Abstract
Summary
The health and economic burden of osteopenia- and osteoporosis-attributable hip fractures (OHF) in Germany was estimated for 2002 and projected until 2050. We found 108,341 OHF resulting in 2,998 million Euros cost, which will more than double by the year 2050, calling for improvement and development of prevention strategies for OHF.
Introduction
This study aimed to estimate the health impact and the societal costs of OHF in Germany in the year 2002 and to extrapolate these estimates to the years 2020 and 2050.
Methods
We estimated OHF-attributable deaths, years of potential life lost (YPLL) and quality-adjusted life years lost (QALYs) using attributable fractions. Direct costs for acute treatment, rehabilitation, nursing care, non-medical costs and indirect costs for sickness absence, early retirement and mortality were estimated. All estimates were extrapolated to 2020 and 2050 using an estimation of future population composition and life expectancy.
Results
We found 108,341 OHF resulting in 3,485 deaths, 22,724 YPLL, 114,058 QALYs, 2,736 millions of Euros direct cost and 262 millions of Euros indirect costs. Projection to 2020 showed corresponding increases of 44%, 62%, 56%, 49%, 47% and 33%, whereas the projection to 2050 resulted in changes of 128%, 215%, 196%, 152%, 138% and 90%, respectively.
Conclusions
OHF have considerable impact on health and direct costs in the elderly. Both may strongly increase in future decades due to demographic changes, calling for improvement and development of effective strategies for preventing and dealing with OHF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteopenia and osteoporosis are reductions in bone density that are found widespread especially among postmenopausal females [1]. Such decreases lead to a reduction of stability of bones, creating a considerable risk factor for various types of fractures [2]. Hip fractures (HF), the fractures of this type with the severest consequences, can be traced to osteoporosis to an ever greater extent with increasing age. This is particularly problematic, since the percentage of the elderly in the population of industrial societies is expected to increase sharply in the next decades (demographic change) [3]. This leads to an increasing prevalence of osteopenia, osteoporosis and complications resulting from HF [4].
There are various ways to estimate the health impact resulting from osteopenia- and osteoporosis-attributable hip fractures (OHF). The determination of OHF-attributable mortality in a population allows an initial estimate of the health impact of OHF. Based on OHF-attributable mortality, years of potential life lost (YPLL) and the loss of quality-adjusted life years (QALYs) can be determined. YPLL provide the average remaining life that a person who died from HF would have experienced without HF, viewed purely statistically from their point of death. In determining QALYs, the remaining life is weighted with an index score of health-related quality of life. Morbidity plays—next to mortality—a decisive role in determining the health impact of a risk factor. For example, morbidity is demonstrated in hospital stays, rehabilitation, nursing care or early retirement. In addition, both mortality and morbidity are connected with societal costs which must also be considered when comprehensively assessing the risk factors osteopenia and osteoporosis. There are two cost categories: direct and indirect costs. Direct costs correspond to the use of resources from medical care for an illness. Indirect costs correspond to the loss of production resulting from the morbidity and mortality of an illness for society. The human capital approach is normally used to determine indirect costs. With this approach, the expected productivity of all future life years of deceased or of persons retiring early are considered.
In a first step, this study aimed to estimate OHF-attributable deaths, YPLL, the use of health services, direct and indirect costs as well as QALY losses for OHF cases occurring in Germany in 2002. In a second step, a projection of future health impact followed, taking expected demographic change into consideration. To accomplish this, the health impact for 2002 determined in step 1 was extrapolated onto the years 2020 and 2050.
Materials and methods
Osteopenia- and osteoporosis-attributable fraction
To estimate the proportion of morbidity and mortality through HF due to osteopenia and osteoporosis, age- and gender-specific osteopenia- and osteoporosis-attributable fractions (OAF) were calculated. In calculating the OAF, data on osteopenia and osteoporosis prevalence P i in the risk class i (i = 0, 1, 2) were combined with data on the relative fracture risk RR i in the risk class i [5]:
The risk classes i were defined according to the World Health Organization classification [2]: 0 = normal bone density (T score ≥ −1), 1 = osteopenia (−1 > T score ≥ −2.5), 2 = osteoporosis (T score < −2.5). We took the prevalence of osteopenia and osteoporosis in Germany from a study by Wildner ([6], personal communication). In this study, the prevalence of osteopenia and osteoporosis were determined in gender-specific segments for the age groups 20–29 years, for 30–89 years old in 5-year age segments and for over 89 years old. The resulting OAF are shown in Table 1.
For the bone mineral density (BMD)-dependent relative risk for HF, a value of 2.6 per standard deviation was used [7]. For the standard deviation, the T score values were used, corresponding to the risk class i.
Mortality and years of potential life lost
The calculation of mortality and YPLL due to OHF was based on an official statistic [8], listing all deaths in Germany by age, gender and cause of death (four-figure ICD-10 code). The OHF-attributable deaths were determined by age- and gender-specific multiplication of the OAF with the number of deaths due to hip fracture. To determine the YPLL, the average remaining years of life of OHF-attributable deaths was determined from death records for Germany [9].
Resource utilisation and direct costs
We determined direct costs for inpatient treatment, rehabilitation, outpatient treatment, nursing care and non-medical costs from health protection, rescue services, administration, research, education, investments and other facilities.
Our first step was to determine the OHF cases that occurred in 2002. This was based on an official statistic listing all hospital cases and days in Germany by age, gender and four-digit ICD-10 code [10]. The OHF cases were estimated by age- and gender-specific multiplication of the HF cases listed in this statistic with the OAF.
To determine the direct costs from OHF-attributable hospital stays and rehabilitation, we determined age- and gender-specific OHF-attributable inpatient care days and valued them via the average costs of an inpatient day [11]. To calculate inpatient days for rehabilitation, we used an official statistic [12] recording all rehabilitation cases in Germany for the first time in 2004. To find out rehabilitations for 2002, we determined the proportion of HF patients receiving rehabilitation after a hospital stay in 2004. This proportion was allocated to the inpatient OHF cases for 2002.
Calculating outpatient costs included physician costs, other medical services, medication, other medical products and other medical facilities. Calculations used the cost of illness assessment of the Federal Statistical Office [13], which provides the best evidence available for the outpatient sector. This assessment lists gender-specific costs for the diagnosis group S70–S79. To determine OHF-attributable costs, we assumed that the proportion of direct OHF costs in the costs for S70–S79 corresponded to the proportion of inpatient OHF cases in the inpatient S70–S79 cases.
The number of current and future nursing care cases was determined with a study by Osnes et al. [14]. They reported age-specific probabilities for outpatient or inpatient nursing care needs based on HF. These probabilities were multiplied by the OHF cases (minus OHF-attributable deaths) and corrected for the age- and gender-specific probability of already being a nursing home case [15], the future probability of becoming a nursing home case without HF, and the future probability of dying. To determine direct costs for nursing care, the current and future nursing care cases were multiplied by the costs for inpatient and outpatient nursing care [15]. In this study, the first year was taken into consideration by 50% to correct for time differences in the appearances of cases within the year. Costs of future years were discounted with a discount rate of 5% per year.
The direct OHF-attributable costs for health protection, rescue services, administration and other facilities were taken from the same statistic as with outpatient costs [13] and were calculated analogous to the outpatient costs. Direct costs for research, education and investments were taken from a statistic providing the entire expenditures of these areas without further delineation [16]. To determine the OHF-attributable share in these costs, we determined the gender-specific proportions of all OHF-attributable medical costs in the entire medical costs [13] and applied them to the total costs for research, education and investments.
Indirect costs
Among indirect costs, we considered loss of productivity from OHF-attributable sickness absence, early retirement and mortality using the human capital approach. Future costs were discounted by 5% per year.
Production was the total production from paid and unpaid work. For paid work, we used average age- and gender-specific wages [17], corrected by the employer’s proportion of contributions to social security [18] and by the age- and gender-specific probability that a person would work at all [19] as productivity. Productivity from unpaid work resulted from age- and gender-specific time used for unpaid work [20] multiplied by the net wages of housekeeping help (7.10 Euros [20]).
To estimate indirect costs for sickness absence, we multiplied the average of 19.4 days per OHF case for females and 25.4 days for males [21] plus the estimated OHF-attributable rehabilitation days with the productivity. The Association of Germans Retirement Insurers (VDR) provides information on age- and gender-specific HF-associated early retirement [22]. Since the loss of resources with early retirement is permanent, future years were also considered and discounted by 5% per year. For the first year, half of the loss of productivity was used to correct for the different times at which the cases appeared in the first year. Indirect costs through mortality were calculated analogously to the calculation for early retirement, but, in this study, based on the estimated OHF age- and gender-specific attributable deaths.
Quality-adjusted life years lost
We determined QALY losses for the first 2 years following fracture, for OHF-attributable nursing care and for OHF-attributable mortality.
The basis for determining the QALY loss through fracture were the estimated OHF cases. To avoid double counting, we subtracted the OHF-attributable deaths from the OHF cases. Based on data provided by Brazier et al. [23] and Hiligsmann et al. [24], we assumed a QALY loss per HF of 0.2 QALYs for the first year and 0.1 QALYs for the second year after HF.
The health-related quality of life of people becoming a long-term nursing care case through the HF should be negatively affected in the long-term. To estimate QALY losses, we multiplied the QALY loss used for the second post-fracture year with the estimated future nursing care cases, starting in the third year after fracture.
The calculation of OHF-attributable QALY losses from mortality was conducted analogously to the calculation of OHF-attributable YPLL, by weighting the YPLL with age- and gender-specific EQ-5D index values. The EQ-5D is a short generic quality of life questionnaire that can be used to determine preference-based index values of health-related quality of life [25]. König et al. [26] measured the EQ-5D health states of the general German population in a representative random sample. Based on these health states, age- and gender-specific EQ-5D index values for the German general population were calculated with an algorithm from Dolan et al. [25] and used as QALY weights.
Projection to the years 2020 and 2050
An increasing life expectancy and decreasing birth rate in Germany and in other western nations is causing a change in the age structure of society. The German Federal Office of Statistics has simulated the distribution of the population among various age groups as well as the death rates for 2020 and 2050 [3]. This simulation serves as a basis for the prognosis of the OHF-attributable burden of illness in 2020 and 2050. We determined the age- and gender-specific OHF-attributable health impact per inhabitant for the year 2002 and extrapolated it to the expected inhabitants for 2020 and 2050. In calculating YPLL, QALYs and future costs beyond the target years (2020 and 2050) from nursing care, mortality and early retirement, we used the life tables predicted for 2020 and 2050 as a basis. We determined expected costs just as we did for the calculation for 2002. Prices for 2002 were used, and corresponding future costs were discounted at a rate of 5% per year from the corresponding target year.
Sensitivity analysis
To test the robustness of our results, we varied the most important parameters in a sensitivity analysis. In particular, we used the following parameter variations:
-
Variations of the BMD-dependent relative risks per standard deviation (2.6) by ±50%,
-
Use of age-dependent relative risks, published by Johnell et al. [27],
-
Limiting the analysis to persons 55 years old or older,
-
Discounting future costs by 0% and 7%,
-
Not considering unpaid work or valuing it with the costs of a household worker (net salary plus payments to social security),
-
Variations of the post-fracture QALY loss by ±50%,
-
Consideration of a secular trend of 1% increase of incidence per year for projections for the years 2020 and 2050.
Results
OHF cases
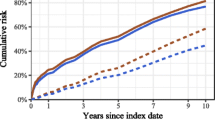
In 2002, osteopenia and osteoporosis caused a total of 108,341 OHF cases (Table 1), 85% of which were in persons over 70 years and 78% in females. Interestingly, OHF occurred more frequently in males than in females in all age groups up to the age group 55–59 years. Beginning with the age group 60–64 years, the frequency was clearly greater in females. Figure 1 shows the OHF cases per one million inhabitants for the year 2002 by age groups. As can be seen, the OHF cases per one million inhabitants increased exponentially with age in both genders, whilst the increase was greater among females than among males.
Projecting OHF cases onto the years 2020 and 2050 led to an increase of OHF cases by 44% in 2020 and 128% in 2050 (Table 1). Age- and gender-specific differences were obvious. In 2020, the number of fractures decreased in the age groups up to 45–49 years, and in 2050, the number decreased in even higher age groups. There was a greater increase in the number of cases with males than with females. The cases increased more than twice as much with males as they did with females.
Mortality, YPLL, QALYs and resource utilisation
In 2002, the OHF resulted in 3,485 deaths, which corresponded to 22,724 YPLL—this was on average 6.5 YPLL per death—and 17,535 lost QALYs (Table 2). Compared with the QALY loss from morbidity, the QALY loss from mortality was relatively low, corresponding to only 26.4% of the entire QALY loss, whilst 46.0% of the entire QALY loss resulted from the HF alone. In the years 2020 and 2050, the deaths increased by 62% and 215%, respectively, whilst the YPLL increased by 56% and 196%, respectively. We noticed that—compared with OHF cases—the deaths as well as the YPLL and the QALYs increased over-proportionally especially in males.
The 108,341 OHF cases in 2002 resulted in a use of about 2.2 million hospital days, corresponding to 20.3 days per OHF on average. About one-fifth of these patients used inpatient rehabilitation after hospital treatment. More than half needed outpatient or inpatient nursing care. Aside from the OHF-attributable mortality, about 2.8 million sick leave days and 168 early retirement cases were calculated into the indirect costs. Early retirement was the only parameter in which the males clearly took the lead over the females. This resulted from the fact that most early retirement cases occurred during years in which more males than females suffered an OHF. Projecting onto the years 2020 and 2050 demonstrates an over-proportionally strong increase in outpatient treatment, nursing care and non-medical costs compared to the OHF cases. Days of hospital stay and days of sick leave increased approximately as strong as the OHF cases, whilst rehabilitations and early retirement cases increased over-proportionally. In 2050, the number of early retirement cases actually decreased compared to 2002.
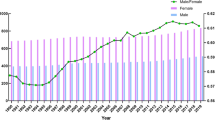
Direct and indirect costs
Table 3 shows that OHF caused 2,998 million Euros of total costs in 2002. Of the total costs, 91.3% were direct costs, of which 80.4% originated from females. More than half of the direct costs were caused by nursing care; yet one must observe that nursing care costs also included future costs. Nursing care costs from only the first year were 142 (26) million Euros for females (males). Acute hospital treatment took second place with 750 million Euros, followed by non-medical costs at 249 million Euros.
The indirect OHF-attributable costs were relatively low compared with direct costs. This resulted from the fact that OHF occurred primarily in a higher age in which no paid productivity and only slight unpaid productivity are done. The highest indirect costs came from mortality (117 million Euros), followed closely by sickness absence (97 million Euros). Interestingly, the proportion of indirect costs falling on males was 42%, clearly higher than with direct costs (19.6%). This resulted from higher salaries and higher employment rates for males in comparison to females.
Projecting direct costs onto the years 2020 and 2050 showed a cost increase corresponding to the development in the case numbers with the exception of nursing care and rehabilitation. Yet costs for nursing care increased over-proportionally, whilst costs for rehabilitation developed under-proportionally. Indirect costs for paid work in 2020 corresponded approximately to those in 2002, whilst they decreased by up to 19% in 2050. In contrast, indirect costs for unpaid work increased by between 22% and 53% in 2020. In 2050, indirect costs from unpaid work increased by 89% in sickness absence and by 15% with mortality, whilst indirect costs decreased by 2% with early retirement.
Figure 2 shows age- and gender-specific direct and total costs per OHF case. All OHF-attributable costs per case ranged between 14,000 and 36,000 Euros.
Without recording nursing care, the direct OHF-attributable costs took a course of slowly increasing values up to the 75- to 79-year age group; after this group, the costs decreased slightly. Beginning with the 60- to 64-year age group, we also included costs of nursing care, which caused about a threefold increase in the OHF-attributable direct costs. After the initial peak of the nursing care costs in the 60- to 64-year age group, the nursing care costs per case were then decreasing, since an increase in age causes a decrease in the expected life years left, which in turn decreases the future nursing care costs per case. In the 75- to 79-year age group, the nursing care costs increased again, since beginning with this age group the percentage of persons needing inpatient nursing care after HF almost doubled, rising from 6% to 11%.
The indirect OHF-attributable costs per case increased with males up to the 40- to 44-year age group. Then the costs decreased as a result of a sinking productivity in the life years left. In females, the indirect OHF-attributable costs per case already began to decrease in the 25- to 29-year age group. This resulted primarily from the fact that the average gross monthly salary for females reaches its maximum in the 30- to 35-year age group and then decreases. Beginning in the 60- to 64-year age group for males and females, almost no additional indirect costs per case appear, since almost no paid work and only limited unpaid work is performed.
Sensitivity analysis
Table 4 shows that an increase of the BMD-dependent relative risk of 50% only leads to a narrow variation of the results—between 7.3% and 25.0%. The variations were more pronounced with males than with females and were the strongest with indirect costs. These both resulted from the fact that the variation of relative risk primarily affected the OAF in young working groups, which, compared with older working groups, contained significantly more males than females. The 50% reduction of the BMD-dependent relative risk led to variations of the results between −50.6% and −68.3%. Again, the variations in males were stronger than in females and were the strongest with indirect costs. But the gender-specific differences were smaller than the differences resulting from risk increase. Using age-dependent relative risks increased attributable fractions up to the age of 75 but decreased attributable fractions beyond this age. Since the majority of fractures occurs beyond the age of 75, this resulted in slight decreases for nearly all estimated outcomes, which were most pronounced among deaths, decreasing between 10.6% and 13.8%. However, among men, indirect costs increased by 10.4% for 2002, 7.2% for 2020 and 0.3% for 2050. This resulted from the fact that a considerable portion of hip fractures in men occurred among younger age groups, which have high indirect costs from paid work.
Only considering those over 55 years led to very heterogeneous variations of the results. The strongest variations were in indirect costs, which decreased by up to 45% in males and up to 8.2% in females. It was also noticeable that the case numbers in males in 2002 decreased by 12% and for females by 1.7%, which resulted from the differing distribution of cases among the various age groups. The rest of the results varied relatively little, whilst the percentage change in males was sometimes considerably greater than in females.
Not discounting future costs increased the direct costs (indirect costs) by 14.8% to 16.2% (17.1% to 31.0%), whilst a discount rate of 7% reduced the direct costs (indirect costs) by 4.3% to 4.4% (4.7% to 7.4%). Not considering unpaid work led to a substantial decrease of indirect costs of up to 96.8%, whilst valuing unpaid work in with the gross salary of a household helper increased indirect costs by up to 115.8%. Considering a secular trend increased all results in 2020 by 19.6% and in 2050 by 61.2%.
Discussion
We estimated 108,341 OHF, a result similar to a study by Häussler et al. [28], which calculated 99,973 OHF for Germany. As expected with the prevalence of osteopenia and osteoporosis, OHF occurred above all in females and in higher age groups. Yet more OHF occurred in males up to the 55- to 59-year age group. This resulted from the fact that, up to this age group, the total number of hip fractures was higher in males than in females. The statistics used for our study allow no assumptions on the conditions bringing about the fractures. Yet a substantial proportion of the fracture excess in males may result from risky behaviour not from osteopenia or osteoporosis. For these reasons, the excess of OHF in young males should be considered critically.
OHF led to a loss of 66,495 QALYs where about half of the QALY loss resulted from limited quality of life as a consequence of the fracture. Mortality and health status requiring long-term nursing care caused the remaining QALY loss, although relatively few persons were affected by mortality, when compared with the number of fractures. We considered future QALY losses beyond the initial year for nursing care and mortality. Additionally, for mortality, we calculated the entire QALY loss based on age- and gender-specific mean EQ-5D index scores.
OHF resulted in 2,736 million Euros direct costs, of which more than half were costs for nursing care in 2002 and the following years. These results are similar to those of Häussler et al. [28]. Häussler et al. estimated direct costs of 3,321 million Euros for a total of 333,322 osteoporosis-attributable fractures, of which 99,973 were OHF. Assuming that the proportion of OHF-attributable costs corresponds to the proportion of OHF in all osteoporosis-attributable fractures, the OHF-attributable direct costs for Häusler et al. were about 996 million Euros. In addition to Häussler et al., we also determined future nursing care costs, non-medical direct costs and indirect costs. Looking only on cost categories comparable to Häusler et al., we estimated direct costs of 1,132 million Euros. The distribution of costs among individual cost sectors determined in our study was also similar to the results of Häussler et al. Indirect costs were 262 million Euros, about 10% of the total costs to society. This relatively small value resulted from the fact that OHF occurred above all in more advanced age groups where, aside from negligible unpaid work, no productivity resulted.
Projecting the cases of osteoporosis-attributable hip fractures to the years 2020 and 2050 showed an overall increase of 44% and 128%, respectively. There was a decrease in cases for younger age groups in 2020 and even stronger in 2050. Yet, since only few cases occurred in younger age groups compared to older age groups, this decrease was almost meaningless for the total final result. Among the oldest age groups, the number of cases increased sharply, resulting from an over-proportional increase of the oldest old in the context of demographic change, combined with the highest prevalence rates of osteopenia and osteoporosis in these age groups. We found a considerably stronger relative increase for males than for females. The present number of males older than 75 years is skewed to a lower value as a result of the Second World War. This leads to an over-proportionally strong increase of males in theses age groups and subsequently male mortality, YPLL, QALYs and costs compared with females for the years 2020 and 2050. Compared to OHF cases, mortality and nursing care—appearing primarily in old age—increased over-proportionally, whereas rehabilitation and early retirement—appearing primarily in younger age—increased under-proportionally or even decreased.
Projecting corresponding costs showed similar results. In total, the costs increased slightly stronger than the number of cases, but differentiating according to direct and indirect costs showed clear differences. Whilst direct costs increased over-proportionally compared to the number of cases, indirect costs increased under-proportionally, whereas indirect cost from paid work even decreased to 2050.
Current international studies projecting osteoporosis-attributable cases and costs onto future years [4, 29, 30] came to differing results. Whilst the values of Burge et al. [29], Schwenkglenks et al. [31] and Sanders et al. [4] came relatively close to the values we determined, the results of Borgström et al. [30] were considerably below the cost increase we determined up to 2050. But these comparisons must be handled with care, since differing population mixtures and differing demographic prognoses limit international comparability.
Our results contain various uncertainties. First of all, relative risks are tainted with uncertainty, and in this study, this applies especially to the danger of overestimating the OHF. And so, a 50% increase of the relative risk ratio only leads to a narrow increase of examined parameters between 7.3% and 25.0%, whilst a 50% reduction of the relative risk reduces the examined parameters by 50.6% to 68.3%. This difference resulted from the fact that very high OAF were already present in higher age groups due to the high prevalence of osteoporosis and osteopenia in these groups. Based on these high initial values, the OAF itself could only be narrowly increased by a 50% increase of the BMD-dependent risks, whilst they could decrease strongly from a 50% reduction. The highest change of the OAF from an increase of the relative risk was, as expected, in younger age groups where the prevalence of osteopenia and osteoporosis was relatively small. Compared with the other parameters, this caused a relatively strong reaction of indirect costs to the increase of the relative risk. If the analysis were limited to persons 55 years and older, a strong reaction would also occur above all in indirect costs, since indirect costs emerge primarily in younger age groups. However, the other results had only little reaction to this variation.
The valuation of unpaid work had a strong influence on indirect costs. This resulted from the fact that three-fourths of the indirect costs came from unpaid work. Variations in the discount rate only resulted in narrow changes of costs, since discounting has an effect if costs lie far in the future, meaning they originate in young years. This was present in indirect costs above all, and they reacted as expected in a stronger way to variations of the discount rate than direct costs did. With direct costs, only future nursing care costs were discounted that initially appeared after 60 years of age and only contributed to a proportion of the direct costs. The reaction of direct costs to changes in the discount rate was correspondingly smaller than the reaction of indirect costs. Aside from these uncertainties, one can critically observe that various costs, such as outpatient treatment and non-medical costs, were taken from highly aggregated data.
Conclusion
OHF create a relevant health and economic impact on German society that can strongly increase in the future. With this background, osteoporosis and prevention of falls should receive more attention in research and in practical application in a long-term strategic perspective.
References
Cooper C (1999) Epidemiology of osteoporosis. Osteoporos Int 9(Suppl 2):S2–S8
WHO Scientific Group on the Prevention and Management of Osteoporosis (2003) Prevention and management of osteoporosis: report of a WHO scientific group. World Health Organization, Geneva
Statistisches Bundesamt (2006) Bevölkerung Deutschlands bis 2050. Ergebnisse der 11. koordinierten Bevölkerungsvorausberechnung [Population in Germany up to the year 2050. Results of the 11th coordinated projection of population]. Statistisches Bundesamt, Wiesbaden
Sanders KM, Nicholson GC, Ugoni AM, Pasco JA, Seeman E, Kotowicz MA (1999) Health burden of hip and other fractures in Australia beyond 2000. Projections based on the Geelong Osteoporosis Study. Med J Aust 170:467–470
Kleinbaum DG, Kupper LL, Morgenstern H (1982) Epidemiologic research, principles and quantitative methods. Van Nostrand Reinold, New York
Wildner M (2000) Osteoporose. Dtsch Med Wochenschr 126:A1170–A1172
De Laet CE, Van Hout BA, Burger H, Weel AE, Hofman A, Pols HA (1998) Hip fracture prediction in elderly men and women: validation in the Rotterdam study. J Bone Miner Res 13:1587–1593
Statistisches Bundesamt (2004) Fachserie 12 Reihe 4, Todesursachen in Deutschland 2002 [Causes of death in Germany 2002, series 12(4)]. Statistisches Bundesamt, Wiesbaden
Statistisches Bundesamt (2004) Statistisches Jahrbuch 2004 [Statistical yearbook 2004]. Statistisches Bundesamt, Wiesbaden
Statistisches Bundesamt (2002) Tiefgegliederte Diagnosedaten der Krankenhauspatientinnen und -patienten 2002 [Deep stratified diagnosis data from female and male inpatients 2002]. Statistisches Bundesamt, Wiesbaden
Statistisches Bundesamt (2005) Fachserie 12 Reihe 6.3, Kostennachweis der Krankenäuser 2002 [Hospital cost documentation 2002, series 12(6.3)]. Statistisches Bundesamt, Wiesbaden
Statistisches Bundesamt (2006) Fachserie 12, Reihe 6.2.2, Diagnosedaten der Rehabilitationspatienten 2004 [Diagnoses of patients in rehabilitation units 2004]. Statistisches Bundesamt, Wiesbaden
Statistisches Bundesamt (2002) Krankheitskostenrechnung [Calculation of costs of illness]. Accessed 26 March 2005. www.gbe-bund.de
Osnes EK, Lofthus CM, Meyer HE et al (2004) Consequences of hip fracture on activities of daily life and residential needs. Osteoporos Int 15:567–574
Statistisches Bundesamt (2005) Bericht: Pflegestatistik 2003—Pflege im Rahmen der Pflegeversicherung—Deutschlandergebnisse [Statistics on care 2003—care in the context of the care insurance—results for Germany]. Statistisches Bundesamt, Bonn
Statistisches Bundesamt (2004) Gesundheit, Ausgaben 2002 [Health, expenditures 2002]. Statistisches Bundesamt, Wiesbaden
Statistisches Bundesamt (2004) Fachserie 16 Heft 1, Löhne und Gehälter, Gehalts- und Lohnstrukturerhebung 2001 [Wages and salaries, survey about wages and salaries 2001, Series 16(1)]. Statistisches Bundesamt, Wiesbaden
Statistisches Bundesamt (2003) Löhne und Gehälter, Arbeitskostenerhebung, Ergebnisse der Arbeitskostenerhebung 2000 für Deutschland [Wages and salaries, survey about labour costs, results of the survey about labour costs for Germany in 2000]. Statistisches Bundesamt, Wiesbaden
Statistisches Bundesamt (2003) Statistisches Jahrbuch 2003 [Statistical yearbook 2003]. Statistisches Bundesamt, Wiesbaden
Statistisches Bundesamt (2004) Forum der Bundesstatistik Band 43. Alltag in Deutschland, Analysen zur Zeitverwendung. [Forum of federal statistics series 43, everyday life in Germany, analysis of time use]. Statistisches Bundesamt, Wiesbaden
BKK Bundesverband (2003) Gesundheit und Arbeitswelt, BKK Gesundheitsreport 2003 [Health and work environment, BKK health report 2003]. BKK Bundesverband, Essen
Verband deutscher Rentenversicherungsträger VDR (2002) Rentenzugang des Jahres 2002, Band 145. [Statistics about new pensions in 2002, volume 145]. VDR, Frankfurt/Main
Brazier JE, Green C, Kanis JA (2002) A systematic review of health state utility values for osteoporosis-related conditions. Osteoporos Int 13:768–776
Hiligsmann M, Ethgen O, Richy F, Reginster JY (2008) Utility values associated with osteoporotic fracture: a systematic review of the literature. Calcif Tissue Int 82:288–292
Dolan P (1997) Modeling valuations for EuroQol health states. Med Care 35:1095–1108
König HH, Bernert S, Angermeyer MC (2005) Health Status of the German population: results of a representative survey using the EuroQol questionnaire. Gesundheitswesen 67:173–182
Johnell O, Kanis JA, Oden A et al (2005) Predictive value of BMD for hip and other fractures. J Bone Miner Res 20:1185–1194
Häussler B, Gothe H, Gol D, Glaeske G, Pientka L, Felsenberg D (2007) Epidemiology, treatment and costs of osteoporosis in Germany—the BoneEVA Study. Osteoporos Int 18:77–84
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res 22:465–475
Borgström F, Sobocki P, Strom O, Jonsson B (2007) The societal burden of osteoporosis in Sweden. Bone 40:1602–1609
Schwenkglenks M, Lippuner K, Hauselmann HJ, Szucs TD (2005) A model of osteoporosis impact in Switzerland 2000–2020. Osteoporos Int 16:659–671
Acknowledgement
We are most grateful to Claus König, M.Sc. for providing mathematical advice.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Alexander Konnopka and Nadine Jerusel were equally contributing to this manuscript.
Appendix
Appendix
Relative risk of HF due to osteopenia and osteoporosis
For a BMD-dependent, variable we used—according to De Laet et al. [7]—a value of 2.6 per standard deviation and we used the T score as the basis for the standard deviation. Osteopenia and Osteoporosis are defined by intervals of bone density in a standard normal distribution. In order to consider the probability that a person has a certain bone density, a 2.6 T score was weighted with the density function of a standard normal distribution to account for the probability of having a certain T score. The relative risks for osteopenia (RR 1 ) and osteoporosis (RR 2 ) were calculated as follows:
Mortality (M OHF )
Age- and gender-specific multiplication of the OAF with the HF-associated deaths M HF :
Years of potential life lost
Determination of gender-specific probabilities p l of reaching future ages A + n (n = 1, 2, 3… 100 − A) of maximally up to 100 years for each age group A. For each age group A, addition of the p l of all future years of life and multiplication with M OHF :
Quality-adjusted life years lost
Fracture associated QALY loss (QALY1)
Age- and gender-specific multiplication of the OAF with the inpatient HF cases HF IC and subtraction of M OHF . Then multiplication with post-fractural QALY loss and correction by p l for the second post-fractural year:
QALY loss among people who need nursing care (QALY2)
Age- and gender-specific determination of OHF-attributable nursing care cases from inpatient cases HF IC with the help of:
-
Probability p c of outpatient or inpatient nursing care needs according to HF,
-
Probability p cp that a person needed no nursing care before HF,
-
Probability p cf of a person in age A without HF also needing no nursing care in the future,
-
Probability p l of a person in age A experiencing future life years A + n (n = 2, 3, 4… 100 − A).
Multiplication of the care cases with QALY loss whilst considering future years:
Mortality-attributable QALY loss (QALY3)
Calculated as with YPLL, but weighting p l with age- and gender-specific EQ-5D index values EQ:
Resource utilisation and direct costs
Inpatient medical treatment and rehabilitation (DC1)
Age- and gender-specific multiplication of the OAF with the HF-associated hospital care days HF ID and rehabilitation days HF RD and the average costs per care day C 1ID and C 1RD :
Outpatient treatment and non-medical costs for health protection, rescue services, administration and “other services” (DC2)
Determination of the portion of inpatient OHF cases in inpatient cases of S70–S79 (ICD-10: injuries of hip and thigh) and application to recorded costs C S70–S79 :
Nursing care (DC3)
Determination of OHF-attributable nursing care cases analogous to QALY 2 . Multiplication of the current and future OHF-attributable nursing care cases by the costs for inpatient and outpatient nursing care C 3. Consideration of the first year at 50% and discounting of costs of future n years by r = 5% per year:
Non-medical costs for research, education and investments (DC4)
Determination of the gender-specific portion of all OHF-attributable medical costs of the year 2002 from the entire medical costs of the year 2002 C t and application to the costs for research, education and investments C 4:
Indirect costs
Yearly productivity (P)
Age- and gender-specific multiplication of the sum of yearly average gross salaries GS and employer participation in social security S by the probability of a paid activity p w. Addition of the product of the yearly unpaid work hours T and net salary per hour of a household helper:

Sickness absence (IC1)
Age- and gender-specific multiplication of the OAF by the product of inpatient HF cases HF IC and average HF-associated inability to work I W as well as HF-associated rehabilitation days HF RD followed by evaluation with P:
Early retirement (IC2)
Age- and gender-specific multiplication of the OAF by the early retirements ER and the severity level of the early retirement SC. Consideration of the first year at 50% and evaluation with P. Starting at 70 years old, reduction of unpaid productivity by 10% every 5 years (not shown in formula) and discounting future n years by r = 5%:
Mortality (IC3)
Determination as in early retirement, but based on OHF-attributable deaths M OHF :
Rights and permissions
About this article
Cite this article
Konnopka, A., Jerusel, N. & König, HH. The health and economic consequences of osteopenia- and osteoporosis-attributable hip fractures in Germany: estimation for 2002 and projection until 2050. Osteoporos Int 20, 1117–1129 (2009). https://doi.org/10.1007/s00198-008-0781-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-008-0781-1