Abstract
Summary
In a child, bone mineral density (BMD) may differ from an age-expected normal value, not only because of the presence of disease, but also because of deviations of height or weight from population averages. Appropriate adjustment for body size deviations simplifies interpretation of BMD measurements.
Introduction
For children, a bone mineral density (BMD) measurement is normally expressed as a Z score. Interpretation is complicated when weight or height distinctly differ from age-matched children. We develop a procedure to allow for the influence of body size deviations upon measured BMD.
Methods
We examined the relation between body size deviation and spine, hip and whole body BMD deviation in 179 normal children (91 girls). Expressions were developed that allowed derivation of an expected BMD based on age, gender and body size deviation. The difference between measured and expected BMD was expressed as a HAW score (Height-, Age-, Weight-adjusted score).
Results
In a second independent sample of 26 normal children (14 girls), measured spine, total femur and whole body BMD all fell within the same single normal range after accounting for age, gender and body size deviations. When traditional Z scores and HAW scores were compared in 154 children, 17.5% showed differences of more than 1 unit and such differences were associated with height and weight deviations.
Conclusion
For almost 1 in 5 children, body size deviations influence BMD to an extent that could alter clinical management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
X-ray-based dual energy absorptiometry (DXA) is an accepted technique for the detection of abnormalities of bone mineral mass in children. Recent studies in a population of Canadian children presented normal values as a function of age for the DXA-measured variables of lumbar spine bone mineral areal density (BMD), proximal femur BMD and whole body BMD [1]. Such measurements allowed the development of a means for predicting expected-for-age values in boys and girls in order to assist in the interpretation of DXA measurements in children suspected to be suffering from disorders of bone metabolism. The 95% confidence limits for the sample of children were considered to define normal population ranges so that the extent of deviation for diagnostic measurements could be expressed in terms of the number of population standard deviations or as a Z score.
The clinical interpretation of a Z score originates from the fact that the 5-year fracture risk is about 7% for children when the spine BMD Z score is −1 [2]. The identification of fracture-prone children is also aided by accounting for independent risk factors such as age, body weight, breast-feeding history, fracture history, height, inhaled corticosteroids, menarcheal age, nutritional status and physical activity level [3–8]. In particular, during the period of rapid growth, bone strength may not increase rapidly enough to meet the demands of the mechanical burdens imposed [9].
It has been reported that errors in the interpretation of DXA measurements in children and adolescents can lead to over-diagnosis of osteoporosis [10]. When measurements are made in children whose body size is inappropriate for their age, the interpretation of Z scores is complicated. For example, it might be expected that a child who is small for his chronological age may have a measured BMD that is less than the expected-for-age BMD. In this case the Z score is likely to be negative, but bone strength may be adequate to sustain lower than average mechanical burdens imposed by a smaller body size.
Many attempts have been made to adjust BMD measurements in children to take into account the influences of body size [11–16]. Generally, an adjustment is made based on body weight or height. To some extent, body size is incorporated within expected-for-age values of BMD because age and size are inevitably correlated in children. In reality, the body size included in this way is the expected-for-age body size and does not account for height and weight deviations from normal patterns of growth. The accuracy of anticipated DXA bone and body composition variables based solely on age and gender is likely to be improved by incorporating the effect of body size deviations. The corollary to this is that if a measured DXA variable deviates from an expected-for-age value because of an unusual body size, the difference between the measured and predicted values (the BMD residual) will be a function of the deviation of body size from the size expected for the chronological age of a child. To explore this possibility, body size deviations were derived from the difference between measured height or weight and expected-for-age height or weight. Body size deviations were then compared to the magnitude of DXA residuals. The observed relations supported the concept that the accuracy of predicted values could be improved by accounting for body size deviations. The purpose of this paper is to describe the derivation of body size correction factors and to explore the merits of including such corrections in the interpretation of clinical DXA measurements in children and adolescents.
Materials and methods
Normal participants
Previously, we recruited a convenience sample of 179 normal children (91 girls and 88 boys) between the ages of 3 and 18 years for the purpose of establishing normal expected-for-age values in boys and girls [1]. Height and weight were measured for each child using standard clinical scales. Expected heights and weights for each child were taken as the 50th percentile value for a child of the same age according to the growth charts produced by the National Center for Chronic Disease Prevention and Health Promotion [17]. Height and weight deviations were calculated as the difference between the measured and expected values.
A second independent sample of 26 normal children (14 girls and 12 boys) was recruited locally in order to validate the predictive equations derived from the larger initial sample of children. The predictive equations were also applied retrospectively to patients who had undergone up to 14 serial DXA measurements in the past. Finally, the predictive equations were applied prospectively to 154 children (80 girls and 74 boys) referred for clinical DXA measurements. The children attended clinics at the Children’s Hospital, Hamilton Health Sciences. They were either new patients suspected to be suffering from diseases or conditions that were associated with bone mineral loss or were returning patients undergoing treatment for or follow-up of chronic diseases known to affect bone mineral status. The study was approved by the Research Ethics Board of Hamilton Health Sciences/McMaster University. In all cases, written informed consent was obtained from a parent or guardian of each child and, where appropriate, assent was obtained from the participants themselves.
DXA measurements
All measurements for the sample of 179 children were performed with Hologic Densitometers (either a QDR 4500A or a Discovery A). A between-machine comparison showed that the results of lumbar spine and proximal femur measurements were correlated strongly (r > 0.98) and that absolute inter-machine differences were small compared to population variances. All measurements for the smaller population of 26 children were performed using the Discovery A densitometer.
Each child had a lumbar spine (L1–L4), left proximal femur and a whole body scan. All DXA scans were reviewed for technical adequacy by a single experienced densitometrist. Expected-for-age values for each DXA variable were obtained using the predictive equations published previously [1].
Development of predictive equations incorporating height and weight deviations
The difference between an expected-for-age prediction and the measured value for a given DXA variable is the residual value. A positive residual value may be the consequence of excess body weight and, by the same token, a measured value may be less than expected because of a diminished body size. In both cases, a correlation should be apparent between residual DXA values and weight deviations. If such a correlation can be demonstrated, then accounting for weight and/or height deviations should improve the accuracy of prediction for DXA variables, and the chances of identifying true clinical abnormalities should rise.
To develop correction terms, the dependence of DXA residuals upon height and weight deviations was determined. Since weight deviations were expected to be more common and of greater relative magnitude than height deviations, the first step was to examine the relationship between residuals for a particular DXA variable and the corresponding weight deviations. The equation fitted to the data by linear regression will yield a correction to an expected-for-age value that will depend on the weight deviation for the subject of concern. Application of this correction to the original expected-for-age value will yield a second, intermediate predicted value based on age, gender and weight deviation so that a second residual can be generated. The dependence of the second residual value for each child upon height deviation can then be examined. Again, a linear regression line fitted to the data will yield a correction to the second predicted value that will be based upon height deviation. The final gender-specific predicted value for a given DXA variable will be based on age and modified by factors that account for weight and height deviations.
Application of predictive equations
The effect of including height and weight deviations was assessed initially by examining relationships between measurements and predictions. That is for boys and girls, the extent of agreement between measurement and prediction based on age was compared with the extent of agreement between measurement and prediction based on age and body size deviations. First, the comparisons were made in the same population of normal children used to derive the body size deviation correction procedure. To provide a more rigorous test, the extent of agreement between measured and predicted values was examined in a second, independent sample of normal children drawn from the same local population. In addition, the merit of basing expected values on gender and age alone or upon gender, age and body size deviations was examined using retrospective data from patients who were suffering from, or recovering from, acute lymphoblastic leukemia (ALL). They were selected to encompass various ages at first measurement and were followed for at least 3 years with lumbar spine measurements. Finally, a prospective comparison between measured spine BMD and values predicted from age, gender, weight deviation and height deviation was performed in 154 children referred to the Department of Nuclear Medicine, Hamilton Health Sciences for clinical DXA measurement.
Results
The dependence of DXA-measured variables upon age and gender in the group of 179 children has been reported previously [1, 18]. In those reports, expressions were derived that described the age-dependent increase for a given DXA variable measured in boys or girls as the sum of two logistic equations, one of which accounted for steady growth associated with aging and the other allowed for a more acute change associated with puberty. Residual values are the difference between measured values and values predicted from age and gender alone. Residuals for lumbar spine BMD increased steadily with increasing age for both girls and boys. The residuals for proximal femur BMD and whole body BMD also increased with age in boys, but were essentially unchanged with age in girls.
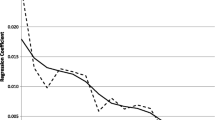
The dependence of spine BMD residuals upon body weight deviations is shown for boys in Fig. 1. The correlation coefficient is 0.61 and suggests that accounting for weight deviation could allow prediction of the spine BMD residual for a given child and therefore permit an adjustment to be made to the expected-for-age BMD. A similar relationship was observed in girls. Again, similar relationships between lumbar spine residuals and height deviations were observed for girls and boys, suggesting that the addition of height deviations could also improve predictions of expected BMD. The weakest correlations between weight deviations and BMD residuals were for whole body BMD (r = 0.27 for girls and 0.38 for boys), while the correlations for spine BMD (r = 0.48 for girls and 0.61 for boys) and femur BMD (r = 0.50 for girls and 0.62 for boys) were stronger and were similar to each other. In every case, the correlation coefficients were larger for boys. Correlation coefficients for the relationships between BMD residuals and height deviations were strongest for the lumbar spine (r = 0.50 for girls and 0.63 for boys), similar for the femur (r = 0.41 for girls and 0.58 for boys) and weakest for whole body BMD (r = 0.32 for girls and 0.43 for boys) and were always stronger in boys. These results, which probably reflect a greater size heterogeneity in boys than in girls, support the conclusion that expressions can be derived based on body size deviations that would improve the prediction of an expected BMD.
For each child, a correction to the expected-for-age lumbar spine BMD was obtained from the regression relationship between lumbar spine residuals and the observed weight deviation for that subject. That is, a second expected BMD value was generated based on age, gender and weight deviation. Comparison of the second expected BMD with the measured BMD yielded a second residual BMD. This second residual BMD was related to height deviations for each child. The resultant regression relationship was used to generate a correction that accounted for the height deviation for a given participant. The final predicted BMD was therefore based on the expected-for-age value modified by factors dependent on both height and weight deviation.
Table 1 shows the progressive improvements in correlation between measured and predicted DXA results when the basis of prediction is age alone, age and weight deviation, and finally age, weight deviation and height deviation. In all cases the addition of a weight deviation term improved the correlation between measured and predicted values. The subsequent inclusion of corrections based on height deviations also improved the correlation for all variables, but not to any great extent. For lumbar spine BMD, expected-for-age values accounted for 85.6% of the variance in measured values. The addition of weight deviations improved this value to 89.3%. The additional inclusion of height deviations means that ultimately 90.6% of the variance can be accounted for by age, gender and weight and height deviations.
Figure 2a shows the relationship between the measured lumbar spine BMD and the expected-for-age value for the 91 girls. If no other variables contributed significantly to the measured BMD, then all points would lie along the line of identity with no spread in measured BMD values. The dashed lines encompass more than 95% of measurements and could be considered as a normal range for measured BMD that spans 0.36 g cm−2. Figure 2b shows the same relationship between the measured lumbar spine BMD and the BMD predicted for each girl based on age, weight deviation and height deviation. Again, the dashed lines indicate reasonable confidence limits for the normal population of girls. The boundaries of the normal range for measured spine BMD have shrunk to 0.32 g cm−2.
For boys, the span of the normal range for measured BMD when plotted as a function of the expected-for-age BMD is 0.46 g cm−2, considerably greater than the corresponding range for girls. When the measured spine BMD is plotted as a function of the BMD predicted from age, weight deviation and height deviation, precisely the same normal range (0.32 g cm−2) emerges for boys as was developed for girls. The relationships between measured BMD and BMD predicted from gender, age, weight deviation and height deviation for the femur and whole body also revealed the same range of normal (0.32 g cm−2) in both girls and boys.
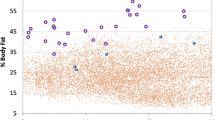
Figure 3 shows the normal range derived from the first sample of 179 children together with the results of measurements of lumbar spine BMD, proximal femur and whole body BMD made in the second sample of 26 children drawn from the local normal population. All BMD results for boys and girls, whether measured at the spine, hip or the whole body, fall within the same normal range after allowing for body size deviations.
Measured BMD for spine (white circles girls, black circles boys), femur (white triangles girls, black triangles boys) and whole body (white squares girls, black squares boys) compared with predicted BMD based on age, gender, weight deviation and height deviation in an independent sample of 26 normal children. The normal range was derived from the first sample of 179 normal children
The retrospective comparison of measured and expected values for a selected patient is shown in Fig. 4. The measured spine BMD is shown together with the expected-for-age BMD and the expected BMD based on age, weight deviation and height deviation. The measured BMD was considerably below both predicted BMD values at the time of first measurement. The early deficit at age 3.5 to 4.5 may be due to the effects of the disease or to the detrimental effect of the treatment of the disease on the skeleton. Accounting for weight and height deviations explains almost one third of the anticipated deficit when only the expected-for-age value is used. The measured BMD recovers to some extent after age 5.5 and despite a set-back at age 7, continues to improve, but never returns to the expected-for-age value. Consequently, without accounting for weight and height deviations, the patient would have been considered to have a spine BMD deficit. However, when the deviation in body size is allowed for, the patient had, in fact, recovered the BMD appropriate for age, gender, height and weight.
The deviation of a measured BMD from the expected-for-age BMD is expressed as the Z score. A deviation of a measured BMD from the BMD predicted from age and body size deviations can be expressed as a HAW score (Height-, Age-, Weight-adjusted score). Figure 5 compares Z scores and HAW scores for 154 children referred to the Department of Nuclear Medicine for clinical DXA measurement. The correlation coefficient for all patients was 0.75. For points within the region between the two dashed lines in Fig. 5, the Z score and the HAW score differ by 1.0 unit or less. Twenty-seven (17.5%) results lie outside the dashed lines, indicating differences between the two scores of greater than 1.0. The difference between a HAW score and a Z score is given by:
where SDHAW is the population standard deviation when the measured BMD is plotted as a function of the BMD predicted from age and body size deviation, and SDAge is the population standard deviation when the measured BMD is plotted as a function of the BMD predicted from age alone. The 2 population standard deviations will be similar and can be substituted by the term SD so that the above equation reduces to:
where SD is an average population standard deviation. This equation shows that, for the HAW score to be less than the Z score, which is the situation for the 9 participants (4 boys, 5 girls) below the lower dashed line in Fig. 5, the expected-for-age BMD must be less than the BMD expected from age and body size deviation. Conceptually, this will happen when an increased body weight and/or height results in an increase in the predicted BMD. A greater body size will have no impact on the expected-for-age BMD. For the 9 cases of concern, the mean body weight deviation (± standard error) was + 35.2 ± 4.6 kg. Body weights ranged from 23.1 kg to 64.2 kg above the 50th percentile for weight. The mean height deviation was + 5.9 ± 2.1 cm.
On the other hand, there were 18 participants above the upper dashed line (6 boys, 12 girls), in which case the HAW score is more than 1 unit greater than the Z score. From the above equation this outcome would be anticipated if the expected-for-age BMD was greater than the BMD expected from age and body size deviation. This would be true for children who were small-for-age such that the small body size lowered the expected density. The mean body weight deviation for the 18 children was −8.8 ± 1.6 kg. Weight deviations ranged from 1.4 kg above to 21.8 kg below the 50th percentile for weight. The mean height deviation was −11.2 ± 1.7 cm in the 18 children. For the majority of children in whom the two scores differed by less than 1 unit, the mean weight deviation was 0 ± 0.9 kg in boys (n = 64) and 1.3 ± 1.0 kg in girls (n = 63). The corresponding height deviations were −0.5 ± 0.8 cm in boys and −1.2 ± 0.8 cm in girls. Six (5 girls, 1 boy) of the 127 children for whom the Z and HAW scores were within 1 unit of each other had spine BMD Z scores that were either above +2.0 or below –2.0. Weight was more than 2 population standard deviations from the expected-for-age weight in 17 children, 3 of whom had abnormal HAW scores. Height was more than 2 population standard deviations from the expected-for-age height in 19 children, 4 of whom had abnormal HAW scores.
Discussion
Dual energy X-ray-based measurements of areal bone mineral density are used more and more frequently in children as the skeletal problems associated with the presence of various diseases and their treatments are appreciated [19]. A DXA measurement for a given child is generally interpreted by deriving a Z score that expresses the deviation of the result from an expected-for-age-and-gender value in terms of the population standard deviation appropriate for the age of the child [1]. In previous work, we measured lumbar spine BMD, proximal femur BMD and whole body BMD for a reasonable number of children (N = 179) whose ages were uniformly distributed between 3 and 18 years. Expressions were derived that allowed the calculation of an expected-for-age value and an expected standard deviation for each DXA variable based on the age and gender of a given child. We assume the expected-for-age values adequately represent those of the population of children at large, so that we can report the results of clinical measurements as Z scores.
Z scores only account for BMD variations due to age and gender. The covariance between age and body size means that Z scores also allow for the typical, average changes expected during growth. Any deviation of height or weight from an expected height or weight may impact BMD, but will not change the expected-for-age BMD nor the expected-for-age population standard deviation. Thus, body size deviations may affect BMD, but will not affect expected-for-age values. That is, Z scores may change without the influence of skeletal disease or the changes due to skeletal disease may be masked by body size deviations. The results given in this paper show that, for a specific child, any deviation in weight and/or height from the pattern of growth described for an average child has an impact on BMD, particularly at the spine and femur, but also for the whole body. The strength of the relationships between height and weight deviations on the one hand and BMD residuals on the other allow the derivation of expressions that could be used to modify expected-for-age values to account for body size deviations.
Comparison of measured and expected-for-age values would show no deviation from the line of identity if age was the single, unique determinant of BMD at any skeletal site. The range of results shown in Fig. 2 indicates that other factors are important. For a fixed expected-for-age spine BMD, the measured BMD in normal girls extends over a range of 0.36 g cm−2. For boys, the range was greater at 0.46 g cm−2. The incorporation of weight and height deviations into the prediction of expected values shrunk both ranges of measured values to 0.32 g cm−2 for girls and boys. That is, allowing for the weight and height deviations that existed in our population of normal children decreased the spread in results observed for both genders. The same outcome was observed for both femur BMD and whole body BMD. Based on age alone, normal femur BMD extended over a range of 0.42 g cm−2 for girls and 0.44 g cm−2 for boys. For whole body BMD the corresponding ranges were 0.34 g cm−2 and 0.36 g cm−2. When body size deviations were included in the derivation of an expected BMD, the ranges for femur and whole body BMD were the same as those for the spine (0.32 g cm−2) for both boys and girls.
Allowing for the effect of height and weight deviations decreased the observed range for measured BMD. At the same time, the range for the predicted BMD was extended. In Fig. 2, for example, expected-for-age lumbar spine densities vary from 0.45 g cm−2 to 1.01 g cm−2 for girls. Accounting for body size deviations extended that range to 0.42–1.22 g cm−2. Similar effects were observed for boys and for predicted values based on age and body size deviations for the femur and whole body.
To provide an acceptable test of normal predicted values, DXA measurements were made in a small but independent sample of 26 normal children drawn from the same local population. As shown in Fig. 3, the BMD values for these children at the spine, at the hip and for the whole body all fell within the expected, restricted, narrow range of normal values. That is, all 78 DXA measurements of spine, hip and whole body BMD obtained from boys and girls fell within the same, single range of normal. This has considerable implications for the reporting of BMD results in children. This single range of values is appropriate for the interpretation of DXA measurements in boys and girls of all ages and applies to the spine, the hip and the whole body.
Prediction of expected values based on gender, age and weight and height deviations means that the term Z score is no longer applicable because the Z score refers strictly to an expected-for-age value only. However, an analogous score can be derived. The procedure for deriving a HAW score is to modify the expected-for-age value [1] by two additional terms. The weight and height deviations are obtained for a particular patient and, using the appropriate intercept and coefficient from Table 2, a predicted BMD is obtained. Consequently, the data required for derivation of a HAW score in a specific patient are the measured BMD, the age, weight and height. The population standard deviation for any BMD variable is 0.08 g cm−2. For example, the first spine BMD data point shown in Fig. 4 is 0.329 g cm−2. This result was obtained from a boy aged 3.5 years who weighed 11.7 kg and was 96.6 cm tall. The expected-for-age spine BMD was 0.462 g cm−2 and the expected-for-age spine BMD population standard deviation was 0.062 g cm−2 [1]. Therefore, the Z score was (0.329–0.462)/0.062 or −2.1. The expected-for-age weight and height were 15.0 kg and 97.8 cm respectively [17]. Consequently, the participant had weight and height deviations of −3.3 kg and −1.2 cm. Using the equation shown in Table 2, together with the spine data listed for boys, the expected spine BMD becomes (0.462 + [−0.02068 + 0.004746 × (−3.3)] + [−0.004913 + 0.002592 × (−1.2)] or 0.418 g cm−2. The HAW score will be (0.329–0.418)/0.08 or −1.1. The task of calculating a predicted BMD and the resultant HAW score for a given patient can be assigned to a spreadsheet with the relevant formulae embedded.
The fact that the same range of measured BMD values was defined for the spine, the femur and the whole body in normal girls and boys means that adjusting for body size deviations accounts for the differences observed between gender-specific, expected-for-age normal values. When expected values based on gender, age and body size deviations were applied to a patient in order to illustrate the clinical application of HAW scores, it appeared as though spine BMD reached the predicted value based on age and body size (i.e. HAW score = 0) while the Z score remained negative (Z = -0−3). This demonstrates a complete recovery of spine BMD appropriate for the gender, age and size of the patient. Another similar patient demonstrated a lack of recovery to the expected-for-age value, which was only partially explained by a small body size. In another case, an apparently small deficiency in BMD (Z = −0.4) masked a considerable deficit compared with the expected-for-age and size value (HAW = −1.8).
Not surprisingly, the comparison of Z scores and HAW scores showed reasonable correlation, although in 17.5% of cases the two scores differed by more than 1 unit. A difference of this magnitude might be considered a threshold of clinical significance. That is, clinical decisions based upon a given Z score might not be the same as decisions based upon a HAW score that differs by more than 1 unit. Eighteen participants had Z scores more than 1 unit below their HAW scores. All were small for their chronological ages with a mean weight deviation of −8.8 kg and a mean height deviation of −11.2 cm. The 9 children in whom the HAW scores were considerably less than the Z scores, had a mean weight deviation of +35.2 kg and a mean height deviation of +5.9 cm. In children for whom the Z scores and HAW scores were within 1 unit of each other, there were still some who exhibited considerable body size deviations. Three children, for example, weighed more than 20 kg above the 50th percentile (+26.0, +20.7, +30.3); for each child the HAW score was lower than, but less than 1 unit lower than, the Z score.
Our approach may be limited by a number of factors. For example, our adjustment of expected-for-age BMD values for weight deviations does not distinguish between the impact of changes in lean mass compared with the impact of changes in adipose tissue mass. No direct adjustment is made for bone size variation, pubertal status or for the fact that BMD is only a two-dimensional measurement. The adjustments described in this paper are based on BMD measurements obtained from Hologic equipment. In addition, the expected-for-age BMD values we have utilised were based on a relatively small (N = 179) population of normal, local children. Differences may exist between our results and populations of different ethnic origin.
The ultimate objective of a BMD measurement is to identify children who may be at increased risk of fracture. Currently, the relationship between a BMD measurement and its associated fracture risk is expressed through a Z score. The work reported in this paper has shown that body size deviations exert a considerable impact on measured BMD for approximately 17.5% of children. Other pediatric populations might be more heterogeneous with even greater size effects. Body size deviations could mean that a negative Z score may be appropriate for a small-for-age child and that fracture risk is not increased. Alternatively, a positive Z score may mask an increased fracture risk because the effect of an increased mechanical demand originating from a greater than expected body size overrides a decreased BMD arising from mineral deficiency. The calculation of HAW scores will account for body size deviations in both cases and should provide more accurate assessments of bone integrity. It remains to be shown whether HAW scores can predict fracture risk with greater accuracy than Z scores.
References
Webber CE, Beaumont LF, Morrison J et al (2007) Age predicted values for lumbar spine, proximal femur and whole body bone mineral density; results from a population of normal children aged 3 to 18 years. Can Assoc Radiol J 58:37–45
Jones G, Ma D, Cameron F (2006) Bone density interpretation and relevance in Caucasian children aged 9–17 years of age: insights from a population-based fracture study. J Clin Densit 9:202–209
Goulding A, Jones IE, Taylor RW et al (2000) More broken bones: a 4-year double cohort study of young girls with and without distal forearm fractures. J Bone Min Res 15:2011–2018
Ma DQ, Jones G (2002) Clinical risk factors but not bone density are associated with prevalent fractures in prepubertal children. J Paediatr Child Health 38:497–500
Jones IE, Williams SM, Goulding A (2004) Associations of birth weight and length, childhood size and smoking with bone fractures during growth: evidence from a birth cohort study. Am J Epidemiol 159:343–350
Chevalley Y, Rizzoli R, Hans D et al (2005) Interaction between calcium intake and menarcheal age on bone mass gain: an eight year follow-up study from prepuberty to postmenarche. J Clin Endocrinol Metab 90:44–51
Goulding A, Grant AM, Williams SM (2005) Bone and body composition of children and adolescents with repeated forearm fractures. J Bone Min Res 20:2090–2096
Ferrari SL, Chevalley T, Bonjour J-P et al (2006) Childhood fractures are associated with decreased bone mass gain during puberty: an early marker of persistent bone fragility? J Bone Min Res 21:501–507
Rauch F, Neu C, Manz F et al (2001) The development of metaphyseal cortex—implications for distal radius fractures during growth. J Bone Min Res 16:1547–1555
Gafni RI, Baron J (2004) Overdiagnosis of osteoporosis in children due to misinterpretation of dual-energy X-ray absorptiometry (DEXA). J Pediatr 144:253–257
Lu PW, Briody JN, Ogle GD et al (1994) Bone mineral density of total body, spine, and femoral neck in children and young adults: a cross-sectional and longitudinal study. J Bone Min Res 9:1451–1458
Mølgaard C, Thomsen BL, Prentice A et al (1997) Whole body bone mineral content in healthy children and adolescents. Arch Dis Child 76:9–15
Warner JT, Cowan FJ, Dunstan FDJ et al (1998) Measured and predicted bone mineral content in healthy boys and girls aged 6–16 years: adjustment for body size and puberty. Acta Paediatr 87:244–249
Fewtrell MS, Gordon I, Biassoni L et al (2005) Dual X-ray absorptiometry (DXA) of the lumbar spine in a clinical paediatric setting: does the method of size adjustment matter? Bone 37:413–419
Prentice A, Parsons TJ, Cole TJ (1994) Uncritical use of bone mineral density in absorptiometry may lead to size-related artifacts in the identification of bone mineral determinants. Am J Clin Nutr 60:837–842
Horlick M, Wang J, Pierson RN et al (2004) Prediction models for evaluation of total-body bone mass with dual-energy X-ray absorptiometry among children and adolescents. Pediatrics 114:e337–e345
Centers for Disease Control and Prevention. Clinical growth charts. Available at: http://www.cdc.gov/growthcharts, Accessed December 2006
Sala A, Webber CE, Morrison J et al (2007) Whole body mineral mass, lean body mass and fat mass measured by dual photon absorptiometry in a population of normal Canadian children and adolescents. Can Assoc Radiol J 58:46–52
Binkoviyz LA, Henwood MJ (2007) Pediatric DXA: technique and interpretation. Pediatr Radiol 37:21–31
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Webber, C.E., Sala, A. & Barr, R.D. Accounting for body size deviations when reporting bone mineral density variables in children. Osteoporos Int 20, 113–121 (2009). https://doi.org/10.1007/s00198-008-0642-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-008-0642-y