Abstract
Summary
We observed similar prevalence of short vertebral height without endplate depression (SVH) in young women aged 20–39 years and older women aged 55–79 years. There was no association between SVH and low bone density. In older women, therefore, SVH may be largely long standing and not indicative of osteoporotic fracture.
Introduction
Algorithm-based qualitative (ABQ) definition of osteoporotic vertebral fracture (VF) requires evidence of endplate fracture, and there is no minimum threshold for apparent ‘reduction’ in vertebral height. In older women, SVH without endplate fracture identified on baseline assessment may be long standing and unrelated to VF. If this is so, we would expect to see a similar prevalence of SVH in younger women. We aimed to compare the prevalence of pre- and postmenopausal women with SVH and the characteristics of women with and without SVH.
Methods
We used the ABQ method to classify baseline vertebral images (DXA-based imaging) from 257 premenopausal and 1,361 postmenopausal women participating in the population-based Osteoporosis and Ultrasound Study. Images were classified as follows: normal (no VF, no SVH), SVH (no VF) or VF (with/without SVH in unfractured vertebrae). We compared proportions of women with SVH (chi-squared test) and compared age, height, weight and bone mineral density (BMD) by ABQ classification (two-sample t test/analysis of variance).
Results
The prevalence of pre- and postmenopausal women with SVH was 37% and 33%, respectively (P>0.05). Compared to women without SVH, premenopausal women with SVH were older (P<0.001) and heavier (P=0.05), and postmenopausal women with SVH were taller (P<0.05), with higher spine BMD (P<0.01). Postmenopausal women with VF were older (P<0.001) and shorter (P<0.01) with lower BMD (P<0.001) than women without VF.
Conclusions
Short vertebral height without endplate fracture is equally prevalent in pre- and postmenopausal women and not associated with low bone density.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prevalent vertebral fracture is usually identified when vertebral height appears reduced by a pre-specified amount in comparison to expected appearances (visual assessment) or to normal reference values (morphometric assessment). However, true change in vertebral height can only be determined longitudinally; thus, we cannot always be certain that short vertebral height observed on baseline assessment is the result of a fracture. A qualitative visual approach, algorithm-based qualitative (ABQ) definition of fracture requires evidence of fracture at the vertebral endplate, with no minimum threshold for apparent reduction in vertebral height [1]. When vertebral height appears shorter than expected without evidence of endplate fracture, it is excluded as non-fracture short vertebral height (SVH). The appearance of SVH may be mainly due to long-standing normal or developmental variation and as such, we would expect to see similar appearances in younger people. In previous studies, we have found no significant association between SVH and low bone density in men or women over 50 years of age [2, 3], but have not previously performed these analyses in a younger population. Such studies have been difficult in the past, due to the radiation dose associated with spinal radiography, but we now have access to densitometric vertebral fracture assessment (VFA) which uses only a fraction of the radiation used in conventional radiography [4] and thus represents a low-risk alternative. We wished to test the theory that SVH is largely a long-standing variant by comparing the prevalence of SVH in younger and older women. The specific aims of this study were to (1) compare the prevalence of SVH in pre- and postmenopausal women and (2) compare the characteristics of women with and without SVH.
Methods
Study participants
We analysed vertebral images obtained from women participating in the population-based Osteoporosis and Ultrasound Study (OPUS). This was a prospective study based in five European centres, namely Aberdeen, Sheffield, Paris, Kiel and Berlin [5]. Baseline visits were attended by 463 premenopausal women, aged 20–39 years, and 2,374 postmenopausal women, aged 55–79 years. This report is based on the evaluation of vertebral images obtained at baseline in a subset of the full study population; these were obtained in Aberdeen (Department of Rheumatology, NHS Grampian in association with the University of Aberdeen, Aberdeen, UK), Kiel (Medizinishce Physik, Klinik fur Diagnostische Radiologie, Univesitats-klinikum Schleswig-Holstein, Campus Kiel, Kiel, Germany), Paris (Centre d’Evaluation des Maladies Osseuses, Service de Rhumatologie, Assistance-Publique, Hopital Cochin, Universite Rene Descartes, Paris, France) and Sheffield (Metabolic Bone Centre, Northern General Hospital, UK). Exclusion criteria for entry into the study were disorders that precluded valid quantitative ultrasound measurements or general inability to undergo the study examinations. UK women were recruited from local general practices, German women were randomly selected from government registers and French women were randomly selected from the registers of a complementary health insurance system. Women included in the current analysis had attended OPUS baseline visits between 1999 and 2001 for densitometric VFA. Women who attended the Berlin centre were not included in this analysis, due to problems in accessing baseline vertebral scan images. In total, 1,618 women were included in the current analysis; of these, 257 were premenopausal, and 1,361 were postmenopausal.
Vertebral imaging and bone density assessments
Baseline vertebral images were obtained in Sheffield, Paris and Kiel using a Hologic QDR 4500A densitometer (Hologic Inc., Bedford, MA). Aberdeen images were obtained using a Lunar Expert XL (Lunar, Madison, WI). The spine was imaged in the posterior–anterior and lateral projections between vertebrae T4 and L4. Bone density scans of the lumbar spine and hip were obtained by dual-energy x-ray absorptiometry (DXA) using the same devices. Areal bone mineral density (BMD) measurements were standardised and cross-calibrated across centres; these procedures were performed at the coordinating centre in Kiel.
Assessment of vertebral images
Hologic vertebral images were viewed using the Hologic Discovery analysis software version 12.0; GE Lunar vertebral images were converted to TIFF files and viewed in Adobe Photoshop version 5.0. Vertebrae T4 through L4 were assessed visually (LF) using the ABQ approach [1], and the researcher was blinded to the age and identity of each participant.
Vertebral images were categorised as follows:
-
(i)
Normal (no evidence of SVH or osteoporotic fracture)
-
(ii)
SVH in one or more vertebrae (no evidence of osteoporotic fracture)
-
(iii)
One or more vertebral fractures (with or without SVH in unfractured vertebrae)
Short vertebral height was identified when one or more heights (anterior, central or posterior) appeared short (compared to expected appearances for normal vertebral dimensions), without evidence of endplate fracture. Vertebral heights were not measured directly and ‘shortness’ of vertebral height in the absence of fracture was estimated visually. Short vertebral height was recorded as approximately ≥20% shorter or <20% shorter than expected for normal vertebral dimensions. We estimate that the minimum that can feasibly be observed by the naked eye equates to a threshold of around 15% shorter than expected, but this is likely to vary slightly according to visual acuity and image quality. Vertebral fracture was identified when the appearances were in keeping with endplate fracture, with or without fracture of the cortex [1]. When endplate depression was identified, the severity of fracture was also estimated subjectively. Fractures were recorded as mild if vertebral height appeared reduced by up to 25% compared to expected appearances, or moderate/severe if vertebral height appeared reduced by more than 25%.
Data analysis
The percent prevalence of women with SVH or vertebral fracture was calculated separately for pre- and postmenopausal women. The proportions of pre- and postmenopausal women with SVH were compared using the chi-squared test. Mean values for age, height, weight and BMD were compared in women classified as normal or SVH (two-sample t test); these analyses were performed separately in pre- and postmenopausal women. The mean values were also compared in women classified normal, SVH or vertebral fracture (one-way analysis of variance, ANOVA). Statistical analysis was performed using MedCalc® version 11.3.3.0 (MedCalc Software bvba). We used a threshold of P<0.05 to indicate statistical significance.
Results
Prevalence of non-fracture short vertebral height and vertebral fracture
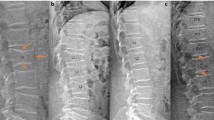
The prevalence of women with non-fracture SVH was similar in pre- and postmenopausal women (difference in proportions=4.0%; 95% CI for the difference −2.5%, 10.7%; P=0.24) (Table 1). The result remained similar when we included women from the fracture group who also had SVH in unfractured vertebrae (difference in proportions=5.0%; 95% CI for the difference −3.5%, 13%; P=0.26). Short vertebral height was predominantly characterised by short anterior height, with peaks in the vertebral level distribution of SVH in the mid-thoracic region and at the thoraco-lumbar junction (Fig. 1). The prevalence of women with vertebral fracture was significantly greater in postmenopausal compared to premenopausal women (difference in proportions=4.0%; 95% CI for the difference 0.86%, 6.3%; P=0.02) (Table 1). Among the women with both vertebral fracture and SVH in unfractured vertebrae, the majority of fractures (85%) were mild in severity: at least half of these (54%) had appearances in keeping with long-standing fracture. Approximately 10% of vertebrae could not be reliably assessed due to poor image resolution or obscuration of the vertebral endplates by artefacts.
Non-fracture SVH in pre-and postmenopausal women. Results are presented as a vertebral level-specific distribution of SVH and b height-specific distribution of SVH; for middle height, results are shown for vertebrae in which a single endplate or both endplates were identified as shorter than expected. Vertebral height was not measured, and a lower limit for SVH was not applied: we estimate the lowest threshold that can be visually detected without direct measurements to be approximately 15%
Characteristics of women with short vertebral height
Premenopausal women
Premenopausal women with SVH (no fracture) were significantly older (P<0.001) and heavier (P<0.05) than premenopausal women classified normal (no SVH or fracture) (Table 2). When women with vertebral fractures were included in the within-group comparisons (ANOVA), the significant difference in age (normal/SVH) remained (P<0.01), and there was a trend towards greater weight with SVH (P=0.065). Women with vertebral fracture did not differ significantly from other premenopausal women in terms of any of the variables assessed in this analysis.
Postmenopausal women
Postmenopausal women with SVH were significantly taller (P<0.05) and had higher lumbar spine BMD (P<0.01) than women classified normal (Table 2). There was also a trend towards older age with SVH (P=0.05). The differences in height and lumbar spine BMD remained significant when women with vertebral fractures were included in the analysis (ANOVA). Women with vertebral fractures were significantly older (P<0.001) and shorter (P<0.01) and had lower lumbar spine and total hip BMD (P<0.001) compared to women classified SVH or normal.
Discussion
We proposed that SVH without evidence of endplate fracture observed on baseline assessment in postmenopausal women is largely long-standing and unrelated to osteoporotic fracture. We tested this theory by comparing the prevalence of SVH in pre- and postmenopausal women on DXA-based VFA. The prevalence of SVH was similar in both age groups and was not associated with low bone density in either age group. In contrast, the prevalence of vertebral fracture was significantly lower in premenopausal women.
The International Society for Clinical Densitometry (ISCD) position statement on VFA recommends that prevalent vertebral fracture is identified when vertebral height appears ≥20% shorter than expected. In addition, the ISCD guidelines suggest that the reader should also take the appearance of the endplate into account [6], and this has also been noted previously [7, 8]. Our results reinforce the importance of evaluating the endplate as well as vertebral height. Inexperienced readers, or those who have not undergone formal training in the diagnosis of vertebral fractures, might find this challenging and rely instead on the manufacturer's VFA quantitative analysis software for confirmation of fracture. Such an approach could lead to incorrect classification of SVH.
In both pre- and postmenopausal women with SVH, we predominantly observed short anterior height and peaks in the frequency of SVH in the mid-thoracic spine and at the thoraco-lumbar junction. Some researchers have proposed that wedging of the vertebral bodies increases with ageing, particularly in the thoracic region, but we observed a similar prevalence of short anterior height in both age groups. The evidence for non-fracture change in vertebral dimensions over life remains unclear; some studies suggest a decrease in vertebral height with ageing [9, 10], while others have not replicated these observations [11, 12]. Vernon-Roberts and Pirie described a decrease in intervertebral disc height with ageing [13], but there have been several reports of increases that reach a peak by ages 50 to 70 years [14–16]. Increased concavity of the lumbar vertebrae with age has also been reported [14, 16, 17]. The concept of bone ‘creep’ under lifelong loading has been proposed as an explanation for apparent changes in vertebral dimensions with ageing [18].
If non-fracture concavity does increase with age, this can be differentiated from osteoporotic fracture by careful observation of the endplate and the vertebral ring apophysis on the lateral projection [1]. In a true lateral projection, the unfractured endplate will appear superimposed on the vertebral ring and thus be indistinguishable from it. If the central endplate is depressed due to fracture, it will be imaged below the level of the vertebral ring, with the concavity extending between the inner anterior and posterior borders of the ring. The lines representing the vertebral ring will then be imaged very faintly and may be difficult to see, because the ring will no longer be superimposed on the endplate, and the reduced thickness of the structure when imaged in profile will provide poor attenuation of the x-ray beam. The appearances may be less easy to interpret, however, when the projection is oblique or when there is scoliosis.
The age difference in younger women classified normal or SVH is difficult to explain and may be an artefact. Degenerative changes can give the appearance of short anterior vertebral height, when there is modelling and overgrowth of bone at the anterior surface of the vertebral body. The original anterior border may remain evident on a radiograph with good image contrast, but it may be less easy to determine on VFA due to the slightly inferior image resolution. Although we might expect degenerative changes to predominate in older women, degenerate intervertebral discs and vertebral osteophytosis have been reported in young women [19, 20]. We did not evaluate the reasons for SVH in this analysis, nor did we specifically exclude short vertebrae with the appearance of degenerative changes. However, we did ignore osteophytosis and ‘lipping’ in the determination of SVH, in keeping with the approach recommended for locating the endplates in quantitative morphometry [21].
There were some limitations to our analysis. Firstly, the subset of women studied did not represent all five participating centres in the OPUS study, due to difficulties in converting the Berlin GE Lunar images into a readable format within the allocated timeframe. However, the images from Aberdeen were acquired using a similar GE Lunar system, so our results may be applicable to images obtained by either GE Lunar or Hologic devices. Secondly, around 10% of vertebrae could not be reliably assessed by VFA, so the true prevalence of SVH or vertebral fracture in this study population could be higher. This was a low-risk study population, and we might expect to exclude a greater number of vertebrae from analysis when performing VFA in a high-risk population with lower bone density and greater prevalence of fracture. The ABQ method is a visual method that does not employ direct measurements of vertebral dimensions. We believe that visual assessment is advantageous over morphometric analysis because it enables the expert reader to rule out non-osteoporotic deformities. However, the downside of this and other visual approaches is that the method is more subjective than the quantitative approaches. For this reason, it is essential that the visual assessments are conducted by appropriately trained and experienced readers. Other less experienced readers, therefore, could obtain different results on analysis of our dataset. Finally, there is no agreed gold standard definition of osteoporotic vertebral fracture, and all methods are subject to error. It is possible that some of the women identified as having short vertebral height without fracture represented false negative diagnosis by ABQ, particularly when vertebral height appeared more than 20% shorter than expected. However, on post hoc analysis of these women, we found no significant differences in lumbar spine BMD in either age group (two-sample t tests, P>0.44; data not shown). Total hip BMD was borderline lower in women with vertebral height ≥20% shorter than expected (0.877 g/cm2 compared to 0.909 g/cm2 in women with height <20% shorter than expected; P=0.05), but remained significantly higher than in women with vertebral fracture (P<0.0001).
In conclusion, short vertebral height without evidence of endplate fracture is equally prevalent in pre- and postmenopausal women and is not associated with low bone density.
References
Jiang G, Eastell R, Barrington NA, Ferrar L (2004) Comparison of methods for the visual identification of prevalent vertebral fracture in osteoporosis. Osteoporos Int 15(11):887–896
Ferrar L, Jiang G, Armbrecht G, Reid DM, Roux C, Glüer CC, Felsenberg D, Eastell R (2007) Is short vertebral height always an osteoporotic fracture? The Osteoporosis and Ultrasound Study (OPUS). Bone 1:5–12
Ferrar L, Jiang G, Cawthon PM, San Valentin R, Fullman R, Lambert L, Cummings SR, Black DM, Orwoll E, Barrett-Connor E, Ensrud K, Fink HA, Eastell R (2007) Identification of vertebral fracture and non-osteoporotic short vertebral height in men: the MrOS study. J Bone Miner Res 22(9):1434–1441
Blake GM, Rea JA, Fogelman I (1997) Vertebral morphometry studies using dual-energy x-ray absorptiometry. Semin Nucl Med 27:276–290
Glüer CC, Eastell R, Reid DM, Felsenberg D, Roux C, Barkmann R, Timm W, Blenk T, Armbrecht G, Stewart A, Clowes J, Thomasius FE, Kolta S (2004) Association of five quantitative ultrasound devices and bone densitometry with osteoporotic vertebral fractures in a population-based sample: the OPUS study. JBMR 19:782–793
Schousboe JT, Vokes T, Broy SB, Ferrar L, McKiernan F, Roux C, Binkley N (2008) Vertebral fracture assessment: the 2007 ISCD official positions. J Clin Densitom 11(1):92–108
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res Sep 8(9):1137–1148
Grigoryan M, Guermazi A, Roemer FW, Delmas PD, Genant HK (2003) Recognizing and reporting osteoporotic vertebral fractures. Eur Spine J 12(Suppl 2):S104–S112
Hedlund LR, Gallagher JC (1988) Vertebral morphometry in diagnosis of spinal fractures. Bone Miner 5(1):59–67
Diacinti D, Acca M, D’Erasmo E, Tomei E, Mazzuoli GF (1995) Aging changes in vertebral morphometry. Calcif Tissue Int 57(6):426–429
Davies KM, Recker RR, Heaney RP (1989) Normal vertebral dimensions and normal variation in serial measurements of vertebrae. J Bone Miner Res 4(3):341–349
Rühli FJ, Müntener M, Henneberg M (2005) Age-dependent changes of the normal human spine during adulthood. Am J Hum Biol 17:460–469
Vernon-Roberts B, Pirie CJ (1977) Degenerative changes in the intervertebral discs of the lumbar spine and their sequelae. Rheumatol Rehabil 16:13–21
Shao Z, Rompe G, Schiltenwolf M (2002) Radiographic changes in the lumbar intervertebral discs and lumbar vertebrae with age. Spine 27:263–268
Amonoo-Kuofi HS (1991) Morphometric changes in the heights and anteroposterior diameters of the lumbar intervertebral discs with age. J Anat 175:159–168
Twomey LT, Taylor JR (1985) Age changes in lumbar intervertebral discs. Acta Orthop Scand 56:97–104
Evans SF, Nicholson PH, Haddaway MJ et al (1993) Vertebral morphometry in women aged 50–81 years. Bone Miner 21:29–40
Pollintine P, Luo J, Offa-Jones B, Dolan P, Adams MA (2009) Bone creep can cause progressive vertebral deformity. Bone 45:466–472
Takatalo J, Karppinen J, Niinimäki J, Taimela S, Näyhä S, Järvelin MR, Kyllönen E, Tervonen O (2009) Prevalence of degenerative imaging findings in lumbar magnetic resonance imaging among young adults. Spine (Phila Pa 1976) 34:1716–1721
Powell MC, Wilson M, Szypryt P, Symonds EM, Worthington BS (1986) Prevalence of lumbar disc degeneration observed by magnetic resonance in symptomless women. Lancet 13:1366–1367
Jenssen KK, Tougaard L (1981) A simple x-ray method for monitoring progress of osteoporosis. Lancet 2:19–20
Acknowledgements
The OPUS study was sponsored by Eli Lilly, Sanofi–Aventis, Procter & Gamble Pharmaceuticals, Hoffman-La Roche, Pfizer and Novartis, and we acknowledge the support of the National Institute for Health Research, UK, via its Biomedical Research Units funding scheme. We thank the following members of the OPUS teams at the five participating centres for their contributions: Alison Stewart, Rosie Reid and Lana Gibson (Aberdeen); the members of the Zentrum fur Muskel und Knochenforschung (Berlin), Gabriele Armbrecht, Friederike Tomasius, Frank Touby, Martina Kratzsch and Tilo Blenk; Reinhard Barkmann, Wolframm Timm, Antonia Gerwin, Maren Glüer, Roswitha John, Roswitha Marunde-Ott, Marika Mohr, Regina Schlenger, Pia Zschoche, Carsten Liess and Carsten Rose (Kiel); Therese Kolta and Nathalie Delfau (Paris) and Jackie Clowes, Margaret Paggiosi, Nicky Peel, Judy Finigan and Debbie Swindell (Sheffield).
Conflicts of interest
Richard Eastell is a consultant for Unilever and receives research funding. He has received consulting fees from Amgen, AstraZeneca, GlaxoSmithKline, Medtronics, Nastech, Nestle, Fonterra Brands, Novartis, Ono Pharma, Osteologix, Pfizer, Lilly, Sanofi–Aventis, Procter and Gamble, Tethys, Unilever, Unipath, Inverness Medical and grants from AstraZeneca, Amgen, Procter and Gamble, Unipath, Pfizer, Lilly, Novartis, Osteologix, Medical Research Council, Arthritis Research UK, Crescent Diagnostics, Nittoboseki, Nestle, and Sanofi–Aventis. He has also received honoraria from Takeda, Lilly, Amgen, the National Osteoporosis Foundation, Procter and Gamble, and GlaxoSmithKline Nutrition. This study was supported by the following funding sources: Sanofi–Aventis, Eli Lilly, Novartis, Proctor and Gamble Pharmaceuticals, Roche, Medical Research Council UK and the National Institute for Health Research, UK (via its Biomedical Research Units funding scheme); the views expressed in this publication are those of the authors and not necessarily those of the NHS, the NIHR or the UK Department of Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ferrar, L., Roux, C., Reid, D.M. et al. Prevalence of non-fracture short vertebral height is similar in premenopausal and postmenopausal women: the osteoporosis and ultrasound study. Osteoporos Int 23, 1035–1040 (2012). https://doi.org/10.1007/s00198-011-1657-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-011-1657-3