Abstract
Summary
We studied the nature of the relationship between bone mineral density (BMD) and the risk of death among elderly men. BMD was associated with mortality risk and was independent of adjustments for other co-morbidities. A piecewise linear function described the relationship more accurately than assuming the same gradient of risk over the whole range of BMD (p = 0.020). Low BMD was associated with a substantial excess risk of death, whilst a higher than average BMD had little impact on mortality.
Introduction
Previous studies have demonstrated an association between low BMD and an increased risk of death among men and women. The aim of the present study was to examine the pattern of the risk in men and its relation to co-morbidities.
Methods
We studied the nature of the relationship between BMD and death among 3,014 elderly men drawn from the population and recruited to the MrOS study in Sweden. Baseline data included general health questionnaires, life style questionnaires and BMD measured using DXA. Men were followed for up to 6.5 years (average 4.5 years). Poisson regression was used to investigate the relationship between BMD, co-morbidities and the hazard function of death.
Results
During follow-up, 382 men died (all-cause mortality). Low BMD at all measured skeletal sites was associated with increased mortality. In multivariate analyses, the relationship between BMD and mortality was non-linear, and a piecewise linear function described the relationship more accurately than assuming the same gradient of risk over the whole range of BMD (p = 0.020).
Conclusions
Low BMD is associated with a substantial excess risk of death compared to an average BMD, whereas a higher than average BMD has a more modest effect on mortality. These findings, if confirmed elsewhere, have implications for the constructing of probability-based fracture risk assessment tools.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The measurement of bone mineral density (BMD) is an integral component of the assessment of osteoporosis. It is variously used for the diagnosis of osteoporosis, to assess fracture risk and to monitor the natural history of the treated or untreated disorder [1]. For the assessment of fracture risk, there has been a great deal of interest in expressing risk as a probability of fracture [2]. Fracture probability depends on two competing hazards, namely the risk of fracture and the risk of death. Whereas the predictive value of BMD for fracture has been well characterised [3, 4], there is less information available on the relationship between BMD and death.
Several studies have shown that low BMD is a predictor of death in both men and women [5–14]. In the Third National Health and Nutrition Examination Survey (NHANES III), Mussolino and Gillum [12] reported that subjects in the lowest quartile of BMD had a greater risk of death than those within the highest quartile (relative risk, 1.53; 95% confidence interval (CI) 1.08–2.18). Other studies report gradients of risk (hazard ratios per 1 standard deviation in BMD) that ranged from 1.10 to 1.44 for death, adjusted for several risk factors for death, and from 1.16 to 2.30 for cardiovascular death [5, 7, 8, 10, 11]. Van Der Klift et al. showed that the relationship between risk of mortality and BMD may not be linear [9]. The risk of mortality increased when BMD was below average.
Our hypothesis was that the relationship between BMD and death (the logarithm of the hazard function) is non-linear and that the relationship therefore is not correctly described by a simple gradient of risk (GR). The aim of the present study was to investigate the relationship between BMD and mortality in more than 3,000 men between the ages of 70–81 years in Sweden.
Methods
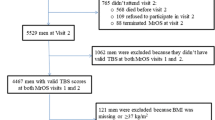
MrOS is a multi-centre study including elderly men in Sweden, Hong Kong and the USA [15]. The population in the present study was from the Swedish part of MrOS (n = 3,014) recruited at medical centres in Gothenburg (n = 1,010), Malmö (n = 1,005) and Uppsala (n = 999), described previously [16, 17]. Participants in MrOS Sweden (men aged 70–81 years) were randomly identified using national population registers. To be eligible for the study, men had to be able to walk without aids, provide self-reported data and give signed informed consent. There were no other exclusion criteria. The participation rate in MrOS Sweden was 45%. In the present report, the baseline data in MrOS Sweden was used together with follow-up for death.
Areal BMD was measured at the total body, lumbar spine, femoral neck, trochanter and total hip with calibrated scanners: Lunar Prodigy DXA (GE Lunar Corp., Madison, WI, USA) in Malmö and Uppsala and Hologic QDR 4500/A-Delphi (Hologic, Bedford, MA, USA) in Gothenburg. The coefficients of variation for the BMD measurements ranged from 0.5% to 3%. DXA measurements performed with equipment from different manufacturers were converted to standardised BMD, as previously described [16–18]. Conversion of BMD to T-scores were based on the NHANES III reference data for women aged 20–29 years [19] as recently recommended [20].
Height (in centimetres) and weight (in kilograms) were measured using standard equipment [16] and body mass index (BMI) was calculated as kilograms per square metre. Lean body mass and total body fat were measured using the Hologic QDR 4500/A-Delphi. Since the mean values were significantly different in the three cohorts, a Z-score based on age was calculated within each cohort. Systolic blood pressure was measured in millimetres of mercury. The international MrOS questionnaire [15] was used for collecting information about current smoking, physical activity, number and type of medications, self-estimated general health, level of education, fracture history, family history of hip fracture, history of diseases (has a doctor told you that you have rheumatoid arthritis, hypertension, cancer, stroke, myocardial infarction, diabetes or angina?) and the use of alcohol. Physical activity was quantified using parts of the questions in the Physical Activity Scale for Elderly [21]. The patients were asked to estimate the amount of time spent in the past week in activity categories: sitting, walking, light sport and recreation (bowling, fishing, boules), moderate sport (dancing, hunting, skating, golf), heavy sport and recreation (running, swimming, cycling, tennis, aerobics, skiing) and heavy training (weight training, push-ups). The relevant activity was categorised as never (0), seldom 1 to 2 days (1), sometimes 3 to 4 days (2) and often 5–7 days (3).
Participants brought current prescription medication to the baseline clinic where study staff recorded the name of all medications. General health was self-estimated as ‘Compared to other people of your own age, how would you describe your own health? Very good (1), good (2), fair (3), bad (4) or very bad (5)’. Level of education was coded 7 years education as 3, 9 years education as 4, upper secondary school as 6 and university as 8. Use of alcohol was expressed as three or more glasses of alcohol containing drinks per day, calculated from questions about frequency and amount of alcohol use.
All participants were followed up in the National Cause of Death Register until the end of 2007. This register comprises records of all deaths in Sweden and is more than 99% complete. Emigrants were followed up to the day of immigration. Causal mortality was assessed from ICD 10 codes. A cardiovascular death was defined with ICD 10 codes I110–I776.
A special Poisson regression model was used to study the relationship between age, the time since baseline, BMD, other covariates on the one hand and the risk of death on the other hand [22]. In contrast to a logistic model, the Poisson regression utilises person years of follow-up and the hazard function is assumed to be exp(β 0 + β 1 × current time from baseline + β 2 × current age + β 3 × current variable of interest). The beta coefficients reflect the effect size of the variables as in a logistic model, and β x = 0 denotes that the corresponding variable does not contribute to fracture risk. A similar approach was used to examine other predictors of mortality, and a final multivariate model was constructed to determine independent predictors. A spline Poisson regression model was fitted using knots at the 1st, 10th, 90th and 99th percentiles of BMD. The splines were second-order functions between the breakpoints and linear functions at the tails resulting in a smooth curve.
If A is the regression coefficient in an interval for the piecewise linear function carrying the original variable to a standardised normal one and B is the beta coefficient from Cox regression or Poisson regression in the same interval describing the change of risk in the original scale (without transformation), then the gradient of risk per 1 standard deviation is exp(B/A).
Mortality for any given BMD was compared to mortality of the general population. The risk of death in the general population was obtained from official statistics (Statistics Sweden).
Tests between BMD and centres used Fisher’s permutation test [23]. When other variables were adjusted for, linear regression was used. Two-sided p value was used for all analyses, and p < 0.05 was considered to be significant.
Results
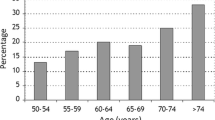
At the time of analysis, the 3,014 men aged 70–81 years had been followed for up to 6.5 years, with an average follow-up of 4.5 years. Of these, 382 men (12.7%) had died including 144 deaths from cardiovascular diseases, 153 from cancer and 66 from other causes. Nineteen causes of death were unclassified. Table 1 shows baseline characteristics of the study population divided into cases and controls.
Men who died were significantly older, had lower BMD, had lower lean body mass, had lower systolic blood pressure, more medications, worse general health and walked less than men who survived during the study. In addition, the former one took moderate or strenuous exercise less frequently. The prevalence of taking glucocorticoids, smoking, cancer, reported stroke, reported myocardial infarction, reported angina and diabetes was also higher. Men from Malmö had a significantly higher risk of death than men from Gothenburg and Uppsala.
Although the BMD values were standardised, there were differences in BMD between centres. Men from Gothenburg had higher BMD values than men at the other centres (p < 0.001), and men from Malmö had lower BMD values than men at other centres (p < 0.001). These differences persisted after adjustment for corticosteroid use, weight, BMI, current smoking, previous fracture, family history of hip fracture, general health, physical activity and education (p < 0.001).
Standardised BMD at all sites was significantly lower in men who subsequently died compared with men who remained alive during the follow-up. The hazard ratio for 1 standard deviation decrease in BMD (GR) ranged from 1.15 (95% confidence interval 1.03–1.28) for lumbar spine to 1.28 (95% CI 1.15–1.43) for total hip, adjusted for age and time since baseline (Fig. 1).
In order to explore the independent determinants of death, a multivariate analysis was performed using BMD at the total hip since this site was shown to have the highest GR. Table 2 shows the result of a multivariable analysis using a Poisson regression model in a forward stepwise manner, starting with the variable with the smallest p value. All variables in Table 1 that had a p value less than 0.05 were candidates for the multivariable analysis. Current age, current time since baseline, total hip BMD, past history of cancer, angina and diabetes, systolic blood pressure and general health had significant importance for overall mortality (Table 2). None of the other variables listed in Table 1 had any significant independent effect nor did a combined cardiovascular outcome (stroke + acute myocardial infarction + angina).
Although study centre had no significant importance for the risk of dying, we additionally adjusted for centre in the multivariable model in Table 2, but this had no effect on the results (data not shown). There was no significant interaction between centre and BMD (p > 0.30). Additionally, there was no significant interaction between age and BMD (p = 0.30). Thus, the relationship of BMD to death was the same for all ages. The GR was 1.27 (95% CI 1.14–1.42) for total hip BMD in the multivariable model in Table 2.
To investigate the relationship between total hip BMD and mortality, the variables in Table 2 were used to determine a hazard function of death as a function of BMD using a spline function. Figure 2 shows that a change in BMD below average value had more importance for death than a similar change of BMD value above the average value.
The hazard function of death (momentary risk) and 95% confidence intervals depending on total hip BMD for a man aged 75 years after 2 years from baseline, with no history of cancer, angina or diabetes and with an average systolic blood pressure and self-estimated general health. The dashed diagonal line represents the relationship assuming that the gradient of risk is the same all over the whole range of BMD. The vertical dashed lines in the figure represent the 1st, 25th, 50th, 75th and the 99th percentiles
The dashed diagonal line in Fig. 2 describes the relation between death and BMD at the total hip when it is assumed that there is a constant gradient of risk of 1.27 all over the observed range of BMD. Using piecewise linear regression, the only interval where the importance of BMD for death was significant was when BMD was lower than the 20th percentile (p = 0.0013), whilst for the other intervals, there was no significant interaction (p > 0.20). With a piecewise linear Poisson regression with one knot in 25th percentile, there was a significant difference between the slope before and after the knot (p = 0.020), indicating that the spline function shown in Fig. 2 described the data more accurately than when the same GR was assumed over the whole range of BMD.
A BMD of 0.93 g/cm2 at the total hip (the median in this cohort) corresponded to a BMD T-score of −0.2. The 1st, 25th, 75th and 99th percentile BMD corresponded to a BMD T-score of −2.6, −1.0, +0.6 and +2.9 SD, respectively. The GR below the 25th percentile of BMD (0.84 g/cm2) was 1.62, between 0.84 and 1.11 g/cm2 (the 89th percentile) the GR was 1.13 and above 1.11 g/cm2 the GR was 1.19. Thus, a man with a total hip BMD measurement lying at the 1st percentile (T-score = −2.6 SD) would have a 3.7-year lower life expectancy than a man with a median BMD, whereas at the other extreme (99th percentile, T-score = +2.9 SD), there was a gain in life expectancy of 1.7 years compared to that at the median BMD.
Different causes of death
Gradient of risk was examined according to the cause of death. The highest gradient of risk between total hip BMD and mortality was for deaths other than cancer and cardiovascular causes followed by deaths from cancer and deaths from cardiovascular disease (Table 3). The association of higher death rate with lower BMD persisted with multivariate analysis. When total hip BMD was examined with spline multivariable models, there was a similar relationship as seen for total death, although not of statistical significance (Fig. 3).
The hazard function of different causes of death (momentary risk) with 95% confidence intervals at three levels of total hip BMD for a man aged 75 years after 2 years from baseline. The three levels of BMD are examples from continuous distributions analogous to that shown in Fig. 2. a With no history of myocardial infarction and diabetes and with an average self-estimated general health. b With no history of myocardial infarction and cancer and with an average self-estimated general health. c With an average heavy physical activity, systolic blood pressure and self-estimated general health
Discussion
The principal finding in the present study was that bone mineral density was a strong predictor of death in elderly men aged 70–81 years. The effect was non-linear and low BMD had the more marked effect on mortality. In other words, low BMD was a stronger predictor of mortality than high BMD. The effect was independent of age, height, weight, blood pressure, self-assessed general health, physical activity, education, medication intake, smoking, alcohol use, previous fracture, family history of fracture and known co-morbidities.
The majority of previous studies that have examined the association between mortality and BMD have assumed that there was a linear gradient of risk for death with BMD [5, 6] or reported hazard ratios comparing tertiles or quartiles of BMD [7, 8, 10–14]. The comparison of quartiles (or quintiles, etc.) may give results that are difficult to interpret. If, for example, a variable has a normal distribution and a continuous gradient of risk of say 1.35 per standard deviation, then the hazard ratio between Q1 and Q2 will be 1.32 and the hazard ratio between Q2 and Q3 will be 1.21. The difference in HR arises because Q1 captures a greater range of the index variable whereas Q2 and Q3 cover a smaller interval. Thus, differences in hazard ratios should not be interpreted as evidence for non-linearity of risk and vice versa. These considerations suggest that hazard functions rather than hazard ratios should be examined. This has been addressed in one previous study of Van Der Klift et al. [9] who studied 5,819 men and women aged ≥55 years and described a threshold around the average of BMD for men and the risk of death increased with below average values but also increased at higher than average values. It is possible that this phenomenon was a product of the cubic model used. In the present study, we used spline functions with four breakpoints and hence introduced greater freedom to the model.
There are several limitations to the present study. The participation rate was only 45% and there is likely to be a healthy selection bias though the median BMD at the total hip (0.93 g/cm2) corresponding to a BMD T-score of –0.13 [19, 20] is close to that reported for non-Hispanic men aged 70–79 years in the population-based NHANES study [19] (T-score = –0.20 SD). This might suggest little bias in terms of BMD but does not exclude other selection biases. A biased sample is expected to converge with the general population over time, and evidence for such a bias is the significant variable ‘time since baseline’ in Table 2. This indicates that there is higher death risk the longer the time since follow-up even with adjustment for the other variables including current age. This suggests that the longer the follow-up in MrOS, the more the cohort resembles that of the general community. This is a factor to be aware of when interpreting the results, but since ‘time since baseline’ is in the model, we have in part adjusted for this effect.
A limitation of our findings is the narrow age range of the MrOS cohort (70–81 years). Within this age range, there was no evidence of any age dependency, but this does not exclude an important effect at other ages. Other studies have not addressed age-dependent effects [5, 7–14], but it would be important to do so for judging the impact of the effect of BMD-associated mortality on the estimate of fracture probability (see below).
The importance of BMD as a predictor of death will depend to some extent on the fact that a fracture event causes death [24]. In the present study, there was a significant relationship between BMD and death among men in whom no fracture had occurred (data not shown). However, this analytic approach is difficult to interpret and should usually be avoided because the censoring event, fracture, is strongly dependent on BMD. Thus, the exclusion of fracture cases will bias any relationship between BMD and death.
The present study sheds little light on the reason for the association of low BMD with mortality. A low BMD was a significant risk factor for death even adjusting for co-morbidities. In our multivariate analysis, BMD had importance for death independent of age, blood pressure, general health and history of angina, diabetes and cancer. Several other variables had importance in univariate analysis (adjusted for age and time since baseline) such as physical activity and smoking, but they had no significant importance beyond the variables above. When analysing subgroups of death causes, the relationship was strongest between BMD and death for other causes of death than cardiovascular diseases and cancer. And when attaching spline models to data, the pattern was also non-linear, but the number of deaths comprised less than 20% of all deaths and the analysis is likely to be underpowered. With this caveat, the analysis suggests that low BMD is a marker for ill health, even beyond self-rated health.
Our findings have implications for fracture risk assessment if confirmed in independent studies over a broader age range and in women. In the FRAX® risk assessment tool, the probability of fracture is computed from the death hazard as well as the fracture hazard [25]. Moreover, the clinical risk factors modify both hazards. The factors that affect the death hazard significantly in FRAX® are age, sex, BMI, current smoking, use of corticosteroids and BMD, several of which are shown to affect mortality in the present study including an effect of BMD (see Tables 1 and 2). In the case of BMD, the risk model for death in FRAX® assumes a constant gradient of risk across the whole range of BMD. If our present findings are confirmed, this would suggest that the predictive value of FRAX® could be improved by using a non-linear relationship between death and BMD. This would mostly affect men having very low BMD in whom the higher risk of death would reduce the computed fracture probability.
In conclusion, the results of this study indicate that, in men, there is a non-linear association between BMD and mortality, which is independent of covariates of co-morbidity. For the average value of BMD, the difference between the linear and the non-linear importance is not large, so for the population, this has no large importance. But for the men with low BMD and especially for those with extremely low BMD, under the 1st percentile (a T-score below –2.60 SD), the risk of death is much higher than hitherto considered.
References
World Health Organisation (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. WHO technical report series 843. WHO, Geneva
Kanis JA, on behalf of the World Health Organization Scientific Group (2008) Assessment of osteoporosis at the primary health-care level. Technical report. WHO Collaborating Centre, University of Sheffield, UK
Marshall D, Johnell O, Wedel H (1996) Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. Br Med J 312:1254–1259
Johnell O, Kanis JA, Oden A, Johansson H, De Laet C, Delmas P, Eisman JA, Fujiwara S, Kroger H, Mellstrom D, Meunier PJ, Melton LJ 3rd, O'Neill T, Pols H, Reeve J, Silman A, Tenenhouse A (2005) Predictive value of BMD for hip and other fractures. J Bone Miner Res 20:1185–1194
Browner WS, Seeley DG, Vogt TM, Cummings SR (1991) Non-trauma mortality in elderly women with low bone mineral density. Study of osteoporotic fractures research group. Lancet 338:355–358
Johansson C, Black D, Johnell O, Oden A, Mellstrom D (1998) Bone mineral density is a predictor of survival. Calcif Tissue Int 63:190–196
von der Recke P, Hansen MA, Hassager C (1999) The association between low bone mass at the menopause and cardiovascular mortality. Am J Med 106:273–278
Trivedi DP, Khaw KT (2001) Bone mineral density at the hip predicts mortality in elderly men. Osteoporos Int 12:259–265
Van Der Klift M, Pols HA, Geleijnse JM, Van Der Kuip DA, Hofman A, De Laet CE (2002) Bone mineral density and mortality in elderly men and women: the Rotterdam study. Bone 30:643–648
Mussolino ME, Madans JH, Gillum RF (2003) Bone mineral density and mortality in women and men: the NHANES I epidemiologic follow-up study. Ann Epidemiol 13:692–697
Pinheiro MM, Castro CM, Szejnfeld VL (2006) Low femoral bone mineral density and quantitative ultrasound are risk factors for new osteoporotic fracture and total and cardiovascular mortality: a 5-year population-based study of Brazilian elderly women. J Gerontol A Biol Sci Med Sci 61:196–203
Mussolino ME, Gillum RF (2008) Low bone mineral density and mortality in men and women: the Third National Health and Nutrition Examination survey linked mortality file. Ann Epidemiol 18:847–850
Suzuki T, Yoshida H (2009) Low bone mineral density at femoral neck is a predictor of increased mortality in elderly Japanese women. Osteoporos Int 21:71–79
Nguyen ND, Center JR, Eisman JA, Nguyen TV (2007) Bone loss, weight loss, and weight fluctuation predict mortality risk in elderly men and women. J Bone Miner Res 22:1147–1154
Orwoll E, Blank JB, Barrett-Connor E, Cauley J, Cummings S, Ensrud K, Lewis C, Cawthon PM, Marcus R, Marshall LM, McGowan J, Phipps K, Sherman S, Stefanick ML, Stone K (2005) Design and baseline characteristics of the osteoporotic fractures in men (MrOS) study—a large observational study of the determinants of fracture in older men. Contemp Clin Trials 26:569–585
Mellstrom D, Vandenput L, Mallmin H, Holmberg AH, Lorentzon M, Oden A, Johansson H, Orwoll ES, Labrie F, Karlsson MK, Ljunggren O, Ohlsson C (2008) Older men with low serum estradiol and high serum SHBG have an increased risk of fractures. J Bone Miner Res 23:1552–1560
Mellstrom D, Johnell O, Ljunggren O, Eriksson AL, Lorentzon M, Mallmin H, Holmberg A, Redlund-Johnell I, Orwoll E, Ohlsson C (2006) Free testosterone is an independent predictor of BMD and prevalent fractures in elderly men: MrOS Sweden. J Bone Miner Res 21:529–535
Lewis CE, Ewing SK, Taylor BC, Shikany JM, Fink HA, Ensrud KE, Barrett-Connor E, Cummings SR, Orwoll E (2007) Predictors of non-spine fracture in elderly men: the MrOS study. J Bone Miner Res 22:211–219
Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC Jr, Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8:468–489
Lu Y, Fuerst T, Hui S, Genant HK (2001) Standardization of bone mineral density at femoral neck, trochanter and Ward's triangle. Osteoporos Int 12:438–444
Washburn RA, Smith KW, Jette AM, Janney CA (1993) The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol 46:153–162
Breslow NE, Day NE (1987) Statistical methods in cancer research. Volume II—the design and analysis of cohort studies. IARC Sci Publ 82:1–406
Good P (ed) (2000) Permutation tests. Springer, New York
Kanis JA, Oden A, Johnell O, De Laet C, Jonsson B, Oglesby AK (2003) The components of excess mortality after hip fracture. Bone 32:468–473
Kanis JA, Oden A, Johansson H, Borgstrom F, Strom O, McCloskey E (2009) FRAX and its applications to clinical practice. Bone 44:734–743
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Johansson, H., Odén, A., Kanis, J. et al. Low bone mineral density is associated with increased mortality in elderly men: MrOS Sweden. Osteoporos Int 22, 1411–1418 (2011). https://doi.org/10.1007/s00198-010-1331-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-010-1331-1