Abstract
Summary
A high circulating osteoprotegerin (OPG) level may be a risk factor for vascular calcification and mortality in hemodialysis patients. OPG and pulse wave velocity (PWV) were measured at baseline in 151 normoalbuminemic, long-term (>3 years) Japanese hemodialysis patients who were prospectively followed for 6 years. In long-term normoalbuminemic Japanese hemodialysis patients, OPG levels were strongly linked with both arterial stiffness and worse outcome.
Introduction
A high circulating OPG level is reported to be a risk factor for vascular calcification and mortality in Western chronic kidney disease (CKD) patients but it is not known if this is true for Japanese CKD patients, where a different risk profile may operate.
Methods
OPG and PWV were measured at baseline in 151 normoalbuminemic, long-term (>3 years) Japanese hemodialysis patients (median age 62 years) who were prospectively followed for 6 years.
Results
OPG levels were associated in multivariate analysis with age, dialysis vintage, history of cardiovascular disease (CVD) and parathyroid hormone levels. C-reactive protein levels did not correlate with OPG. Patients with clinical history of CVD had significantly higher OPG levels and OPG levels were positively correlated to PWV, an index of arterial stiffness. These associations were independent of age, sex, dialysis vintage, and diabetes. During the follow-up period, 40 deaths, including 25 cardiovascular deaths, were recorded. In crude analysis, each unit of increase in OPG was associated with increased all-cause (hazard ratios 1.14, 95% confidence interval 1.08–1.20) and CVD mortality (1.14 [1.07–1.21]), which persisted after adjustment for age, sex, dialysis vintage, diabetes, and baseline CVD (1.12 [1.05–1.19] and 1.11 [1.02–1.19], all-cause and CVD mortality, respectively).
Conclusions
In long-term normoalbuminemic Japanese hemodialysis patients, with low prevalence of inflammation, OPG levels were strongly linked with both arterial stiffness and worse outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with chronic kidney disease (CKD) have a high risk of dying prematurely due to cardiovascular disease (CVD) and one strong contributing factor is vascular calcification resulting in arterial stiffness [1]. Vascular calcification in CKD patients may be caused by underlying conditions (such as diabetes mellitus, atherosclerosis, inflammation, and certain medications) as well as by uremic disorders in bone and mineral metabolism including those of calcium, phosphate, parathyroid hormone (PTH), vitamin D, and proteins related to bone turnover and vascular calcification, such as osteoprotegerin (OPG) [1]. Pulse wave velocity (PWV) is often used as a surrogate indicator of arterial stiffness in CKD patients [2], and is a strong predictor of CVD mortality in hemodialysis (HD) patients [3].
Osteoprotegerin (OPG) is a member of the tumor necrosis factor receptor family and a decoy receptor that blocks the interaction between the receptor activator of nuclear factor-κB with its ligand, thus inhibiting osteoclast differentiation and activity [4, 5]. On the other hand, OPG knockout mouse exhibited an increase of arterial calcification [6, 7] which was prevented by experimentally obtained increased expression of OPG [7]. Despite this apparent protective effect on the vascular system and bone, the increased levels of circulating OPG levels in CKD patients [8] are reported to be associated with both aortic calcification [9, 10] and increased mortality [11, 12].
Although arterial calcification is highly prevalent in Japanese dialysis patients [13], mortality rates are much lower than in Western dialysis patients [14] suggesting that mortality risk factors may differ between these populations perhaps due to differences in genetic factors, nutrition, and life-style. OPG has been identified as a mortality risk factor in Western HD patients [11, 12], but this association is modified by the presence of concurrent inflammation [11, 15]. At present, it is unknown whether this is the case in Japanese patients as well, in whom, inflammation is a less common finding [16].
The aim of the present study was to look into the associations between OPG levels, arterial stiffness, and mortality in a cohort of long-term HD patients with normal albumin levels.
Subjects and methods
Study patients
This cross-sectional study with mortality follow-up including 151 ethnically Japanese HD patients from the Hakuai Hospital (currently: Hakuai Clinic, Kure, Japan). Inclusion criteria were long-term HD patients (over 3 years on HD) [8], normal albumin levels (serum albumin level ≥ 35 g/L) [17], and not receiving intravenous active vitamin D therapy [18]. There were no patients who had evidence of acute infection at time of inclusion and none of the patients had undergone continuous ambulatory peritoneal dialysis or renal transplantation. Study entry and baseline sampling occurred in 1st July 2003. In a next step, patients were prospectively followed-up for mortality assessment until 30th July 2009. Cardiovascular mortality was defined as death resulting from coronary heart disease or congestive heart failure or stroke. This study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the hospital ethics committee. Signed informed consent was obtained from all patients before inclusion in this study.
Forty-three (29%) of the 151 patients presented diabetes mellitus at baseline, whereas 50 (33%) had a clinical history of CVD. Patients were treated with HD three times a week (4 h per session) using bicarbonate dialysate and high-flux dialysis membranes.
Biochemical parameters
Venous blood samples were collected before the HD session for routine measurement of serum concentrations of albumin (bromocresol purple), total cholesterol, high-density lipoprotein cholesterol (HDL cholesterol), calcium, phosphate, and C-reactive protein (CRP). The intact-parathyroid hormone (intact-PTH) was measured with a commercial kit from Roche Diagnostics (Tokyo, Japan). OPG was measured in duplicates using a sandwich enzyme immunoassay from Immundiagnostik (Bensheim, Germany) that employed two highly specific antibodies for human OPG. The adjusted calcium levels were calculated using Payne's formula [19] and the low-density lipoprotein cholesterol (LDL cholesterol) level was calculated using Friedewald's formula [20].
Brachial–ankle pulse wave velocity and ankle–brachial pressure index
Before HD, after resting for at least 10 min, PWV and ankle–brachial pressure index (ABI) was measured as previously described [21, 22] using a Vasera VS-1000 (Fukuda Denshi, Tokyo, Japan) which simultaneously recorded the PWV, ABI, blood pressure, electrocardiogram, and heart sounds. Normal ABI is defined as >0.9 [21]. An ABI <0.9 suggests the presence of arteriosclerosis obliterans, and in patients with such values the PWV measurement is underestimated.
Statistical analysis
All variables were expressed as the mean ± SD or median (25th and 75th percentile), unless otherwise indicated. Statistical significance was set at the level of P < 0.05. We used non-parametric Spearman's rank correlation analysis to determine the degree of association between OPG and other variables. Multivariate regression linear and logistic analyses were used to assess independent predictors of OPG, PWV, and clinical history of CVD. For these analyses, age, dialysis vintage, BMI, albumin, total cholesterol, phosphate, and intact-PTH were dichotomized according to median values. Restricted cubic splines were used to evaluate nonlinear relationships between OPG levels and outcome [23]. We chose four knots at quartiles, which have been suggested to offer adequate fit of the model and are good compromise between flexibility and loss of precision caused by overfitting a small sample. Thereafter, univariate and multivariate Cox regression analyses were presented as hazard ratio (HR) and 95% confidence interval (CI), using OPG concentrations as a continuous variable. All statistical analyses were performed using statistical software SAS version 9.2 (SAS Campus Drive, Cary, North Carolina, USA).
Results
Clinical characteristics and correlates of osteoprotegerin levels
Clinical characteristics of the 151 HD patients included in the study are summarized in Table 1. The levels of OPG presented a median value of 10.5 (25th–75th percentiles 7.3 to 15.1) pmol/L. Univariate correlations as assessed by Spearman's rank test are also shown in Table 1. Briefly, OPG levels were positively associated with age, dialysis vintage, clinical history of CVD and PWV, and negatively associated with body mass index (BMI), albumin, total cholesterol, phosphate, intact-PTH and ABI. CRP values were very low for all patients and did not associate with OPG concentration.
Using variables associated with OPG in univariate analysis, we performed a multivariate regression predicting for OPG (pmol/L; Table 2). Results showed independent associations of OPG with age, dialysis vintage, clinical history of CVD, and intact-PTH, but not with sex, diabetes mellitus, BMI, albumin, total cholesterol, and phosphate.
Patients with a clinical history of CVD had higher OPG levels as compared with those with no history of CVD (13.6 [8.6 to 18.5] vs. 9.4 [6.5 to 13.4] pmol/L; P < 0.001). In a logistic regression model, such association remained and was independent of age, sex, dialysis vintage, and diabetes (Table 3).
One hundred and 38 patients had a normal ABI, defined as ABI > 0.9 [21] and PWV was assessed in those. In these 138 patients, OPG levels were positively correlated to PWV (Table 1 and Fig. 1). The association between PWV (m/s) and OPG (pmol/L) was independent (estimate for OPG = 0.169, Standard error = 0.071, P = 0.018) after inclusion of age, sex, dialysis vintage, and diabetes mellitus in a multivariate regression model (Table 4).
Osteoprotegerin levels and clinical outcome
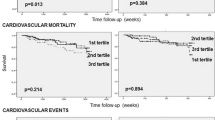
During 6 years of follow-up, 40 patients died due to cardiovascular causes [n = 25: acute myocardial infarction (n = 10), chronic heart failure (n = 5), dissecting aortic aneurysm (n = 1), cerebral infarction (n = 6), cerebral hemorrhage (n = 3)], malignancies (n = 3), infectious diseases (n = 7) and other (n = 5). Three patients who underwent kidney transplantation and two patients who were transferred to another hospital were censored. When presenting data as an age- and sex-adjusted restricted cubic spline curve, we could observe that increasing OPG concentrations had an impact on all-cause mortality (Fig. 2). Cox regression analysis revealed that patients with high OPG levels had increased all-cause and CVD-related mortality, which persisted after adjustment for age, sex, dialysis vintage, diabetes mellitus, and clinical history of CVD (Table 5).
Discussion
This is the first report linking high OPG concentrations with increased mortality in Japanese HD patients. At the time of study initiation, there was no evidence linking OPG concentrations and mortality in dialysis patients. However, during the follow-up period several reports have now documented such relationship in both chronic HD [11, 12] and pre-dialysis CKD stages [15, 24, 25]. It is interesting to pinpoint, however, that while previous studies have suggested that OPG concentrations are influenced by residual renal function [8], malnutrition [17], inflammation [11, 15], and intravenous maxacalcitol therapy [18], none of these conditions were present in our patient population. Thus, a strength of our study is that our conclusions are based on less biased and therefore more robust associations between OPG, arterial stiffness, and outcome. Our results also further reinforce the involvement of a high OPG concentration in the mortality risk of HD patients by the demonstrated association with both the presence of clinically evident CVD and arterial stiffness.
It should be noted that these associations were statistically significant despite the low mortality risk of Japanese as compared to Western HD patients. The mortality rate of our patients (4.4/100 patient years) agrees with, but is even lower, than the reported Japanese mortality rate for HD patients (6.6/100 patient years) [14], presumably attributed to the exclusion of hypoalbuminemic patients. Another phenotypical feature which deviates from typical findings in Western HD patients is that CRP had a median value of 1.0 mg/L, in line with the lower prevalence of inflammation in Japanese CKD patients [16]. Thus, the patients in the current study are unlikely to present with the malnutrition, inflammation, and atherosclerosis syndrome. Recent studies suggested that OPG levels were associated to mortality only in the presence of concurrent inflammation [11, 15], leading to the hypothesis that low-grade persistent inflammation serves as a catalyst and modifies/exacerbates the atherosclerosis process [15, 26]. However, the current study cannot confirm this hypothesis as OPG was related to increased mortality risk in a group of well-nourished and uninflamed HD Japanese patients.
Our study also shows that OPG in multivariate analyses was associated with arterial stiffness as well as both clinically evident CVD and CVD mortality. Extending this, a recent Japanese report associated OPG concentrations with the prediction of non-fatal CVD events in HD patients [27], while others have suggested similar associations using different surrogates of arterial calcification in chronic HD patients [9, 10, 12]. The cross-sectional nature of this analysis precludes us from inferring whether these factors are causally linked. However, the hypothesis that OPG may be causing vascular calcification in these patients by inhibiting bone remodeling is not consistent with the known actions of OPG. In animal models, absence of OPG increases vascular calcification [6], while excess levels reduce vascular calcification [7] even in the face of acute challenges [28]. In addition, the circulating levels of OPG observed are likely too low to have a systemic effect and may reflect low levels of escape from local tissue sources, perhaps vessels themselves. Thus, it would seem more likely that the observed association with vascular mortality represents a compensatory, rather than causative relationship.
Some limitations of the present study should be noted, including the abovementioned cross-sectional design, and the fact that fatal cardiovascular events are recorded based on patient records and not confirmed by autopsies, probably underestimating the true prevalence of cardiac endpoints. Another limitation is the lack of repeated measurements of both OPG levels and PWV during follow-up, which would have enabled us to make a stronger case. In summary, we report that in normoalbuminemic Japanese HD patients with no apparent inflammation, circulating OPG levels are independent prognosticators of all-cause and CVD-related mortality, being closely related also to the degree of arterial stiffness. These conclusions, while in agreement with observations in non-Japanese and thus ethnically different CKD populations, are based on more unbiased relationships and strengthened by the fact that several reported confounders of OPG levels, such as malnutrition or inflammation were excluded or not present.
References
Cannata-Andía JB, Rodríguez-García M, Carrillo-López N, Naves-Díaz M, Díaz-López B (2006) Vascular calcifications: pathogenesis, management, and impact on clinical outcomes. J Am Soc Nephrol 17:S267–S273
Blacher J, Demuth K, Guerin AP, Safar ME, Moatti N, London GM (1998) Influence of biochemical alterations on arterial stiffness in patients with end-stage renal disease. Arterioscler Thromb Vasc Biol 18:535–541
London GM, Marchais SJ, Guerin AP, Pannier B (2004) Arterial stiffness: pathophysiology and clinical impact. Clin Exp Hypertens 26:689–699
Simonet WS, Lacey DL, Dunstan CR et al (1997) Osteoprotegerin: a novel secreted protein involved in the regulation of bone density. Cell 89:309–319
Lacey DL, Timms E, Tan HL et al (1998) Osteoprotegerin ligand is a cytokine that regulates osteoclast differentiation and activation. Cell 93:165–176
Bucay N, Sarosi I, Dunstan CR et al (1998) Osteoprotegerin-deficient mice develop early onset osteoporosis and arterial calcification. Genes Dev 12:1260–1268
Min H, Morony S, Sarosi I et al (2000) Osteoprotegerin reverses osteoporosis by inhibiting endosteasl osteoclasts and prevents vascular calcification by blocking a process resembling osteoclastogenesis. J Exp Med 192:463–474
Kazama JJ, Shigematsu T, Yano K et al (2002) Increased circulating levels of osteoclastogenesis inhibitory factor (osteoprotegerin) in patients with chronic renal failure. Am J Kidney Dis 39:525–532
Nitta K, Akiba T, Uchida K et al (2003) The progression of vascular calcification and serum osteoprotegerin levels in patients on long-term hemodialysis. Am J Kidney Dis 42:303–309
Barreto DV, Barreto FC, Carvalho AB et al (2005) Coronary calcification in hemodialysis patients: the contribution of traditional and uremia-related risk factors. Kidney Int 67:1576–1582
Morena M, Terrier N, Jaussent I et al (2006) Plasma osteoprotegerin is associated with mortality in hemodialysis patients. J Am Soc Nephrol 17:262–270
Speer G, Fekete BC, El Hadj Othmane T et al (2008) Serum osteoprotegerin level, carotid-femoral pulse wave velocity and cardiovascular survival in haemodialysis patients. Nephrol Dial Transplant 23:3256–3262
Nakamura S, Ishibashi-Ueda H, Niizuma S, Yoshihara F, Horio T, Kawano Y (2009) Coronary calcification in patients with chronic kidney disease and coronary artery disease. Clin J Am Soc Nephrol 4:1892–1900
Coodkin DA, Bragg-Gresham JL, Koenig KG et al (2003) Association of comorbid conditions and mortality in hemodialysis patients in Europe, Japan, and the United States: The dialysis outcomes and practice patterns study (DOPPS). J Am Soc Nephrol 14:3270–3277
Matsubara K, Stenvinkel P, Qureshi AR et al (2009) Inflammation modifies the association of osteoprotegerin with mortality in chronic kidney disease. J Nephrol 22:774–782
Honda H, Ueda M, Kojima S et al (2009) Assessment of myeloperoxidase and oxidative alpha1-antitrypsin in patients on hemodialysis. Clin J Am Soc Nephrol 4:142–151
Misra M, Soyka LA, Miller KK et al (2003) Serum osteoprotegerin in adolescent girls with anorexia nervosa. J Clin Endocrinol Metab 88:3816–3832
Kazama JJ, Omori K, Takahashi N et al (2005) Maxacalcitol therapy decreases circulating osteoprotegerin levels in dialysis patients with secondary hyperparathyroidism. Clin Nephrol 64:64–68
Payne RB, Little AJ, Williams RB, Milner JR (1973) Interpretation of serum calcium in patients with abnormal serum proteins. Br Med J 4:643–646
Friedewald WT, Levy RI, Fredrickson DS (1972) Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18:499–502
Yamashina A, Tomiyama H, Takeda K et al (2002) Validity, reproducibility, and clinical significance of noninvasive brachial–ankle pulse wave velocity measurement. Hypertens Res 25:359–364
Suzuki E, Kashiwagi A, Nishio Y et al (2001) Increased arterial wall stiffness limits flow volume in the lower extremities in type 2 diabetic patients. Diab Care 24:2107–2114
Heinzl H, Kaider A (1997) Gaining more flexibility in Cox proportional hazards regression models with cubic spline functions. Comput Methods Programs Biomed 54:201–208
Sigrist MK, Levin A, Er L, McIntyre CW (2009) Plasma osteoprotegerin is an independent risk factor for mortality and an early biomarker of coronary vascular calcification in chronic kidney disease. Nephrol Dial Transplant 24:3157–3162
Mesquita M, Demulder A, Damry N et al (2009) Plasma osteoprotegerin is an independent risk factor for mortality and an early biomarker of coronary vascular calcification in chronic kidney disease. Clin Chem Lab Med 47:339–346
Carrero JJ, Stenvinkel P (2009) Persistent inflammation as a catalyst for other risk factors in chronic kidney disease: a hypothesis proposal. Clin J Am Soc Nephrol 4:S49–S55
Nishiura R, Fujimoto S, Sato Y et al (2009) Elevated osteoprotegerin levels predict cardiovascular events in new hemodialysis patients. Am J Nephrol 29:257–263
Price PA, June HH, Buckley JR, Williamson MK (2001) Osteoprotegerin inhibits artery calcification induced by warfarin and by vitamin D. Arterioscler Thromb Vasc Biol 21:1610–1616
Acknowledgments
We would like to thank the patients and personnel involved in the creation of this study at Hakuai Hospital's dialysis unit. Baxter Novum is the result of a grant from Baxter Healthcare to the Karolinska Institutet. JJC is supported by the Loo and Hans Osterman's Foundation and the Swedish Kidney Association.
Conflicts of interest
BL is employed by Baxter Healthcare, Inc. No other author declares a personal or financial conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nakashima, A., Carrero, J., Qureshi, A. et al. Plasma osteoprotegerin, arterial stiffness, and mortality in normoalbuminemic Japanese hemodialysis patients. Osteoporos Int 22, 1695–1701 (2011). https://doi.org/10.1007/s00198-010-1377-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-010-1377-0