Abstract
Summary
The incidence of non-hip femur fractures increased between 1984 and 2007, with an increase in the rates for women after 1996.
Introduction
Recent reports have suggested that non-hip femur fractures may be decreasing over time, similar to proximal femur fractures.
Methods
Incidence rates for non-hip femur fractures among Olmsted County, Minnesota, residents were assessed before and after 1995 when the oral bisphosphonate, alendronate, was approved in the USA.
Results
From 1984 to 2007, 727 non-hip femur fractures were observed in 690 Olmsted County residents (51% female [median age, 71.6 years] and 49% male [21.4 years]). Altogether, 20% of the fractures were subtrochanteric, 51% were diaphyseal, and 29% involved the distal femur. Causes included severe trauma in 51%, minimal to moderate trauma in 34%, and pathologic causes in 15%. The overall age- and sex-adjusted annual incidence of first non-hip femur fracture was 26.7 per 100,000 (25.0 per 100,000 for women and 26.6 per 100,000 for men). Incidence rates increased with age and were greater in women than men. Between 1984–1995 and 1996–2007, age-adjusted rates increased significantly for women (20.4 vs. 28.7 per 100,000; p = 0.002) but not for men (22.4 vs. 29.5 per 100,000; p = 0.202).
Conclusion
The incidence of first non-hip femur fractures rose between 1984 and 2007, with an increase in the rates for women after 1995.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The epidemiology of subtrochanteric, diaphyseal, and distal femur fractures is less well studied than that of hip (femur neck and intertrochanteric) fractures. Non-hip femur fractures occur much less commonly than proximal femur fractures, which are associated with falls and osteoporosis [1]. By contrast, non-hip femur fractures are often linked with severe trauma in younger patients. However, previous studies have shown that the incidence of non-hip femur fractures increases with age; moreover, this increase occurs mostly in women and is associated with fractures due to only moderate trauma [2–13]. Since both cortical and trabecular bone are lost with aging, it is not surprising that some of these fractures might share characteristics of the hip fractures attributed to age-related osteoporosis. More recently, interest in non-hip femur fractures has been driven by concerns that they may represent a complication of long-term bisphosphonate therapy [14]. The purpose of this study was to estimate the incidence of subtrochanteric, diaphyseal, and distal femur fractures among Olmsted County, Minnesota, residents in 1984–2007. This analysis extends an earlier population-based study of non-hip femur fractures among Rochester, Minnesota, residents in 1965–1984 [13].
Materials and methods
Population-based research can be conducted in Olmsted County (2000 population, 124,000) because medical care is virtually self-contained within the community, and there are relatively few providers [15]. Most orthopedic care, for example, is provided by the Mayo Clinic, which has maintained a common medical record with its two affiliated hospitals (St. Mary's and Rochester Methodist) for over 100 years. Recorded diagnoses and surgical procedures are indexed, including the diagnoses made for outpatients seen in office or clinic consultations, emergency room visits, or nursing home care, as well as diagnoses recorded for hospital inpatients, at autopsy, or on death certificates. Medical records of the other providers who serve the local population, most notably the Olmsted Medical Center, are also indexed and retrievable [15]. Thus, details of the medical care provided to community residents are available for study through this unique medical records linkage system (the Rochester Epidemiology Project).
Following approval by the Institutional Review Boards of Mayo Clinic and the Olmsted Medical Center, we used this database to identify all non-hip femur fractures that occurred among Olmsted County residents during the period 1984–2007. Except for four patients who declined to authorize the use of their records for research [16], detailed provider-linked inpatient and outpatient medical records were reviewed for all residents with any diagnosis attributable to diagnostic rubric 820–821 in the International Classification of Diseases, Ninth Revision, Clinical Modification [17], or equivalent codes in earlier classification systems. Almost all were admitted to local hospitals, but the availability of outpatient data allowed us to identify fractures that occurred elsewhere, as well as a few nursing home residents who were not hospitalized. All non-hip femur fractures, which account for about 5% of all femur fractures [13], were included.
Radiographic confirmation was obtained in virtually all instances, but the original radiographs from earlier years were not available for review. Designation of the fracture site was, therefore, based on radiologists' and surgeons' reports. Fracture x-rays or reports were reviewed by two of the authors (A.N., S.A.S.), one of whom is an orthopedic surgeon, to verify classification. The Arbeitsgemeinschaft für Osteosynthesefragen/Orthopedic Trauma Association (AO/OTA) classification [18] was used to classify non-hip femur fractures: Subtrochanteric fractures were defined as AO/OTA categories 32A1.1, 32A2.1, 32A3.1, 32B1.1, 32B2.1, and 32B3.1, while mid-diaphyseal fractures included all remaining AO/OTA category 32 fractures; distal femur fractures were defined as all AO/OTA category 33 fractures. Differentiation of initial from subsequent fractures was based on review of complete contemporary medical record documentation. Non-hip femur fractures were categorized as due to severe trauma, to no more than moderate trauma, or to pathologic causes. Severe trauma fractures occurred with motor vehicle accidents, falls from greater than standing height, and high-impact recreational activities. By convention, fractures attributed to minimal to moderate trauma occurred with falls from standing height or less or in the absence of an obvious precipitating event. Pathologic fractures were associated with a specific pathological lesion of the femur (e.g., metastatic malignancy).
Incidence rates were estimated separately for the people affected by their initial non-hip femur fracture during the study period (first fractures), as well as for all such fracture events that occurred in that interval (all fractures), including those subsequent fractures observed among individuals whose first fracture occurred prior to residency in the community. In calculating incidence rates, the entire population of Olmsted County was considered to be at risk. Denominator age- and sex-specific person-years were estimated from decennial census data with linear interpolation between census years [19] and extrapolation from 2000 to 2008. Assuming that fracture risk for any individual is proportional and approximately constant over intervals defined in the underlying rate table (e.g., 1 year), the likelihood is equivalent to a Poisson regression [20], allowing the use of standard software to estimate standard errors and calculate 95% confidence intervals (95% CI). Incidence rates for all non-hip femur fracture events, and for first non-hip femur fractures alone, were directly age and/or sex adjusted to the population distribution of US whites in 2000; confidence intervals for the adjusted rates are based on the same assumptions above. Data were evaluated to compare non-hip femur fractures in females vs. males, and fractures from 1984 to 1995 vs. 1996–2007, with statistical tests of secular trends included.
Results
During the 24-year study period, 1984–2007, 727 non-hip femur fractures occurred in 690 Olmsted County residents. Fifty-one percent of the patients were female, with a median age at first fracture of 71.6 years (mean, 59.7 years); the median age at first fracture for men was only 21.4 years (mean, 31.2 years). In accordance with the racial composition of the community (96% white in 1990), 96% of the patients were white by self-report. Of the total, 690 (95%) were first fractures in this time period, including 18 concurrent bilateral fractures and 5 concurrent fractures of different AO classification on the same side, and 14 were subsequent non-hip femur fractures. Altogether, these 727 fractures were caused by severe trauma in 51% of the cases, minimal to moderate trauma in 34%, and a specific pathologic lesion in the remaining 15%. Of the total fractures, 20% were subtrochanteric, 51% were diaphyseal, and 29% involved the distal femur. Of the 278 fractures that occurred in 1984–1995, 11% were subtrochanteric, 63% were diaphyseal, and 27% were distal. By contrast, 26% of the 449 fractures observed in 1996–2007 were subtrochanteric, while 44% were diaphyseal, and 30% were distal.
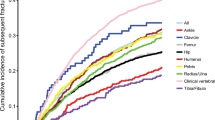
The overall age- and sex-adjusted (to 2000 US whites) annual incidence of any non-hip femur fracture among Olmsted County residents during the study period was 28.2 per 100,000 (95% CI, 26.1–30.3). The age- and sex-adjusted rate for first non-hip femur fractures alone was 26.7 per 100,000 (95% CI, 24.7–28.7), with an age-adjusted incidence of 25.0 per 100,000 (95% CI, 22.3–27.7) among females and 26.6 per 100,000 (95% CI, 23.6–29.7) among males. The incidence of first non-hip femur fractures had a J-shaped distribution, with the highest rates in female (21.0 per 100,000) and male (37.8 per 100,000) children aged 0–9 years, and in women (362 per 100,000) and men (260 per 100,000) ≥90 years of age (Fig. 1). Incidence rates were lowest in 30–39-year-old women (5.4 per 100,000) and 40–49-year-old men (9.1 per 100,000), although the pattern varied somewhat by fracture site (Table 1). Thus, it was the diaphyseal fractures, especially in males, that accounted for the high fracture incidence in children and young adults, whereas the peak at older ages was explained by subtrochanteric and distal femur fractures, especially among women. This, in turn, related to the etiology of the fractures at specific skeletal sites in females and males, as the majority of diaphyseal fractures resulted from severe trauma (Fig. 2).
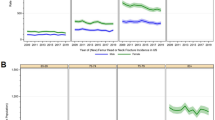
Trends in first non-hip femur fractures are illustrated in Fig. 3. The overall age- and sex-adjusted annual incidence rate was 22.1 per 100,000 (95% CI, 19.4–24.8) in 1984–1995, compared to 30.2 per 100,000 (95% CI, 27.2–33.1) in 1996–2007 (p = 0.003) (Table 2). In females, the rate increased significantly (p = 0.002) from 20.4 per 100,000 (95% CI, 16.8–24.1) in 1984–1995 to 28.7 per 100,000 (95% CI, 24.9–32.5) in 1996–2007. The change in males, from 22.4 per 100,000 (95% CI, 18.3–26.4) to 29.5 per 100,000 (95% CI, 25.1–33.8), was of similar magnitude but not statistically significant (p = 0.202). There was little change in the incidence of non-hip femur fractures due to severe trauma between the two time periods (11.0 per 100,000 [95% CI, 9.2–12.8] vs. 13.4 per 100,000 [95% CI, 11.6–15.3]; p = 0.160) or in those due to pathological lesions (3.7 per 100,000 [95% CI, 2.5–5.0] vs. 5.1 per 100,000 [95% CI, 3.9–6.4]; p = 0.117). Instead, the overall increase in incidence was mainly accounted for by the fractures attributed to minimal to moderate trauma, where rates rose from 7.4 per 100,000 (95% CI, 5.7–9.0) in 1984–1995 to 11.9 per 100,000 (95% CI, 10.0–13.8) in 1996–2007 (p = 0.004). In the subgroup of women age 60 years and over, moderate trauma fractures increased from 40.8 per 100,000 (95% CI, 29.2–55.3) in 1984–1995 to 76.1 per 100,000 (95% CI, 61.7–93.0) in 1996–2007 (p = 0.001). In younger women, rates increased only from 2.9 per 100,000 (95% CI, 1.7–4.7) in 1984–1995 to 3.5 per 100,000 (95% CI, 2.2–5.3) in 1996–2007 (p = 0.571).
Discussion
Although often considered a high-trauma fracture of young men, our study confirms previous work showing that the incidence of non-hip femur fractures is greater in women than men and increases dramatically with aging in both sexes [2–13]. Among men, subtrochanteric, diaphyseal, and distal femur fractures were all more likely to be attributed to severe, high-energy trauma, but this was true only for diaphyseal femur fractures among women. Women were also more apt to experience a subtrochanteric or distal femur fracture than one of the femur shaft, and the etiology was more often a fall. These findings suggest that many non-hip femur fractures are due also to osteoporosis, especially in older individuals who are at greatest risk.
More importantly, perhaps, this investigation demonstrated an increase in overall incidence between 1984 and 2007, with the increase due mainly to subtrochanteric and distal femur fractures in older women, similar to the recent study by Wang and Bhattacharyya [12]. These investigators reported that, while hospitalizations for femur neck and intertrochanteric fractures in the USA decreased from 263,623 in 1996 to 229,942 in 2007, subtrochanteric fractures increased from 8,273 to 10,853. Likewise, Nieves et al. [4] compared the epidemiology of hip fractures to subtrochanteric and femur shaft fractures among US adults aged 50 years and older using both the National Hospital Discharge Survey and MarketScan, a large medical claims database, and showed that annual hospital discharge rates for hip fracture (including femur neck and intertrochanteric fractures) decreased from about 600 per 100,000 to roughly 400 per 100,000 between 1996 and 2006, while the incidence of subtrochanteric and femur shaft fractures did not change over this interval from a baseline rate under 30 per 100,000 in 1996. In Sweden, the number of hospital admissions for femur shaft fractures was also unchanged between 1998 and 2004 [2]. However, none of these investigators was able to evaluate these trends in the context of incidence rates prior to 1995, nor to evaluate the radiological features of the non-hip femur fractures that they found. In the present study, we did find a slight increase in non-hip femur fracture rates among Olmsted County women after 1995, when bisphosphonates were first widely introduced into clinical practice [21], and the secular increase in non-hip femur fractures contrasts with the temporal trend of decreasing hip fracture incidence in this population over a similar time period [1].
Strengths of this study are that it is population based and medical records, including both inpatient and outpatient records, are available for the duration of each subject's residency in the community. Due to redundant data systems, fracture ascertainment is believed to be complete [5]. The main limitation of this study is that most residents of Olmsted County are white, so that results from this community may not be generalizable to other populations. However, hip fracture incidence rates in Olmsted County are similar to those seen in US whites nationally [1].
Conclusions
This population-based study suggests that non-hip femoral fractures increased between 1984 and 2007 in Olmsted County, largely because of an increase in moderate trauma fractures in older women over this interval.
References
Melton LJ III, Kearns AE, Atkinson EJ et al (2009) Secular trends in hip fracture incidence and recurrence. Osteoporos Int 20:687–694
Weiss RJ, Montgomery SM, Al Dabbagh Z, Jansson KA (2009) National data of 6409 Swedish inpatients with femur shaft fractures: stable incidence between 1998 and 2004. Injury 40:304–308
Singer BR, McLaughlan GJ, Robinson CM, Christie J (1998) Epidemiology of fractures in 15,000 adults: the influence of age and gender. J Bone Joint Surg Br 80:243–248
Nieves JW, Bilezikian JP, Lane JM et al (2010) Fragility fractures of the hip and femur: incidence and patient characteristics. Osteoporos Int 21:399–408
Melton LJ 3rd, Crowson CS, O’Fallon WM (1999) Fracture incidence in Olmsted County, Minnesota: comparison of urban with rural rates and changes in urban rates over time. Osteoporos Int 9:29–37
Knowelden J, Buhr AJ, Dunbar O (1964) Incidence of fractures in persons over 35 years of age. A report to the M.R.C. Working Party on Fractures in the Elderly. Br J Prev Soc Med 18:130–141
Soveid M, Serati AR, Masoompoor M (2005) Incidence of hip fractures in Shiraz, Iran. Osteoporos Int 16:1412–1416
Baron JA, Karagas M, Barrett J et al (1996) Basic epidemiology of fractures of the upper and lower limb among Americans over 65 years of age. Epidemiology 7:612–618
Donaldson LJ, Cook A, Thomson RG (1990) Incidence of fractures in a geographically defined population. J Epidemiol Community Health 44:241–245
Wong PC (1966) Fracture epidemiology in a mixed southeastern Asian community (Singapore). Clin Orthop Relat Res 45:55–61
Hedlund R, Lindgren U (1986) Epidemiology of diaphyseal femur fracture. Acta Orthop Scand 57:423–427
Wang Z, Bhattacharyya T (2011) Trends in incidence of subtrochanteric fragility fractures and bisphosphonate use among the US elderly, 1996–2007. J Bone Miner Res 26:553–560
Arneson TJ, Melton LJ III, Lewallen DG, O’Fallon WM (1988) Epidemiology of diaphyseal and distal femoral fractures in Rochester, Minnesota, 1965–1984. Clin Orthop Relat Res 234:188–194
Shane E, Burr D, Ebeling PR et al (2010) Atypical subtrochanteric and diaphyseal femur fractures: report of a Task Force of the American Society for Bone and Mineral Research. J Bone Miner Res 25:2267–2294
Melton LJ III (1996) History of the Rochester Epidemiology Project. Mayo Clin Proc 71:266–274
Melton LJ III (1997) The threat to medical-records research. N Engl J Med 337:1466–1470
Commission on Professional and Hospital Activities (1978) International classification of disease, 9th revision, clinical modification, volume 1, diseases tabular list. Commission on Professional and Hospital Activities, Ann Arbor, MI
Marsh JL, Slongo TF, Agel J et al (2007) Fracture and dislocation classification compendium-2007: Orthopaedic Trauma Association Classification, Database, and Outcomes Committee. J Orthop Trauma 21(10 Suppl):S1–S133
Bergstralh EJ, Offord KP, Chu CP et al (1992) Calculating incidence, prevalence and mortality rates for Olmsted County, Minnesota: an update. Technical Report no. 49, Division of Biostatistics, Mayo Clinic, Rochester, MN
Berry G (1983) The analysis of mortality by the subject-years method. Biometrics 39:173–184
Bilezikian JP (2009) Efficacy of bisphosphonates in reducing fracture risk in postmenopausal osteoporosis. Am J Med 122(2 Suppl):S14–S21
Acknowledgments
The authors would like to thank Mary Roberts for help in preparing the manuscript.
Financial support
This project was supported in part by research grant AG-04875 and made possible by the Rochester Epidemiology Project (AG-034676) from the National Institute on Aging, US Public Health Service.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ng, A.C., Drake, M.T., Clarke, B.L. et al. Trends in subtrochanteric, diaphyseal, and distal femur fractures, 1984–2007. Osteoporos Int 23, 1721–1726 (2012). https://doi.org/10.1007/s00198-011-1777-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-011-1777-9