Abstract
Summary
Using combined dual-energy X-ray absorptiometry (DXA) and quantitative computed tomography, we demonstrate that men matched with women for femoral neck (FN) areal bone mineral density (aBMD) have lower volumetric BMD (vBMD), higher bone cross-sectional area, and relatively similar values for finite element (FE)-derived bone strength.
Introduction
aBMD by DXA is widely used to identify patients at risk for osteoporotic fractures. aBMD is influenced by bone size (i.e., matched for vBMD, larger bones have higher aBMD), and increasing evidence indicates that absolute aBMD predicts a similar risk of fracture in men and women. Thus, we sought to define the relationships between FN aBMD (assessed by DXA) and vBMD, bone size, and FE-derived femoral strength obtained from quantitative computed tomography scans in men versus women.
Methods
We studied men and women aged 40 to 90 years and not on osteoporosis medications.
Results
In 114 men and 114 women matched for FN aBMD, FN total cross-sectional area was 38% higher (P < 0.0001) and vBMD was 16% lower (P < 0.0001) in the men. FE models constructed in a subset of 28 women and 28 men matched for FN aBMD showed relatively similar values for bone strength and the load-to-strength ratio in the two groups.
Conclusions
In this cohort of young and old men and women from Rochester, MN, USA who are matched by FN aBMD, because of the offsetting effects of bone size and vBMD, femoral strength and the load-to-strength ratio tended to be relatively similar across the sexes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Dual-energy X-ray absorptiometry (DXA) is an excellent clinical tool for the diagnosis and management of osteoporosis [1]. Despite its clinical utility, however, DXA does have some limitations. Specifically, it is influenced by bone size; thus, bones with identical volumetric bone mineral density (vBMD), but differing in size, will have different areal BMD (aBMD) values, with the larger bone having a greater aBMD. This effect of bone size is the key reason men have higher aBMD values than women at all skeletal sites, despite similar (or lower) vBMD values [2, 3].
While osteoporosis was originally defined in women, relative to young normal women (the “young reference value”), as a T-score of ≤−2.5 (i.e., aBMD 2.5 standard deviations or more below the mean of young normal women) [4], the extension of this definition to men has been controversial [2, 5]. By analogy with the definition used for women, osteoporosis in men has often been defined on the basis of T-scores that use gender-specific reference values. However, some data indicate that fracture risk depends on the absolute level of aBMD [6], leading to the recommendation that the same young reference value (i.e., that for women) should also be used to diagnose osteoporosis in men [7–9]. In fact, the current World Health Organization fracture risk assessment tool (FRAX) requires the use of female-referenced femoral neck (FN) aBMD in both sexes for estimating 10-year fracture risks [10], with the assumption that for a given FN aBMD, fracture risk is similar in men and women. If fracture risk is directly related to the strength of the proximal femur, then this assumption suggests that the relation between FN aBMD and femoral strength may be similar in men and women.
To gain mechanistic insight into whether sex-specific young reference values should be used in assessment of fracture risk, we used FN aBMD assessed by DXA, vBMD, and bone geometrical parameters at the FN assessed by quantitative computed tomography (QCT) and femoral strength estimated from the QCT images using finite element (FE) models [11–15] to define, in a population-based sample of men and women, the gender-specific interrelationships among FN aBMD, vBMD, bone size, and FE-derived femoral strength.
Methods
Study subjects
We recruited subjects from an age-stratified, random sample of Rochester, MN, USA residents who were selected using the medical records linkage system of the Rochester Epidemiology Project [16]. This community is highly characteristic of the US White population but underrepresented with respect to Blacks, Hispanics, and Asians. Reflecting the ethnic composition of the community, 96% of the men and 99% of the women were White. The sample spanned ages from 27 to 95 years and included 215 women and 182 men; since FRAX is applicable to men and women aged 40 to 90 years, we used the 192 women and 156 men in this age range from this cohort for analysis. In addition, since FRAX is not applicable to patients being treated for osteoporosis, we excluded subjects on estrogen therapy, bisphosphonates, or selective estrogen receptor modulators; none were on therapy with teriparatide. This resulted in a final cohort for analysis of 136 women and 146 men. All subjects had QCT scans of the proximal femur (see below) and had aBMD assessed by DXA.
QCT of the proximal femur
As previously described for this cohort [3], single energy scans were made at the proximal femur with a multi-detector CT scanner. For the analysis of the scan images, we assessed a single reformatted oblique section contiguous at the midportion of and orthogonal to the FN, between the superior aspect of the head of the femur and the inferior aspect of the inferior trochanter. For all scanning sites, slice width was 2.5 mm and the in-plane voxel size was 0.74 mm. Calibration standards scanned with the patient were used to convert CT numbers directly to equivalent vBMD in milligrams per cubic centimeter [17]. To validate our image processing algorithm, we made ten scans of the European Spine Phantom (ESP), which is composed of hydroxyapatite [18]. The correlation between bone density results determined by our algorithm and that of the ESP was 0.998.
To study age- and sex-specific changes in bone mineral distribution, we developed software for the analysis of bone structure, geometry, and volumetric density from the CT images [19]. The CT data are treated as a 3D volume and reformatted in an orientation that is perpendicular to the primary loading forces on the bone in the region of interest. On this plane, the software program automatically places a single image line that extends from the centroid of the bone to outside the periosteal surface, and this line is then rotated about its centroid end in 3-degree increments. From the range of gray levels in the image, the cortex is identified as the maximal brightness found on this line. The full-width half-maximal points on either side of this maximum are interpreted as the periosteal and endocortical boundaries of the cortex. The resulting points are joined to create 2D cortical and subcortical regions. The vBMD and area of the two regions are measured independently, and a circular central trabecular region is also measured. The FN total cross-sectional area is also derived from this analysis as the area within the periosteal boundary as identified above.
DXA analysis
aBMD of the FN was obtained using the Lunar Prodigy (GE Medical Systems), with a coefficient of variation <1%.
FE estimates of proximal femoral strength
This was assessed in a subset of 28 men and 28 women who were randomly sampled from the larger group. The details of the finite element modeling are described elsewhere [12, 13]. Briefly, each QCT image was rotated into a standard orientation to simulate the femoral position at impact for a sideways fall. Each image voxel was resampled and converted into a 1.5-mm cube eight-noded finite element, and material properties for cortical or trabecular bone were assigned to each element using calibrated QCT density information and empirical relations between measured bone density and tissue mechanical properties [20–22], using lower strengths for tension than compression [23, 24]. Loads and boundary conditions were then applied to simulate a sideways fall. This technique has provided strong Y = X type correlations between measurements of femoral strength in elderly cadaver femora loaded in a similar sideways fall configuration (n = 76, R = 0.88) [25], and others using similar techniques have also found consistently strong correlations [14, 15]. Further, the finite element technique, as implemented in this study, was highly predictive of new hip fractures in a prospective, blinded analysis of hip fracture in elderly men [13].
Estimation of fall loads and the load-to-strength ratio (Φ)
We calculated the load-to-strength ratio for a simulated sideways fall and impact directly on the greater trochanter. The “load” is an estimate of the impact force during a sideways fall, and the “strength” is the FE-derived estimate of the femoral strength for such a fall. Higher values of the load-to-strength ratio (Φ) place an individual at higher risk of hip fracture [26]. As described in more detail elsewhere [13],we calculated the in vivo impact force on the side of the trochanter for each subject using biomechanical theory [27, 28] and patient-specific weight and height information. A uniform value of trochanteric soft tissue thickness of 25 mm was assumed for all subjects, both men and women, since patient-specific measures of soft tissue thickness were not measured from the QCT scans for this study.
Statistical analysis
Variables were summarized using means and standard deviations (SD). The Pearson correlation coefficient was used to compare continuous variables, and the unpaired t test was used in analyses B and C to test for similarities between males and females. In analysis A, linear regression models were used to test for gender differences in vBMD and bone size after adjusting for aBMD and age. Model assumptions, including normality, were checked.
Results
We initially used the entire set of 282 scans available for analysis. Table 1 (analysis A) shows the clinical characteristics of the subjects. The men and women were similar in age and BMI, but the men were taller and weighed more than the women. We adjusted for FN aBMD and age, and then compared FN total cross-sectional area and vBMD (total, trabecular, and cortical) in men versus women. As shown in Table 2, this analysis demonstrated that following adjustment for aBMD and age, male sex had a positive parameter estimate for FN total cross-sectional area (larger area). For FN total, trabecular, and cortical vBMD, following adjustment for aBMD and age, male sex had a negative parameter estimate (lower vBMD values). Thus, following adjustment for FN aBMD and age, men had larger bones and lower vBMD as compared with women.
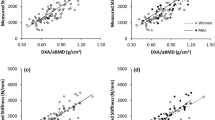
In analysis B, we next matched 114 men to 114 women for FN aBMD. As shown in Table 1 (analysis B), matching subjects for FN aBMD resulted in the mean (±SD) age of the men (66.6 ± 13.1 years) being significantly greater than the women (61.0 ± 13.0 years, P < 0.001). Consistent with analysis A, matching for FN aBMD (Fig. 1a) resulted in men having significantly greater FN total cross-sectional area than the women (Fig. 1b). By contrast, the FN aBMD matching resulted in the men having significantly lower total (Fig. 1c), trabecular (Fig. 1d), and cortical vBMD (Fig. 1e) at the FN as compared with the women. Thus, the structural basis for the identical FN aBMD in the men and women was very different. These trends are visually apparent in Fig. 2, which shows representative images of cross sections of femur necks from men and women matched for FN aBMD.
a Areal BMD (aBMD) of the femur neck (FN) by DXA; b FN total cross-sectional area by QCT; c FN total volumetric BMD (vBMD) by QCT; d FN trabecular vBMD by QCT; and e FN cortical vBMD by QCT in 116 women and 116 men matched for FN aBMD. To better reflect the relative differences between women and men for each of the parameters, all values are normalized to a value of 100 for women. Bars denote SDs. *P < 0.05, **P < 0.01, and ***P < 0.001 versus men
This different structural basis for aBMD between men and women extended to femoral strength. In a third analysis (Table 1, analysis C), we constructed voxel-based FE models for bone strength in a subset of 28 men and 28 women (selected randomly, due to the resources needed to construct FE models, from the group of matched 114 men and 114 women in analysis B). As shown in Fig. 3, matching for FN aBMD (Fig. 3a) resulted in similar sex-related differences in FN total cross-sectional area (Fig. 3b), total (Fig. 3c) trabecular (Fig. 3d), and cortical vBMD (Fig. 3e) as we observed when analyzing the larger group of 228 matched subjects. Further, matching for FN aBMD resulted in the men and women having statistically similar (P = 0.335) values of FE-derived femoral strength (Fig. 3f), although this was ~11% higher in the men. Of note, fall loads were also ~11% higher in the men (Fig. 3g, P = 0.041), resulting in relatively similar values for the load-strength-ratio, Φ, in men and women (P = 0.609). These trends are visually apparent in Fig. 4, which shows representative FE models for a woman and man matched for aBMD, demonstrating the similar FE-derived femoral strength in the two subjects as a result of the greater vBMD but smaller bone size in the woman.
a Areal BMD (aBMD) of the femur neck (FN) by DXA; b FN total cross-sectional area by QCT; c FN total volumetric BMD (vBMD) by QCT; d FN trabecular vBMD by QCT; e FN cortical vBMD by QCT; f FE-derived bone strength; g estimated fall loads; and h load-to-strength ratio, Φ, in 28 women and 28 men matched for FN aBMD. To better reflect the relative differences between women and men for each of the parameters, all values are normalized to a value of 100 for women. Bars denote SDs. *P < 0.05, **P < 0.01, and ***P < 0.001 versus men
Discussion
Using DXA to measure FN aBMD, QCT to assess bone size and vBMD at the FN, and FE modeling to evaluate hip strength, our study provides a potential structural explanation for the ability of FN aBMD by DXA to predict hip fracture risk equivalently in men and women [7–9]. The key findings of our study are that matching men and women for FN aBMD results in the men (1) being ~6 years older than the women; (2) having larger bone size (i.e., FN total cross-sectional area); and (3) having lower vBMD. Since DXA is inherently influenced by bone size, with larger bones having higher aBMD [2], this property of DXA integrates effects of vBMD and bone size. In our cohort of men and women who were matched for DXA FN aBMD, this integrative effect resulted in quite similar measures of FE-derived femoral strength and even closer values of the load-to-strength ratio. From a clinical perspective, our findings therefore provide mechanistic support for using the same young reference values (i.e., those of women) in the T-score calculation for FN aBMD when estimating 10-year fracture probabilities in men and women, as is currently being done in the FRAX algorithm [10].
We recognize, however, that the in vivo risk of fracture is more complex than the parameters reported here, and there could be a different relationship of aBMD to fracture risk in men versus women due to such factors as risk of falls, differences in soft tissues protecting the femur, etc., as suggested by some [29] but not other [6] studies. In a recent prospective FE study of hip fracture in men and women, Keyak and colleagues [30] recently found that there were sex differences between the association of FE-derived femoral strength and hip fracture risk. However, their key finding was that incident hip fracture was associated with a greater decrement in FE strength between fracture cases versus controls in men than in women. To the extent that, as shown here, men and women having matched values of FN DXA aBMD had quite similar values for FE strength at the hip and even closer values of the load-to-strength ratio; the findings of Keyak et al. [30] would suggest that even using a female reference range to define osteoporosis in men may overestimate the risk of fractures in men identified as having osteoporosis, using a male-specific reference range would overestimate risk even more.
We estimated femoral strength using FE models that consistently provide very high degrees of correlation with measured femoral strength, although these models are limited insofar as the in vivo resolution of the QCT scans does not allow them to fully account for differences in bone microstructure at the femoral neck, including the thin cortical shell that may also play a role in determining femoral strength. We should note, however, that our FE technique has been shown recently in a prospective, blinded study to be highly predictive of new hip fractures in elderly men [13]. Moreover, since aging women lose bone at a faster rate than aging men [3, 31], matching women and men for FN aBMD resulted in the men being ~6 years older than the women. This may result in additional age-related deficits in bone microstructure or tissue material properties in the men that contribute to the overall risk of fracture, and the techniques used in this study did not account for these possible deficits. However, since there is no evidence of any appreciable sex effect in the relation between vBMD and mechanical properties of trabecular bone, and since the CT scans and FE models account for any sex differences of vBMD in men versus women, it is unlikely that the FE technique used here would not also be highly predictive of hip fracture in women. Indeed, our preliminary analysis of the AGES cohort validated the finite element implementation used in this study for prospective hip fracture prediction in both women and men [29]. Finally, due to resource limitations, we performed FE models only in a subset of the overall cohort, but the pattern of differences in bone size and vBMD between men and women observed for this sub-cohort were similar to those for the larger cohort analyzed only for DXA aBMD and QCT parameters.
Our study focused on FN aBMD, vBMD, and femoral strength, since the current FRAX tool for estimating fracture risk uses aBMD at this site rather than the spine [10]. Whether the relationships observed here are also true for vertebral aBMD, vBMD and bone strength is unclear and requires further study. Indeed, we did not explain why the differences in geometry and vBMD between the sexes just happens to largely cancel out for both aBMD and for femoral strength, and this effect may or may not extend to femoral strength for habitual gait loading, for example. In addition, it is also possible that in different populations of men and women from the one studied here, these opposing effects of femoral geometry and vBMD on femoral strength may or may not cancel each other out, leading to some differences in FE-derived bone strength and the load-to-strength ratio between men and women matched for aBMD. Clearly, further studies are needed to address these issues.
In summary, our study demonstrates that matching for FN aBMD between the sexes leads to quite similar values of both FE-derived femoral strength and the load-to-strength ratio, Φ, in men and women, but the structural basis for this integrative effect differs between the sexes. Specifically, matching men and women for FN aBMD results in the men having lower vBMD but greater bone size. These two parameters impact femoral strength in opposite directions, which at least in this cohort, resulted in relatively similar values of femoral strength and Φ between the sexes.
References
Miller PD, Zapalowski C, Kulak CAM, Bilezikian JP (1999) Bone densitometry: the best way to detect osteoporosis and to monitor therapy. J Clin Endocrinol Metab 84:1867–1871
Orwoll E (2000) Perspective. Assessing bone density in men. J Bone Miner Res 15:1867–1870
Riggs BL, Melton LJ III, Robb RA, Camp JJ, Atkinson EJ, Peterson JM, Rouleau PA, McCollough CH, Bouxsein ML, Khosla S (2004) Population-based study of age and sex differences in bone volumetric density, size, geometry, and structure at different skeletal sites. J Bone Miner Res 19:1945–1954
Kanis JA, WHO Study Group (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: synopsis of a WHO report. Osteoporos Int 4:368–381
Khosla S, Amin S, Orwoll E (2008) Osteoporosis in men. Endocr Rev 29:441–464
Kanis JA, Johnell O, Oden A, De Laet C, Mellstrom D (2001) Diagnosis of osteoporosis and fracture threshold in men. Calcif Tissue Int 69:218–221
De Laet CEDH, Van Hout BA, Burger H, Weel AEAM, Hofman A, Pols HAP (1998) Hip fracture prediction in elderly men and women: validation in the Rotterdam study. J Bone Miner Res 13:1587–1593
Melton LJ, Orwoll ES, Wasnich RD (2001) Does bone density predict fractures comparably in men and women? Osteoporos Int 12:707–709
Johnell O, Kanis JA, Oden A et al (2005) Predictive value of BMD for hip and other fractures. J Bone Miner Res 20:1185–1194
Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E (2008) FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int 19:385–397
Crawford RP, Cann CE, Keaveny TM (2003) Finite element models predict in vitro vertebral body compressive strength better than quantitative computed tomography. Bone 33:744–750
Keaveny TM, Hoffmann PF, Singh M, Palermo P, Bilezikian JP, Greenspan SL, Black DM (2008) Femoral bone strength and its relation to cortical and trabecular changes after treatment with PTH, alendronate, and their combination as assessed by finite element analysis of quantitative CT scans. J Bone Miner Res 23:1974–1982
Orwoll E, Marshall LM, Nielson CM et al (2009) Finite element analysis of the proximal femur and hip fracture risk in older men. J Bone Miner Res 24:475–483
Keyak JH (2001) Improved prediction of proximal femoral fracture load using nonlinear finite element models. Med Eng Phys 23:165–173
Cody DD, Gross GJ, Hou FJ, Spencer HJ, Goldstein SA, Fyhrie DP (1999) Femoral strength is better predicted by finite element models than QCT and DXA. J Biomech 32:1013–1020
Melton LJ III (1996) History of the Rochester Epidemiology Project. Mayo Clin Proc 71:266–274
Cann CE (1988) Quantitative CT for determination of bone mineral density: a review. Radiology 166:509–522
Kalender WA, Felsenberg D, Genant HK, Fischer M, Dequeker J, Reeve J (1995) The European spine phantom: a tool for standardization and quality control in spinal bone mineral measurements by DXA and QCT. Eur J Radiol 20:83–92
Camp JJ, Karwoski RA, Stacy MC, Atkinson EJ, Khosla S, Melton LJ, Riggs BL, Robb RA (2004) A system for the analysis of whole-bone strength from helical CT images. Proc SPIE 5369:74–88
Morgan EF, Keaveny TM (2001) Dependence of yield strain of human trabecular bone on anatomic site. J Biomech 34:569–577
Morgan EF, Bayraktar HH, Keaveny TM (2003) Trabecular bone modulus–density relationships depend on anatomic site. J Biomech 36:897–904
Bayraktar HH, Morgan EF, Niebur GL, Morris GE, Wong EK, Keaveny TM (2004) Comparison of the elastic and yield properties of human femoral trabecular and cortical bone tissue. J Biomech 37:27–35
Keaveny TM, Morgan EF, Niebur GL, Yeh OC (2001) Biomechanics of trabecular bone. Annu Rev Biomed Eng 3:307–333
Reilly DT, Burstein AH (1975) The elastic and ultimate properties of compact bone tissue. J Biomech 8:393–405
Roberts BJ, Kopperdahl DL, Thrall E, Muller J, Keaveny TM, Bouxsein ML (2009) Prediction of femoral strength in a sideways fall configuration using QCT-based finite element analysis. Bone 44:S72
Keaveny TM, Bouxsein ML (2008) Theoretical implications of the biomechanical fracture threshold. J Bone Miner Res 23:1541–1547
van den Kroonenberg AJ, Hayes WC, McMahon TA (1995) Dynamic models for sideways falls from standing height. J Biomech Eng 117:309–318
Robinovitch SN, McMahon AP, Hayes WC (1995) Force attenuation in trochanteric soft tissues during impact from a fall. J Orthop Res 13:956–962
Cummings SR, Cawthon PM, Ensrud KE, Cauley JA, Fink HA, Orwoll ES, Osteoporotic Fractures in Men (MrOS) Research Groups, Study of Osteoporotic Fractures Research Groups (2006) BMD and risk of hip and nonvertebral fractures in older men: a prospective study and comparison with older women. J Bone Miner Res 21:1550–1556
Keyak JH, Sigurdsson S, Karlsdottir G et al (2011) Male-female differences in the association between incident hip fracture and proximal femoral strength: a finite element analysis study. Bone 48:1239–1245
Riggs BL, Melton LJI, Robb RA, Camp JJ, Atkinson EJ, McDaniel L, Amin S, Rouleau PA, Khosla S (2008) A population-based assessment of rates of bone loss at multiple skeletal sites: evidence for substantial trabecular bone loss in young adult women and men. J Bone Miner Res 23:205–214
Acknowledgments
We would like to thank Sara Achenbach for her help with the statistical analyses, Jim Peterson for his help with data management, and Margaret Holets for the DXA aBMD measurements and analysis of the QCT scans.
Conflicts of interest
B.S., S.A., E.J.A., J.C., R.A.R., B.L.R., L.J.M., and S.K. have nothing to disclose. D.L.K. is an employee of O. N. Diagnostics and T.M.K. has a financial interest in O. N. Diagnostics and both they and the company may benefit from the results of this research.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was supported by NIH grants R01 AR027065, R43 AR052234, and 1UL1RR024150.
Rights and permissions
About this article
Cite this article
Srinivasan, B., Kopperdahl, D.L., Amin, S. et al. Relationship of femoral neck areal bone mineral density to volumetric bone mineral density, bone size, and femoral strength in men and women. Osteoporos Int 23, 155–162 (2012). https://doi.org/10.1007/s00198-011-1822-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-011-1822-8