Abstract
Summary
In patients with femoral neck fracture, clinical factors, bone metabolism markers (in serum, urine, and bone), bone mineral density, radiographic parameters, and bone histomorphometric parameters were investigated to detect determinants of fragility fracture. The osteocalcin/deoxypyridinoline ratio and osteopontin/calcium ratio of cortical bone were selected as significant predictors.
Introduction
Measurement of bone mineral density is widely used to assess bone strength, but this also depends on other bone components and on bone structure. The objective of this study was to investigate risk factors for fracture related to bone quality, the patient’s history, and the patient’s lifestyle.
Methods
Twenty-one patients with femoral neck fracture and 18 patients with osteoarthritis were enrolled. Blood and urine samples were collected on admission to hospital, and bone samples were obtained from femoral necks resected during surgery. Multivariate logistic regression analysis was performed using osteoarthritis and femoral neck fracture as combined variables to assess the influence of alcohol or coffee intake, eating natto (fermented soybeans), osteocalcin and calcium concentrations, the osteocalcin/deoxypyridinoline ratio and osteopontin/calcium ratios of cortical bone and cancellous bone, various bone histomorphometric parameters, the bone mineral density of the lumbar spine and the intact contralateral femoral neck, and various radiographic parameters of the spine
Results
By forward stepwise multivariate analysis, the osteocalcin/deoxypyridinoline and osteopontin/calcium ratios of cortical bone were selected as significant factors for fracture (the odds ratios were 0.493 and <0.001, respectively; both P < 0.001).
Conclusions
A decrease of osteopontin and osteocalcin in bone is important for promoting vulnerability to hip fracture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
At present, the risk of fracture is evaluated in two different ways. One method involves assessing the strength of the bones from parameters, while the other method is to evaluate the risk of fracture based on the history of each patient [1–3].
The strength of bone is dependent on four factors, which are the bone mineral density, bone structure, bone matrix, and accumulation of microcracks [4–16]. However, there are no methods for direct measurement of the bone matrix or microcracks in vivo. Bone structure is not often assessed because of radiation exposure and lack of suitable equipment. Therefore, in clinical practice, bone mineral density is commonly used as the indicator of bone strength. However, research performed to date has shown that it is difficult to completely explain the risk of fracture on the basis of the bone mineral density [17, 18].
The concept of fracture risk has recently been employed in epidemiological surveys [19, 20]. This refers to the risk of fracture occurring in a particular patient, and not only the bone mineral density but also the past history and lifestyle factors are taken into consideration when comparing patients with or without fragility fractures. However, the clinical evaluation of fracture risk is still heavily influenced by bone mineral density, since assessment of bone strength depends on the measurement of bone mineral density and current therapy to reduce fracture risk focuses on increasing bone mineral density. Instead, we considered that evaluation of fracture risk should not be based solely on measurement of bone mineral density and should also include other factors related to bone structure and the bone matrix.
Accordingly, we conducted a survey of patients who had femoral neck fractures and patients who had osteoarthritis with the objective of clarifying the risk of fracture based on the bone mineral density, bone matrix, and bone structure, as well as the patient’s past history. Bone metabolism markers obtained from biochemistry tests and urinalysis, degenerative changes on X-ray films of the spine, the bone mineral density of the femoral neck and lumbar spine, histomorphometric parameters of the femoral head, markers of osteoblast growth, and typical items from the past history and lifestyle factors were investigated in order to identify factors that contributed to the risk of fracture.
Materials and methods
Study design
The subjects were postmenopausal women who underwent hemi or total hip replacement because of femoral neck fracture due to osteoporosis or osteoarthritis of the hip at five hospitals during the period from April 2006 to March 2007. The subjects gave written informed consent to participation after receiving an adequate explanation of the study. An interview (past history and lifestyle factors) was performed, along with blood and urine sampling, bone densitometry, and spinal radiography. The femoral heads and necks that were resected during hip surgery were collected and sectioned. Some of the sections were used for analysis of the bone protein content and others were employed for bone histomorphometry. This study was performed with the approval of the Ethics Committee of University of Occupational and Environmental Health (Kitakyushu, Japan).
Subjects
The subjects were all postmenopausal women over 50 years of age who fitted into either of the groups below among those hospitalized for femoral head replacement.
-
(1)
Patients undergoing femoral neck replacement (Fx group)
These patients had primary osteoporosis according to the diagnostic criteria of the Japanese Society of Bone and Mineral Research and suffered from femoral neck fracture requiring femoral head replacement [21].
-
(2)
Patients with osteoarthritis of the hip (OA group)
These patients required hip replacement because of progressive osteoarthritis of the hip.
Patients were excluded from the study if they fitted any of the following exclusion criteria:
-
1)
Patients with bacterial or viral (hepatitis B or C) infection
-
2)
Patients with bone metastasis of cancer
-
3)
Patients receiving warfarin therapy
-
4)
Patients who had participated in a clinical trial of osteoporosis treatment within the previous 6 months
-
5)
Patients who were judged to be inappropriate for this study by the attending physician (e.g., patients with rheumatoid arthritis)
-
6)
Patients who had used vitamin K supplements within 1 month before giving informed consent
-
7)
Patients using glucocorticoids (except for topical products) within 6 months before giving informed consent
-
8)
Patients who had already undergone surgery on the contralateral proximal femur
Interview
After each patient gave written informed consent to the study, an interview was performed to obtain data on the history and lifestyle habits. The questions included the number of years after menopause, the number of deliveries, the performance of ovariectomy, smoking, alcohol consumption, complications, medical history, history of surgery, concomitant medications, coffee consumption, and consumption of natto (fermented soybeans).
Biochemistry tests and urinalysis
After admission to hospital and before surgery, 6 ml of blood and 10 ml of urine were collected from each patient. Serum was separated by centrifugation and was stored at −20°C until the following parameters were measured: intact osteocalcin (iOC; BGP IRMA “Mitsubishi,” Mitsubishi Chemical Medience Corporation, Tokyo, Japan), bone alkaline phosphatase (BAP; Osteolinks “BAP”, DS Pharma Biomedical Co., Ltd., Osaka, Japan), N-terminal telopeptide of type I procollagen (P1NP; UniQ P1NP RIA, Orion Diagnostica, Espoo, Finland), N-linked telopeptide of type I collagen (NTX; Osteomark NTx Serum, Inverness Medical Japan Co., Ltd., Tokyo), carboxylated OC (Gla-type Osteocalcin (Gla-OC) EIA Kit (Precoated), Takara Bio Inc., Shiga, Japan), and undercarboxylated OC (ucOC; Glu-OC Competitive EIA Kit, Takara Bio. Inc.). Urine levels of calcium (Ca), phosphate (P), and NTX (Osteomark, Inverness Medical Japan Co., Ltd.) were also measured and represented by the ratio to the level of creatinine (Cr). The central Laboratory of Mitsubishi Chemical Medience Corporation performed all of these measurements.
Spinal radiography
Conventional thoracic and lumbar spinal plain roentgenograms in lateral and anteroposterior projection were obtained from participants. Both lateral projections in the lateral decubitus position and A-P projections in the supine position were taken at a constant focus-film distance of 1.5 m. The severities of spinal degeneration including osteophyte formation, endplate sclerosis, disc space narrowing, and vertebral wedge deformity were assessed semi-quantitatively from Th4/5 to L4/5 disc level or from Th4 to L4 vertebrae by using the grading scale of Genant [22]. Then we assessed radiographical spinal disc degeneration using scoring system as previously reported [23–25]. Briefly, osteophyte formation at a given disc was graded 0–3°, endplate sclerosis at given vertebra was graded 0–2°, and disc space narrowing and vertebral wedge deformity were graded 0–1°, respectively. Then we defined sum of each degree from Th4/5 to L4/5 disc level for osteophyte formation on anteroposterior radiographs as a score of osteophyte formation. We also defined sum of each degree from Th4 to L4 vertebra for endplate sclerosis and vertebral wedge deformity and that from Th4/5 to L4/5 disc level for disc space narrowing on lateral radiographs as a score of endplate sclerosis and disc space narrowing, respectively.
Bone mineral density measurement
Using dual energy X-ray absorptiometry (DXA; UOEH; Hologic-Delphi at Ken-ai-Kinen Hospital; Hologic-QDR 4500 at Shin-Kokura Hospital; Hologic QDR at Shin-Mizumaki Hospital; and Hologic QDR at Kitakyushu General Hospital), the lumbar bone mineral density (L2 to L4) and that of the proximal femur on the unaffected side were measured. The following parts of the proximal femur were evaluated: neck, trochanter, intertrochanteric region, total proximal femur, and Ward’s triangle. Differences of measured values between the different devices were corrected.
Harvesting of femoral heads
The femoral heads (including the neck) resected during surgery were cut into two coronal sections for measurement of bone tissue components and for bone histomorphometry. The sections for measurement of bone tissue components were stored at −20°C, after which each section was divided into cortical bone and cancellous bone components, and then crushed and pulverized. After dividing the femoral head in two using a hand saw, the cancellous bone was scraped away from the cortical bone using a chisel and spatula. The cancellous and cortical bone pieces were then, using nippers and a chisel, separately broken up into small fragments, which were washed in acetone and water to remove any adipose tissue. The resulting fragments were frozen and broken down using a micro dismembrator [CRYO-PRESS; Microtec Nition, Funabashi, Japan] to sample sizes able to pass through a 500-μm mesh, and again washed with acetone and water for delipidation. The resulting test samples were freeze-dried for 24 h and stored at −20°C. Measurements of OC, ucOC, and osteopontin (OPN) were performed using these test samples. Demineralization extraction was performed by reacting 1.5 mL 0.5 M of dimethyl sulfoxide (pH 7.4) containing 0.1 mL of 10% protease inhibitor (P8340, Sigma Co. Ltd), with a 20 mg initial sample at 4°C for 24 h. The resulting solution was centrifuged at 3,000 rpm for 5 min, and the supernatant then centrifuged at 10,000 rpm using an Ultrafree-MC filter [Millipore, MA, USA], and the supernatant used as the test sample. OC and OPN levels of the extracts were determined as for the blood samples, using the kits as described above. Collagen derivatives were extracted by adding 2.0 mL of 6 mol/L HCl to a 40 mg initial sample.
Then the levels of OC (BGP IRMA “Mitsubishi,” Mitsubishi Chemical Medience Corporation), ucOC (Glu-OC Competitive EIA Kit, Takara Bio. Inc.), and OPN (Human Osteopontin Assay Kit-IBL, Immuno-Biomedical Laboratories Co., Ltd., Gunma, Japan) were measured in the bone tissue. Pyridinoline (PYD), deoxypyridinoline (DPD), and hydroxypyridine (HYP) were measured by high-performance liquid chromatography. All of the bone components were measured by the Central Laboratory of Mitsubishi Chemical Medience Corporation, while crushing and pulverizing of the bone samples was performed by the Central Research Laboratories of BML (Saitama, Japan).
The bone histomorphometry specimens were temporarily stored at 4°C in 4% paraformaldehyde immediately after sectioning. A 1-cm2 of cancellous bone was resected from the center of each specimen. After immersion in Villaneuva staining solution, the bone squares were embedded in methyl methacrylate. Specimens were resected and embedded by staff at the University of Occupational and Environmental Health (Kitakyusyu, Japan).
Bone histomorphometry
For bone histomorphometry, specimens of bone were obtained from the center of the femoral head and were cut into sections 6 μm thick after being immersed in Villaneuva staining solution and embedded in methyl methacrylate. The sections were stained with Goldner stain before examination. The parameters that were measured or calculated for histomorphometry were the bone volume to total volume ratio (BV/TV; %), trabecular thickness (Tb.Th; μm), trabecular number (Tb.N; #/mm), trabecular separation (Tb.Sp; μm), osteoid volume to bone volume ratio (OV/BV; %), and osteocyte number to bone surface ratio (N.Ot/BS; #/mm). Calculations were performed by UOEH using a Histometry-RT-Camera (System Supply; Nagano, Japan). The abbreviations used are based on the nomenclature of the American Society for Bone and Mineral Research [26].
Parameters analyzed
Demographic characteristics analyzed included the age, time after menopause, height, weight, body mass index (BMI), and number of deliveries.
With regard to the past history and lifestyle habits, analysis included the performance of ovariectomy, smoking, alcohol consumption, complications, medical history, surgical history, concomitant medications, coffee consumption, and intake of natto (fermented soybeans).
The following bone metabolism markers were also assessed: serum iOC, serum BAP, serum P1NP, serum NTX, urine NTX, serum Gla-OC, serum ucOC, ucOC/Gla-OC, Gla-OC/iOC, and ucOC/iOC.
Statistical analysis
Frequencies and percentages were calculated for discrete variables and ordinal categorical data. Summary statistics were calculated for continuous variables. Intergroup comparison of the OA and Fx groups were performed by using the χ 2 test for discrete variables, the U test for categorical data, and t test for continuous variables. For measured values from the same patient (continuous variables), comparisons were performed with the paired t test. The level of significance was set at P ≤ 0.05 (two-sided), unless otherwise specified.
For investigation of factors affecting the presence/absence of fracture (OA group and Fx group), multivariate analysis was performed by multiple logistic regression analysis. This analysis employed the items that remained after screening by the following exclusion criteria:
-
1.
Missing data (number of years after menopause, number of deliveries, presence/absence of ovariectomy, or presence/absence medical history)
-
2.
Bone tissue components that might include cartilage (HYP and PYD)
-
3.
Bone tissue components with a very low affinity for bone (ucOC)
-
4.
Variables with a probability >0.15 according to univariate logistic regression analysis
The forward selection method, backward elimination method, and stepwise selection method were used to select variables. The level of significance for deciding whether a candidate variable would be included in the model was set at P ≤ 0.3 (two-sided).
Since this study was exploratory, adjustment for multiplicity associated with verification of multiple hypotheses was not performed. All analyses were conducted with SAS software (release 9.1; SAS Institute Inc. Cary, NC, USA).
Results
Subjects
Forty-two patients gave written informed consent, and analysis of 39 patients was performed [18 in the OA group and 21 in the Fx group]. Three patients were excluded because radiography or DXA not performed (n = 2) or because of a measurement date violation (n = 1). None of the patients included in these analyses was taking inhibitors of bone resorption such as bisphosphonates or selective estrogen receptor modulators. In comparison with the OA group, the age was significantly greater, postmenopausal duration significantly longer, and body weight and BMI significantly lower in the FX group (P < 0.001, P = 0.002, P = 0.038, and P = 0.046, respectively: t test), but the height of the subjects and the number of deliveries showed no significant differences (Table 1). With respect to the past history and lifestyle habits, significantly more patients in the Fx group had complications, a past medical history, and used concomitant medications (P < 0.001, P = 0.005, and P = 0.005, respectively: χ 2 test). In the OA group, more patients had a high frequency of coffee consumption (P = 0.005; U test, Table 2).
Bone metabolism markers and bone minerals
The serum and urine markers of bone metabolism showed no significant differences between the two groups (Table 3). There were also no significant differences between the two groups with regard to serum ucOC/Gla-OC and Gla-OC/iOC or urine Ca/Cr and P/Cr.
Bone metabolism markers in cortical bone and cancellous bone
The OC level of cortical bone was significantly lower in the Fx group than in the OA group, but no significant difference was found for cancellous bone (P < 0.001, P = 0.103; t test, Table 4). ucOC was significantly lower in the Fx group than in the OA group for both cortical bone and cancellous bone (P < 0.001 and P = 0.044, respectively: t test). OPN was also significantly lower in the Fx group than in the OA group for both cortical bone and cancellous bone (both P < 0.001: t test). PYD was significantly higher in the Fx group than in the OA group for both cortical bone and cancellous bone (both P < 0.001: t test). Although the DPD level of cortical bone showed no difference between the two groups, the Fx group had a significantly higher DPD level in cancellous bone (P < 0.001: t test). The HYP level of cortical bone was significantly higher in the Fx group than the OA group (P < 0.001: t test), but that level in cancellous bone were significantly higher in the OA group than in the FX group (P = 0.037, t test).
The Ca level of cortical bone was also significantly higher in the Fx group (P < 0.001; t test), but showed no significant difference between the two groups for cancellous bone.
ucOC accounted for 1.67–2.22 percentage of total bone OC in both groups, suggesting that ucOC shows a very low affinity for bone. Therefore, it was judged to be unnecessary to investigate ucOC as a bone component and it was excluded from multivariate analysis. The differences of PYD and HYP levels between cortical bone and cancellous bone were much greater in the Fx group than in the OA group, probably due to loss of cartilage from the femoral head in the OA group, while cartilage was preserved in the Fx group. Therefore, it was judged that PYD and HYP values were influenced by the cartilage component and these variables were also excluded from multivariate analysis.
Non-collagen protein/Ca ratio and non-collagen protein/collagen ratio in cortical and cancellous bone
The ratio of OC to Ca (OC/Ca) in cortical bone and the ratio of OPN to Ca (OPN/Ca) in both cortical and cancellous bone were significantly lower in the Fx group than the OA group (all P < 0.001: t test), while the ratio of DPD to Ca (DPD/Ca) was significantly higher in both cortical and cancellous bone (P < 0.001 and P = 0.001, respectively: t test). The ratios of OC and OPN to DPD in cortical bone and cancellous bone were all significantly lower in the Fx group than the OA group (P < 0.001, P = 0.001, P < 0.001, and P < 0.001, respectively: t test; Table 5).
Radiographic findings of the thoracic and lumbar spine
More patients had deformities of the vertebral bodies (P < 0.001: χ 2 test), but there was a higher number of vertebral deformities (P = 0.024: t test) in the Fx group than in the OA group. When the thoracic and lumbar spine were compared, the Fx group had significantly more deformed lumbar vertebrae (P = 0.009: t test). The presence/absence of narrowing of the intervertebral disks did not differ between the two groups, but there were significantly more narrow intervertebral disks in the Fx group than the OA group (P = 0.038: t test). No significant differences were found for the other parameters (data not shown).
Bone mineral density measurements
Bone densities of the femoral neck were significantly lower in all sites in the FX group than in the OA group (Table 6).
Histomorphometry of cancellous bone in the femoral head
BV/TV and trabecular thickness were significantly lower in the Fx group than in the OA group (P < 0.001 and P = 0.043, respectively: t test). No significant differences were found for the other parameters (Table 7).
Results of multivariate analysis
Multiple logistic regression analysis was performed by using the presence/absence of fracture (OA group and Fx group) as the response variables and the analytical parameters as the explanatory variables.
Variables fitting the following criteria were excluded as candidate variables for the model:
-
1.
Variables with missing data (postmenopausal duration, parity, oophorectomy or past history)
-
2.
Variables discussed at the interim ressession, conducted before all data was collated, for which multivariate analysis was considered unnecessary (bone ucOC, HYP, PYD)
-
3.
Variables with a probability greater than 15% on univariate logistical regression analysis
As a result, we performed variable selection on the following variables using minimum redundancy, maximum relevance, and minimum redundancy maximum relevance selection. The two-tailed significance level for candidate variables included in the model was set at 30%.
-
Patient background factors
Age, body weight, BMI, intake of fermented soybeans, alcohol consumption, coffee consumption, complications
-
Bone constituents
Cortical bone: OC, Ca, OC/DPD, OC/Ca, OPN/Ca, DPD/Ca
Cancellous bone: OC, DPD, OPN, OC/DPD, OC/Ca, OPN/DPD, OPN/Ca, DPD/Ca
-
Bone density
L2–4 vertebrae, femoral neck, troch, inter, total, Ward’s
-
Radiological evaluation
Number of narrowed intervertebral disks, mean osteophyte surface area (L1/2-4/5), presence of deformed vertebral bodies, number of deformed vertebral bodies, number of deformed thoracic vertebrae, Walter Reed Visual Assessment Scale for scoliosis
-
Bone metabolism measurements
Cancellous bone mass, cancellous bone width, bone gap, cancellous bone OPN/osteoid mass, cortical bone OPN/osteoid mass, cortical bone OC/osteoid mass
The results of variable selection are given below. The results of minimum redundancy selection and minimum redundancy maximum relevance selection were in agreement (Table 8).
As a result, the factors that significantly predicted fracture were OC/DPD and OPN/Ca in cortical bone by the forward selection method, as well as OPN/Ca in cortical bone by both the backward elimination and forward selection methods (Table 8).
However, since the model employing the forward selection method was unstable, the age distribution of OC/DPD and OPN/Ca was investigated. Because of the significant difference in age distribution (P < 0.001: t test), the same multivariate analysis was conducted for a subpopulation stratified by age in the two groups (22 subjects aged 59–80 years old).
When subpopulation analysis was performed, similar results were obtained as for the analysis of all 39 subjects.
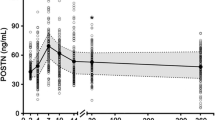
Maximum relevance selection placed two variables, cortical bone OC/DPD and cortical bone OPN/Ca. We therefore produced a scatter diagram of cortical bone OC/DPD and cortical bone OPN/Ca (Fig. 1) and examined the relationship between these 2 variables.
The distributions of cortical bone OC/DPD and cortical bone OPN/Ca were separate and distinct for each group.
Discussion
In the present study, we investigated factors that influence the occurrence of fragility fractures in patients with osteoporotic femoral neck fractures and patients with osteoarthritis of the hip. Multiple logistic regression analysis identified OC/DPD and OPN/Ca of cortical bone as important predictors of the risk of fragility fracture, both of which have a similar predictive value.
Although bone mineral density of the lumbar spine tended to be lower, and femoral neck and intertrochanter bone mineral density were significantly lower in the FX group than in the OA group, the results of this study agree with previous reports indicating a relatively small contribution by bone mineral density to bone strength [17, 18]. On the other hand, decreases in either OC/DPD or OPN/Ca were significant predictive factors for fragility fracture, and low bone mineral density was not a predictive factor. Decreases in bone volume or bone formation are not observed in either osteocalcin gene or osteopontin gene deficit mice [27, 28].
Osteocalcin suppresses formation of calcium phosphate nuclei, and an osteocalcin deficit does not result in a reduction in calcification [29]. Decreased levels of fully carboxylated osteocalcin inhibit calcification crystal accumulation and cause random calcification of collagen fibers. This random calcification of collagen fibers can cause bone fragility irrespective of the mineral density [30] or early destruction of the collagen fibers [31]. These earlier reports agree with the findings of this study that decreased OC/DPD causes bone vulnerability independent of the bone mineral density. To maintain high quality bone, osteocalcin strictly regulates the formation of calcium phosphate nuclei, accumulation of calcified crystals, and the calcification of collagen fibers.
Osteopontin suppresses the growth of calcium phosphate crystals, and an osteocalcin deficit does not result in reduced calcification or bone formation [28, 29]. Although it is also produced by immature osteoblasts, 55 kDa osteopontin is synthesized mainly by mature osteoblasts prior to the precipitation of calcium phosphate crystals, and controls the growth of calcified crystals [32]. Low OPN/Ca conditions cause the accumulation of large calcified crystals, possibly reducing bone strength in spite of increased calcification [31].
Osteoblasts synthesize type 1 collagen from an early stage of differentiation [33], but most osteocalcin and osteopontin are produced by more mature osteoblasts [29]. Decreases in both the osteocalcin/type 1 collagen ratio and the osteopontin/calcium ratio indicate that patients with bone vulnerability suffer from a disturbance of osteoblast maturation. Promotion of osteoblast maturation is important in avoid fragility fracture in patients with osteoporosis, but no clinically applicable methods have so far been discovered. It is however possible that facilitation of osteocalcin carboxylation may increase osteocalcin uptake from the circulation and normalize abnormal calcification. It has been reported that reduced osteocalcin uptake correlates with the occurrence of fragility fractures [34]. It was also reported that vitamin K reversed warfarin-induced random calcification of collagen fibers in an animal study [30].
In a previous study of the relationship between decreased osteocalcin carboxylation and increased fracture risk [35], the serum level of undercarboxylated osteocalcin was an explanatory factor, but no significant difference was seen between groups in this parameter in the present study. This is likely because the capacity for osteocalcin synthesis cannot be assessed by measuring levels of carboxylation. The most important new finding of the present study is that carboxylation should be assessed with reference to the level of osteocalcin synthesis, rather than simply evaluating bone fragility from circulating levels of undercarboxylated osteocalcin. In other words, increased levels of undercarboxylated osteocalcin are a problem, as reported previously [34, 35], but only if there has been no alteration in the level of osteocalcin synthesis. If the ability to synthesize osteocalcin is reduced, we would naturally expect a decrease of undercarboxylated osteocalcin. In the present study, blood levels of undercarboxylated osteocalcin were similar in the FX and OA groups, despite the reduced osteocalcin synthesis capacity in the former group, suggesting a decrease in the extent of carboxylation. Although we have stated that impaired differentiation of osteoblasts was a crucial factor in fragility fractures, at present the only way we have to elucidate the status of osteoblasts is bone biopsy. Determination of bone uptake of aspartic acid, needed to synthesize osteopontin, may be a good predictor of bone vulnerability in combination with serum undercarboxylated osteocalcin levels.
This study has a number of limitations. Firstly, we used patients with end-stage osteoarthritis of the hip as the control group. The femoral heads of these patients contain osteosclerotic lesions and cannot be considered normal bone. However, this was an exploratory study, so we opted for using specimens that could be obtained during routine treatment without additional invasiveness. Another limitation is that many Japanese patients with osteoarthritis of the hip develop it secondarily to dysplasia of the acetabulum. The osteoarthritis group was therefore younger than the fracture group, necessitating statistical adjustment of the patient characteristics. Furthermore, when investigating bone structure it is considered important to assess osteoid and osteocytes in cancellous bone, and we used data obtained by two-dimensional morphometry in the present study. Different results might have been obtained if we had performed microcomputed tomography analysis.
In conclusion, our assessment revealed that the OC/DPD and OPN/Ca ratios of cortical bone are important predictors of fragility fracture and a decrease of non-collagenous protein synthesis by osteoblasts and of osteocalcin uptake are possible causes of fragility fracture.
References
NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis, and Therapy (2001) Osteoporosis prevention, diagnosis, and therapy. JAMA 285:785–795
Seeman E, Delmas PD (2006) Bone quality—the material and structural basis of bone strength and fragility. N Engl J Med 354:2250–2261
Seeman E (2002) Pathogenesis of bone fragility in women and men. Lancet 359:1841–1850
Borah B, Dufresne TE, Chmielewski PA, Johnson TD, Chines A, Manhart MD (2004) Risedronate preserves bone architecture in postmenopausal women with osteoporosis as measured by three-dimensional microcomputed tomography. Bone 34:736–746
Dufresne TE, Chmielewski PA, Manhart MD, Johnson TD, Borah B (2003) Risedronate preserves bone architecture in early postmenopausal women in 1 year as measured by three-dimensional microcomputed tomography. Calcif Tissue Int 73:423–432
Bell KL, Loveridge N, Jordan GR, Power J, Constant CR, Reeve J (2000) A novel mechanism for induction of increased cortical porosity in cases of intracapsular hip fracture. Bone 27:297–304
Jordan GR, Loveridge N, Bell KL, Power J, Rushton N, Reeve J (2000) Spatial clustering of remodeling osteons in the femoral neck cortex: a cause of weakness in hip fracture? Bone 26:305–313
Roschger P, Rinnerthaler S, Yates J, Rodan GA, Fratzl P, Klaushofer K (2001) Alendronate increases degree and uniformity of mineralization in cancellous bone and decreases the porosity in cortical bone of osteoporotic women. Bone 29:185–191
Mori S, Harruff R, Ambrosius W, Burr DB (1997) Trabecular bone volume and microdamage accumulation in the femoral heads of women with and without femoral neck fractures. Bone 21:521–526
Saito M, Fujii K, Soshi S, Tanaka T (2006) Reductions in degree of mineralization and enzymatic collagen cross-links and increases in glycation-induced pentosidine in the femoral neck cortex in cases of femoral neck fracture. Osteoporos Int 17:986–995
Tang SY, Zeenath U, Vashishth D (2007) Effects of non-enzymatic glycation on cancellous bone fragility. Bone 40:1144–1151
Garnero P, Borel O, Gineyts E, Duboeuf F, Solberg H, Bouxsein ML, Christiansen C, Delmas PD (2006) Extracellular post-translational modifications of collagen are major determinants of biomechanical properties of fetal bovine cortical bone. Bone 38:300–309
Viguet-Carrin S, Garnero P, Delmas PD (2006) The role of collagen in bone strength. Osteoporos Int 17:319–336
Vashishth D (2007) The role of the collagen matrix in skeletal fragility. Curr Osteoporos Rep 5:62–66
Saito M, Fujii K, Mori Y, Marumo K (2006) Role of collagen enzymatic and glycation induced cross-links as a determinant of bone quality in spontaneously diabetic WBN/Kob rats. Osteoporos Int 17:1514–1523
Saito M, Mori S, Mashiba T, Komatsubara S, Marumo K (2008) Collagen maturity, glycation-induced pentosidine, and mineralization are increased following 3-year treatment with incadronate in dogs. Osteoporos Int 19:1343–1354
Sarkar S, Mitlak BH, Wong M, Stock JL, Black DM, Harper KD (2002) Relationships between bone mineral density and incident vertebral fracture risk with raloxifene therapy. J Bone Miner Res 17:1–10
Cummings SR, Karpf DB, Harris F, Genant HK, Ensrud K, LaCroix AZ, Black DM (2002) Improvement in spine bone density and reduction in risk of vertebral fractures during treatment with antiresorptive drugs. Am J Med 112:281–289
Kanis JA, Black D, Cooper C, Dargent P, Dawson-Hughes B, De Laet C, Delmas P, Eisman J, Johnell O, Jonsson B, Melton L, Oden A, Papapoulos S, Pols H, Rizzoli R, Silman A, Tenenhouse A (2002) A new approach to the development of assessment guidelines for osteoporosis. Osteoporos Int 13:527–536
Kanis JA, Oden A, Johnell O, Johansson H, De Laet C, Brown J, Burckhardt P, Cooper C, Christiansen C, Cummings S, Eisman JA, Fujiwara S, Gluer C, Goltzman D, Hans D, Krieg MA, La Croix A, McCloskey E, Mellstrom D, Melton LJ 3rd, Pols H, Reeve J, Sanders K, Schott AM, Silman A, Torgerson D, van Staa T, Watts NB, Yoshimura N (2007) The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int 18:1033–1046
Orimo H, Hayashi Y, Fukunaga M, Sone T, Fujiwara S, Shiraki M, Kushida K, Miyamoto S, Soen S, Nishimura J, Oh-Hashi Y, Hosoi T, Gorai I, Tanaka H, Igai T, Kishimoto H (2001) Diagnostic criteria for primary osteoporosis: year 2000 revision. J Bone Miner Metab 19:331–337
Yu W, Gluer CC, Fuerst T, Grampp S, Li J, Lu Y, Genant HK (1995) Influence of degenerative joint disease on spnal bone mineral measurements in postmenopausal women. Calcif Tissue Int 57:169–174
Urano T, Shiraki M, Narusawa K, Usui T, Sasaki N, Hosoi T, Ouchi Y, Nakamura T, Inoue S (2007) Q89R polymorphism in the LDL receptor-related protein 5 gene is associated with spinal osteoarthritis in postmenopausal Japanese women. Spine 32:25–29
Urano T, Narusawa K, Shiraki M, Usui T, Sasaki N, Hosoi T, Ouchi Y, Nakamura T, Inoue S (2007) Association of a single nucleotide polymorphism in the WISP1 gene with spinal osteoarthritis in postmenopausal Japanese women. J Bone Miner Metab 25:253–258
Urano T, Narusawa K, Shiraki M, Usui T, Sasaki N, Hosoi T, Ouchi Y, Nakamura T, Inoue S (2008) Association of a single nucleotide polymorphism in the insulin-like growth factor-1 receptor gene with spinal disc degeneration in postmenopausal Japanese women. Spine 33:1256–1261
Parfitt AM, Drezner MK, Glorieux FH, Kanis JA, Malluche H, Meunier PJ, Ott SM, Recker RR (1987) Bone histomorphometry: standardization of nomenclature, symbols, and units. Report of the ASBMR Histomorphometry Nomenclature Committee. J Bone Miner Res 2:595–610
Ducy P, Desbois C, Boyce B, Pinero G, Story B, Dunstan C, Smith E, Bonadio J, Goldstein S, Gundberg C, Bradley A, Karsenty G (1996) Increased bone formation in osteocalcin-deficient mice. Nature 382:448–452
Ishijima M, Rittling SR, Yamashita T, Tsuji K, Kurosawa H, Nifuji A, Denhardt DT, Noda M (2001) Enhancement of osteoclastic bone resorption and suppression of osteoblastic bone formation in response to reduced mechanical stress do not occur in the absence of osteopontin. J Exp Med 193:399–404
Hunter GK, Hauschka PV, Poole AR, Rosenberg LC, Goldberg HA (1996) Nucleation and inhibition of hydroxyapatite formation by mineralized tissue proteins. Biochem J 317(Pt 1):59–64
Amizuka N, Li M, Kobayashi M, Hara K, Akahane S, Takeuchi K, Freitas PH, Ozawa H, Maeda T, Akiyama Y (2008) Vitamin K2, a gamma-carboxylating factor of gla-proteins, normalizes the bone crystal nucleation impaired by Mg-insufficiency. Histol Histopathol 23:1353–1366
Amizuka N, Li M, Hara K, Kobayashi M, de Freitas PH, Ubaidus S, Oda K, Akiyama Y (2009) Warfarin administration disrupts the assembly of mineralized nodules in the osteoid. J Electron Microsc (Tokyo) 58:55–65
Sodek J, Chen J, Nagata T, Kasugai S, Todescan R Jr, Li IW, Kim RH (1995) Regulation of osteopontin expression in osteoblasts. Ann N Y Acad Sci 760:223–241
Stein GS, van Wijnen AJ, Stein JL, Lian JB, Bidwell JP, Montecino M (1994) Nuclear architecture supports integration of physiological regulatory signals for transcription of cell growth and tissue-specific genes during osteoblast differentiation. J Cell Biochem 55:4–15
Vergnaud P, Garnero P, Meunier PJ, Breart G, Kamihagi K, Delmas PD (1997) Undercarboxylated osteocalcin measured with a specific immunoassay predicts hip fracture in elderly women: the EPIDOS Study. J Clin Endocrinol Metab 82:719–724
Szulc P, Chapuy MC, Meunier PJ, Delmas PD (1993) Serum undercarboxylated osteocalcin is a marker of the risk of hip fracture in elderly women. J Clin Invest 91:1769–1774
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tanaka, S., Narusawa, K., Onishi, H. et al. Lower osteocalcin and osteopontin contents of the femoral head in hip fracture patients than osteoarthritis patients. Osteoporos Int 22, 587–597 (2011). https://doi.org/10.1007/s00198-010-1328-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-010-1328-9