of the distal radius in hemodialysis patients using peripheral quantitative computed tomography. J Biomech 37:751–756
Nickolas TL, McMahon DJ, Shane E (2006) Relationship between moderate to severe kidney disease and hip fracture in the United States. J Am Soc Nephrol 17:3223–3232
Ensrud KE, Lui LY, Taylor BC, Ishani A, Shlipak MG, Stone KL, Cauley JA, Jamal SA, Antoniucci DM, Cummings SR (2007) Renal function and risk of hip and vertebral fractures in older women. Arch Intern Med 167:133–139
Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, Van Lente F, Levey AS (2007) Prevalence of chronic kidney disease in the United States. JAMA 298:2038–2047
(2002) K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 39:S1-266.
(1994) Assessment of osteoporotic fracture risk and its role in screening for postmenopausal osteoporosis. WHO Technical Series, Geneva.
Black DM, Palermo L, Nevitt MC, Genant HK, Christensen L, Cummings SR (1999) Defining incident vertebral deformity: a prospective comparison of several approaches. The study of Osteoporotic Fractures Research Group. J Bone Miner Res 14:90–101
Genant HK, Jergas M, Palermo L, Nevitt M, Valentin RS, Black D, Cummings SR (1996) Comparison of semiquantitative visual and quantitative morphometric assessment of prevalent and incident vertebral fractures in osteoporosis. The Study of Osteoporotic Fractures Research Group. J Bone Miner Res 11:984–996
Boutroy S, Bouxsein ML, Munoz F, Delmas PD (2005) In vivo assessment of trabecular bone microarchitecture by high-resolution peripheral quantitative computed tomography. J Clin Endocrinol Metab 90:6508–6515
Vico L, Zouch M, Amirouche A, Frere D, Laroche N, Koller B, Laib A, Thomas T, Alexandre C (2008) High-resolution pQCT analysis at the distal radius and tibia discriminates patients with recent wrist and femoral neck fractures. J Bone Miner Res 23:1741–1750
Hanley JA, McNeil BJ (1983) A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology 148:839–843
McClish DK (1987) Comparing the areas under more than two independent ROC curves. Med Decis Making 7:149–155
Miller PD, Roux C, Boonen S, Barton IP, Dunlap LE, Burgio DE (2005) Safety and efficacy of risedronate in patients with age-related reduced renal function as estimated by the Cockcroft and Gault method: a pooled analysis of nine clinical trials. J Bone Miner Res 20:2105–2115
Jamal SA, Bauer DC, Ensrud KE, Cauley JA, Hochberg M, Ishani A, Cummings SR (2007) Alendronate treatment in women with normal to severely impaired renal function: an analysis of the fracture intervention trial. J Bone Miner Res 22:503–508
Ishani A, Blackwell T, Jamal SA, Cummings SR, Ensrud KE (2008) The effect of raloxifene treatment in postmenopausal women with CKD. J Am Soc Nephrol 19:1430–1438
Miller PD, Schwartz EN, Chen P, Misurski DA, Krege JH (2007) Teriparatide in postmenopausal women with osteoporosis and mild or moderate renal impairment. Osteoporos Int 18:59–68
Miller PD (2009) Diagnosis and treatment of osteoporosis in chronic renal disease. Semin Nephrol 29:144–155
Duan Y, De Luca V, Seeman E (1999) Parathyroid hormone deficiency and excess: similar effects on trabecular bone but differing effects on cortical bone. J Clin Endocrinol Metab 84:718–722
Elder G (2002) Pathophysiology and recent advances in the management of renal osteodystrophy. Bone and Mineral Research 17:2094–2105
(2009) KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD). Kidney International S1-130.
Acknowledgments
The authors would like to thank Paul Miller for his careful review of this manuscript. Funding was provided by the Canadian Institutes of Health Research (FRN: 93785), the Physicians Services Incorporated Foundation, and The Kidney Foundation of Canada. Some results of this study were presented in abstract format at the 2010 ASN Renal Week and in abstract format at the 2010 and 2011 American Society for Bone and Mineral Research Annual Meeting.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jamal, S.A., Cheung, A.M., West, S.L. et al. Bone mineral density by DXA and HR pQCT can discriminate fracture status in men and women with stages 3 to 5 chronic kidney disease. Osteoporos Int 23, 2805–2813 (2012). https://doi.org/10.1007/s00198-012-1908-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-012-1908-y