Abstract
Vitamin D deficiency is prevalent among patients with end-stage organ failure awaiting transplant. Low serum 25-hydroxyvitamin D (25-OHD) levels in these patients may be related to many disease-specific factors, as well as decreased sunlight exposure and limited intake of foods containing vitamin D. Low serum 25-OHD levels are also extremely common following solid organ transplantation, both during the immediate postoperative period and in long-term graft recipients. Demographic and lifestyle factors are important in determining D status in transplant recipients. Worse vitamin D status is associated with poorer general health, lower albumin, and even decreased survival among these patients. Although several studies have demonstrated that active forms of vitamin D and its analogues prevent bone loss following transplantation, the data do not show consistent benefit. These therapies may have particular utility after renal transplantation. However, given the narrow therapeutic window with respect to hypercalcemia and hypercalciuria, and the demonstrated efficacy of bisphosphonates to prevent post-transplantation bone loss, we regard these agents as adjunctive rather than primary therapy for transplantation osteoporosis. The effects of 1,25(OH)2D on the immune system, which are still being elucidated, may have potential for reducing infections and preventing allograft rejection after transplantation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
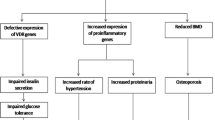
The many skeletal and extraskeletal sequelae of vitamin D deficiency are of particular consequence in the population of patients who have received an organ transplant. Musculoskeletal effects of vitamin D deficiency include secondary hyperparathyroidism, bone loss, and fracture, as well as indirect effects on muscle weakness and falls [1, 2]. Extraskeletal sequelae include insulin resistance, hypertension, and malignancy [3, 4]. Among transplant patients, a potentially important role of vitamin D relates to its regulation of immune function [5]. In this article, we will review the prevalence of vitamin D deficiency in organ transplant candidates and in long-term transplant recipients, with assessment of vitamin D status based upon 25-hydroxyvitamin D (25-OHD) measurements, the most reliable and stable indicator of vitamin D stores. We will summarize interventional trials evaluating vitamin D, 1,25(OH)2D, and its analogues for the prevention and treatment of bone loss following solid organ transplantation. Finally, we will review the role of vitamin D in immune function as it relates to the transplant population. In this review, the term parent vitamin D will be used to refer to cholecalciferol and ergocalciferol. We will not differentiate between these two forms as there are no data comparing them in transplant patients and data in healthy populations are conflicting [6–8].
Vitamin D deficiency in organ transplant candidates
Vitamin D insufficiency and deficiency are extremely common among patients with end-stage organ failure; insufficient vitamin D levels have been documented in organ transplant candidates with congestive heart failure [9], end-stage pulmonary disease [10], liver failure [11, 12], and chronic kidney disease [13, 14]. Several factors place patients with end-stage organ failure at particular risk for vitamin D deficiency (Table 1). These include limited sunlight exposure and low dietary intake of vitamin D-containing foods. In addition, hepatic dysfunction, which can result from intrinsic liver disease or from hepatic congestion in heart failure patients, may contribute to vitamin D deficiency. For the purposes of this review, we will define insufficiency as 25-OHD <30 ng/mL, deficiency as 25-OHD <20 ng/mL, and severe deficiency as 25-OHD <10 ng/mL. As categorization of vitamin D status differs in the various published reports, it is not always possible to ascertain the percentage of subjects in each of these categories. We have tried to present the data available in a uniform manner.
Vitamin D deficiency in patients with congestive heart failure
In patients with congestive heart failure, we reported that mean 25-OHD was in the deficient range (18 ng/mL). Furthermore, 18% of patients had severe deficiency (<9 ng/mL). Lower 25-OHD was associated with lower serum calcium, phosphorus, and albumin and higher total alkaline phosphatase activity and bone resorption markers, but not with serum 1,25(OH)2D. Those patients in the highest tertile of 25-OHD had significantly lower parathyroid hormone (PTH) levels [9]. In another study of patients with end-stage heart failure, lower circulating calcitriol was associated with poor clinical outcomes, including death and the need for transplantation [15].
Vitamin D deficiency in patients with end-stage pulmonary disease
In patients with end-stage pulmonary disease, 25-OHD deficiency is common and profound. Severe vitamin D deficiency has been reported in 20–50% of subjects [10, 16, 17]. In cystic fibrosis (CF), a common indication for lung transplantation, vitamin D deficiency is an important factor associated with osteoporosis and fractures [18–20]. We have observed that vitamin D deficiency, related in part to pancreatic insufficiency, is extremely common in CF patients despite supplementation; bone density is significantly lower in D-deficient patients [19]. In patients with advanced pulmonary disease, low 25-OHD is associated with lower fat mass, obstructive pulmonary disease, and low dietary vitamin D intake and was a predictor of decreased walking distance [21].
Vitamin D deficiency in patients with liver failure
Vitamin D deficiency is also common among liver transplant candidates. In 45 patients awaiting transplantation, mean 25-OHD was 9 ng/mL [11]. A study of 58 patients with cirrhotic end-stage liver disease referred for liver transplantation [22] reported that serum 25-OHD, 1,25(OH)2D, intact PTH, and osteocalcin (a marker of bone formation) were lower and urinary hydroxyproline excretion (a marker of bone resorption) was higher in cirrhotic patients than controls. Liver transplant candidates with a model for end-stage liver disease score of >15, indicative of worse disease and poorer health, had lower serum 25-OHD levels [23]. However, patients with severe liver disease may have lower levels of vitamin D binding protein as a result of reduced synthetic capacity, and consequently, free vitamin D levels may not be as low as suggested by total serum 25-OHD measurements.
Vitamin D deficiency in patients with chronic kidney disease
In patients with chronic kidney disease (CKD), calcitriol deficiency worsens with declining renal function as a result of glomerular loss [24, 25]. Deficiency of 25-OHD is also common among patients with CKD [13, 14, 25], and lower levels are associated with poorer kidney function [26]. In a population based study, 25-OHD insufficiency was found in 71% of patients with stage 3 and 83% with stage 4 CKD; severe deficiency was found in 14% of patients with stage 3 and 26% with stage 4 CKD [14]. A recent study of patients with chronic kidney disease found a similar prevalence; 39% of patients had 25-OHD between 16 and 30 ng/mL, 33% <16 ng/mL, and 6% <5 ng/mL [13]. Factors that have been associated with low 25-OHD in CKD patients include female sex, African-American race, latitude, season, diabetes, and low serum albumin [25]. Baseline 25-OHD was shown to be an independent predictor of death over 6 years in 168 patients with CKD [26]; however, this finding likely reflects the poorer general health of the subjects with vitamin D deficiency at baseline. Calcitriol treatment is associated with improved mortality in patients on hemodialysis [27, 28] and pre-dialysis patients [29]. However, studies finding a mortality benefit have not differentiated between patients with high turnover and adynamic bone disease. Whether there may be differential effects of treatment with active vitamin D analogies on cardiovascular outcomes or mortality requires further investigation.
Vitamin D deficiency in transplant recipients
The reported prevalence of vitamin D insufficiency after transplant ranges from 51% to 97% and of severe deficiency from 26% to 33% [30–34]. Variability in these estimates relates to the patient population, type of organ transplanted, and assay utilized for measurement of 25-OHD as significant variability exists with commercial assays [35–37]. Transplant recipients are at risk for vitamin D deficiency because of poor health following transplant, which can lead to decreased dietary intake of vitamin D-containing foods. In addition, because of an increased risk of skin cancer in organ transplant recipients, many patients dramatically limit their sun exposure [38, 39]. Furthermore, data from animal studies suggest that glucocorticoids, commonly used for immunosuppression, can increase catabolism of 25-OHD [40, 41]. Vitamin D deficiency in transplant recipients may result in secondary hyperparathyroidism which can further contribute to bone loss and fracture [42]. Patient-specific factors associated with worse vitamin D status after transplant include African-American race [34, 43], avoidance of sun, low dietary intake [33], and transplant during winter months [43]. Not all studies have observed variations related to sun exposure [30], perhaps because in the most severely ill patients there is less variation.
Vitamin D deficiency at the time of organ transplantation
Very few studies have examined vitamin D levels at the time of transplantation. We recently reported that severe vitamin D deficiency was extremely prevalent among heart and liver transplant recipients at the time of transplantation; 91% of patients had vitamin D insufficiency, 55% had deficiency (25-OHD 10 to <20 ng/mL), and 16% had severe deficiency. Liver transplant recipients had significantly lower vitamin D levels than heart transplant recipients (Fig. 1), likely because of disease-related factors such as malabsorption and impaired hepatic 25-hydroxylation of vitamin D [30]. In one study that evaluated vitamin D status in patients at the time of renal transplant, vitamin D insufficiency and deficiency were also prevalent; 59% had 25-OHD <30 ng/mL and 29% had 25-OHD <10 ng/mL [43].
Comparison of serum 25-hydroxy vitamin D levels in heart and liver transplant recipients at the time of organ transplantation. Adapted from Stein et al. [30]
Vitamin D deficiency in long-term transplant recipients
Most studies of vitamin D status in patients after organ transplantation have been performed in kidney transplant recipients and have focused on patients several years after transplantation. Vitamin D deficiency is common and severe in patients after kidney transplantation [31, 34, 44]. In one study, 31 renal transplant recipients, who were on average 7 years post-transplant, were found to have significantly lower levels than age-matched controls [31]. Among transplant recipients, mean serum 25-OHD was 10 ng/mL, and one third of patients had undetectable levels (<4 ng/mL) [31]. Factors associated with low 25-OHD in renal transplant recipients include African-American race [34]; inadequate dietary vitamin D intake, reported in 87–91% of renal transplant recipients [45]; female sex; measurement in autumn and winter months [34]; recent transplantation [44]; proteinuria [46]; and use of ACE inhibitors or aldosterone receptor blockers [44]. Persistent elevations in FGF-23 after kidney transplantation are associated with lower calcitriol levels [47].
Insufficient 25-OHD levels were reported in 97% of cardiac transplant recipients in another recent study. Though not directly associated with vertebral fractures, low 25-OHD was associated with higher PTH, which was significantly associated with vertebral fractures [42]. Relevant metabolic changes that occur after cardiac transplantation include sustained increases in serum creatinine [48–50] and decreases in 1,25(OH)2D [49, 51]. Furthermore, low concentrations of 1,25(OH)2D measured 21 days post-transplantation were associated with 1-year mortality in cardiac transplant recipients (Fig. 2) [51]. Whether this observation reflects a causal relationship between calcitriol and mortality, the effects of calcineurin inhibitors on renal function, or rather the role of low calcitriol as a marker of renal dysfunction or poorer health is unclear.
Kaplan–Meier survival estimates in cardiac transplant recipients according to categories of serum calcitriol concentrations 21 days after transplant (log-rank test P < 0.001). From Zittermann et al. [51]
In long-term liver transplant recipients, 65–68% had 25-OHD levels below 15 ng/mL [32, 52]. Low 25-OHD was associated with low femoral neck Z-score [52]. Biochemical changes following liver transplantation include increases in both 25-OHD and PTH [11, 12, 53, 54]. These increases appear to be sustained for at least 3–4 years following transplantation [11, 53], although some authors have not found significant changes [55–57]. Despite this increase, most authors have found that 25-OHD remains in the insufficient range. Factors associated with vitamin D deficiency in transplant recipients are detailed in Table 1.
Treatment of post-transplant bone loss with vitamin D and analogues
Administration of vitamin D or its analogues is often recommended to prevent or treat osteoporosis after transplantation [58]. There are several potential mechanisms by which vitamin D and its analogues may influence post-transplantation bone loss. They may overcome GC-induced decreases in intestinal calcium absorption, reduce secondary hyperparathyroidism, promote differentiation of osteoblast precursors into mature cells, or influence the immune system and potentiate the immunosuppressive action of calcineurin inhibitors or prednisone, thus reducing the required dose of immunosuppressive drugs [59–61]. There are several limitations common to the interventional studies evaluating treatment of bone loss following transplantation. Most are single-center studies, with small sample sizes. Most importantly, the majority have had inadequate power to detect differences in fracture.
Since the observation or control arm of most studies of bone loss after organ transplantation have included at least 400 IU of parent vitamin D in the post-transplant regimen [62–65], it is clear that the RDA for vitamin D is not sufficient to prevent transplantation osteoporosis. In two recent studies, parent vitamin D, at doses of 800 IU daily in 40 patients [66] or 25,000 IU monthly in 90 patients [67], also did not prevent bone loss after kidney transplantation.
Active forms of vitamin D may be more effective. Calcidiol (25-OHD) prevented bone loss and increased lumbar spine (LS) bone mineral density (BMD) after cardiac transplantation [68]. Alfacalcidiol (1-α-OHD) prevented or attenuated LS and femoral neck (FN) bone loss when given immediately after kidney transplantation [69–71]. De Sevaux et al. [70] found that treatment with alfacalcidiol for the first 6 months following renal transplant resulted in the attenuation of bone loss at the lumbar spine and greater trochanter and prevented loss at the femoral neck (Fig. 3).
Change in bone mineral density in renal transplant recipients treated with calcitriol or placebo (% from baseline ± SE; significance shown for differences between groups at 6 months). From de Sevaux et al. [70]
Studies of calcitriol have found contradictory results, although some report beneficial effects at doses >0.5 μg/day. Calcitriol may be of particular benefit in kidney transplant recipients in whom calcitriol production by the transplanted kidney may be inadequate to suppress excess PTH secretion by hyperplastic parathyroid tissue [72]. Treatment with calcitriol may prevent hyperparathyroidism after both renal [73] and cardiac [62] transplantation. Calcitriol given during the first year after kidney transplantation was associated with an increase in LS, FN, and forearm BMD [74]. In another study of renal transplant recipients, intermittent calcitriol and calcium prevented total hip (TH) but not LS bone loss [75]. In a stratified, placebo-controlled randomized study in which heart and lung transplant recipients received calcitriol or placebo for 12 or 24 months after transplantation [76], LS bone loss was equivalent between groups, and the amount of FN bone loss at 24 months was significantly reduced only in the group that received calcitriol for the entire period. While these results suggest that the protective effects of calcitriol are not sustained after cessation of treatment, we found no bone loss when we discontinued calcitriol after the first post-transplant year [77]. In contrast to the above findings, studies of long-term kidney [78] and heart transplant patients [79, 80] have failed to find any benefit of calcitriol. The randomized trials evaluating vitamin D analogues for prevention of bone loss following transplantation are summarized in Table 2.
The efficacy of vitamin D analogues compared to bisphosphonates has been evaluated by several studies, again with mixed results. In a randomized trial, we found that both alendronate (10 mg daily) and calcitriol (0.25 μg twice daily) given immediately after cardiac transplant provided similar protection against bone loss at the LS, FN, and TH 1 year after transplant (Fig. 4) compared with a reference group receiving only calcium and vitamin D [62]. BMD remained stable during the second year after cardiac transplant, after discontinuation of both drugs [77]. Calcitriol (0.5–0.75 mcg/day) prevented spine and hip bone loss during the first 6 months after heart or lung transplantation and was as effective as cyclic etidronate [64]. Kidney transplant patients treated with alendronate, calcitriol (0.25 μg daily), and calcium carbonate had marked increases in LS BMD compared to decreases in those who received only calcium and calcitriol [81]. A trial of 40 long-term kidney transplant patients who were started on alendronate, calcitriol, and calcium or only calcitriol and calcium approximately 5 years after transplantation documented significant improvements in LS and FN BMD in the alendronate group, while BMD in the other group was stable [82]. In a small, randomized trial of 80 long-term kidney transplant recipients that compared alendronate and alfacalcidiol plus alendronate for 1 year, BMD improved at the LS and FN in both groups. The increase was only significant in the combination alendronate–alfacalcidiol group, however, likely because of inadequate power in this small study [83]. Histomorphometric changes after kidney transplantation were examined in a subset (n = 14) of a larger study of 72 subjects who received calcitriol with or without pamidronate [84]; paired iliac crest bone biopsies were obtained in six subjects randomized to calcitriol plus pamidronate and eight subjects who received calcitriol alone. Pamidronate plus calcitriol was associated with maintenance of trabecular bone structure. Activation frequency at 6 months was lower in subjects who received pamidronate, but was also low in six of eight subjects who received calcitriol alone.
Comparison of mean (±SE) percent change in bone mineral density from baseline in cardiac transplant subjects treated with alendronate or calcitriol and untreated reference group. From Shane et al. [62]
The major side effects of therapy with active vitamin D and analogues are hypercalcemia and hypercalciuria, which may develop suddenly and at any time during the course of treatment. Thus, frequent urinary and serum monitoring is required. If hypercalcemia occurs, it must be recognized and reversed promptly because of the adverse effects on renal function and the life-threatening potential of a severely elevated serum calcium concentration. Given the requirement for serial monitoring, the narrow therapeutic window with respect to hypercalcemia and hypercalciuria, and the demonstrated efficacy of bisphosphonates to prevent post-transplantation bone loss [62, 85], we regard pharmacologic doses of vitamin D and its analogues as adjunctive rather than primary therapy for the prevention and treatment of transplantation osteoporosis. In contrast to active vitamin D metabolites, the therapeutic index for parent vitamin D is wide. Very high and sustained doses of ergocalciferol or cholecalciferol are required to develop toxicity [86].
Deficiency of 25-OHD may complicate treatment of bone loss following transplantation. Bisphosphonates may not be optimally effective in the setting of severe vitamin D deficiency. Furthermore, intravenous bisphosphonate treatment has been reported to precipitate symptomatic hypocalcemia in patients with severe, unrecognized vitamin D deficiency [87].
Effects of vitamin D on immunity and graft rejection
Immune effects of vitamin D
Vitamin D potentiates the innate immune system and has been shown to be protective against bacterial infections and tuberculosis [88]. When 1,25(OH)2D is produced by monocytes and macrophages in sufficient quantities, it has intracellular antimicrobial effects and can also interact with and govern the cytokine profiles of activated T and B lymphocytes in the local environment [89]. The ability of monocytes and macrophages to synthesize 1,25(OH)2D is dependent on the availability of adequate serum concentrations of 25-OHD and increases in response to vitamin D supplementation [89]. Thus, in the setting of insufficient 25-OHD to serve as substrate, there will be a decrease in local production of 1,25(OH)2D. The resultant decreased binding of 1,25(OH)2D to the macrophage vitamin D receptor will result in reduced antimicrobial activity against ingested microbes [89]. This can have deleterious effects on immunity. Of particular importance to transplant recipients is that the antimicrobial actions of 1,25(OH)2D also occur in barrier epithelial cells of the skin [90, 91], gut [92], and lungs [93]. Animals treated with calcitriol were able to resist infection with Candida albicans and herpes simplex virus-1 [94], two common opportunistic infections in transplant patients. In a population study, the prevalence of upper respiratory tract infections was greater in individuals with lower 25-OHD levels [95].
Role of vitamin D in allograft rejection
Recent studies have demonstrated a role for vitamin D in the regulation of immune cell proliferation, differentiation, and responsiveness [5]. Evidence from animal studies suggests that administration of 1,25-dihydroxyvitamin D can prevent acute allograft rejection following liver [96, 97], kidney [98], and heart [99] transplantation. There are limited data from human studies. In kidney transplant recipients, calcitriol supplementation was associated with fewer episodes of acute cellular rejection [100], reduced glucocorticoid requirements [73], and decreased expression of co-stimulatory and HLA-DR molecules, suggesting a possible mechanism for allograft survival [101]. In one study, patients treated with calcitriol following heart transplantation had a reduction in their requirement for cyclosporine [59]. However, we did not observe a reduction in cyclosporine or prednisone dose in our clinical trial of heart transplant recipients treated with calcitriol [62]. In a retrospective study, lower preoperative 25-OHD was associated with increased numbers of moderate to severe rejection episodes in the first 2 months after cardiac transplantation [23]. Those patients who were supplemented with cholecalciferol, in a clinical non-experimental setting, had fewer rejection episodes [23]. Further prospective human studies are needed to explore the role of 1,25(OH)2D and of parent vitamin D in the prevention of graft rejection and infection after transplantation.
Conclusions
Given the high prevalence of 25-OHD deficiency in patients with organ failure prior to and following transplantation, patients should be assessed before transplantation and receive treatment for vitamin D insufficiency and deficiency, if present. In addition, long-term transplant recipients should be monitored and treated for vitamin D deficiency as part of broader management of bone disease. We recommend treatment with parent vitamin D for patients with insufficient 25-OHD (<30 ng/mL) regardless of the type of underlying disease. In patients with stage 3 and 4 CKD (estimated GFR 15–60 mL/min), therapy with an active oral vitamin D analogue (calcitriol, alfacalcidol, or doxercalciferol) should be initiated when serum levels of 25-OHD are sufficient (>30 ng/mL) and plasma levels of intact PTH are above the target range for the CKD stage, as outlined in the K/DOQI guidelines [102]. Patients treated with hemodialysis or peritoneal dialysis with serum levels of intact PTH levels >300 pg/mL should receive an active vitamin D sterol to reduce the serum levels of PTH to a target range of 150–300 pg/mL [102]. For patients with other types of end-organ failure, including liver disease, we suggest replacement with parent vitamin D alone. If monitoring during treatment reveals that 25-OHD is not increasing by the expected amount and is suggestive of a significant impairment in 25-hydroxylase activity, we would consider adding an active vitamin D analogue.
Pharmacologic doses of vitamin D and its analogues have clear utility after renal transplant, but should be utilized as adjunctive rather than primary therapy for osteoporosis in patients after other types of solid organ transplantation because of their narrow therapeutic window and inconsistent efficacy.
There is a need for longitudinal studies to evaluate the efficacy of different repletion regimens to restore 25-OHD levels after transplantation and to examine whether restoring 25-OHD at the time of transplant reduces the development of infectious complications and immunosuppressant requirements. Epidemiologic studies and one randomized controlled clinical trial [103] suggest that adequacy of vitamin D is associated with lower incidence of malignancy [103, 104] as well as cardiovascular disease [105, 106] and mortality [107–109] in healthy populations; these data may be applicable to transplant patients as well. At present, physicians who care for transplant patients should screen all patients for 25-OHD deficiency. Treatment of this condition and subsequent improvement in vitamin D status may reduce skeletal and extraskeletal morbidity in transplant patients.
References
Dhesi JK, Bearne LM, Moniz C, Hurley MV, Jackson SH, Swift CG, Allain TJ (2002) Neuromuscular and psychomotor function in elderly subjects who fall and the relationship with vitamin D status. J Bone Miner Res 17:891–897
Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, Staehelin HB, Bazemore MG, Zee RY, Wong JB (2004) Effect of Vitamin D on falls: a meta-analysis. JAMA 291:1999–2006
Vieth R (1999) Vitamin D supplementation, 25-hydroxyvitamin D concentrations, and safety. Am J Clin Nutr 69:842–856
Holick MF (2007) Vitamin D deficiency. N Engl J Med 357:266–281
Lemire JM (1995) Immunomodulatory actions of 1,25-dihydroxyvitamin D3. J Steroid Biochem Mol Biol 53:599–602
Armas LA, Hollis BW, Heaney RP (2004) Vitamin D2 is much less effective than vitamin D3 in humans. J Clin Endocrinol Metab 89:5387–5391
Holick MF, Biancuzzo RM, Chen TC, Klein EK, Young A, Bibuld D, Reitz R, Salameh W, Ameri A, Tannenbaum AD (2008) Vitamin D2 is as effective as vitamin D3 in maintaining circulating concentrations of 25-hydroxyvitamin D. J Clin Endocrinol Metab 93:677–681
Trang HM, Cole DE, Rubin LA, Pierratos A, Siu S, Vieth R (1998) Evidence that vitamin D3 increases serum 25-hydroxyvitamin D more efficiently than does vitamin D2. Am J Clin Nutr 68:854–858
Shane E, Mancini D, Aaronson K, Silverberg SJ, Seibel MJ, Addesso V, McMahon DJ (1997) Bone mass, vitamin D deficiency and hyperparathyroidism in congestive heart failure. Am J Med 103:197–207
Shane E, Silverberg SJ, Donovan D, Papadopoulos A, Staron RB, Addesso V, Jorgensen B, McGregor C, Shulman L (1996) Osteoporosis in lung transplantation candidates with end stage pulmonary disease. Am J Med 101:262–269
Monegal A, Navasa M, Guanabens N, Peris P, Pons F, Martinez de Osaba MJ, Ordi J, Rimola A, Rodes J, Munoz-Gomez J (2001) Bone disease after liver transplantation: a long-term prospective study of bone mass changes, hormonal status and histomorphometric characteristics. Osteoporos Int 12:484–492
Compston J, Greer S, Skingle S, Stirling D, Price C, Friend P, Alexander G (1996) Early increase in plasma parathyroid hormone level following liver transplantation. J Hepatol 25:715–718
Stavroulopoulos A, Porter CJ, Roe SD, Hosking DJ, Cassidy MJ (2008) Relationship between vitamin D status, parathyroid hormone levels and bone mineral density in patients with chronic kidney disease stages 3 and 4. Nephrol (Carlton) 13:63–67
LaClair RE, Hellman RN, Karp SL, Kraus M, Ofner S, Li Q, Graves KL, Moe SM (2005) Prevalence of calcidiol deficiency in CKD: a cross-sectional study across latitudes in the United States. Am J Kidney Dis 45:1026–1033
Zittermann A, Schleithoff SS, Gotting C, Dronow O, Fuchs U, Kuhn J, Kleesiek K, Tenderich G, Koerfer R (2008) Poor outcome in end-stage heart failure patients with low circulating calcitriol levels. Eur J Heart Fail 10:321–327
Tschopp O, Schmid C, Speich R, Seifert B, Russi EW, Boehler A (2006) Pretransplantation bone disease in patients with primary pulmonary hypertension. Chest 129:1002–1008
Tschopp O, Boehler A, Speich R, Weder W, Seifert B, Russi EW, Schmid C (2002) Osteoporosis before lung transplantation: association with low body mass index, but not with underlying disease. Am J Transplant 2:167–172
Aris RM, Renner JB, Winders AD, Buell HE, Riggs DB, Lester GE, Ontjes DA (1998) Increased rate of fractures and severe kyphosis: sequelae of living into adulthood with cystic fibrosis. Ann Intern Med 128:186–193
Donovan DS Jr, Papadopoulos A, Staron RB, Addesso V, Schulman L, McGregor C, Cosman F, Lindsay RL, Shane E (1998) Bone mass and vitamin D deficiency in adults with advanced cystic fibrosis lung disease. Am J Respir Crit Care Med 157:1892–1899
Ott SM, Aitken ML (1998) Osteoporosis in patients with cystic fibrosis. Clin Chest Med 19:555–567
Forli L, Bjortuft O, Boe J (2009) Vitamin D status in relation to nutritional depletion and muscle function in patients with advanced pulmonary disease. Exp Lung Res 35:524–538
Monegal A, Navasa M, Guanabens N, Peris P, Pons F, MJMd O, Rimola A, Rodes J, Munoz-Gomez J (1997) Osteoporosis and bone mineral metabolism in cirrhotic patients referred for liver transplantation. Calcif Tissue Int 60:148–154
Bitetto D, Fabris C, Falleti E, Fornasiere E, Fumolo E, Fontanini E, Cussigh A, Occhino G, Baccarani U, Pirisi M, Toniutto P (2010) Vitamin D and the risk of acute allograft rejection following human liver transplantation. Liver Int 30:417–444
Hruska KA, Matthew S (2008) Chronic kidney disease mineral bone disorder (CKD-MBD). In: Rosen C (ed) Primer on the metabolic bone diseases and disorders of mineral metabolism. American Society for Bone and Mineral Research, Washington, pp 343–348
Ishimura E, Nishizawa Y, Inaba M, Matsumoto N, Emoto M, Kawagishi T, Shoji S, Okuno S, Kim M, Miki T, Morii H (1999) Serum levels of 1,25-dihydroxyvitamin D, 24,25-dihydroxyvitamin D, and 25-hydroxyvitamin D in nondialyzed patients with chronic renal failure. Kidney Int 55:1019–1027
Ravani P, Malberti F, Tripepi G, Pecchini P, Cutrupi S, Pizzini P, Mallamaci F, Zoccali C (2009) Vitamin D levels and patient outcome in chronic kidney disease. Kidney Int 75:88–95
Teng M, Wolf M, Lowrie E, Ofsthun N, Lazarus JM, Thadhani R (2003) Survival of patients undergoing hemodialysis with paricalcitol or calcitriol therapy. N Engl J Med 349:446–456
Teng M, Wolf M, Ofsthun MN, Lazarus JM, Hernan MA, Camargo CA Jr, Thadhani R (2005) Activated injectable vitamin D and hemodialysis survival: a historical cohort study. J Am Soc Nephrol 16:1115–1125
Kovesdy CP, Ahmadzadeh S, Anderson JE, Kalantar-Zadeh K (2008) Association of activated vitamin D treatment and mortality in chronic kidney disease. Arch Intern Med 168:397–403
Stein EM, Cohen A, Freeby M, Rogers H, Kokolus S, Scott V, Mancini D, Restaino S, Brown R, McMahon DJ, Shane E (2009) Severe vitamin D deficiency among heart and liver transplant recipients. Clin Transplant 23:861–865
Querings K, Girndt M, Geisel J, Georg T, Tilgen W, Reichrath J (2006) 25-Hydroxyvitamin D deficiency in renal transplant recipients. J Clin Endocrinol Metab 91:526–529
Segal E, Baruch Y, Kramsky R, Raz B, Ish-Shalom S (2001) Vitamin D deficiency in liver transplant patients in Israel. Transplant Proc 33:2955–2956
Ewers B, Gasbjerg A, Moelgaard C, Frederiksen AM, Marckmann P (2008) Vitamin D status in kidney transplant patients: need for intensified routine supplementation. Am J Clin Nutr 87:431–437
Tripathi SS, Gibney EM, Gehr TW, King AL, Beckman MJ (2008) High prevalence of vitamin D deficiency in African American kidney transplant recipients. Transplantation 85:767–770
Lips P, Chapuy MC, Dawson-Hughes B, Pols HA, Holick MF (1999) An international comparison of serum 25-hydroxyvitamin D measurements. Osteoporos Int 9:394–397
Binkley N, Krueger D, Cowgill CS, Plum L, Lake E, Hansen KE, DeLuca HF, Drezner MK (2004) Assay variation confounds the diagnosis of hypovitaminosis D: a call for standardization. J Clin Endocrinol Metab 89:3152–3157
Glendenning P, Noble JM, Taranto M, Musk AA, McGuiness M, Goldswain PR, Fraser WD, Vasikaran SD (2003) Issues of methodology, standardization and metabolite recognition for 25-hydroxyvitamin D when comparing the DiaSorin radioimmunoassay and the Nichols Advantage automated chemiluminescence protein-binding assay in hip fracture cases. Ann Clin Biochem 40:546–551
Reichrath J (2010) Dermatologic management, sun avoidance and vitamin D status in organ transplant recipients (OTR). J Photochem Photobiol B 101:150–159
Courbebaisse M, Souberbielle JC, Thervet E (2010) Potential nonclassical effects of vitamin D in transplant recipients. Transplantation 89:131–137
Akeno N, Matsunuma A, Maeda T, Kawane T, Horiuchi N (2000) Regulation of vitamin D-1alpha-hydroxylase and -24-hydroxylase expression by dexamethasone in mouse kidney. J Endocrinol 164:339–348
Pascussi JM, Robert A, Nguyen M, Walrant-Debray O, Garabedian M, Martin P, Pineau T, Saric J, Navarro F, Maurel P, Vilarem MJ (2005) Possible involvement of pregnane X receptor-enhanced CYP24 expression in drug-induced osteomalacia. J Clin Invest 115:177–186
Giannini S, Sella S, Netto FS, Cattelan C, Dalle Carbonare L, Lazzarin R, Marchini F, Rigotti P, Marcocci C, Cetani F, Pardi E, D’Angelo A, Realdi G, Bonfante L (2010) Persistent secondary hyperparathyroidism and vertebral fractures in kidney transplantation: role of calcium-sensing receptor polymorphisms and vitamin D deficiency. J Bone Miner Res 25:841–848
Sadlier DM, Magee CC (2007) Prevalence of 25(OH) vitamin D (calcidiol) deficiency at time of renal transplantation: a prospective study. Clin Transplant 21:683–688
Marcen R, Ponte B, Rodriguez-Mendiola N, Fernandez-Rodriguez A, Galeano C, Villafruela JJ, Teruel JL, Burgos FJ, Ortuno J (2009) Vitamin D deficiency in kidney transplant recipients: risk factors and effects of vitamin D3 supplements. Transplant Proc 41:2388–2390
Lynch IT, Eustace JA, Plant WD, Cashman KD, O’Keefe M, Lordan S, Moloney R (2007) Inadequate dietary calcium and vitamin D intakes in renal-transplant recipients in Ireland. J Ren Nutr 17:408–415
Sezer S, Yavuz D, Canoz MB, Ozdemir FN, Haberal M (2009) Vitamin D status, bone mineral density, and inflammation in kidney transplantation patients. Transplant Proc 41:2823–2825
Bhan I, Shah A, Holmes J, Isakova T, Gutierrez O, Burnett SM, Juppner H, Wolf M (2006) Post-transplant hypophosphatemia: tertiary ‘hyper-phosphatoninism’? Kidney Int 70:1486–1494
Sambrook PN, Kelly PJ, Fontana D, Nguyen T, Keogh A, Macdonald D, Spratt P, Freund J, Eisman JA (1994) Mechanisms of rapid bone loss following cardiac transplantation. Osteoporos Int 4:273–276
Shane E, Rivas M, McMahon DJ, Staron RB, Silverberg SJ, Seibel MJ, Mancini D, Michler R, Aaronson K, Addesso V, Lo SH (1997) Bone loss and turnover after cardiac transplantation. J Clin Endocrinol Metab 82:1497–1506
Valimaki MJ, Kinnunen K, Tahtela R, Loyttyniemi E, Laitinen K, Makela P, Keto P, Nieminen M (1999) A prospective study of bone loss and turnover after cardiac transplantation: effect of calcium supplementation with or without calcitonin. Osteoporos Int 10:128–136
Zittermann A, Schleithoff SS, Gotting C, Fuchs U, Kuhn J, Kleesiek K, Tenderich G, Koerfer R (2009) Calcitriol deficiency and 1-year mortality in cardiac transplant recipients. Transplantation 87:118–124
Segal E, Baruch Y, Kramsky R, Raz B, Tamir A, Ish-Shalom S (2003) Predominant factors associated with bone loss in liver transplant patients—after prolonged post-transplantation period. Clin Transplant 17:13–19
Guichelaar MM, Kendall R, Malinchoc M, Hay JE (2006) Bone mineral density before and after OLT: long-term follow-up and predictive factors. Liver Transplant 12:1390–1402
Floreani A, Mega A, Tizian L, Burra P, Boccagni P, Baldo V, Fagiuoli S, Naccarato R, Luisetto G (2001) Bone metabolism and gonad function in male patients undergoing liver transplantation: a two-year longitudinal study. Osteoporos Int 12:749–754
Hawkins FG, Leon M, Lopez MB, Valero MA, Larrodera L, Garcia-Garcia I, Loinaz C, Gonzales EM (1994) Bone loss and turnover in patients with liver transplantation. Hepato Gastroenterol 41:158–161
Meys E, Fontanges E, Fourcade N, Thomasson A, Pouyet M, Delmas P (1994) Bone loss after orthotopic liver transplantation. Am J Med 97:445–450
Valero M, Loinaz C, Larrodera L, Leon M, Morena E, Hawkins F (1995) Calcitonin and bisphosphonate treatment in bone loss after liver transplantation. Calcif Tissue Int 57:15–19
Sambrook P (1999) Alfacalcidol and calcitriol in the prevention of bone loss after organ transplantation. Calcif Tissue Int 65:341–343
Briffa NK, Keogh AM, Sambrook PN, Eisman JA (2003) Reduction of immunosuppressant therapy requirement in heart transplantation by calcitriol. Transplantation 75:2133–2134
Lemire JM (1992) Immunomodulatory role of 1,25 dihydroxyvitamin D3. J Cell Biochem 49:26–31
Lemire JM, Archer DC, Reddy GS (1994) Dihydroxy-24-oxo-16-ene-vitamin D3, a renal metabolite of the vitamin D analog 1, 25-dihydroxy-16ene-vitamin D3, exerts immunosuppressive activity equal to its parent without causing hypercalcemia in vivo. Endocrinology 135:2818–2821
Shane E, Addesso V, Namerow PB, McMahon DJ, Lo SH, Staron RB, Zucker M, Pardi S, Maybaum S, Mancini D (2004) Alendronate versus calcitriol for the prevention of bone loss after cardiac transplantation. N Engl J Med 350:767–776
Krieg MA, Seydoux C, Sandini L, Goy JJ, Berguer DG, Thiebaud D, Burckhardt P (2001) Intravenous pamidronate as treatment for osteoporosis after heart transplantation: a prospective study. Osteoporos Int 12:112–116
Henderson K, Eisman J, Keogh A, MacDonald P, Glanville A, Spratt P, Sambrook P (2001) Protective effect of short-term calcitriol or cyclical etidronate on bone loss after cardiac or lung transplantation. J Bone Miner Res 16:565–571
Shane E, Papadopoulos A, Staron RB, Addesso V, Donovan D, McGregor C, Schulman LL (1999) Bone loss and fracture after lung transplantation. Transplantation 68:220–227
Al-Gabri S, Zadrazil J, Krejci K, Horak P, Bachleda P (2005) Changes in bone mineral density and selected metabolic parameters over 24 months following renal transplantation. Transplant Proc 37:1014–1019
Wissing KM, Broeders N, Moreno-Reyes R, Gervy C, Stallenberg B, Abramowicz D (2005) A controlled study of vitamin D3 to prevent bone loss in renal-transplant patients receiving low doses of steroids. Transplantation 79:108–115
Garcia-Delgado I, Prieto S, Gil-Fraguas L, Robles E, Rufilanchas JJ, Hawkins F (1997) Calcitonin, etidronate, and calcidiol treatment in bone loss after cardiac transplantation. Calcif Tissue Int 60:155–159
El-Agroudy AE, El-Husseini AA, El-Sayed M, Ghoneim MA (2003) Preventing bone loss in renal transplant recipients with vitamin D. J Am Soc Nephrol 14:2975–2979
De Sevaux RG, Hoitsma AJ, Corstens FH, Wetzels JF (2002) Treatment with vitamin D and calcium reduces bone loss after renal transplantation: a randomized study. J Am Soc Nephrol 13:1608–1614
El-Agroudy AE, El-Husseini AA, El-Sayed M, Mohsen T, Ghoneim MA (2005) A prospective randomized study for prevention of postrenal transplantation bone loss. Kidney Int 67:2039–2045
Fleseriu M, Licata AA (2007) Failure of successful renal transplant to produce appropriate levels of 1,25-dihydroxyvitamin D. Osteoporos Int 18:363–368
Uyar M, Sezer S, Arat Z, Elsurer R, Ozdemir FN, Haberal M (2006) 1,25-Dihydroxyvitamin D(3) therapy is protective for renal function and prevents hyperparathyroidism in renal allograft recipients. Transplant Proc 38:2069–2073
Josephson MA, Schumm LP, Chiu MY, Marshall C, Thistlethwaite JR, Sprague SM (2004) Calcium and calcitriol prophylaxis attenuates posttransplant bone loss. Transplantation 78:1233–1236
Torres A, Garcia S, Gomez A, Gonzalez A, Barrios Y, Concepcion MT, Hernandez D, Garcia JJ, Checa MD, Lorenzo V, Salido E (2004) Treatment with intermittent calcitriol and calcium reduces bone loss after renal transplantation. Kidney Int 65:705–712
Sambrook P, Henderson NK, Keogh A, MacDonald P, Glanville A, Spratt P, Bergin P, Ebeling P, Eisman J (2000) Effect of calcitriol on bone loss after cardiac or lung transplantation. J Bone Miner Res 15:1818–1824
Cohen A, Addesso V, McMahon DJ, Staron RB, Namerow P, Maybaum S, Mancini D, Shane E (2006) Discontinuing antiresorptive therapy one year after cardiac transplantation: effect on bone density and bone turnover. Transplantation 81:686–691
Cueto-Manzano AM, Konel S, Freemont AJ, Adams JE, Mawer B, Gokal R, Hutchison AJ (2000) Effect of 1,25-dihydroxyvitamin D3 and calcium carbonate on bone loss associated with long-term renal transplantation. Am J Kidney Dis 35:227–236
Stempfle HU, Werner C, Siebert U, Assum T, Wehr U, Rambeck WA, Meiser B, Theisen K, Gartner R (2002) The role of tacrolimus (FK506)-based immunosuppression on bone mineral density and bone turnover after cardiac transplantation: a prospective, longitudinal, randomized, double-blind trial with calcitriol. Transplantation 73:547–552
Stempfle HU, Werner C, Echtler S, Wehr U, Rambeck WA, Siebert U, Uberfuhr P, Angermann CE, Theisen K, Gartner R (1999) Prevention of osteoporosis after cardiac transplantation: a prospective, longitudinal, randomized, double-blind trial with calcitriol. Transplantation 68:523–530
Kovac D, Lindic J, Kandus A, Bren AF (2001) Prevention of bone loss in kidney graft recipients. Transplant Proc 33:1144–1145
Giannini S, Dangel A, Carraro G, Nobile M, Rigotti P, Bonfante L, Marchini F, Zaninotto M, Dalle Carbonare L, Sartori L, Crepaldi G (2001) Alendronate prevents further bone loss in renal transplant recipients. J Bone Miner Res 16:2111–2117
Trabulus S, Altiparmak MR, Apaydin S, Serdengecti K, Sariyar M (2008) Treatment of renal transplant recipients with low bone mineral density: a randomized prospective trial of alendronate, alfacalcidol, and alendronate combined with alfacalcidol. Transplant Proc 40:160–166
Coco M, Glicklich D, Faugere MC, Burris L, Bognar I, Durkin P, Tellis V, Greenstein S, Schechner R, Figueroa K, McDonough P, Wang G, Malluche H (2003) Prevention of bone loss in renal transplant recipients: a prospective, randomized trial of intravenous pamidronate. J Am Soc Nephrol 14:2669–2676
Crawford BA, Kam C, Pavlovic J, Byth K, Handelsman DJ, Angus PW, McCaughan GW (2006) Zoledronic acid prevents bone loss after liver transplantation: a randomized, double-blind, placebo-controlled trial. Ann Intern Med 144:239–248
Vieth R (2007) Vitamin D toxicity, policy, and science. J Bone Miner Res 22(Suppl 2):V64–V68
Breen TL, Shane E (2004) Prolonged hypocalcemia after treatment with zoledronic acid in a patient with prostate cancer and vitamin D deficiency. J Clin Oncol 22:1531–1532
Bikle DD (2008) Vitamin D and the immune system: role in protection against bacterial infection. Curr Opin Nephrol Hypertens 17:348–352
Adams JS, Hewison M (2010) Update in vitamin D. J Clin Endocrinol Metab 95:471–478
Peric M, Koglin S, Kim SM, Morizane S, Besch R, Prinz JC, Ruzicka T, Gallo RL, Schauber J (2008) IL-17A enhances vitamin D3-induced expression of cathelicidin antimicrobial peptide in human keratinocytes. J Immunol 181:8504–8512
Schauber J, Oda Y, Buchau AS, Yun QC, Steinmeyer A, Zugel U, Bikle DD, Gallo RL (2008) Histone acetylation in keratinocytes enables control of the expression of cathelicidin and CD14 by 1,25-dihydroxyvitamin D3. J Invest Dermatol 128:816–824
Liu N, Nguyen L, Chun RF, Lagishetty V, Ren S, Wu S, Hollis B, DeLuca HF, Adams JS, Hewison M (2008) Altered endocrine and autocrine metabolism of vitamin D in a mouse model of gastrointestinal inflammation. Endocrinology 149:4799–4808
Hansdottir S, Monick MM, Hinde SL, Lovan N, Look DC, Hunninghake GW (2008) Respiratory epithelial cells convert inactive vitamin D to its active form: potential effects on host defense. J Immunol 181:7090–7099
Cantorna MT, Hullett DA, Redaelli C, Brandt CR, Humpal-Winter J, Sollinger HW, Deluca HF (1998) 1,25-Dihydroxyvitamin D3 prolongs graft survival without compromising host resistance to infection or bone mineral density. Transplantation 66:828–831
Ginde AA, Mansbach JM, Camargo CA Jr (2009) Association between serum 25-hydroxyvitamin D level and upper respiratory tract infection in the Third National Health and Nutrition Examination Survey. Arch Intern Med 169:384–390
Zhang AB, Zheng SS, Jia CK, Wang Y (2003) Effect of 1,25-dihydroxyvitamin D3 on preventing allograft from acute rejection following rat orthotopic liver transplantation. World J Gastroenterol 9:1067–1071
Redaelli CA, Wagner M, Tien YH, Mazzucchelli L, Stahel PF, Schilling MK, Dufour JF (2001) 1 alpha, 25-Dihydroxycholecalciferol reduces rejection and improves survival in rat liver allografts. Hepatology 34:926–934
Becker BN, Hullett DA, O’Herrin JK, Malin G, Sollinger HW, DeLuca H (2002) Vitamin D as immunomodulatory therapy for kidney transplantation. Transplantation 74:1204–1206
Hullett DA, Cantorna MT, Redaelli C, Humpal-Winter J, Hayes CE, Sollinger HW, Deluca HF (1998) Prolongation of allograft survival by 1,25-dihydroxyvitamin D3. Transplantation 66:824–828
Tanaci N, Karakose H, Guvener N, Tutuncu NB, Colak T, Haberal M (2003) Influence of 1,25-dihydroxyvitamin D3 as an immunomodulator in renal transplant recipients: a retrospective cohort study. Transplant Proc 35:2885–2887
Ahmadpoor P, Ilkhanizadeh B, Ghasemmahdi L, Makhdoomi K, Ghafari A (2009) Effect of active vitamin D on expression of co-stimulatory molecules and HLA-DR in renal transplant recipients. Exp Clin Transplant 7:99–103
National Kidney Foundation (2003) K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis 42:1–201
Lappe JM, Travers-Gustafson D, Davies KM, Recker RR, Heaney RP (2007) Vitamin D and calcium supplementation reduces cancer risk: results of a randomized trial. Am J Clin Nutr 85:1586–1591
Wactawski-Wende J, Kotchen JM, Anderson GL, Assaf AR, Brunner RL, O’Sullivan MJ, Margolis KL, Ockene JK, Phillips L, Pottern L, Prentice RL, Robbins J, Rohan TE, Sarto GE, Sharma S, Stefanick ML, Van Horn L, Wallace RB, Whitlock E, Bassford T, Beresford SA, Black HR, Bonds DE, Brzyski RG, Caan B, Chlebowski RT, Cochrane B, Garland C, Gass M, Hays J, Heiss G, Hendrix SL, Howard BV, Hsia J, Hubbell FA, Jackson RD, Johnson KC, Judd H, Kooperberg CL, Kuller LH, LaCroix AZ, Lane DS, Langer RD, Lasser NL, Lewis CE, Limacher MC, Manson JE (2006) Calcium plus vitamin D supplementation and the risk of colorectal cancer. N Engl J Med 354:684–696
Pilz S, Dobnig H, Fischer JE, Wellnitz B, Seelhorst U, Boehm BO, Marz W (2008) Low vitamin D levels predict stroke in patients referred to coronary angiography. Stroke 39:2611–2613
Pilz S, Marz W, Wellnitz B, Seelhorst U, Fahrleitner-Pammer A, Dimai HP, Boehm BO, Dobnig H (2008) Association of vitamin D deficiency with heart failure and sudden cardiac death in a large cross-sectional study of patients referred for coronary angiography. J Clin Endocrinol Metab 93:3927–3935
Dobnig H, Pilz S, Scharnagl H, Renner W, Seelhorst U, Wellnitz B, Kinkeldei J, Boehm BO, Weihrauch G, Maerz W (2008) Independent association of low serum 25-hydroxyvitamin D and 1,25-dihydroxyvitamin d levels with all-cause and cardiovascular mortality. Arch Intern Med 168:1340–1349
Autier P, Gandini S (2007) Vitamin D supplementation and total mortality: a meta-analysis of randomized controlled trials. Arch Intern Med 167:1730–1737
Virtanen JK, Nurmi T, Voutilainen S, Mursu J, Tuomainen TP (2010) Association of serum 25-hydroxyvitamin D with the risk of death in a general older population in Finland. Eur J Nutr Oct 26. doi:10.1007/s00394-010-0138-3
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stein, E.M., Shane, E. Vitamin D in organ transplantation. Osteoporos Int 22, 2107–2118 (2011). https://doi.org/10.1007/s00198-010-1523-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-010-1523-8