Abstract
Summary
Despite adolescent black females experiencing the highest rates of obesity, the effect of excess fat mass on bone structure and strength in this population is unknown. Our findings in postadolescent black females suggest that excess weight in the form of fat mass may adversely influence cortical bone structure and strength.
Introduction
Although adolescent obesity has been associated with reduced bone structure and strength in white females, this relationship has not been studied in adolescent black females, a population experiencing the highest rates of obesity. Our objective was to compare bone structure and strength between postadolescent black females with normal and high levels of adiposity.
Methods
Black females with ≤32% body fat were classified as normal body fat (NF; n = 33, aged 19.3 ± 1.3 years); females exceeding this cutoff were classified as high body fat (HF; n = 15, aged 19.0 ± 1.1 years). Using peripheral quantitative computed tomography, tibial and radial bones were scanned at the 4% (trabecular) and 20% (cortical) sites from the distal metaphyses. Fat-free soft-tissue mass (FFST) and %body fat were assessed by dual-energy X-ray absorptiometry.
Results
After controlling for either FFST or body weight, the HF vs. NF group had lower total cross-sectional area (CSA; 9–17%), cortical CSA (6–15%), and strength–strain index (SSI; 13–24%) at the cortical site of the tibia (all p < 0.05). At the cortical site of the radius, the HF vs. NF group had lower total CSA (14%, p = 0.03), cortical CSA (9%, p = 0.04), and SSI (15%, p = 0.07) after control for body weight. There were no group differences in either the FFST-adjusted cortical bone values at the radius or in the trabecular bone parameters (body weight- or FFST-adjusted) at the tibia and radius.
Conclusions
Consistent with our adiposity and bone data in late-adolescent white females, our findings in black females entering adulthood also suggest that obesity may adversely influence cortical bone strength.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As the evidence linking childhood obesity to skeletal fractures is mounting [1–7], being overweight may be associated with suboptimal bone growth and development. Determining whether adiposity is either beneficial or detrimental to the growing skeleton has been challenging. For instance, some reports indicate that childhood obesity is associated with greater bone mass at the spine, hip, and total body, even after adjustment for height, sexual maturation, and lean mass [8–11]. Others conclude that obesity is linked to lower bone mass or that extra weight from fat mass had no effect on bone mass [12–14]. Discrepancies in these results may be attributed, in part, to the limitations of using dual-energy X-ray absorptiometry (DXA) when studying the pediatric skeleton [15]. Since DXA-derived bone outcomes are two-dimensional and measure only integral bone, they are confounded by differences in bone and body size and do not differentiate between trabecular and cortical compartments.
Using three-dimensional bone-imaging techniques, such as quantitative computed tomography (QCT) or peripheral QCT (pQCT) to assess skeletal strength in the study of pediatric bone–fat relationships, researchers have shown that fat mass does not provide additional weight-loading benefits to either trabecular bone density at the spine [16] or cortical bone geometry at appendicular skeletal sites [17, 18]. In a 16-month investigation, Wetzsteon et al. [19] found that change in strength–strain index, a pQCT-derived measure of torsional bone strength [20], was associated with change in muscle mass, but not fat mass in overweight children. Taken together, these findings support Frost’s mechanostat theory that the bone adapts primarily to dynamic forces produced by muscle and not static forces imposed by the extra weight of fat [21]. Why bone seems to adapt only to muscle mass and not fat mass is unclear.
Because obesity rates are highest in young African American females, a limitation of the aforementioned bone–fat investigations was that study participants were predominately white children and adolescents. The National Health and Nutrition Examination Survey, 2003–2006, estimated that the overweight prevalence among black females, aged 12 to 19 years, was almost double the rate for white females (28% versus 15%) [22]. If obesity has a negative impact on bone, skeletal health in this population could be a public health concern. However, this notion might seem incongruous given that postmenopausal black females experience fewer fragility fractures than do white females [23]. Racial differences in fragility fractures are thought to be the result of a stronger skeleton in black vs. white individuals that seems to be present in childhood and tracks into adulthood [24–26]. It is possible that the high obesity rates in blacks could be a contributing factor to the racial differences in fracture risk. Since fat mass is a component of body weight, it is plausible that adiposity could induce a stronger bone in blacks because of the extra weight it imposes on the skeleton [27]; however, this proposition warrants further investigation.
In the only investigation to date of the bone–fat relationship in African American youth, Afghani and Goran [28] linked visceral obesity, assessed by QCT, to lower total body bone mass, measured by DXA, in prepubertal black children. Although this finding proposes a potential concern for bone health in a population experiencing high rates of obesity, further work is warranted. In a previous investigation [17], we determined associations between adiposity and pQCT-derived bone parameters in 115 late-adolescent females; however, only two of the participants were of the African American race. As a result, we sought to investigate in a larger sample of black females entering adulthood the effect of adiposity on bone structure and strength. Therefore, in this study, we compared tibial and radial bone structure and strength parameters between two adiposity groups defined as having normal and high levels of body fat. Since muscle size and skeletal size are known to be strong predictors of bone [29–32], it is possible that they may confound the connection between fat and bone. Accordingly, we took into consideration muscle and/or skeletal size as potential confounders in this investigation of the bone–fat relationship.
Methods
Study participants
African American female college students (N = 48; aged 18 to 22 years) attending University of Georgia (UGA) were used in this investigation. We elected to include black females only and the specific age range in order to minimize any confounding effects from race, sex and pubertal maturation on the bone outcome variables. Black or African American race was determined by self-report, in accordance with the National Institutes of Health Policy and Guidelines on the Inclusion of Women and Minorities as Subjects in Clinical Research [33]. All participants must have reported normal menstruation (e.g., greater than or equal to four menstrual periods in the last 6 months) for inclusion in the study. Participants were excluded if they reported significant weight loss or gain in the past 6 months (±10% initial body weight), participation in competitive high-school (grade 9–12) or college athletics, diagnosis of eating disorders, prior skeletal fracture, present illness or chronic disease and/or use of oral contraceptives, dietary supplements or medications known to affect body weight, body fat, or bone metabolism. Procedures were approved by the Institutional Review Board for Human Subjects at UGA, and all participants provided written consent.
Anthropometry
Height and body weight measurements were collected by a trained laboratory technician. Participants were measured for height and weighed in light indoor clothing following the removal of shoes. Height was measured to the nearest 0.1 cm using a wall-mounted stadiometer (Novel Products Inc., Rockton, IL). Body weight was measured to the nearest 0.1 kg using an electronic scale (Seca Bella 840, Columbia, MD). Prior to testing each week, the scale was checked for accuracy using known weights. Recalibration of the scale was not required during the testing sessions. Limb lengths were measured with anthropometric tape (Rosscraft, Inc) to the nearest 0.10 mm at the forearm (distance between the ulnar styloid process and olecranon) and tibia (the distal edge of the medial malleolus to the tibial plateau).
Dual-energy X-ray absorptiometry
Body composition variables [fat mass (kg), fat-free soft-tissue mass (FFST) mass (kg) and percentage body fat] and bone outcomes of the total body [bone mineral content, BMC (g) and bone area (cm2)] were measured using DXA (Delphi A; S/N 70467; Hologic Inc., Bedford, MA). The same technician analyzed all scans using Hologic software, version 11.2. Quality assurance for DXA was performed via calibration against the manufacturer’s three-step soft-tissue wedge (model TBAR; SN 2275) and anthropomorphic spine phantom (model DPA/QDR-1; SN 9374) composed of different thickness levels of aluminum and lucite, calibrated against stearic acid (100% fat) and water (8.6% fat). In our laboratory, a coefficient of variation of 0.36% was observed from 648 scans of the spine phantom over a 3-year period. For determination of measurement reproducibility, one-way random effects model, single measure intraclass correlation coefficients (ICCs) were calculated in females 18–30 years of age (n = 10) scanned twice in our lab during a 7-day period for total body fat mass, FFST mass and %fat (all R ≥ 0.87) and for BMC of the whole body (R = 0.98).
Peripheral quantitative computed tomography
Peripheral QCT (XCT-2000; Stratec Medizintechnic, Pforzheim, Germany) measurements were taken of the nondominant radius and tibia. Radial and tibial measures were taken at the 4% and 20% sites for bone outcomes, proximal to the articular surface of the distal end of the tibia and radius. The 4% and 20% sites represent areas high in trabecular and cortical bone, respectively. Each scan was acquired with a 0.4 mm voxel size and a slice thickness of 2.4 mm. The anatomic reference line (for determination of the distal end of the radius or tibia) was identified by acquisition of a 30-mm planar scout view of the joint line and automatically set by the software at 4% or 20% sites. Image processing and calculation of the various bone measures were determined using the Stratec software (version 5.50d), which allows modal options for the following: Contour Mode for detecting the outer bone edge, Peel Mode for defining the way subcortical and trabecular bone are separated, and Cort Mode for separating cortical bone from trabecular bone.
At the trabecular site of the radius and tibia, total and trabecular vBMD (mg/cm3) and total cross-sectional area (CSA, mm2) were measured using Contour Mode 2 (200 mg/cm3), Peel Mode 2 (400 mg/cm3), and Cort Mode 3 (169 mg/cm3). Using total vBMD and total CSA, bone strength index (mg2/mm4, Eq. 1) was calculated, which reflects the strength of bone against compression [34, 35]. The following bone variables were assessed at the radial and tibial cortical sites: cortical vBMD (mg/cm3), cortical CSA (mm2), total CSA, cortical BMC (mg/mm), cortical thickness (mm), endosteal circumference (mm), and polar strength–strain index (mm3). Cortical bone variables for the 20% site were assessed using Contour Mode 1 (710 mg/cm3), Peel Mode 2 (540 mg/cm2), and Cort Mode 1 (480 mg/cm3). The strength–strain index (mm3), an estimate of torsional bone strength, is calculated as the integrated product of the section modulus and the density of cortical bone Eq. 2. Section modulus is calculated as (a × d 2)/d max, where a is the CSA of a voxel, d is the distance of the voxel from the center of gravity, and d max is the maximum distance of one voxel to the center of gravity. The ratio of cortical vBMD and normal physiological density (ND = 1,200 mg/cm3) provides an estimate of the modulus of elasticity [20].
A third measurement, muscle CSA (mm2), was also assessed at the 66% site of the tibia and radius. All pQCT measures were assessed and analyzed by the same trained operator. The pQCT operator scanned the phantom daily to maintain quality assurance. Test–retest measurements were performed on five females, aged 18 to 24 years, to determine reliability of the pQCT in our laboratory. The one-way random effects model, single measure ICCs for all pQCT measurements were calculated to be R ≥ 0.97.
Definition of adiposity groups
Participants were dichotomized by the DXA-derived percentage body fat cutoff suggested by Going, Lohman, and Falls (Fitnessgram/Activitygram 3rd Edition, The Cooper Institute, Dallas, TX) [36]. Going, Lohman, and Falls [36] indicate that, regardless of race and age (6–18 years), a normal range of percentage body fat for females is 18–32%, while levels >32% body fat are associated with cardiovascular disease risk factors (i.e., hypertension, dyslipidemia, and impaired glucose tolerance) [37–39]. Therefore, females with ≤32% body fat were classified as normal body fat; females exceeding this cutoff were classified as high body fat.
Statistical analyses
Statistical analyses were performed using SPSS version 18.02 for Mac OS X (PASW Statistics, Chicago, IL). A P value ≤ 0.05 was considered statistically significant for all analyses. Normal distribution and homogeneity of variances were confirmed by Shapiro–Wilks W and Levene’s tests, respectively. Pearson’s bivariate correlations were used to examine the associations of body weight, fat mass, and FFST mass with bone variables. Partial Pearson’s correlation coefficients were performed to determine the associations of fat mass with the bone variables, with control for FFST mass. Group differences for anthropometric, body composition, and unadjusted bone variables were determined using unpaired (i.e., independent samples) two-tailed t tests. Descriptive statistics for raw variables are presented as mean ± SD. An F test was performed to test the assumption of homogeneity of regression slopes with regard to the interaction between the independent variables (i.e., adiposity groups) and the covariate (i.e., FFST mass or body weight). Because there were no interactions, analysis of covariance was used to compare the differences in bone response variables between the normal body fat and high body fat groups after adjusting for either FFST mass or body weight differences. Estimated means of bone variables in the adjusted analyses are reported as mean (95% CI).
Sample size determination was estimated using data previously collected in our laboratory [17]. From these data in white females, aged 18–19 years, the mean ± SD tibial bone values in the lowest quartile for total vBMD, cortical CSA, and strength–strain index are 287 ± 35 mg/cm3, 177 ± 15 mm2, and 1101 ± 97 mm3, respectively. Radial bone values in the lowest quartile for total vBMD, cortical CSA, and strength–strain index were 307 ± 40 mg/cm3, 63 ± 7.9 mm2, and 189 ± 20 mm3, respectively. Based on these tibial and radial bone data in white late-adolescent females, we estimated that 12–15 subjects in each adiposity group would provide 81–84% power (α = 0.05) to detect at least a 10% difference in total vBMD, cortical CSA, and strength–strain index at the tibia and radius between adiposity groups (Sample Power, software version 2.0, SPSS, Chicago, IL).
Results
Participant characteristics
Mean age, weight, height, BMI, menarche, FFST, fat mass, percentage body fat, total body BMC, total body bone area, tibial and forearm lengths and muscle CSA, and pQCT-derived bone variables of the participants are provided in Table 1. Age, height, and menarche were not different between adiposity groups. The high body fat group, however, was found to have greater body weight, BMI, FFST mass, and percentage body fat than the normal body fat group (all p < 0.05). There were no significant differences between groups in total body BMC, total body bone area, tibial length, tibial muscle CSA, forearm length, forearm muscle CSA, or the pQCT-derived bone parameters.
Bivariate correlations of body weight, fat mass, and FFST mass with bone measurements
Total body BMC was positively related with weight (r = 0.69, p < 0.01), fat mass (r = 0.52, p < 0.01), and FFST mass (r = 0.79, p < 0.01). Total body bone area was also positively associated with weight (r = 0.72, p < 0.01), fat mass (r = 0.55, p < 0.01), and FFST mass (r = 0.82, p < 0.01).
Among the pQCT-derived bone parameters, body weight was not associated with total vBMD or trabecular vBMD at the trabecular site of the tibia and radius, although it was positively associated with total CSA (tibia; r = 0.26, p = 0.07 and radius; r = 0.33, p = 0.02) and bone strength index (tibia; r = 0.58, p < 0.01 and radius; r = 0.29, p = 0.05). At the cortical bone site, body weight was negatively associated with cortical vBMD at the tibia (r = −0.31, p = 0.04) but not at the radius. At the other cortical sites, however, body weight was positively correlated with cortical CSA, total CSA, cortical BMC, cortical thickness, and strength–strain index at the tibia and radius (\( r = 0.{42} - 0.{63} \), all p < 0.05). Positive relations were observed between fat mass and bone strength index (radius only), cortical CSA, total CSA (cortical site of tibia only), cortical BMC, cortical thickness (tibia only), and strength–strain index (\( r = 0.{3}0 - 0.{47} \), all p < 0.05). Positive associations were also found between FFST mass and total CSA (4% and 20% bone sites), bone strength index, cortical CSA, cortical BMC, cortical thickness (tibia only), endosteal circumference, and strength–strain index (\( r = 0.{42} - 0.{63} \), all p < 0.05). Cortical vBMD at the tibia only was inversely related with fat mass (r = −0.25, p = 0.07) and FFST mass (r = −0.33, p = 0.03).
Partial correlations between fat mass and bone measurements after controlling for FFST mass
After controlling for FFST mass, fat mass was inversely related with cortical CSA (radius only), total CSA (20% site), endosteal circumference (radius only), and strength–strain index (\( r = - 0.{31}\;{\hbox{to}} - 0.{45} \), all p < 0.05). There were no significant relations between fat mass and DXA bone variables or pQCT variables at the trabecular bone site (total vBMD, trabecular vBMD, total CSA, and bone strength index) and the following bone parameters at the cortical bone site: cortical vBMD, cortical CSA (tibia only), cortical BMC, cortical thickness, and endosteal circumference (tibia only).
Bone comparisons between normal- and high fat groups after adjustment for either body weight or FFST mass
Peripheral QCT
Tibia
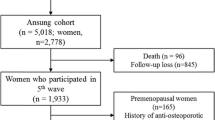
After controlling for body weight, the high body fat vs. normal body fat group had significantly lower total CSA [319.5 (295.6–343.5) vs. 378.1 (362.7–393.4), p < 0.01), cortical CSA [193.0 (180.5–205.6) vs. 224.7 (216.7–232.7), p < 0.01], cortical BMC [230.3 (215.5–244.7) vs. 267.2 (258.0–276.5), P < 0.01], and strength–strain index [1,224 (1,096–1,353) vs. 1,562 (1,480–1,644), p < 0.01]. Table 2 shows similar tibial bone findings between groups at the 20% site after controlling for FFST mass. Specifically, the cortical bone strength (strength–strain index) of the high body fat group was 13% lower than the normal body fat group (p < 0.01; Fig. 1). In the high body fat group, the lower cortical bone strength was due to smaller bone dimensions [total CSA (9%, p = 0.01) and cortical CSA (6%, p = 0.05)] compared to the normal body fat group. No significant differences were observed between adiposity groups at the trabecular bone site of the tibia after controlling for either body weight or FFST mass.
Schematic representation of the average magnitude of difference [A − B/(A + B)/2 × 100] at the cortical site of the tibia and radius, after controlling for either fat-free soft-tissue mass (FFST), in normal body fat (n = 33) vs. high body fat (n = 15) postadolescent black females. The outer white circles represent cortical bone, the textured circles represent trabecular bone and the gray circles represent the medullary cavity. a P < 0.05
Radius
After controlling for body weight, the high body fat vs. normal body fat group had significantly lower total CSA [97.4 (86.6–108.2) vs. 112.5 (105.6–119.4), p = 0.03] and cortical CSA [69.8 (65.1–74.5) vs. 76.2 (73.2–79.2), p = 0.04] at the cortical site. In the high body fat group, the smaller cortical bone dimensions for a given amount of body weight reflected a 15% weaker bone (strength–strain index) compared to the normal body fat group, but the difference did not reach significance [221.2 (189.7–252.8) vs. 257.7 (237.6–277.9), p = 0.07]. There were no significant radial bone differences between groups at the trabecular site after control for body weight. Table 2 displays radial bone values, controlling for FFST mass, of the normal body fat and high body fat groups. At the cortical site, the FFST-adjusted radial bone values tended to follow a similar pattern as the FFST-adjusted tibial bone values, but the differences were smaller in magnitude and did not reach significance (Fig. 1). There were no significant differences between groups at the trabecular bone site after control for FFST mass. Adjusted radial and tibial bone outcomes were also determined for the adiposity groups after control for muscle CSA for each respective bone site, but no significant differences in tibial or radial bone parameters at the trabecular or cortical sites were found between groups (data not shown).
Discussion
In this study of postadolescent black females, we compared bone structure and strength parameters of the tibia and radius between two adiposity groups defined as having normal and high levels of percentage body fat. The unadjusted tibial and radial bone measurements were not significantly different between adiposity groups, even though the high body fat group was carrying significantly greater soft-tissue loads (an average of 14-kg fat mass and 4-kg of FFST mass) than the normal body fat group. After controlling for either the higher FFST mass or the greater body weight in the high body fat group, we observed smaller cortical bone dimensions at the tibia and radius in the high body fat group compared to the normal body fat group. Consistent with our adiposity and bone data in late-adolescent white females [17], our findings in black females entering adulthood also suggest that obesity may adversely influence cortical bone strength.
It has recently been proposed that race may modify the relationship between adiposity and bone. In postmenopausal women, Castro et al. [40] demonstrated that for each unit increase in BMI, the odds ratio for having low aBMD were lower for white women, while black women had slightly higher odds for low aBMD. In prepubertal black and white children, Afghani and Goran [28] observed total abdominal adipose tissue, assessed by QCT, was negatively associated with total body BMC, measured using DXA. However, there were racial differences in the associations of total body BMC with subcutaneous abdominal adipose tissue (SAAT) and visceral adipose tissue (VAT). For instance, an inverse correlation between SAAT and total body BMC was observed in white, but not in black children [28]. Conversely, an inverse association between VAT and total body BMC was found in black, but not in white children [28]. The results in this study and in our analogous work [17] suggest similar relations between total body adiposity and bone structure and strength parameters in young black and white females. We are unable to determine whether race plays a part in the influence of central body adiposity on bone structure and strength, as VAT and SAAT were not assessed in this study or in our previous work [17]. Since obesity-related metabolic abnormalities are more strongly related to visceral adiposity rather than total adiposity, it is worthy to explore whether the influence of visceral adiposity on bone structure and strength is modified by race, as it may provide some insight into why older black females experience fewer fragility fractures than do white females [23].
In developing females, high levels of adipose tissue are associated with an increased production of sex steroids such as estrogen and testosterone [41, 42], although their impact on cortical and trabecular bone in the presence of obesity is unclear. Our data in postadolescent black females suggest that, for a given amount of FFST mass, cortical bone size is more strongly and inversely associated with increasing fat mass compared to the relations that we observed between trabecular bone and adiposity. This lack of relationship between trabecular bone and fat mass was also observed in our previous study in late adolescent white females [17]. In a sample of 677 men, 25–45 years of age, Taes et al. [43] found that fat mass was inversely associated with pQCT-derived cortical bone parameters at both the radius and tibia, after controlling for either body weight or FFST mass. In contrast to our findings, however, the investigators observed negative relations between fat mass and trabecular bone parameters at the radius (trabecular bone parameters at the tibia were not assessed) [43]. One could speculate that because of the variation in estrogen and testosterone concentrations between males and females, these sex steroids may have differential effects on trabecular and cortical bone in the presence of obesity. However, Khosla et al. [44, 45] found that the effects of estrogen and testosterone on trabecular and cortical bone parameters, assessed by pQCT, are similar between young adult males and females. Furthermore, the authors noted that having high levels of estrogen provided no extra skeletal strength benefits for either trabecular or cortical bone, but having low levels of estrogen was more detrimental to trabecular than cortical bone [45]. Estrogen is thought to reduce the bone remodeling threshold on the endosteal surface of cortical bone, thereby sensitizing bone next to marrow to the effect of weight-bearing loads, resulting in greater storage of bone mineral and an increase in bone area [46]. Therefore, it is possible that the lack of association between adiposity and trabecular bone parameters could be attributed to FFST mass being more strongly associated with cortical bone rather than the trabecular bone. Since young overweight black females take part in limited physical activities [47], it is possible that our findings between adiposity and cortical bone size could be the result of low levels of physical activity associated with high levels of body fat. Thus, when we statistically control for surrogates of skeletal loading (e.g., FFST mass or body weight), the observed effect would be greater in (1) cortical vs. trabecular bone and in (2) weight-loaded (tibia) vs. non-weight-loaded (radius) bone. That was the case in both instances in our investigation and in similar studies that assessed cortical and trabecular bone at the tibia and radius [17, 18]. Though we excluded participants who participated in competitive high-school and collegiate sports, we did not collect any information on the types and frequencies of physical activities performed from early to late puberty or any weight history documentations from the participants. Therefore, we are unable to identify which participants engaged in (non-competitive) high impact activities or gained excessive weight due to reduced physical activity during adolescence.
Figure 1 shows a visual representation of the overall effect by which smaller cortical bone dimensions, as was observed in the high body fat group compared with the normal body fat group, had on estimated bone strength (strength–strain index) relative to FFST mass. It is worth noting that in the simple correlation analyses, we found not only FFST mass but also fat mass and body weight to be positively associated with bone parameters at the tibia and radius. Studies have reported positive associations between bone outcomes and body weight or fat mass [9, 12, 48–50]. In our study, however, the strength of these associations was generally greater between the bone parameters and FFST mass rather than fat mass or body weight. FFST mass is predominately muscle and that our bone outcomes were more strongly related to FFST mass is consistent with the Frost mechanostat theory of bone development, which suggests bone adaptation is driven primarily by changes in mechanical load [21]. Since fat mass is a component of body weight, it is indeed possible that adiposity may have a protective effect on the skeleton due to the extra weight it imposes on bone as a mechanical load [27]. Therefore, in addition to our bone analyses controlling for FFST mass differences, we also present bone data between adiposity groups, controlling for body weight. The magnitude of differences between adiposity groups (lower in high body fat vs. normal body fat group) seems to be greater in the body weight-adjusted bone outcomes compared to the FFST mass-adjusted bone outcomes. Similarly, Zhao et al. [51], studying 6,477 Chinese and Caucasian adults ranging in age from 19–90 years of age, found that fat mass was negatively correlated with DXA-derived bone mass, when the mechanical loading effect of body weight was statistically removed. Beck et al. [52] reported similar findings between fat mass and DXA-derived hip structural parameters, after controlling for body weight, in 4,642 postmenopausal women in the Women’s Health Initiative Observational Study. Using pQCT, Ducher et al. [18] showed that, once controlling for forearm length and body weight differences, overweight children had a smaller cortical bone at the radius than normal-weight children. These study findings along with our data would suggest that bone strength of heavier individuals might not be adequate for their higher body weight. However, these bone findings, controlling for body weight, must be interpreted with caution, as the negative association between fat mass and bone outcomes may just be due to the FFST mass having a larger positive effect on bone outcomes than fat mass [53].
The present study has several strengths. First, this study evaluated the effect of excess fat mass on bone structure and strength parameters, assessed by pQCT, at weight-bearing (tibia) and non-weight-bearing (radius) skeletal sites that have not been previously reported in postadolescent black females. In addition, studying only postadolescent black females minimized the degree of variability in factors known to influence bone such as race, sex, and maturational status. Lastly, by grouping the black females by percent body fat (rather than BMI), we exclude the possibility of misclassification of those with high levels of body fat that may have otherwise been classified as normal weight if BMI had been used for the grouping procedure. In contrast, we acknowledge several limitations. In addition to not having historical information on weight-bearing activities and weight status history, another limitation was that our study utilized cross-sectional data and thus was not specifically designed to examine the longitudinal effects of adiposity and bone development. It is also important to note that we did not assess biochemical parameters indicative of metabolic abnormalities, which could have had an effect on bone independent of adiposity. For instance, obese individuals suffer from hyperleptinemia rather than leptin deficiency [54]. Animal studies reveal that leptin treatment elicits a bimodal response, where low doses of leptin can stimulate bone formation and prevent bone loss, but high concentrations of leptin suppress bone formation and increase bone resorption [55]. Obesity is also associated with other metabolic disturbances such insulin resistance and increased inflammation, which both conditions have shown to hinder bone growth [56]. Future studies should include an assessment of endocrine factors to explore these issues.
In summary, our results suggest that excess fat mass may adversely influence cortical bone structure and strength in African American females entering adulthood. Thus, the negative contribution of adipose tissue seems to offset its potential benefit as a mechanical load. Although our study suggests a concern for bone health in a population experiencing the highest rates of obesity, prospective research is needed to confirm a cause and effect relationship that considers physical inactivity, metabolic abnormalities, and environmental influences.
References
Goulding A, Cannan R, Williams SM, Gold EJ, Taylor RW, Lewis-Barned NJ (1998) Bone mineral density in girls with forearm fractures. J Bone Miner Res 13:143–148
Goulding A, Jones IE, Taylor RW, Manning PJ, Williams SM (2000) More broken bones: a 4-year double cohort study of young girls with and without distal forearm fractures. J Bone Miner Res 15:2011–2018
Skaggs DL, Loro ML, Pitukcheewanont P, Tolo V, Gilsanz V (2001) Increased body weight and decreased radial cross-sectional dimensions in girls with forearm fractures. J Bone Miner Res 16:1337–1342
Goulding A, Grant AM, Williams SM (2005) Bone and body composition of children and adolescents with repeated forearm fractures. J Bone Miner Res 20:2090–2096
Taylor ED, Theim KR, Mirch MC, Ghorbani S, Tanofsky-Kraff M, Adler-Wailes DC, Brady S, Reynolds JC, Calis KA, Yanovski JA (2006) Orthopedic complications of overweight in children and adolescents. Pediatrics 117:2167–2174
Pollack KM, Xie D, Arbogast KB, Durbin DR (2008) Body mass index and injury risk among US children 9–15 years old in motor vehicle crashes. Inj Prev 14:366–371
Dimitri P, Wales J, Bishop N (2009) Fat and bone in children-differential effects of obesity on bone size and mass according to fracture history. J Bone Miner Res. 25(3):527–536
De Schepper J, Van den Broeck M, Jonckheer MH (1995) Study of lumbar spine bone mineral density in obese children. Acta Paediatr 84:313–315
Ellis KJ, Shypailo RJ, Wong WW, Abrams SA (2003) Bone mineral mass in overweight and obese children: diminished or enhanced? Acta Diabetol 40(Suppl 1):S274–S277
Leonard MB, Shults J, Wilson BA, Tershakovec AM, Zemel BS (2004) Obesity during childhood and adolescence augments bone mass and bone dimensions. Am J Clin Nutr 80:514–523
Clark EM, Ness AR, Tobias JH (2006) Adipose tissue stimulates bone growth in prepubertal children. J Clin Endocrinol Metab 91:2534–2541
Goulding A, Taylor RW, Jones IE, McAuley KA, Manning PJ, Williams SM (2000) Overweight and obese children have low bone mass and area for their weight. Int J Obes Relat Metab Disord 24:627–632
Goulding A, Taylor RW, Jones IE, Manning PJ, Williams SM (2002) Spinal overload: a concern for obese children and adolescents? Osteoporos Int 13:835–840
Petit MA, Beck TJ, Shults J, Zemel BS, Foster BJ, Leonard MB (2005) Proximal femur bone geometry is appropriately adapted to lean mass in overweight children and adolescents. Bone 36:568–576
Gordon CM, Bachrach LK, Carpenter TO, Crabtree N, El-Hajj Fuleihan G, Kutilek S, Lorenc RS, Tosi LL, Ward KA, Ward LM, Kalkwarf HJ (2008) Dual energy X-ray absorptiometry interpretation and reporting in children and adolescents: the 2007 ISCD Pediatric Official Positions. J Clin Densitom 11:43–58
Janicka A, Wren TA, Sanchez MM, Dorey F, Kim PS, Mittelman SD, Gilsanz V (2007) Fat mass is not beneficial to bone in adolescents and young adults. J Clin Endocrinol Metab 92:143–147
Pollock NK, Laing EM, Baile CA, Hamrick MW, Hall DB, Lewis RD (2007) Is adiposity advantageous for bone strength? A peripheral quantitative computed tomography study in late adolescent females. Am J Clin Nutr 86:1530–1538
Ducher G, Bass SL, Naughton GA, Eser P, Telford RD, Daly RM (2009) Overweight children have a greater proportion of fat mass relative to muscle mass in the upper limbs than in the lower limbs: implications for bone strength at the distal forearm. Am J Clin Nutr 90:1104–1111
Wetzsteon RJ, Petit MA, Macdonald HM, Hughes JM, Beck TJ, McKay HA (2008) Bone structure and volumetric BMD in overweight children: a longitudinal study. J Bone Miner Res 23:1946–1953
FJ SH, Tysarczqk-Niemeyer G, Willnecker J (1996) Non-invasive bone strength index as analyzed y peripheral quantitative computed tomography (pQCT). In: Schoenau E (ed) Pediatric osteology: new developments in diagnosis and therapy. Elsevier, Amsterdam, The Netherlands, pp 141–166
Frost H (1987) Bone “mass” and the “mechanostat”: a proposal. Anat Rec 219:1–9
Ogden CL, Carroll MD, Flegal KM (2008) High body mass index for age among US children and adolescents, 2003–2006. JAMA 299:2401–2405
Barrett-Connor E, Siris ES, Wehren LE, Miller PD, Abbott TA, Berger ML, Santora AC, Sherwood LM (2005) Osteoporosis and fracture risk in women of different ethnic groups. J Bone Miner Res 20:185–194
Gilsanz V, Roe TF, Mora S, Costin G, Goodman WG (1991) Changes in vertebral bone density in black girls and white girls during childhood and puberty. N Engl J Med 325:1597–1600
Gilsanz V, Skaggs DL, Kovanlikaya A, Sayre J, Loro ML, Kaufman F, Korenman SG (1998) Differential effect of race on the axial and appendicular skeletons of children. J Clin Endocrinol Metab 83:1420–1427
Wetzsteon RJ, Hughes JM, Kaufman BC, Vazquez G, Stoffregen TA, Stovitz SD, Petit MA (2009) Ethnic differences in bone geometry and strength are apparent in childhood. Bone 44:970–975
Reid IR (2008) Relationships between fat and bone. Osteoporos Int 19:595–606
Afghani A, Goran MI (2006) Racial differences in the association of subcutaneous and visceral fat on bone mineral content in prepubertal children. Calcif Tissue Int 79:383–388
Seeman E (1998) Growth in bone mass and size—are racial and gender differences in bone mineral density more apparent than real? J Clin Endocrinol Metab 83:1414–1419
Petit MA, Beck TJ, Kontulainen SA (2005) Examining the developing bone: what do we measure and how do we do it? J Musculoskelet Neuronal Interact 5:213–224
Klein GL, Fitzpatrick LA, Langman CB, Beck TJ, Carpenter TO, Gilsanz V, Holm IA, Leonard MB, Specker BL (2005) The state of pediatric bone: summary of the ASBMR pediatric bone initiative. J Bone Miner Res 20:2075–2081
Schoenau E (2005) From mechanostat theory to development of the “Functional Muscle-Bone-Unit”. J Musculoskelet Neuronal Interact 5:232–238
National Institutes of Health Office of Extramural Research. NIH Policy and Guidelines on the Inclusion of Women and Minorities as Subjects in Clinical Research. In
Martin RB (1991) Determinants of the mechanical properties of bones. J Biomech 24(Suppl 1):79–88
Kontulainen SA, Johnston JD, Liu D, Leung C, Oxland TR, McKay HA (2008) Strength indices from pQCT imaging predict up to 85% of variance in bone failure properties at tibial epiphysis and diaphysis. J Musculoskelet Neuronal Interact 8:401–409
Going SB, Lohman TG, Falls HB (2008) Body composition assessments. In Welk GJ, Meredith, MD (ed) Fitnessgram-activitygram reference guide. The Cooper Institute, pp 10.11-10.18. http://www.cooperinstitute.org/ourkidshealth/fitnessgram/references.cfm. Accessed on December 20, 2009
Berenson GS, Webber LS, Srinivasan SR, Voors AW, Harsha DW, Dalferes ER Jr (1982) Biochemical and anthropometric determinants of serum beta- and pre-beta-lipoproteins in children. Bogalusa Heart Study. Arteriosclerosis 2:325–334
Aristimuno GG, Foster TA, Voors AW, Srinivasan SR, Berenson GS (1984) Influence of persistent obesity in children on cardiovascular risk factors: the Bogalusa Heart Study. Circulation 69:895–904
Williams DP, Going SB, Lohman TG, Harsha DW, Srinivasan SR, Webber LS, Berenson GS (1992) Body fatness and risk for elevated blood pressure, total cholesterol, and serum lipoprotein ratios in children and adolescents. Am J Public Health 82:358–363
Castro JP, Joseph LA, Shin JJ, Arora SK, Nicasio J, Shatzkes J, Raklyar I, Erlikh I, Pantone V, Bahtiyar G, Chandler L, Pabon L, Choudhry S, Ghadiri N, Gosukonda P, Muniyappa R, Von-Gicyzki H, McFarlane SI (2005) Differential effect of obesity on bone mineral density in White, Hispanic and African American women: a cross sectional study. Nutr Metab (Lond) 2:9
Klein KO, Larmore KA, de Lancey E, Brown JM, Considine RV, Hassink SG (1998) Effect of obesity on estradiol level, and its relationship to leptin, bone maturation, and bone mineral density in children. J Clin Endocrinol Metab 83:3469–3475
McCartney CR, Blank SK, Prendergast KA, Chhabra S, Eagleson CA, Helm KD, Yoo R, Chang RJ, Foster CM, Caprio S, Marshall JC (2007) Obesity and sex steroid changes across puberty: evidence for marked hyperandrogenemia in pre- and early pubertal obese girls. J Clin Endocrinol Metab 92:430–436
Taes YE, Lapauw B, Vanbillemont G, Bogaert V, De Bacquer D, Zmierczak H, Goemaere S, Kaufman JM (2009) Fat mass is negatively associated with cortical bone size in young healthy male siblings. J Clin Endocrinol Metab 94:2325–2331
Khosla S, Melton LJ 3rd, Robb RA, Camp JJ, Atkinson EJ, Oberg AL, Rouleau PA, Riggs BL (2005) Relationship of volumetric BMD and structural parameters at different skeletal sites to sex steroid levels in men. J Bone Miner Res 20:730–740
Khosla S, Riggs BL, Robb RA, Camp JJ, Achenbach SJ, Oberg AL, Rouleau PA, Melton LJ 3rd (2005) Relationship of volumetric bone density and structural parameters at different skeletal sites to sex steroid levels in women. J Clin Endocrinol Metab 90:5096–5103
Schiessl H, Frost HM, Jee WS (1998) Estrogen and bone-muscle strength and mass relationships. Bone 22:1–6
Kimm SY, Glynn NW, Kriska AM, Barton BA, Kronsberg SS, Daniels SR, Crawford PB, Sabry ZI, Liu K (2002) Decline in physical activity in black girls and white girls during adolescence. N Engl J Med 347:709–715
Reid IR, Ames R, Evans MC, Sharpe S, Gamble G, France JT, Lim TM, Cundy TF (1992) Determinants of total body and regional bone mineral density in normal postmenopausal women—a key role for fat mass. J Clin Endocrinol Metab 75:45–51
Reid IR (2002) Relationships among body mass, its components, and bone. Bone 31:547–555
Ackerman A, Thornton JC, Wang J, Pierson RN Jr, Horlick M (2006) Sex difference in the effect of puberty on the relationship between fat mass and bone mass in 926 healthy subjects, 6 to 18 years old. Obesity (Silver Spring) 14:819–825
Zhao LJ, Liu YJ, Liu PY, Hamilton J, Recker RR, Deng HW (2007) Relationship of obesity with osteoporosis. J Clin Endocrinol Metab 92:1640–1646
Beck TJ, Petit MA, Wu G, LeBoff MS, Cauley JA, Chen Z (2009) Does obesity really make the femur stronger? BMD, geometry, and fracture incidence in the women's health initiative-observational study. J Bone Miner Res 24:1369–1379
Wang MC, Bachrach LK, Van Loan M, Hudes M, Flegal KM, Crawford PB (2005) The relative contributions of lean tissue mass and fat mass to bone density in young women. Bone 37:474–481
Maffei M, Halaas J, Ravussin E, Pratley RE, Lee GH, Zhang Y, Fei H, Kim S, Lallone R, Ranganathan S et al (1995) Leptin levels in human and rodent: measurement of plasma leptin and ob RNA in obese and weight-reduced subjects. Nat Med 1:1155–1161
Martin A, David V, Malaval L, Lafage-Proust MH, Vico L, Thomas T (2007) Opposite effects of leptin on bone metabolism: a dose-dependent balance related to energy intake and insulin-like growth factor-I pathway. Endocrinology 148:3419–3425
Parhami F, Morrow AD, Balucan J, Leitinger N, Watson AD, Tintut Y, Berliner JA, Demer LL (1997) Lipid oxidation products have opposite effects on calcifying vascular cell and bone cell differentiation. A possible explanation for the paradox of arterial calcification in osteoporotic patients. Arterioscler Thromb Vasc Biol 17:680–687
Acknowledgments
The authors are extremely grateful to the study subjects for their participation. We also thank Ruth Taylor, Ashley Ferira, and Maria Breen for coordinating the project. NKP, RDL, EML, MWH, CAB, and DBH were responsible for the study concept and design; NKP, EML, and RDL were responsible for the acquisition of the data. NKP and DBH conducted the statistical analyses. NKP, RDL, EML, and DBH, and were responsible for the interpretation of the data and drafting the manuscript. All authors contributed to the revision of the manuscript. None of the authors had any personal or financial conflicts of interest.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Funding sources
The University of Georgia Research Foundation and College of Family and Consumer Sciences
Rights and permissions
About this article
Cite this article
Pollock, N.K., Laing, E.M., Hamrick, M.W. et al. Bone and fat relationships in postadolescent black females: a pQCT study. Osteoporos Int 22, 655–665 (2011). https://doi.org/10.1007/s00198-010-1266-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-010-1266-6