Abstract
Summary
Sunlight exposure by improving vitamin D status could be a simple public health strategy in reducing falls among frail elder people. In a randomised controlled trial, adherence to sunlight exposure was low (median adherence, 26%) and no effect of increased UV exposure on falls risk was observed (incidence rate ratio (IRR) 1.06, P = 0.73).
Introduction
This study aimed to determine whether increased sunlight exposure was effective to improve vitamin D status and reduce falls in the elderly.
Methods
In a cluster randomised controlled trial (NCT00322166 at ClinicalTrials.gov), 602 residents aged 70 or more (mean age, 86.4 years; 71% female) were recruited from 51 aged care facilities in Northern Sydney, Australia. Participants were randomised by facility to receive either increased sunlight exposure (additional 30–40 min/day in the early morning) with (UV+) or without (UV) calcium supplementation (600 mg/day) or neither (control) for a year. The co-primary endpoints were change in serum 25 hydroxy vitamin D (25OHD) and falls incidence after 12 months.
Results
Adherence to sunlight exposure was low (median adherence, 26%; IQR, 7%–45%). Serum 25OHD levels were low at baseline (median, 32.9 nmol/L) and increased only slightly depending on the number of sunlight sessions attended over 12 months (P = 0.04). During the study, 327 falls occurred in 111 (54%) subjects in the control group, 326 falls in 111 (58%) subjects in the UV only group and 335 falls in 108 (52%) subjects in the UV+ group. By intention-to-treat analysis, there was no significant effect of increased UV exposure on falls risk (IRR, 1.06; 95% CI, 0.76–1.48; P = 0.73). However, in 66 participants who attended ≥130 sessions per year (adherence, ≥50% of 260 sessions–five per week), falls were significantly reduced (IRR, 0.52; 95% CI, 0.31–0.88; P = 0.01) compared with the control group.
Conclusions
Increased sunlight exposure did not reduce vitamin D deficiency or falls risk in frail older people. This public health strategy was not effective most likely due to poor adherence to the intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vitamin D deficiency is increasingly recognized as a major public health problem [1] and is increasingly recognized to be much higher than previously thought, especially in frail older people [2]. Vitamin D deficiency is a major contributor to falls (and hence fracture risk) in older people [3]. Over 95% of hip fractures occur as a result of a fall [4]. Falls are a major health care concern in residential aged care facilities because of high levels of vitamin D deficiency, chronic illness, medication use as well as cognitive, visual, strength and balance impairments [5–7].
The principal index of vitamin D deficiency is serum 25OHD. Although controversy exists about exact thresholds for sufficiency [8], in general serum 25OHD levels below 50 nmol/L are regarded as definitely insufficient. Treatment of vitamin D deficiency reduces both falls and fracture risk in frail older people who are vitamin D deficient [3, 9, 10].
There is near universal agreement that vitamin D status should be optimized in older people, but there is a concern about ‘mass medicating’ such a large population, especially with associated problems of poor compliance documented in other studies. Compliance and adherence with medication is increasingly recognized as an important problem in osteoporosis [11, 12]. Factors which reduce adherence with drug therapy include perceived adverse effects, inconvenience, polypharmacy and physical difficulties [13, 14] and such factors may apply even with supplemental therapy such as calcium and vitamin D [15, 16]. Increased sun exposure, an apparently simple public health measure, has attraction as a way of avoiding issues relating to adherence for treating vitamin D deficiency in the elderly. Vitamin D is produced in the skin by exposure to UVB from sunlight. To maintain adequate 25OHD levels without supplements, people generally need to receive at least a third of a minimal erythemal dose (MED) on at least 15% of the body (e.g. face, arms and hands) for most days of the week [17]. Earlier smaller studies have suggested that limited UV exposure daily can significantly increase vitamin D levels in frail older people [18–20].
Oral vitamin D supplementation appears to be an effective preventative strategy for falls prevention, especially in subjects who are vitamin D deficient [3]. The combination of calcium with vitamin D may enhance this effect [21, 22]. On the other hand, oral calcium supplements may decrease overall compliance [15] and more recently have been suggested to be associated with increased risk of cardiovascular events [23]. Because of the high prevalence of falls and vitamin D deficiency in older people living in residential care facilities [24], this trial aimed to determine the feasibility of increased sunlight exposure and whether this would improve vitamin D status and reduce falls in such a population. We also investigated the effect of adding a calcium supplement because low dietary calcium intakes in older people may exacerbate the effects of vitamin D deficiency [25], and vitamin D deficiency can impair calcium absorption [26]. We randomised hostels (low care residential aged care facilities) rather than individuals because of the potential for contamination if individual residents were randomised to receive different interventions. To improve adherence we appointed ‘Sunlight Officers’ in these hostels as well as sampling attitudes of eligible participants to sunlight exposure [27]. The primary hypothesis was that increased sunlight exposure would reduce falls by improving serum 25OHD levels. Secondary hypotheses were that the intervention would reduce fractures, improve motor function and improve mood.
Methods
Design overview
This is a cluster randomised controlled trial of 12 months duration (ID no NCT00322166 at ClinicalTrials.gov). The study has been approved by the local human research ethics committee. The trial conformed with CONSORT guidelines for reporting cluster randomised trials [28].
Setting and participants
Men and women were recruited from 51 residential aged care facilities (hostels) over 1.5 years in Northern Sydney. Written informed consent was obtained before randomisation. Residents were eligible for inclusion if they were aged >70 years, ambulant, considered likely to survive for more than 12 months [29], not taking vitamin D or calcium supplements and had no history of skin cancer in the last 3 years.
Randomisation and interventions
Hostels agreeing to participate were randomised to one of three arms: increased sunlight exposure (UV), sunlight exposure plus calcium (UV+) or usual care (control). The random allocation sequence, which was in permuted blocks of size 6 or 3, was generated by a statistician who was not involved in the recruitment; and it was concealed from the study coordinators until after randomisation.
Participants in the intervention groups underwent exposure of their face, hands and arms for 30 to 40 min daily for 12 months, 5 days per week. During midsummer, these sessions were run between 8.30 and 9.30 a.m. and during mid-winter, between 9.30 and 11 a.m. To monitor and enhance adherence, ‘Sunlight Officers’ were employed in each intervention institution. In the UV+ group, calcium supplements (Caltrate, calcium carbonate 600 mg, Whitehall) were administered along with other medications. Participants in the control group were provided with a brochure about vitamin D deficiency and how to treat it. Otherwise, they received their usual routine care and nutrition for their institution. To assess factors affecting adherence, a subsample of the residents were interviewed on attitudes to sunlight exposure [27].
Outcomes and follow-up
The co-primary outcomes were falls over 12 months and serum 25OHD measured at baseline, 6 and 12 months. The state government has mandated reporting of falls in residential care, and the management in these facilities required nursing staff to report any fall that they witnessed or became aware of. Falls were recorded by regular two monthly visits to hostels including review of incident reports and clinical record review [30]. 25OHD was measured by liquid chromatography tandem mass spectrometry (Shimadzu Scientific Instruments, USA; API-5000 triple-quadruple mass spectrometer, Applied Biosystems, Canada). The limit of detection was 1.25 nmol/L. Intra and inter-assay coefficients of variation were 6.9% and 8.7%, respectively. Serum levels of intact PTH were determined using a Roche Elecsys® assay (Roche Diagnostics, Rotkreuz, Switzerland). Biochemistry relevant to calcium metabolism was measured at baseline. Other secondary outcomes included motor function measures (static balance and walking speed) assessed at baseline, 6 and 12 months using the same methods employed in a previous study [30] and grip strength was also assessed. Briefly, static balance was measured as the ability of subjects to maintain balance while standing on a firm and compliant surface. Subjects were classified into five grades—from ‘grade 1, not capable’, unable to maintain balance for any period without support on a firm surface, to ‘grade 5, good’, capable of maintaining balance whilst standing on a firm surface or foam rubber mat (70 × 60 × 15 cm thick) for 30 s periods without difficulty. Walking speed (m/s) was assessed over a distance of 8ft (2.44 m) and grip strength (kilogrammes) was measured using a North Coast Medicals hand dynamometer (Sportstek Physical Therapy Supplies Pty Ltd, Victoria, Australia). Fractures were validated by X-ray reports. The effects of the intervention on mood were assessed using the Geriatric Depression Scale (GDS) [31]. Potential adverse effects of intervention were also examined. Because of recent reports of potential increased risk of cardiovascular events, especially myocardial infarction with calcium supplementation, we monitored deaths during and after the completion of the primary study and examined causes of death using death certificates in relation to treatment [23].
Statistical analysis
The primary analyses were by intention to treat. We used negative binomial regression with cluster and robust options in Strata 11 (Strata Corporation, Texas, USA) to analyse differences between intervention and control groups in the primary outcome measure of falls and capped number of falls at 15 to minimize the possibility of subjects who suffered frequent falls unduly influencing the findings. Incidence rate ratio (IRR; the ratio of falling in one group compared with another and similar to relative risk) was reported with 95% confidence interval (CI). We treated falls as count data in the analysis and therefore reported coefficient of variation (k = σ B/λ, where σ 2B is the between-cluster variance and λ is the mean of the cluster rates) instead of intra-class correlation coefficients (ICC), as suggested by Hayes and Moulton [32]. We allowed for cluster randomisation for all other analyses by specifying hostel as a random effect and report ICC for these outcomes. Distributions of 25OHD and PTH were transformed to normal using natural logarithms. As serum 25OHD varies with age, sex and season [24], we developed a regression model of baseline serum 25OHD on age, sex and season, and used it to calculate the residuals at baseline and 12 months. These residuals were then used to assess the effects of the interventions on serum 25OHD using linear regression (i.e. random effects linear model by xtreg command). We also used linear regression to analyse PTH, walking speed and GDS. We analysed balance using ordinal logistic regression with gllamm command and fractures and mortality using Cox’s proportional hazards regression.
We conducted post hoc analyses to investigate the effect of adherence to the intervention on falls and vitamin D. Adherers were defined as those who attended at least 50% of available sunlight sessions. Given sessions were run on weekdays 5 days per week, the total available sessions per year were 260 (52 × 5), i.e. adherers attended ≥130 sessions.
Sample size considerations
We assumed 50% of subjects would fall in the control group, and loss to follow-up would be 20% (deaths and transfers to other institutions). With 12 months of follow-up, if subjects were randomised individually, we would require 148 subjects per group to detect a 30% relative reduction in falls risk from 50% to 35% with 80% power at the two-sided 5% significance level. For cluster randomisation, we calculated the intra-cluster correlation coefficient from our earlier study [30] as 0.02, giving a design effect of 1.48 for our original assumption that 25 subjects would be recruited per hostel. In fact by halfway through recruitment an average of only 11 subjects per hostel had been recruited, so recalculation gave a design effect of 1.20 (1 + (11 − 1) × 0.02), requiring a total of 51 hostels and 561 subjects.
Results
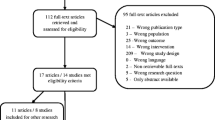
A total of 602 subjects were recruited in 51 hostels with 17 hostels randomised to each treatment group (Fig. 1). Subjects who transferred to other institutions (n = 65) were followed for falls and 25OHD outcomes; however, 16 subjects who transferred to institutions outside of the area were lost to follow-up. Taking account of the 16 lost to follow-up and 63 deaths, 87% of the 602 subjects completed the study. Demographic and other baseline characteristics are shown in Table 1. There were 175 (29%) males and 427 (71%) females; mean age is 86.4 (SD 6.6), ranging from 70 to 107 years. Apart from better cognitive scores in the UV+ group, there were no important baseline differences between groups. Ninety subjects (28 from the control group and 62 from the sunlight groups; P = 0.52) commenced taking vitamin D supplements after randomisation. Blood samples were available in 566 subjects (Table 1). Serum 25OHD levels were low at baseline (median, 32.9 nmol/L; interquartile range (IQR), 23.8 to 47.3 nmol/L) and were similar among groups.
Adherence
Despite the appointment of Sunlight Officers, adherence to increased sunlight exposure was generally low: 70% of the 397 subjects attended >10% of the sessions, 44% attended >30% of the sessions and only 17% of subjects attended >50% of the available 260 sessions in a year. Expressed as a percentage of available sessions, median (IQR) adherence was 26% (7% to 45%). Adherence with calcium supplements at 6 and 12 months was 56% and 46%, respectively. The rate of dropout was reasonably constant over the study period and by season.
Biochemistry
Over 12 months, serum 25OHD increased more in the UV and UV+ groups than placebo but this difference was not statistically significant. Serum PTH levels were significantly reduced over 12 months in the UV+ group (P < 0.001) but not in the UV alone group (Fig. 2a). Given the low adherence to sunlight sessions, we examined the relationship between 25OHD and number of sunlight sessions attended. Serum 25OHD levels at 12 months increased with the number of sunlight sessions attended (P = 0.04). At 12 months, participants who attended >130 sessions (i.e. >2.5 sessions per week or 50% of the total available sessions) had serum 25OHD levels that were slightly higher (5.9 nmol/L) than those who attended <52 sessions (i.e. <1 session/week) (Fig. 2b). However, the difference was only 3.4 nmol/L greater after excluding subjects who commenced vitamin D supplements during the study. In these latter subjects, the adjusted geometric mean of 25OHD was markedly improved at 79.5 nmol/L, which was 48.1 nmol/L higher than those not taking vitamin D supplements.
a Geometric mean of parathyroid hormone (PTH) at baseline and 12 months by intervention group. Note: P = 0.001 from F test comparing means of three groups (df = 2) at 12 months, treating groups as a factor while adjusting for baseline PTH. b Levels of serum 250HD at 12 months. Note: P = 0.04 for test for trend in means across the four ordered groups (df = 1) from a random-effect model, adjusting for age, sex, season at time of blood collection and serum 25OHD at baseline
Falls
There were 988 falls sustained by 330 (55% of 602) subjects during the study. In the control group, there were 327 falls by 111 (54% of 205) subjects, in the UV only group 326 falls by 111(58% of 190) subjects and in the UV+ group 335 falls by 108 (52% of 207) subjects. Because there was no difference between the UV and UV+ groups, we combined them to examine the effect of sunlight exposure. The difference between groups is shown in Table 2. By intention-to-treat analysis, there was no effect of sunlight exposure on falls risk (IRR, 1.06; 95% CI, 0.76 to 1.48). We explored relationships between subsequent sunlight attendance and baseline features and found adherers had better balance (P < 0.002) and lower GDS (P < 0.001) at baseline. We adjusted for these and other variables previously shown to predict falls [33], namely age, sex, past falls, urinary incontinence, cognitive impairment, static balance, co-morbidities, care level (RCS) and GDS. After adjustment for these variables, falls were significantly reduced (IRR, 0.59; 95% CI, 0.36 to 0.98) among 66 subjects who attended more than 130 sunlight sessions compared with the control group (Table 3). There was no additional effect of calcium supplementation on falls.
Fractures
There were 50 fractures sustained by 47 (8%) subjects: 18 fractures by 17 (8%) subjects in the control group; 19 fractures by 17 (9%) subjects in the UV group; and 13 fractures by 13 (6%) subjects in UV+ group. There was no significant difference in fracture incidence among groups.
Other secondary endpoints
Adherers had significantly better balance at 12 months than the controls after adjusting for age, sex, co-morbidities and balance at baseline (P = 0.002; Table 3). There was no significant effect on walking speed (P = 0.16) or GDS (P = 0.41) at 12 months.
Safety
There were 18 new skin cancer events during the study but there was no significant difference in incidence among the three groups. One subject fell once on their way to a sunlight session. During and after the trial (up to 1,300 days), 218 subjects died. By intention to treat analysis, there was increased all cause mortality in the calcium treated group compared with the UV alone group (HR 1.23 vs 0.76; P = 0.03) after adjustment for potential confounders. Examining deaths from myocardial infarction in all subjects using calcium supplements at 6 and 12 months, there was a trend for an increased death rate from myocardial infarction (age-adjusted HR, 3.83; 95% CI, 0.97 to 15.27; P = 0.06 and sex-adjusted HR, 4.17; 95% CI, 0.69 to 25.16; P = 0.12).
Discussion
Falls are a major public health issue in elderly people living in residential care facilities where vitamin D deficiency is common. This study examined whether it was feasible to achieve adequate levels of 25OHD and reduce falls risk with an apparently simple and widely applicable public health measure, namely increased sun exposure. The study findings highlight that from both a clinical and practical standpoint increasing sunlight exposure is a surprisingly challenging form of treatment and difficult to implement due to limited adherence by frail elder people in existing care facilities, even in a country like Australia renowned for mild sunny weather.
Adherence with medication in the real-world setting is increasingly recognized as an important problem in the treatment of postmenopausal osteoporosis [11, 12]. The cluster randomised nature of our trial is closer to the real-world setting than trials of pharmaceutical agents in osteoporosis which are closely monitored [12]. Poor adherence with our public health approach over the duration of the intervention was also the major problem in our trial, despite our strategy of appointing Sunlight Officers to engage and support patients in improving adherence [34]. Although the sunlight officers had a thorough understanding of the study and were trained by the full time research staff, they appear to have had weaker relationships with the participants compared with the research staff, who recruited participants and spent time with them at the baseline assessment gaining trust. Over time participants lost enthusiasm to attend and the sunlight officers, who were only employed part time, appeared less willing to spend time encouraging participants to adhere to the protocol. Although some residents wore hats, use of sunblock was uncommon. It had been anticipated that it may be practically difficult to achieve increased exposure during the winter, but adherence was limited during other seasons as well. Factors which reduce adherence with drug therapy include perceived adverse effects, inconvenience and physical difficulties [13, 14, 34]. Compliance with calcium supplements in our study was comparable with the RECORD study [15]. However, factors affecting compliance with public health approaches may differ. In a survey before randomization of 57 eligible participants from our cohort, we found that poor health, physical disability and perceived difficulty of access to and lack of ownership of outdoor spaces were barriers to sunlight exposure [27]. This may be improved by guidelines to facilitate provision of safe sun exposure [35]. From subsequent interviews of subjects performed during or at the end of the intervention, we found one of the main barriers to attendance was the perceived regimentation of having to attend the sessions every week day at a set time. Some people had other activities at that time, while others found it difficult to get ready in the mornings. Other factors included the discomfort of the heat on the summer mornings, health or mobility problems that prevented attendance, the reluctance to participate as part of a group setting and overall lack of motivation.
If the participant attended 50% or more of the sunlight sessions, there was a significant reduction in falls and improved physical functioning. However, this analysis by level of adherence was not pre-specified and residual confounding is a strong possibility, even though we adjusted for factors influencing falls that we had established in a past study in a very similar population [33]. A number of studies have examined the relationship between serum 25OHD and falls and generally reported reductions in falls require much larger increases in 25OHD. The median value of 41.2 nmol/L at 12 months in our most adherent subjects was still well below some recommended values [8] and was considerably below the median value of 81.9 nmol/L observed in subjects who commenced taking supplements during our study.
To maintain adequate 25OHD levels without supplements, people generally need to receive at least a third of a MED on at least 15% of the body most days of the week, which has been calculated to be approximately equivalent to around 1,000 IU of vitamin D most days [17]. For healthy fair-skinned people, this ought to be achieved in around 10 min, however longer times of around 25 min are required in winter in Sydney. There is evidence that less substrate 7-dehydrocholesterol is present in the skin of older individuals [36]. When subjected to relatively high doses of artificial UV over the whole body, older individuals did not increase their vitamin D levels as much as younger people [37], although when subjects were given lower doses of artificial UV over a limited body area over several days, 25OHD levels were not different between older and young subjects [38]. Overall, our study supports the suggestion that in older people, the ability to make vitamin D may be impaired, though the expected increase in 25OHD after 1,000 IU of vitamin D per day is only around 13 nmol/L [39].
Our findings about the effect of UV exposure on serum 25OHD levels in frail older people are in contrast to several earlier but smaller studies. Two of these studies used artificial UV sources, whereas the study most analogous to ours was by Reid et al. [20] which included 15 elderly people (mean age, 80) in residential care in Auckland (latitude 37° S). After sun exposure for either 15 or 30 min outdoors, supervised by nursing staff during Spring, serum 25OHD increased by 7 and 18.5 nmol/l, respectively. Adherence was not stated but this study had a duration of only 4 weeks and so may not be inconsistent with our study, since poor adherence was seen progressively in our study after the first month. In one other study from Japan, older subjects were exposed outdoors for 15 min daily for 12 months and achieved significant rises in 25OHD levels, but the generalizability of this study, which involved chronically hospitalised subjects with Alzheimers disease, is unclear [40]. Another benefit of sun exposure in frail older people may be effects on mood. Interestingly, we found those who were more adherent had better baseline GDS score but after adjusting for confounders, increased UV exposure during the study had no effect on GDS.
This study has a number of strengths and weaknesses. To our knowledge, this is the largest published randomised trial evaluating sunlight exposure and the only study to examine falls as a primary outcome measure. The follow-up was greater than 80% and both ITT and per-protocol analyses were conducted. Although individual randomisation of participants would have been preferable, it was not considered feasible, mainly because of the administrative difficulties for hostel staff if residents were randomised to receive different interventions. We asked subjects to be exposed in the morning because of skin cancer concerns and to avoid disruption to the activities of the facilities. The amount of bare skin exposed was not recorded but UV monitors (data not shown) mostly indicated adequate sun available in terms of measured MED. In summer, in Sydney, which is 33° 52 s south, people with skin type II (most of the people in the study) get a standard vitamin D dose at 9 a.m. in around 10 min [41]. A standard dose would take slightly longer at 8.30 a.m., but not substantially, and our people were out for more than 10 min. The UV index in summer in Sydney is well over 3, even fairly early in the morning, which means that vitamin D can be made—this needs a UV index of above 1.7 [41]. Even in mid-winter, a standard vitamin D dose for skin type II people would be obtained in around 30 to 60 min at 10.30 or 9 a.m., respectively [41]. The adherers were different from the controls at baseline in some measures, although we adjusted for these differences. The benefit seen in the most adherent population could be due to the benefit of increased staff contact with sunlight officers or social interaction with other residents and increased ambulation. There was no blinding among participants or research staff, although laboratory staff conducting the biochemical analyses were unaware of group assignment and falls were documented by facility staff who were usually unaware of the resident being part of a study. Of interest, we observed increased all cause mortality with a non-significant trend for increased deaths from myocardial infarction in calcium users which is consistent with a recent meta-analysis which suggested calcium supplementation may increase risk of cardiovascular events especially myocardial infarction [23]. We did not record cardiovascular events prospectively during the trial but because our population was very elderly, we did experience a large number of deaths over follow-up of up to 1,300 days, which allowed us to explore deaths due to such events.
In conclusion, although increased sunlight exposure appears an attractive public health approach to reduce the prevalence of vitamin D deficiency and falls risk, adherence with this approach is even more limited than with oral supplements at least in current facilities. Better planning of aged care facilities to improve access to sunny areas and make them pleasant to be in may help. In the meantime, the importance of this study is that it largely renders the oral supplements vs sun debate academic—at least in older subjects in institutionalized care. Vitamin D supplementation appears to be a much more practical approach.
References
Holick MF, Chen TC (2008) Vitamin D deficiency: a worldwide problem with health consequences. Am J Clin Nutr 87:1080S–1086S
Lips P (2001) Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications. Endocr Rev 22:477–501
Bischoff-Ferrari HA, Dawson-Hughes B, Staehelin HB, Orav JE, Stuck AE, Theiler R, Wong JB, Egli A, Kiel DP, Henschkowski J (2009) Fall prevention with supplemental and active forms of vitamin D: a meta-analysis of randomised controlled trials. BMJ 339:b3692
Norton R, Campbell AJ, Lee-Joe T, Robinson E, Butler M (1997) Circumstances of falls resulting in hip fractures among older people. J Am Geriatr Soc 45:1108–1112
Lord SR, Clark RD, Webster IW (1991) Physiological factors associated with falls in an elderly population. J Am Geriatr Soc 39:1194–1200
Thapa PB, Brockman KG, Gideon P, Fought RL, Ray WA (1996) Injurious falls in nonambulatory nursing home residents: a comparative study of circumstances, incidence, and risk factors. J Am Geriatr Soc 44:273–278
Tinetti ME (1987) Factors associated with serious injury during falls by ambulatory nursing home residents. J Am Geriatr Soc 35:644–648
Bischoff-Ferrari HA (2008) Optimal serum 25-hydroxyvitamin D levels for multiple health outcomes. Adv Exp Med Biol 624:55–71
Bischoff-Ferrari HA, Willett WC, Wong JB, Stuck AE, Staehelin HB, Orav EJ, Thoma A, Kiel DP, Henschkowski J (2009) Prevention of nonvertebral fractures with oral vitamin D and dose dependency: a meta-analysis of randomized controlled trials. Arch Intern Med 169:551–561
Cameron ID, Murray GR, Gillespie LD, Robertson MC, Hill KD, Cumming RG, Kerse N (2010) Interventions for preventing falls in older people in nursing care facilities and hospitals. Cochrane Database Syst Rev CD005465
Caro JJ, Ishak KJ, Huybrechts KF, Raggio G, Naujoks C (2004) The impact of compliance with osteoporosis therapy on fracture rates in actual practice. Osteoporos Int 15:1003–1008
Siris ES, Selby PL, Saag KG, Borgstrom F, Herings RM, Silverman SL (2009) Impact of osteoporosis treatment adherence on fracture rates in North America and Europe. Am J Med 122:S3–S13
Hughes CM (2004) Medication non-adherence in the elderly: how big is the problem? Drugs Aging 21:793–811
Yasin S (1998) Detecting and improving compliance. Is concordance the solution? Aust Fam Physician 27:255–260
Grant AM, Avenell A, Campbell MK, McDonald AM, MacLennan GS, McPherson GC, Anderson FH, Cooper C, Francis RM, Donaldson C, Gillespie WJ, Robinson CM, Torgerson DJ, Wallace WA (2005) Oral vitamin D3 and calcium for secondary prevention of low-trauma fractures in elderly people (randomised evaluation of calcium or vitamin D, RECORD): a randomised placebo-controlled trial. Lancet 365:1621–1628
Jackson RD, LaCroix AZ, Gass M, Wallace RB, Robbins J, Lewis CE, Bassford T, Beresford SA, Black HR, Blanchette P, Bonds DE, Brunner RL, Brzyski RG, Caan B, Cauley JA, Chlebowski RT, Cummings SR, Granek I, Hays J, Heiss G, Hendrix SL, Howard BV, Hsia J, Hubbell FA, Johnson KC, Judd H, Kotchen JM, Kuller LH, Langer RD, Lasser NL, Limacher MC, Ludlam S, Manson JE, Margolis KL, McGowan J, Ockene JK, O’Sullivan MJ, Phillips L, Prentice RL, Sarto GE, Stefanick ML, Van Horn L, Wactawski-Wende J, Whitlock E, Anderson GL, Assaf AR, Barad D (2006) Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med 354:669–683
Nowson CA, Diamond TH, Pasco JA, Mason RS, Sambrook PN, Eisman JA (2004) Vitamin D in Australia. Issues and recommendations. Aust Fam Physician 33:133–138
Chel VG, Ooms ME, Popp-Snijders C, Pavel S, Schothorst AA, Meulemans CC, Lips P (1998) Ultraviolet irradiation corrects vitamin D deficiency and suppresses secondary hyperparathyroidism in the elderly. J Bone Miner Res 13:1238–1242
Corless D, Gupta SP, Switala S, Barragry JM, Boucher BJ, Cohen RD, Diffey BL (1978) Response of plasma-25-hydroxyvitamin D to ultraviolet irradiation in long-stay geriatric patients. Lancet 2:649–651
Reid IR, Gallagher DJ, Bosworth J (1986) Prophylaxis against vitamin D deficiency in the elderly by regular sunlight exposure. Age Ageing 15:35–40
Tang BM, Eslick GD, Nowson C, Smith C, Bensoussan A (2007) Use of calcium or calcium in combination with vitamin D supplementation to prevent fractures and bone loss in people aged 50 years and older: a meta-analysis. Lancet 370:657–666
DIPART (vitamin D individual patient analysis of randomized trials) Group (2010) Patient level pooled analysis of 68 500 patients from seven major vitamin D fracture trials in US and Europe. BMJ 340:B5463
Bolland MJ, Avenell A, Baron JA, Grey A, MacLennan GS, Gamble GD, Reid IR (2010) Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: meta-analysis. BMJ 341:c3691
Zochling J, Chen JS, Seibel M, Schwarz J, Cameron ID, Cumming RG, March L, Sambrook PN (2005) Calcium metabolism in the frail elderly. Clin Rheumatol 24:576–582
Clements MR, Johnson L, Fraser DR (1987) A new mechanism for induced vitamin D deficiency in calcium deprivation. Nature 325:62–65
Heaney RP (2003) Vitamin D depletion and effective calcium absorption. J Bone Miner Res 18:1342
Durvasula S, Kok C, Sambrook PN, Cumming RG, Lord SR, March LM, Mason RS, Seibel MJ, Simpson JM, Cameron ID (2010) Sunlight and health: attitudes of older people living in intermediate care facilities in southern Australia. Arch Gerontol Geriatr 51:e94–e99
Campbell MK, Elbourne DR, Altman DG (2004) CONSORT statement: extension to cluster randomised trials. BMJ 328:702–708
Holtzman J, Lurie N (1996) Causes of increasing mortality in a nursing home population. J Am Geriatr Soc 44:258–264
Sambrook PN, Cameron ID, Chen JS, Cumming RG, Lord SR, March LM, Schwarz J, Seibel MJ, Simpson JM (2007) Influence of fall related factors and bone strength on fracture risk in the frail elderly. Osteoporos Int 18:603–610
Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, Leirer VO (1982) Development and validation of a Geriatric Depression Screening Scale: a preliminary report. J Psychiatr Res 17:37–49
Hayes RJ, Moulton LH (2009) Cluster randomised trials: a practical approach. Chapman & Hall, London
Lord SR, March LM, Cameron ID, Cumming RG, Schwarz J, Zochling J, Chen JS, Makaroff J, Sitoh YY, Lau TC, Brnabic A, Sambrook PN (2003) Differing risk factors for falls in nursing home and intermediate-care residents who can and cannot stand unaided. J Am Geriatr Soc 51:1645–1650
Cutler DM, Everett W (2010) Thinking outside the pillbox—medication adherence as a priority for health care reform. N Engl J Med 362:1553–1555
Chief Health Officer VA. Vitamin D and the Built Environment in Victoria—A guideline for planners, engineers, architects and policy makers in local and state government 2009. Available at: http://www.health.vic.gov.au/chiefhealthofficer/publications/vitamind.htm. Accessed 08/03/2010. 2010
MacLaughlin J, Holick MF (1985) Aging decreases the capacity of human skin to produce vitamin D3. J Clin Invest 76:1536–1538
Holick MF, Matsuoka LY, Wortsman J (1989) Age, vitamin D, and solar ultraviolet. Lancet 2:1104–1105
Davie M, Lawson DE (1980) Assessment of plasma 25-hydroxyvitamin D response to ultraviolet irradiation over a controlled area in young and elderly subjects. Clin Sci Lond 58:235–242
Heaney RP, Davies KM, Chen TC, Holick MF, Barger-Lux MJ (2003) Human serum 25-hydroxycholecalciferol response to extended oral dosing with cholecalciferol. Am J Clin Nutr 77:204–210
Sato Y, Iwamoto J, Kanoko T, Satoh K (2005) Amelioration of osteoporosis and hypovitaminosis D by sunlight exposure in hospitalized, elderly women with Alzheimer’s disease: a randomized controlled trial. J Bone Miner Res 20:1327–1333
Webb AR, Engelsen O (2006) Calculated ultraviolet exposure levels for a healthy vitamin D status. Photochem Photobiol 82:1697–1703
Acknowledgement
The authors gratefully acknowledge the support we received from the staff members in the participating institutions.
Funding
This work was supported by a project grant from the Australian National Health and Medical Research Council.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sambrook, P.N., Cameron, I.D., Chen, J.S. et al. Does increased sunlight exposure work as a strategy to improve vitamin D status in the elderly: a cluster randomised controlled trial. Osteoporos Int 23, 615–624 (2012). https://doi.org/10.1007/s00198-011-1590-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-011-1590-5