Abstract
Summary
Osteoporosis is a well acknowledged complication of spinal cord injury. We report that motor complete spinal cord injury and post-injury alcohol consumption are risk factors for hospitalization for fracture treatment. The clinical assessment did not include osteoporosis diagnosis and treatment considerations, indicating a need for improved clinical protocols.
Introduction
Treatment of osteoporotic long bone fractures often results in lengthy hospitalizations for individuals with spinal cord injury. Clinical features and factors that contribute to hospitalization risk have not previously been described.
Methods
Three hundred and fifteen veterans ≥ 1 year after spinal cord injury completed a health questionnaire and underwent clinical exam at study entry. Multivariate Cox regression accounting for repeated events was used to assess longitudinal predictors of fracture-related hospitalizations in Veterans Affairs Medical Centers 1996–2003.
Results
One thousand four hundred and eighty-seven hospital admissions occurred among 315 participants, and 39 hospitalizations (2.6%) were for fracture treatment. Median length of stay was 35 days. Fracture-related complications occurred in 53%. Independent risk factors for admission were motor complete versus motor incomplete spinal cord injury (hazard ratio = 3.73, 95% CI = 1.46–10.50). There was a significant linear trend in risk with greater alcohol consumption after injury. Record review indicated that evaluation for osteoporosis was not obtained during these admissions.
Conclusions
Assessed prospectively, hospitalization in Veterans Affairs Medical Centers for low-impact fractures is more common in motor complete spinal cord injury and is associated with greater alcohol use after injury. Osteoporosis diagnosis and treatment considerations were not part of a clinical assessment, indicating the need for improved protocols that might prevent low-impact fractures and related admissions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinal cord injury (SCI) is associated with severe osteoporosis increasing the risk of low-impact fractures (i.e., those that occur in the absence of trauma). The precise mechanisms leading to this extreme bone loss are poorly understood; however, several characteristics distinguish SCI-induced osteoporosis from both postmenopausal and senile osteoporosis affecting neurologically intact elders. Many factors are known to increase the risk of osteoporotic fractures in the general population, including previous fragility fractures, premature menopause, a family history of hip fracture, age, use of glucocorticoids, age, hormonal status, and nutritional status [1]. But all individuals with SCI, including otherwise healthy young men and women, are at risk for immediate, rapid bone loss [2–4]. While osteoporotic fractures lead to increased mortality in the elderly [5–7], little is known about the impact of these fractures on the health of individuals with SCI. Specifically, risk factors for osteoporotic fractures or fracture-related hospitalization and a description of treatment and complications have not been described.
We have been assessing the health of a cohort of individuals with chronic SCI since 1994 and have collected detailed information on personal characteristics and comorbidities [8]. In this study, we assess whether various sociodemographic and health-related factors assessed at baseline prospectively predict hospitalization related to low-impact fractures at Veterans Affairs Medical Centers (VA) and review fracture-related treatment and complications.
Methods
Subjects
Between 01 October 1994 and 31 December 2002, there were 328 veterans recruited as part of the VA Boston SCI Cohort Study, an epidemiological study designed to prospectively assess health in chronic SCI patients. Recruitment was from veterans receiving care from the VA Boston SCI Service. Details of recruitment methodology have been presented previously, but briefly, subjects were eligible if they were one or more years after SCI and were ineligible if they had other neurological conditions, a tracheostomy, required mechanical ventilation, or had recovered from their injury [9]. Subjects completed a standardized respiratory health questionnaire (ATS DLD-78) [10] with additional questions regarding personal habits and medical history, and underwent a neurological examination and an assessment of weight and measured length. Informed consent was obtained, and this study was approved by our institutional review boards.
Spinal cord injury classification
Motor level and completeness of injury were assessed by physical exam. Level of injury was classified according to strength preservation in key muscle groups in the upper and lower extremity and reported regionally as tetraplegia or paraplegia. Injury completeness was reported according to the American Spinal Injury Association (ASIA) guidelines [10, 11]. Participants were assigned as motor complete (equivalent to ASIA motor score of A or B, i.e., no motor function below the neurological level of injury), C (motor incomplete, motor function preserved below the neurological level and more than half the key muscles below the neurological level are not strong enough to overcome gravity), or D (motor incomplete, preservation of motor function below the neurological level and more than half the key muscles below the neurological level are strong enough to overcome gravity).
Hospitalization data
We assessed hospitalization for acute care using VA electronic databases from 10/1/1996 through 12/31/2003 to allow at least one year of follow up. It was not possible to include hospitalization data before 10/1996 due to non-uniform reporting standards. We extracted hospitalization data from the VA National Patient Care Dataset located in Austin, Texas. Each medical record includes an admitting diagnosis (DXPRIME), up to nine secondary diagnoses, and a primary diagnosis (DXLSF) that is the condition responsible for the length of hospital stay. Diagnosis codes follow the clinically modified ninth edition of the International Classification of Diseases (ICD-9-CM).
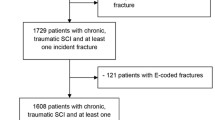
Starting 01 October 1996 or at entry for subjects recruited after that date, the number of days to hospital admission for any cause, and from discharge to the next hospitalization was calculated. Age and injury duration were recalculated following each admission. Hospitalizations related to a fracture were defined based on DXPRIME, DXLSF, or secondary diagnoses coded as 733–733.1 (osteoporotic or pathogenic fracture) or 810–829 (fractures of the upper and lower limbs). There were 44 hospitalizations, 35 based on both DXPRIME and DXLSF, and nine based on secondary diagnoses. As we sought to study fractures consistent with SCI-induced osteoporosis, we defined “low-impact fractures” as those occurring spontaneously or from a fall no greater than standing height as defined by Simonelli and coworkers [10, 12]. Based on medical record review, there were 30 subjects with 39 admissions that met this definition and were associated with a fracture below the SCI neurological level. We excluded two admissions in the same individual that related to chronic non-healing fractures that occurred at the time of the initial SCI and two admissions in different individuals that were unrelated to fracture treatment. Admission and discharge records were reviewed for evidence of evaluation or treatment of osteoporosis.
Variable definition
We considered sociodemographic factors, comorbid illnesses, and various health behaviors reported at study entry (Table 1). Length was measured in 78% of subjects. If measurement was declined or there were joint contractures that precluded accurate assessment, stature was self-reported. Weight was measured in 90%, self-reported in 8%, and weight from a recent clinic visit used in 2%. Body mass index (BMI) was classified as underweight (<18.5 kg/m2) normal weight (BMI ≥ 18.5 - < 25 kg/m2), overweight (BMI ≥ 25 - <30 kg/m2), and obese (BMI ≥ 30 kg/m2). Smokers were defined as smoking 20 or more packs of cigarettes or using 12 ounces of tobacco or more in a lifetime, or smoking one or more cigarettes per day for at least one year. Current smokers reported cigarette use within one month of testing. Lifetime alcohol consumption and alcohol consumption after SCI were calculated based on report of average daily, weekly, or monthly quantity and frequency of alcohol consumption and duration of alcohol use before and after injury. Each glass of wine (4 ounce = 10.8 g), beer (12 ounce = 13.2 g), and shot of liquor (1.5 ounce = 15.1 g) was converted to grams of alcohol [13, 14]. Subjects were asked to report physician-diagnosed hypertension, diabetes, asthma, emphysema and chronic bronchitis [defined as chronic obstructive pulmonary disease (COPD)], and pneumonia since hospital discharge after initial SCI. Heart disease was defined as receiving treatment for “heart trouble” in the 10 years prior to study entry.
Statistical analysis
Models using Cox’s proportional hazards approach with a robust sandwich estimator to adjust for repeated outcomes [TPHREG procedure in SAS software version 9.1 (SAS Inc, Cary, NC)] were used to assess predictors of fracture hospitalization using days to hospitalization as the outcome. Secular trends were tested by considering calendar year in a time dependent manner. The proportional hazards assumption was confirmed by examining the interaction between covariates and the natural logarithm of time to hospitalization.
Results
Participant characteristics
Of the 328 veterans assessed, three died before 10/1/1996, eight did not undergo neurological exam or had recovered from injury, and two had missing information, leaving 315 subjects for analysis. Among these 315 participants, the total time at risk for a fracture-related hospitalization was 1,658 person-years, an average of 5.26 person-years per participant. There were 1,487 all-cause hospitalizations for an overall hospitalization rate of 0.90/person-year, and the rate of fracture-related admissions was 0.02/person-year. The median (q1, q3) length of stay was 35 [20, 59] days for fracture admissions and five (2, 14) days for non-fracture admissions. Of five subjects with repeat fracture-related admissions, one was re-admitted for treatment of the same fracture, three were re-admitted for a new fracture, and one had six admissions related to four new fractures and had two re-admissions for prior fractures. Three individuals fractured multiple bones during the same event (one with bilateral first metatarsal fractures, one with an ankle and great toe fractures, and one with humerus, femur, and tibia/fibula fractures). Both individuals re-admitted for ongoing treatment of a prior fracture were discharged to a second facility for convalescence. Each had lived at home prior to the admission.
Fracture characteristics
The most common fracture requiring hospitalization was a tibia/fibula fracture (47.5%), followed by the distal femoral metaphysis (20%) and then the proximal femur (15%). Humerus (5%), metatarsal (5%), and phalanx (7.5%) fractures were less common. In 20% of admissions, the cause of fracture was unknown or not stated in the discharge summary or admission notes. Fall from a wheelchair was the most common cause (51%), followed by transfers (twisting or catching a lower extremity, 14%), and catching a lower extremity on a doorframe while operating a wheelchair (6%). One individual twisted a leg while boating and fractured a femur. Fractures were usually (87%) treated with bed rest alone or a combination of bed rest with extension bracing. Surgery was performed in three cases (9%), all of which were proximal femur/hip fractures. No specific treatment was prescribed in two cases. Medical complications occurred frequently with 53% of the fracture events resulting in 21 documented complications. Fracture non-union/delayed healing and pressure ulcers from bracing and/or bed rest were the most common, each accounting for 25% of the reported medical complications. Other complications included increased muscle spasms, pain, autonomic dysreflexia, and heterotopic ossification at the fracture site. No individual with a fracture-related admission underwent an evaluation for osteoporosis.
Univariate predictors of fracture admission
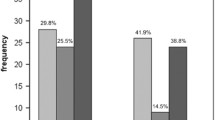
Age, education level, BMI category, smoking history (current, former, never; pack-years), hypertension, heart disease, diabetes, asthma, and COPD were not significant predictors of fracture-related hospitalization (p = 0.16 to 0.85), and there were no significant secular trends (Table 2). Hospitalization risk increased significantly with injury duration [hazard ratio (HR): 3% increase/year, 95% CI = 1%-4%]. Those with a motor complete injury had an increased risk (HR: 3.99; 95% CI = 1.54–10.35) of being hospitalized for a fracture compared to ASIA C or ASIA D injury, and there was no significant difference in the hazard ratio between motor complete tetraplegia and paraplegia for fracture admission risk (p = 0.44). Lifetime alcohol consumption was not a significant predictor of fracture hospitalization, but admission risk increased significantly with greater alcohol consumption after injury (p = 0.03 for linear trend across quartiles) with approximately a threefold increased risk in the highest quartile compared to the lowest quartile.
Multivariate predictors of fracture admission
After adjusting for neurological completeness of injury, injury duration (p = 0.11) was no longer a significant predictor (Table 3). Only neurological completeness of injury (3.73; 95% CI = 1.46–10.50) and greater alcohol consumption after injury (p = 0.04 for linear trend across quartiles) remained significant predictors of fracture-related hospitalization (Table 4). The median alcohol consumption in the quartile with the greatest consumption following SCI was 498 kg-yr, approximately equivalent to 5½ beers, 6¾ wine glasses, or five shots of liquor per day for 20 years (HR: 3.25; 95% CI = 1.54–10.35 compared to the lowest quartile).
Discussion
Our study is the first to prospectively assess risk factors for hospitalization for low-impact fractures in chronic SCI, and we describe a significant relationship between injury completeness and greater alcohol use after injury. Other groups have examined risk factors for sublesional osteoporosis following spinal cord injury, however only injury completeness has been shown to predict the degree of bone loss or fracture rate. Garland et al. reported motor complete injury to increase both knee osteoporosis and lower extremity fracture rates when compared to motor incomplete injury [4, 15]. Our findings are in agreement with this and suggest that individuals with motor complete injury are at greatest risk for fracture hospitalization. We also report increased alcohol consumption after SCI may exacerbate sublesional bone loss. Although the number of fractures that occurred as a result of alcohol intoxication is unknown, it is possible that alcohol-related accidents related to wheelchair use and transfer contributed. The relationship between alcohol consumption and osteoporosis in the general population has been inconsistent, although in general men with a history of alcohol abuse have been found to have lower bone mineral density, and the relative contribution of poor nutrition in these cases is uncertain [16–22]. In contrast to the general population where greater age is a risk factor for osteoporosis, age was not a predictor of fracture hospitalization. Obesity, known to be osteoprotective in the able-bodied [23, 24], did not protect from fracture hospitalization in this study. We also found no relationship between history of comorbid illnesses and fracture hospitalization. Although injury duration was a significant univariate predictor of fracture hospitalization, when SCI completeness was accounted for it was no longer significant. However, the point estimate for injury duration remained positive (HR = 1.02; 95% CI = 1.00–1.04). As sublesional bone loss increases with time following an injury [25–27], it is possible that the relatively small number of cases precluded our ability to assess both injury duration and SCI completeness in a regression model.
The median length of stay was sevenfold greater for fracture admissions than for non-fracture admissions, a finding that reflects the need to immobilize the affected limb until adequate healing occurs. Individuals also required increased levels of assistance for transfers and self-care during immobilization of a fractured limb. Only three subjects underwent surgical fracture stabilization during their admission (length of stay 12 to 36 days), so it was not possible to compare the effects of surgery on length of stay. When re-admissions for a prior fracture occurred, discharge to a second facility was required. Though this occurred in only two cases, it may be that prior fracture is a risk factor for long-term care.
Although admission for osteoporotic fractures accounted for only 2.6% of the admissions, these hospitalizations resulted in longer lengths of stay than other admissions, were characterized by frequent medical complications, and in some cases, resulted in discharge to a second facility instead of home because additional care was required. Prevention of fractures would therefore decrease health care costs and promote independence in this population. The most common cause of fracture was falls, which may be difficult to prevent. However, based on record review, 20% of the fractures resulting in hospitalization were due to transfer and wheelchair ambulation technique. It may be possible to reduce fracture risk by improving counseling and educating patients regarding limb protection during various self-care activities and reinforce the importance of adequate doorway width for wheelchair clearance. In some cases, home modification may be required to achieve the recommended minimum of 81.3–86.4 cm to accommodate the entry of manual and motorized wheelchairs [28].
Surprisingly, osteoporosis diagnosis, prevention, and management were not included in the treatment plan of any of the individuals hospitalized for fractures. No one was taking osteoporosis medications, such as anti-resorptives (bisphosphonates) or calcium/vitamin D, prior to admission. Moreover, no one left the hospital with a prescription for osteoporotic medications, and osteoporosis was not added to anyone’s problem list on discharge. One individual was placed on alendronate after admission, but this was discontinued by the consulted endocrinology team who stated that alendronate has not been shown to protect bone mineral density in the extremities. There is evidence to suggest that bisphosphonates, including alendronate, decrease bone loss both acutely and during the chronic phases of SCI [29–32]; however, bisphosphonate treatment is not currently the standard of care since it has not been shown to decrease fracture rates in SCI. Additional research is needed to establish the efficacy of anti-resorption medications and to explore the potential benefits of anabolic bone agents in bone loss following spinal cord injury. Fracture prevention is an important therapeutic goal in SCI medicine as 54% of the fractures resulted in a secondary complication. The omission of osteoporosis in the discharge diagnoses suggests a need for improved treatment practice standards in SCI. This clinical void may be due to a lack of adequate therapeutic options for treating bone loss following SCI and an absence of appropriate dual energy x-ray absorptiometry (DXA) scanning protocols tailored to this population.
The findings of the current study suggest that injury completeness and alcohol consumption are risk factors for fracture hospitalization in a VA-based cohort of individuals with chronic SCI. These findings should be considered within the context of the study limitations, including few female participants and a relatively small sample size. It is likely that the true incidence of fracture-related admissions is underestimated since these patients may have been hospitalized elsewhere for treatment or possibly treated with bed rest at home. Although lifetime and post-SCI alcohol consumption was estimated by self-report, information obtained using this method has been shown to be valid and without systematic bias [14, 33]. We also analyzed these data within broad categories, comparing risk across quartiles to minimize misclassification. The biologic mechanism whereby complete SCI is a risk factor for fracture-related admissions is not known but is hypothesized to be related to neurogenic control of bone formation and resorption [34, 35]. It is also possible the completeness of injury is a surrogate for other risk factors that were not measured in this study, such as vitamin D deficiency [36].
Conclusions
Motor complete SCI, both paraplegia and tetraplegia, and cumulative alcohol consumption post-injury were significant risk factors for fracture hospitalization. Clinicians involved in the care of individuals with SCI should be aware of relatively long hospitalizations and related complications associated with these fractures. These findings suggest that future studies should address prevention and treatment of bone loss in the motor complete subpopulation. Additionally, studies aimed at a greater understanding of the biologic mechanisms of SCI-induced bone loss are needed to develop therapies to reduce fracture rates, secondary medical complications, and healthcare-related costs associated with fracture-related hospitalization.
References
Kanis JA (2002) Diagnosis of osteoporosis and assessment of fracture risk. Lancet 359(9321):1929–1936 June 1
Dauty M, Perrouin VB, Maugars Y, Dubois C, Mathe JF (2000) Supralesional anmesional bone mineral density in spinal cord-injured patients. Bone 27(2):305–309 August
Frey-Rindova P, de Bruin ED, Stussi E, Dambacher MA, Dietz V (2000) Bone mineral density in upper and lower extremities during 12 months after spinal cord injury measured by peripheral quantitative computed tomography. Spinal Cord 38(1):26–32 January
Garland DE, Stewart CA, Adkins RH, Hu SS, Rosen C, Liotta FJ, Weinstein DA (1992) Osteoporosis after spinal cord injury. J Orthop Res 10(3):371–378 May
Barrett-Connor E (1995) The economic and human costs of osteoporotic fracture. Am J Med 98(2A):3S–8S February 27
Bass E, French DD, Bradham DD, Rubenstein LZ (2007) Risk-adjusted mortality rates of elderly veterans with hip fractures. Ann Epidemiol 17(7):514–519 July
Chrischilles E, Shireman T, Wallace R (1994) Costs and health effects of osteoporotic fractures. Bone 15(4):377–386 July
Jain NB, Brown R, Tun CG, Gagnon D, Garshick E (2006) Determinants of forced expiratory volume in 1 second (FEV1), forced vital capacity (FVC), and FEV1/FVC in chronic spinal cord injury. Arch Phys Med Rehabil 87(10):1327–1333 October
Garshick E, Kelley A, Cohen SA, Garrison A, Tun CG, Gagnon D, Brown R (2005) A prospective assessment of mortality in chronic spinal cord injury. Spinal Cord 43(7):408–416 July
Ferris BG (1978) Epidemiology Standardization Project (American Thoracic Society). Am Rev Respir Dis 118(6 Pt 2):1–120 December
Marino RJ, Barros T, Biering-Sorensen F, Burns SP, Donovan WH, Graves DE, Haak M, Hudson LM, Priebe MM (2003) International standards for neurological classification of spinal cord injury. J Spinal Cord Med 26(Suppl 1):S50–S56
Simonelli C, Chen YT, Morancey J, Lewis AF, Abbott TA (2003) Evaluation and management of osteoporosis following hospitalization for low-impact fracture. J Gen Intern Med 18(1):17–22 January
Dawson DA (2003) Methodological issues in measuring alcohol use. Alcohol Res Health 27(1):18–29
Garshick E, Segal MR, Worobec TG, Salekin CM, Miller MJ (1989) Alcohol consumption and chronic obstructive pulmonary disease. Am Rev Respir Dis 140(2):373–378 August
Garland DE, Adkins RH, Kushwaha V, Stewart C (2004) Risk factors for osteoporosis at the knee in the spinal cord injury population. J Spinal Cord Med 27(3):202–206
Kogawa M, Wada S (2005) Osteoporosis and alcohol intake. Clin Calcium 15(1):102–105 January
Mukamal KJ, Robbins JA, Cauley JA, Kern LM, Siscovick DS (2007) Alcohol consumption, bone density, and hip fracture among older adults: the cardiovascular health study. Osteoporos Int 18(5):593–602 May
Newcombe RG, Clements DG, Evans WD (1993) Alcohol and bone density. BMJ 307(6899):323 July 31
Sampson HW, Chaffin C, Lange J, DeFee B (1997) Alcohol consumption by young actively growing rats: a histomorphometric study of cancellous bone. Alcohol Clin Exp Res 21(2):352–359 April
Saville PD, Lieber CS (1965) Effect of alcohol on growth, bone density and muscle magnesium in the rat. J Nutr 87(4):477–484 December
Schapira D (1990) Alcohol abuse and osteoporosis. Semin Arthritis Rheum 19(6):371–376 June
Wosje KS, Kalkwarf HJ (2007) Bone density in relation to alcohol intake among men and women in the United States. Osteoporos Int 18(3):391–400 March
Ducy P, Amling M, Takeda S, Priemel M, Schilling AF, Beil FT, Shen J, Vinson C, Rueger JM, Karsenty G (2000) Leptin inhibits bone formation through a hypothalamic relay: a central control of bone mass. Cell 100(2):197–207 January 21
Karsenty G (2006) Convergence between bone and energy homeostases: leptin regulation of bone mass. Cell Metab 4(5):341–348 November
Bauman WA, Spungen AM, Wang J, Pierson RN Jr, Schwartz E (1999) Continuous loss of bone during chronic immobilization: a monozygotic twin study. Osteoporos Int 10(2):123–127
Eser P, Frotzler A, Zehnder Y, Schiessl H, Denoth J (2005) Assessment of anthropometric, systemic, and lifestyle factors influencing bone status in the legs of spinal cord injured individuals. Osteoporos Int 16(1):26–34 January
Zehnder Y, Luthi M, Michel D, Knecht H, Perrelet R, Neto I, Kraenzlin M, Zach G, Lippuner K (2004) Long-term changes in bone metabolism, bone mineral density, quantitative ultrasound parameters, and fracture incidence after spinal cord injury: a cross-sectional observational study in 100 paraplegic men. Osteoporos Int 15(3):180–189 March
Stiens SA, Kirshblum SC, Groah SL, McKinley WO, Gittler MS (2002) Spinal cord injury medicine. 4. Optimal participation in life after spinal cord injury: physical, psychosocial, and economic reintegration into the environment. Arch Phys Med Rehabil 83(3 Suppl 1):S72–S78 March
Gilchrist NL, Frampton CM, Acland RH, Nicholls MG, March RL, Maguire P, Heard A, Reilly P, Marshall K (2007) Alendronate prevents bone loss in patients with acute spinal cord injury: a randomized, double-blind, placebo-controlled study. J Clin Endocrinol Metab 92(4):1385–1390 April
Mechanick JI, Liu K, Nierman DM, Stein A (2006) Effect of a convenient single 90-mg pamidronate dose on biochemical markers of bone metabolism in patients with acute spinal cord injury. J Spinal Cord Med 29(4):406–412
Shapiro J, Smith B, Beck T, Ballard P, Dapthary M, BrintzenhofeSzoc K, Caminis J (2007) Treatment with zoledronic acid ameliorates negative geometric changes in the proximal femur following acute spinal cord injury. Calcif Tissue Int 80(5):316–322 May
Zehnder Y, Risi S, Michel D, Knecht H, Perrelet R, Kraenzlin M, Zach GA, Lippuner K (2004) Prevention of bone loss in paraplegics over 2 years with alendronate. J Bone Miner Res 19(7):1067–1074 July
Del Boca FK, Darkes J (2003) The validity of self-reports of alcohol consumption: state of the science and challenges for research. Addiction 98(Suppl 2):1–12 December
Morse L, Teng YD, Pham L, Newton K, Yu D, Liao WL, Kohler T, Muller R, Graves D, Stashenko P, Battaglino R (2008) Spinal cord injury causes rapid osteoclastic resorption and growth plate abnormalities in growing rats (SCI-induced bone loss in growing rats). Osteoporos Int 19(5):645–652 May
Morse LR, Nguyen HP, Jain N, Williams S, Tun CG, Battaglino RA, Stashenko P, Garshick E (2008) Age and motor score predict osteoprotegerin level in chronic spinal cord injury. J Musculoskelet Neuronal Interact 8(1):50–57 January
Bauman WA, Zhong YG, Schwartz E (1995) Vitamin D deficiency in veterans with chronic spinal cord injury. Metabolism 44(12):1612–1616 December
Acknowledgments
We wish to acknowledge Joda Alian for her kind assistance in manuscript editing and preparation.
Conflicts of interest
None.
Disclaimers
The project reported/outlined here was supported by the Office of Research and Development, Health Services R&D Service, Quality Enhancement Research Initiative RRP-07–312 and NIH/NICHD RO1 HD42141 (Dr. Garshick). Dr. Garshick is the Associate Chief of Pulmonary and Critical Care Medicine at VA Boston Healthcare System. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Morse, L.R., Battaglino, R.A., Stolzmann, K.L. et al. Osteoporotic fractures and hospitalization risk in chronic spinal cord injury. Osteoporos Int 20, 385–392 (2009). https://doi.org/10.1007/s00198-008-0671-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-008-0671-6