Abstract
Summary
Few studies have evaluated the effects of homocysteine and methylenetetrahydrofolate reductase (MTHFR) genotype on age-related bone loss. In our 5-year cohort study with 1,213 women aged 70–85 years, high homocysteine is associated with greater hip bone loss but not fracture risk. The effect of MTHFR genotype on bone density and fracture is weak.
Introduction
Previous studies on the effects of homocysteine and MTHFR genotype on bone mineral density (BMD) and osteoporotic fracture risk have shown inconsistent results. Few studies have evaluated their effects on age-related bone loss. We evaluated the effects of homocysteine and MTHFR genotype variation on hip BMD and fracture risk over 5 years in a cohort of 1,213 community-dwelling women aged 70–85 years.
Methods
Nutritional intake and prevalent fracture status were assessed at baseline, plasma homocysteine was measured at year 1, and hip dual-energy X-ray absorptiometry (DXA) BMD was measured at years 1 and 5. Clinical incident osteoporotic fractures confirmed by radiographic report were collected throughout the study and the MTHFR gene C677T and A1298C polymorphisms genotyped. Data were analyzed using analysis of covariance and Cox proportional hazard regression.
Results
The highest tertile of homocysteine was associated with a greater hip BMD loss over 4 years (−2.8%) compared to the middle (−1.6%) and lowest tertiles (−1.2%) (P < 0.001). This effect remained after adjustment for covariates. There was no effect of homocysteine on fracture prevalence or incidence. MTHFR gene variation was only weakly related to one of the bone outcome measures.
Conclusion
In this study population, high homocysteine is associated with greater hip bone loss but not fracture risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introductions
The hypothesis that high homocysteine concentrations could have a deleterious effect on the skeleton has gained some support recently. It has been suggested that high homocysteine concentrations may interfere with collagen cross-linking, a hypothesis supported by Lubec et al. [1] who demonstrated that the bone effects seen in homocysteinuric subjects was associated with defects in collagen cross-linking rather than collagen synthesis compared to matched controls. A reduction in collagen cross-links could result in compromised bone strength and stability and may, therefore, lead to increased fracture susceptibility.
However, there is little agreement on the presence or size of the effect of high homocysteine levels on bone density and fracture risk. Some epidemiological studies have found an association between high homocysteine and low bone mineral density (BMD) [2–4] or increased fracture risk [5–7], while others have not shown any effects on BMD [5, 8, 9] or fracture [3, 10]. Recent randomized controlled trials aimed at lowering plasma homocysteine using B vitamin dietary interventions have also produced variable results. One showed evidence of hip fracture reduction post stroke [11], whereas another showed no effect of fractures of all types [12]. The third one did not show any effect on bone turnover markers [13]. The reasons for the differences in findings may relate to the age of subjects, statistical power, differing environmental backgrounds, or different ethnicity.
Increased homocysteine concentrations are associated with inadequate folate intake, as folate deficiency decreases 5,10-methylenetetrahydrofolate reductase (MTHFR) and reduces homocysteine conversion to methionine. Increased homocysteine concentrations are also associated with inadequate intakes of a variety of B vitamins, including riboflavin, vitamin B6, and vitamin B12 [14, 15], and genetic variation in the MTHFR and CβS genes [16, 17]. Linkage studies have identified an association between low BMD with the 1p36 region on chromosome 1 in the vicinity of the MTHFR gene [18, 19]. However, studies on the association between MTHFR genotype and BMD and fracture risk have yielded inconsistent results [2, 20]. Some studies have suggested that the effects of MTHFR genotype on bone density depends on dietary folate and riboflavin intakes or folate status [21–23].
Few of the abovementioned studies evaluated the effects of homocysteine or MTHFR genotype on age-related bone loss in a longitudinal design. The aims of this 5-year cohort study is to evaluate the effects of high homocysteine concentrations and MTHFR polymorphisms on bone density, age-related bone loss, and fracture risk in a cohort of community-dwelling elderly Australian women aged 70–85 years at baseline. We also examined the association between various nutritional and genetic factors and homocysteine concentration.
Materials and methods
Subjects
The study cohort comprised 1,213 women selected at random from a study population of 1,500 women of Caucasian origin aged between 70 and 85 years in whom plasma homocysteine was measured at 1 year. These subjects were recruited from the Western Australian general population of women over 70 years of age for a 5-year prospective randomized controlled cohort trial of supplemental oral calcium to prevent osteoporotic fractures [24]. A letter was sent to 24,800 individuals selected at random from the electoral roll, which has the names and addresses of all women of this age. Of the 4,312 women who responded to the letter, 34% joined the study. No subjects had any medical condition likely to influence 5-year survival and subjects were not taking bone-related medication including calcium supplements, estrogen, bisphosphonates, and vitamin D. Although women enrolled in this study were weighted in favor of those in higher socioeconomic categories, they did not differ from the whole population in health resource utilization [25]. Subjects were randomized to receive 1.2 g of calcium carbonate daily or matched placebo during the study. Informed consent was obtained from all subjects and the Human Research Ethics Committee of the University of Western Australia approved the study. This study was undertaken in compliance with national legislation and the Declaration of Helsinki.
Demographic and lifestyle assessments
At baseline, demographic information including smoking history and the number of falls in the past 3 months was obtained by questionnaire. Height and weight of the subjects were measured while wearing light clothing and without shoes and body mass index (BMI) in kilograms per square meter was calculated. Dietary intake of a broad range of nutrients was ascertained by a validated food frequency questionnaires (FFQ) [26, 27] and nutrient density per 1,000 kJ was calculated for protein, fat, calcium, thiamine, riboflavin, and folate. Physical activity level was assessed by a questionnaire [25, 28], and activity levels were calculated in kilocalories per day using a validated method utilizing body weight, questions on the number of hours and type of physical activity, and energy costs of such activities [29, 30].
Bone mineral densitometry
At 1 and 5 years, dual-energy X-ray absorptiometry (DXA) bone density was measured at the hip on a Hologic Acclaim 4500A fan beam densitometer (Hologic, Waltham, MA, USA). The coefficient of variation at the total hip was 1.2% [31]. Of those who had homocysteine concentration measured at baseline, 984 had hip BMD measured at 1 year and 815 had 4-year change hip BMD available for analysis.
Fractures
At baseline, prevalent fractures were determined by obtaining a fracture history from each subject that included age at the time of fracture, the site, and how the fracture was sustained. A prevalent fracture was included if the fracture occurred after the age of 50 years; occurred with minimal trauma as defined by falling from a height of 1 m or less; and not of the face, skull, fingers, or toes.
During the 5-year study, atraumatic incident clinical fractures and atraumatic symptomatic vertebral fractures were reported in an adverse events diary which was collected every 4 months. The diagnosis of vertebral and nonvertebral fractures was confirmed by reference to radiographic records.
Biochemistry
At 1 year, blood samples were collected from the 1,213 subjects after an overnight fast and analyzed for red cell folate and plasma homocysteine. Because suboptimal sampling conditions may lead to glycolysis, which can double homocysteine concentrations, special care was taken with the samples for total homocysteine analysis with the plasma separated by centrifugation shortly after venipuncture and transport in ice-cooled containers. Total plasma homocysteine was determined by reverse phase high-performance liquid chromatography after treatment with tributylphosphine, deproteinization, and fluorogenic derivatization by the method of Araki and Sako [32]. The interassay coefficient of variation was 6% in our laboratory. Red cell folate was determined by immunoassay using the Immulite 2000 instrument.
At baseline, fasting blood creatinine was measured using a routine laboratory method and the glomerular filtration rate (GFR) was estimate by the Cockcroft–Gault equation [33].
Genotyping
Genotyping of two nonsynonymous single nucleotide polymorphisms of the MTHFR gene was undertaken. The C677T (rs1801133) polymorphism in exon 5 results in the substitution of valine for alanine at position 222 and the A1298C (rs1801131) polymorphism in exon 8 results in the substitution of a glutamic acid for an alanine at position 429. Genotyping for the C677T polymorphism was determined by Hinfl digestion [34] and for the A1298C polymorphism was determined by MboII digestion [35] of the PCR products.
Statistical analysis
Descriptive statistics are reported as the mean±SD and differences as the mean±SEM for all variables unless otherwise stated. The homogeneity of variance and normality assumptions were checked by visual inspection of residuals from analysis of variance models and by using Kolmogorov–Smirnov goodness-of-fit test, respectively. Correlation analysis was undertaken using the Spearman rank test. Agreement of genotype frequencies with Hardy–Weinberg equilibrium was determined by a chi-square goodness-of-fit test. The effects of MTHFR genotype–diet interaction on plasma homocysteine were examined by testing the significance of interaction terms in linear regression models.
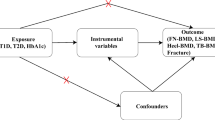
Subjects were grouped according to the tertile of homocysteine concentration. The association of homocysteine tertiles or different MTHFR alleles with cross-sectional and longitudinal measures of BMD was examined using analysis of variance (ANOVA). Further analyses were made by analysis of covariance (ANCOVA) adjusting for covariates. Post hoc comparisons were made by Bonferroni test. The significance of homocysteine tertiles or different MTHFR alleles on prevalent fracture was determined using chi-square analyses, and their effects on incident fractures were examined using Cox proportional hazard regression adjusting for baseline age and weight, 1 year hip BMD, prevalent fracture, and calcium treatment. As the effects of calcium supplementation on fracture prevention have been reported to be dependent on patients’ compliance [24], compliance with study tablets was adjusted in all multivariate analysis. A P value of 0.05 or lower in two-tailed testing was considered significant. The statistical analyses were performed using SPSS 15 software (SPSS, Chicago, IL, USA).
Results
Cohort characteristics
The cohort was aged 75.2 ± 2.7 years at baseline; the mean homocysteine concentration was 12.1 ± 4.6 μmol/L. When subjects were grouped according to the tertile of plasma homocysteine concentrations, high homocysteine is associated with increased age and weight; reduced intakes of folate, thiamine, riboflavin, protein, and calcium; a higher intake of fat; and reduced physical activity, red cell folate concentration, and estimated GFR (Table 1). There were no significances between the three tertiles in the percentage of subjects who received calcium supplementation, their compliance with the study tablets, or smoking history.
Homocysteine and homocysteine covariate effects on hip DXA BMD and fracture
There was no difference in the hip DXA BMD measured at 1 year across the homocysteine tertile groups (Table 2). However, high homocysteine levels were associated with greater loss in hip DXA BMD from year 1 to 5 (Table 2). The percentage reduction in the highest tertile (−2.8 ± 0.4%) was significantly greater than that of the middle tertile (−1.6 ± 0.3%) and the lowest tertile (−1.2 ± 0.3%) (P < 0.001).
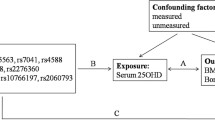
Further analysis was made by ANCOVA adjusting for covariates that are correlated with homocysteine as shown in Table 1 and are potential determinants of bone structure. These covariates demonstrated a positive association with total hip BMD at 1 year in bivariate correlation analysis: baseline age (r = −0.122, P < 0.001), body weight (r = 0.51, P < 0.001), height (r = 0.13, P < 0.001), physical activity (r = 0.07, P = 0.013), estimated GFR (r = 0.30, P < 0.001), intakes of energy, protein, fat, calcium, folate, riboflavin, and thiamine (r = 0.07–0.14, P < 0.01), and red cell folate measured at 1 year (r = 0.07, P = 0.042). The effects of homocysteine on changes in hip BMD over 4 years remained after adjustment for these factors, calcium treatment group, and compliance with study tablets (Fig. 1). The adjusted hip bone loss in the highest tertile (21 ± 3 mg/cm2) was 2.6-fold greater than that of the lowest tertile (8 ± 3 mg/cm2, P = 0.008) and 1.9-fold greater than that of the middle tertile (11 ± 3 mg/cm2, P = 0.039).
Estimated marginal means (SEM) of change in total hip BMD from year 1 to year 5. Adjusted for intakes of energy, protein, fat, calcium, folate, thiamine, and riboflavin, age, body weight, height, daily energy expenditure, estimated GFR, red cell folate, smoking history, calcium treatment group, and compliance with study tablets, F = 5.090, P = 0.006. Bars with different lower case letters are significantly different, P < 0.05 (ANCOVA with Bonferroni test)
At baseline, 324 (26.6%) of the subjects had sustained one or more atraumatic fractures after the age of 50 years. During the 60-month observation period, 209 (17.3%) of the subjects sustained at least one incident fracture confirmed by radiological report. There was no relationship between homocysteine concentration and prevalent or incident fracture risk (Table 2). There was no relationship between dietary folate intake or red cell folate and bone structural or fracture parameters (data not shown).
Effects of MTHFR genotypes and nutritional intake on homocysteine
MTHFR polymorphism C677T
The frequencies of the MTHFR polymorphism C677T CC, CT, and TT genotypes were 40%, 48%, and 12%, respectively. The C and T allele frequencies were determined to be 64% and 36%, respectively, and were in Hardy–Weinberg equilibrium (χ 2 = 1.90, P = 0.39). Demographic and dietary characteristics were not different across the C677T genotype groups (data not shown).
An interaction between both dietary folate and dietary riboflavin intake and C677T genotype was observed, such that those with a TT genotype and low dietary folate or low dietary riboflavin intake had higher homocysteine concentrations (Table 3). These effects remained after adjustment for age and estimated GFR (data not shown).
MTHFR polymorphism A1298C
The frequencies of the MTHFR polymorphism A1298C AA, AC, and CC genotypes were 49%, 41%, and 10%, respectively. The A and C allele frequencies were determined to be 70% and 30%, respectively, and were in Hardy–Weinberg equilibrium (χ 2 = 1.17, P = 0.56). Demographic and dietary characteristics were not different across the A1298C genotype groups (data not shown). The homocysteine concentration was higher in those with an AA genotype compared to those with an AC but not those with a CC genotype (Table 3). No interaction between dietary folate or dietary riboflavin intake and the A1298C genotype on homocysteine concentration was observed (Table 3).
MTHFR genotypes, bone mass, and fracture risk
MTHFR polymorphism C677T
The MTHFR polymorphism C677T was not associated with BMD at 12 months, 4-year change in hip BMD, or prevalent and incident fracture (Table 4). No interaction between low dietary folate, dietary riboflavin, or red cell folate and the C677T genotype was observed on hip DXA BMD or fracture (data not shown).
MTHFR polymorphism A1298C
There were no associations with MTHFR A1298C polymorphisms and BMD at 12 months or the 4-year change in hip BMD (Table 4). However, the CC genotype was associated with a greater number of prevalent fractures (36.8%) compared to those with the other two genotypes AA and AC (25.6%, χ 2 = 6.64, P = 0.01) but showed no relationship with incident fracture (Table 4). No interaction between low dietary folate, dietary riboflavin, or red cell folate and the A1298C genotype was observed on hip DXA BMD or fracture (data not shown).
Discussion
In this cohort study with 1,213 women aged 70–85 years at baseline, we found that high homocysteine is associated with greater hip bone loss over 4 years, and this effect persisted after accounting for confounding factors such as body size, dietary nutrient intakes, physical activity, and renal function. There were no effects of homocysteine on fracture prevalence and incidence. Although an interaction between dietary folate and riboflavin intake and MTHFR C677T genotype was observed and those individuals with a TT genotype and low dietary folate or riboflavin intake had higher homocysteine concentrations, there were no correlation between MTHFR C677T genotype and hip BMD and fracture. MTHFR A1298C genotype was only weakly related to one of the bone outcome measures being a high prevalent fracture rate observed in those with CC genotype.
Factors associated with homocysteine
The mean homocysteine concentration of our study population (12.1 ± 4.6 μmol/L) was similar to other female populations [2, 6]. As expected, those in the upper tertile of homocysteine concentration (>12.7 μmol/L) had a lower red cell folate and folate intake. Consistent with previous reports, individuals with a high homocysteine also had poor nutrition and lifestyle, as shown by a higher fat intake [36] and lower calcium [10], riboflavin [14, 15] and protein intakes [37], reduced physical activity [10, 38], and a reduced estimated GFR [39]. In addition, we noted an association between high homocysteine and low thiamine intake, an association not previously reported. Because of the strong cocorrelations between B vitamin intakes in this population, it is possible that the association between thiamine intake and homocysteine reflects the effects of other B vitamins on homocysteine rather than a direct effect of thiamine on homocysteine metabolism. One limitation of the study is that the FFQ dietary analysis did not provide information on the intakes of vitamin B6 and B12, which has been reported to be related to homocysteine concentration [14]. Another limitation of the study is that we did not evaluate the association between homocysteine levels and some medications, such as anti-epileptic, lipid-lowering, and antihypertensive drugs, that have been reported to influence homocysteine levels [40, 41].
Consistent with previous analyses [15, 42, 43], an increased plasma homocysteine level was observed in those with the MTHFR C677T TT genotype and either low folate intake or low riboflavin intake. These data support that this polymorphism impairs the MTHFR enzyme activity and thus the conversion of homocysteine to methionine, especially in the presence of suboptimal levels of dietary folate and riboflavin, which are both necessary for the conversion.
Effect of homocysteine on hip BMD and fracture
Some previous cross-sectional studies have found an association between high homocysteine and low BMD [2–4], while others have not [5, 8, 9]. Few studies have evaluated the effects of homocysteine on age-related bone loss. In the present study, we found that subjects in the highest tertile of homocysteine had 1.2–1.6% greater hip bone loss over 4 years compared to those in the middle and lowest tertiles. Because subjects with different homocysteine levels varied in factors, such as body size, dietary intakes of protein and calcium, and physical activity, that have been shown to influence bone mass [28, 44], these associates of high plasma homocysteine were accounted for in the adjusted analysis. The association of high homocysteine with greater hip bone loss persisted after accounting for these confounding factors. Our study did not find an association between homocysteine and hip BMD measured at 1 year. The reason could be that homocysteine measured at 1 year in this cohort may not reflect past exposure.
In the present study, we did not find any relationship between homocysteine concentrations and prevalent fracture and incident fracture over the 5-year follow-up period. This is in agreement with studies in postmenopausal women [3, 10] but not with other studies of both male and female subjects [5–7]. The reasons for the differences in findings may relate to the age of subjects, lack of power, differing environmental backgrounds, or different ethnicity. Two of the previous studies showed significant effects of homocysteine on fracture risk also showed that the association was stronger in men than in women [6, 7].
In this study, although lower concentrations of red cell folate and lower levels of dietary folate intakes were seen in those in the highest homocysteine tertile, red cell folate and dietary folate were not associated with BMD at 1 year or the change in hip BMD. Others, however, have found that plasma folate, rather than homocysteine, was related to BMD [8]. In addition, in contrast to the study with Iranian women aged 60.8 ± 6.8 years which showed that the association between homocysteine and BMD was no longer significant after adjusting for folate intake [2], we found that the effect of homocysteine on hip bone loss remained after adjustment for folate intake and red cell folate status. This could be because that our subjects are older and many factors other than folate intake influence homocysteine levels.
Effects of MTHFR genotype on hip BMD and fracture
Despite previous findings that showed that the MTHFR TT genotype was associated with low BMD and increased fracture incidence in early postmenopausal women [20], in the present study, there were no associations between C677T MTHFR genotype and hip BMD or fracture. Furthermore, although a few previous studies have shown that the effects of MTHFR genotype on bone density depends on folate and riboflavin intakes or folate status [21–23] and as mentioned above there was an interaction between dietary folate and riboflavin intake and MTHFR C677T genotype on homocysteine concentrations in the present study, no interaction between low dietary folate, dietary riboflavin, or red cell folate and the C677T genotype was observed on hip DXA BMD or fracture in the present study.
The data in relations to the A1298C polymorphism was inconsistent in that the CC allele was associated with a lower prevalent fracture but not incident rate. Because the fracture finding is not supported by data on improved bone structure, this relationship may due to chance association.
The significance of these data for the use of B vitamins for fracture prevention relates to the large number of dietary and genetic factors that may influence the response to therapy. The one randomized controlled trial that showed evidence of hip fracture reduction post stroke was undertaken in a population with a very high baseline homocysteine levels and a high risk of hip fracture due to a previous hemiplegia [11]. Furthermore, at the end of the study, there was a 60% difference in the homocysteine levels. In the study that showed no effect of dietary interventions using B vitamins on fracture rates [12], the authors point out that the homocysteine levels were 42% lower than those of the Japanese study mentioned above [11] and the serum folate levels were five times higher. Furthermore, the dose of B vitamins was about half of that reported in the Japanese study.
In conclusion, this report has evaluated many interacting nutritional and genetic variables affecting homocysteine concentration and bone density. It is clear that homocysteine may be a reflection of many factors that may have independent effects on impairing skeletal form and function. However, although adjustment for these covariates removed some effects, these data support an independent effect of homocysteine on hip bone loss in elderly women aged over 70 years. Although this is not sufficient to be associated with a clear fracture effect, it may merit further investigation in populations with particularly low B vitamin intake or high prevalence of certain MTHFR genotypes.
References
Lubec B, Fang-Kircher S, Lubec T, Blom HJ, Boers GH (1996) Evidence for McKusick’s hypothesis of deficient collagen cross-linking in patients with homocystinuria. Biochim Biophys Acta 1315:159–162
Golbahar J, Hamidi A, Aminzadeh MA, Omrani GR (2004) Association of plasma folate, plasma total homocysteine, but not methylenetetrahydrofolate reductase C667T polymorphism, with bone mineral density in postmenopausal Iranian women: a cross-sectional study. Bone 35:760–765
Gerdhem P, Ivaska KK, Isaksson A, Pettersson K, Vaananen HK, Obrant KJ, Akesson K (2007) Associations between homocysteine, bone turnover, BMD, mortality, and fracture risk in elderly women. J Bone Miner Res 22:127–134
Morris MS, Jacques PF, Selhub J (2005) Relation between homocysteine and B-vitamin status indicators and bone mineral density in older Americans. Bone 37:234–242
van Meurs JB, Dhonukshe-Rutten RA, Pluijm SM, van der Klift M, de Jonge R, Lindemans J, de Groot LC, Hofman A, Witteman JC, van Leeuwen JP, Breteler MM, Lips P, Pols HA, Uitterlinden AG (2004) Homocysteine levels and the risk of osteoporotic fracture. N Engl J Med 350:2033–2041
McLean RR, Jacques PF, Selhub J, Tucker KL, Samelson EJ, Broe KE, Hannan MT, Cupples LA, Kiel DP (2004) Homocysteine as a predictive factor for hip fracture in older persons. N Engl J Med 350:2042–2049
Dhonukshe-Rutten RA, Pluijm SM, de Groot LC, Lips P, Smit JH, van Staveren WA (2005) Homocysteine and vitamin B12 status relate to bone turnover markers, broadband ultrasound attenuation, and fractures in healthy elderly people. J Bone Miner Res 20:921–929
Cagnacci A, Baldassari F, Rivolta G, Arangino S, Volpe A (2003) Relation of homocysteine, folate, and vitamin B12 to bone mineral density of postmenopausal women. Bone 33:956–959
Herrmann M, Kraenzlin M, Pape G, Sand-Hill M, Herrmann W (2005) Relation between homocysteine and biochemical bone turnover markers and bone mineral density in peri- and post-menopausal women. Clin Chem Lab Med 43:1118–1123
Perier MA, Gineyts E, Munoz F, Sornay-Rendu E, Delmas PD (2007) Homocysteine and fracture risk in postmenopausal women: the OFELY study. Osteoporos Int 18:1329–1336
Sato Y, Honda Y, Iwamoto J, Kanoko T, Satoh K (2005) Effect of folate and mecobalamin on hip fractures in patients with stroke: a randomized controlled trial. JAMA 293:1082–1088
Sawka AM, Ray JG, Yi Q, Josse RG, Lonn E (2007) Randomized clinical trial of homocysteine level lowering therapy and fractures. Arch Intern Med 167:2136–2139
Green TJ, McMahon JA, Skeaff CM, Williams SM, Whiting SJ (2007) Lowering homocysteine with B vitamins has no effect on biomarkers of bone turnover in older persons: a 2-y randomized controlled trial. Am J Clin Nutr 85:460–464
Jacques PF, Bostom AG, Wilson PWF, Rich S, Rosenberg IH, Selhub J (2001) Determinants of plasma total homocysteine concentration in the Framingham Offspring cohort. Am J Clin Nutr 73:613–621
Hustad S, Ueland PM, Vollset SE, Zhang Y, Bjorke-Monsen AL, Schneede J (2000) Riboflavin as a determinant of plasma total homocysteine: effect modification by the methylenetetrahydrofolate reductase C677T polymorphism. Clin Chem 46:1065–1071
Dekou V, Whincup P, Papacosta O, Ebrahim S, Lennon L, Ueland PM, Refsum H, Humphries SE, Gudnason V (2001) The effect of the C677T and A1298C polymorphisms in the methylenetetrahydrofolate reductase gene on homocysteine levels in elderly men and women from the British regional heart study. Atherosclerosis 154:659–666
Lievers KJ, Kluijtmans LA, Blom HJ, Wilson PW, Selhub J, Ordovas JM (2006) Association of a 31 bp VNTR in the CBS gene with postload homocysteine concentrations in the Framingham Offspring Study. Eur J Hum Genet 14:1125–1129
Devoto M, Shimoya K, Caminis J, Ott J, Tenenhouse A, Whyte MP, Sereda L, Hall S, Considine E, Williams CJ, Tromp G, Kuivaniemi H, Ala-Kokko L, Prockop DJ, Spotila LD (1998) First-stage autosomal genome screen in extended pedigrees suggests genes predisposing to low bone mineral density on chromosomes 1p, 2p and 4q. Eur J Hum Genet 6:151–157
Wilson SG, Reed PW, Bansal A, Chiano M, Lindersson M, Langdown M, Prince RL, Thompson D, Thompson E, Bailey M, Kleyn PW, Sambrook P, Shi MM, Spector TD (2003) Comparison of genome screens for two independent cohorts provides replication of suggestive linkage of bone mineral density to 3p21 and 1p36. Am J Hum Genet 72:144–155
Abrahamsen B, Madsen JS, Tofteng CL, Stilgren L, Bladbjerg EM, Kristensen SR, Brixen K, Mosekilde L (2003) A common methylenetetrahydrofolate reductase (C677T) polymorphism is associated with low bone mineral density and increased fracture incidence after menopause: longitudinal data from the Danish osteoporosis prevention study. J Bone Miner Res 18:723–729
McLean RR, Karasik D, Selhub J, Tucker KL, Ordovas JM, Russo GT, Cupples LA, Jacques PF, Kiel DP (2004) Association of a common polymorphism in the methylenetetrahydrofolate reductase (MTHFR) gene with bone phenotypes depends on plasma folate status. J Bone Miner Res 19:410–418
Abrahamsen B, Madsen JS, Tofteng CL, Stilgren L, Bladbjerg EM, Kristensen SR, Brixen K, Mosekilde L (2005) Are effects of MTHFR (C677T) genotype on BMD confined to women with low folate and riboflavin intake? Analysis of food records from the Danish osteoporosis prevention study. Bone 36:577–583
Macdonald HM, McGuigan FE, Fraser WD, New SA, Ralston SH, Reid DM (2004) Methylenetetrahydrofolate reductase polymorphism interacts with riboflavin intake to influence bone mineral density. Bone 35:957–964
Prince RL, Devine A, Dhaliwal SS, Dick IM (2006) Effects of calcium supplementation on clinical fracture and bone structure: results of a 5-year, double-blind, placebo-controlled trial in elderly women. Arch Intern Med 166:869–875
Bruce DG, Devine A, Prince RL (2002) Recreational physical activity levels in healthy older women: the importance of fear of falling. J Am Geriatr Soc 50:84–89
Ireland P, Jolley D, Giles G, O’Dea K, Powles J, Ritishauser I, Wahlqvist ML, Williams J (1994) Development of the Melbourne FFQ: a food frequency questionnaire for use in an Australian prospective study involving an ethnically diverse cohort. Asia Pac J Clin Nutr 3:19–31
Hodge A, Patterson AJ, Brown WJ, Ireland P, Giles G (2000) The Anti Cancer Council of Victoria FFQ: relative validity of nutrient intakes compared with weighed food records in young to middle-aged women in a study of iron supplementation. Aust N Z J Public Health 24:576–583
Devine A, Dhaliwal SS, Dick IM, Bollerslev J, Prince RL (2004) Physical activity and calcium consumption are important determinants of lower limb bone mass in older women. J Bone Miner Res 19:1634–1639
McArdle WD, Katch FI, Katch VL (1991) Energy, nutrition and human performance. Lea & Febiger, Philadelphia, PA
Pollock ML, Wilmore JH, Fox SM (1978) Health and fitness through physical activity. Wiley, New York, NY
Henzell S, Dhaliwal S, Pontifex R, Gill F, Price R, Retallack R, Prince R (2000) Precision error of fan-beam dual x-ray absorptiometry scans at spine, hip, and forearm. J Clin Densitom 3:359–364
Araki A, Sako Y (1987) Determination of free and total homocysteine in human plasma by high-performance liquid chromatography with fluorescence detection. J Chromatogr 422:43–52
Cockcroft DW, Gault MH (1976) Prediction of creatinine clearance from serum creatinine. Nephron 16:31–41
McQuillan BM, Beilby JP, Nidorf M, Thompson PL, Hung J (1999) Hyperhomocysteinemia but not the C677T mutation of methylenetetrahydrofolate reductase is an independent risk determinant of carotid wall thickening. The Perth Carotid Ultrasound Disease Assessment Study (CUDAS). Circulation 99:2383–2388
van der Put NM, Gabreels F, Stevens EM, Smeitink JA, Trijbels FJ, Eskes TK, van den Heuvel LP, Blom HJ (1998) A second common mutation in the methylenetetrahydrofolate reductase gene: an additional risk factor for neural-tube defects? Am J Hum Genet 62:1044–1051
Berstad P, Konstantinova SV, Refsum H, Nurk E, Vollset SE, Tell GS, Ueland PM, Drevon CA, Ursin G (2007) Dietary fat and plasma total homocysteine concentrations in 2 adult age groups: the Hordaland Homocysteine Study. Am J Clin Nutr 85:1598–1605
Stolzenberg-Solomon RZ, Miller ER 3rd, Maguire MG, Selhub J, Appel LJ (1999) Association of dietary protein intake and coffee consumption with serum homocysteine concentrations in an older population. Am J Clin Nutr 69:467–475
Nygard O, Vollset SE, Refsum H, Stensvold I, Tverdal A, Nordrehaug JE, Ueland M, Kvale G (1995) Total plasma homocysteine and cardiovascular risk profile. The Hordaland Homocysteine Study. JAMA 274:1526–1533
Friedman AN, Bostom AG, Selhub J, Levey AS, Rosenberg IH (2001) The kidney and homocysteine metabolism. J Am Soc Nephrol 12:2181–2189
Sener U, Zorlu Y, Karaguzel O, Ozdamar O, Coker I, Topbas M (2006) Effects of common anti-epileptic drug monotherapy on serum levels of homocysteine, vitamin B12, folic acid and vitamin B6. Seizure 15:79–85
Dierkes J, Luley C, Westphal S (2007) Effect of lipid-lowering and anti-hypertensive drugs on plasma homocysteine levels. Vasc Health Risk Manag 3:99–108
Girelli D, Martinelli N, Pizzolo F, Friso S, Olivieri O, Stranieri C, Trabetti E, Faccini G, Tinazzi E, Pignatti PF, Corrocher R (2003) The interaction between MTHFR 677 C→T genotype and folate status is a determinant of coronary atherosclerosis risk. J Nutr 133:1281–1285
Kim KN, Kim YJ, Chang N (2004) Effects of the interaction between the C677T 5,10-methylenetetrahydrofolate reductase polymorphism and serum B vitamins on homocysteine levels in pregnant women. Eur J Clin Nutr 58:10–16
Devine A, Dick IM, Islam AF, Dhaliwal SS, Prince RL (2005) Protein consumption is an important predictor of lower limb bone mass in elderly women. Am J Clin Nutr 81:1423–1428
Acknowledgment
We thank all study participants for their cooperation. This study was supported by research grants from the Healthway Health Promotion Foundation of Western Australia, Australasian Menopause Society and the Australian National Health Medical Research Council (project grant 254627 and 303169).
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhu, K., Beilby, J., Dick, I.M. et al. The effects of homocysteine and MTHFR genotype on hip bone loss and fracture risk in elderly women. Osteoporos Int 20, 1183–1191 (2009). https://doi.org/10.1007/s00198-008-0804-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-008-0804-y