Abstract
Summary
The remodeling transient describes a change in bone mass that lasts one remodeling cycle following an intervention that disturbs the calcium economy. We demonstrated the transient in a study of the response of bone density to calcium/vitamin D3 supplementation and show the hazards of misinterpretation if the transient is not considered.
Introduction
The remodeling transient describes a change in bone mass that lasts for one remodeling cycle following an intervention that disturbs the calcium economy.
Methods
We report an intervention with calcium and vitamin D supplementation in 208 postmenopausal African-American women where the remodeling transient was considered a priori in the study design. Both groups (calcium alone vs. calcium + 20 μg (800 IU) vitamin D3) were ensured a calcium intake in excess of 1200 mg/day.
Results
There were no differences between the two groups in changes in BMD over time. These BMD changes were therefore interpreted to reflect increased calcium intake in both groups but not any influence of vitamin D. A transient increase in bone mineral density was observed during the first year of study, followed by a decline. The remodeling period was estimated at about 9 months, which is similar to histomorphometric estimates.
Conclusion
It is problematic to draw conclusions concerning interventions that influence the calcium economy without considering the remodeling transient in study design. Studies of agents that effect bone remodeling must be carried out for at least two remodeling cycles and appropriate techniques must be used in data analysis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Interpretation of studies evaluating the effect of calcium or vitamin D supplements on bone loss can be incomplete when researchers fail to consider the remodeling transient in their study design. The remodeling transient is a concept that was developed from the understanding of bone histomorphometry and from calcium kinetic analyses [1–7]. A change in the activation frequency of new remodeling units as the result of reduction in parathyroid hormone (PTH) secretion (by increasing calcium and/or vitamin D intake or by administration of any antiresorptive agent) will result in a change in bone mass that persists for one remodeling cycle but may not be retained in subsequent remodeling cycles. This occurs because although the number of units of bone that are active are reduced, previously activated units are progressing at the prior rate. The remodeling space is reduced and bone is transiently in positive balance. After the completion of one remodeling cycle new units are progressing at a rate similar to the rate at which old units are being removed. Thus, the change in remodeling balance lasts only for the duration of one remodeling cycle (at least 6 months) and is appropriately referred to as “transient”. If common linear regression (which assumes proportionality and therefore ignores any ‘peak’ in the data plot) analytic techniques are used to model bone loss studies, or if studies are not conducted for a long enough period of time, the remodeling transient can incorrectly be interpreted as a long term beneficial result of the intervention.
We recently completed a study of the effect of vitamin D supplementation (20–50 μg/d) on bone loss in calcium replete, African-American postmenopausal women [8]. We performed the trial with the remodeling transient considered in our study design. Although we noted no benefit of vitamin D supplementation in the dose used over and above calcium supplementation, we were able to detect the remodeling transient in both the vitamin D plus calcium and calcium alone groups in almost all of the sites observed (the lumbar spine being the exception). We present here a detailed analysis of the remodeling transient and its relevance in interpreting interventions that reduce bone remodeling. We seek to answer the following questions:
-
1).
What period of time best describes the remodeling transient?
-
2).
Are there observable changes in serum PTH and bone remodeling markers that are consistent with the transient effect?
Methods
Participants
Ambulatory postmenopausal African-American women not on hormone replacement therapy were recruited from the Long Island community (Table 1). All the participants provided written informed consent and the trial was approved by the institutional review board of Winthrop-University Hospital. African-American ancestry of the participants was assessed by self-declaration that both parents and at least three out of four grandparents were African-American. Exclusion criteria included previous treatment with bone active agents and any medication or illness that affects skeletal metabolism.
Study design
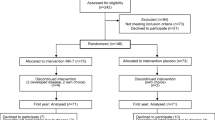
The participants were randomly assigned using a computer-generated sequence to receive either 20 μg/d (800 IU/day) of oral vitamin D3 or a matched placebo. Data are presented for the first 24 months, which includes the remodeling transient and at least one subsequent remodeling cycle. Calcium intake was assessed by food frequency on each visit and supplements were given to both groups to ensure a total daily intake of 1200–1500 mg calcium. Supplements were supplied as calcium carbonate (500 mg or 250 mg of elemental calcium) and were taken with meals in divided doses. Vitamin D3 (20 μg) and matched placebo capsules were custom-manufactured for the study (Tishcon Corp., Westbury, NY).
Outcome variables
Bone density measurements
Bone mineral density (BMD) was measured at 6-month intervals at the total femur, non-dominant mid-radius, whole body, and spine (AP) with a dual-energy x-ray absorptiometer (model QDR 4500, Hologic Inc. version 9.80D). The coefficient of variation at our center for lumbar spine (L1–L4) is 0.81%, total hip is 0.62%, total body is 0.49% and mid-radius is 0.78%. Total body BMC is reported with data from the skull region deleted.
Laboratory tests
A fasting blood sample was collected for analyses of calcium, parathyroid hormone (PTH), 25-hydroxyvitamin D (25-OHD), osteocalcin, and c-terminal telopeptide (CTX) at baseline, 3, 6, 12, 18, 24, 27, 30 and 36 months. Serum albumin was measured annually. Serum PTH was measured by the Allegro intact-PTH immunoassay purchased from Nichols Institute Diagnostics (San Juan Capistrano, CA) [9]. Serum 25-OHD was measured by radioimmunoassay (RIA) using a kit manufactured by DiaSorin, Inc. (Stillwater, MN) [10]. Serum osteocalcin and serum CTX (c-terminal telopeptide of Type-1 collagen) were measured by a one step enzyme-linked immuno-absorbent assay (ELISA). The kits were manufactured by Nordic Bioscience Diagnostics A/S (Herlev, Denmark).
Statistical methods
The theory behind the remodeling transient suggests a quadratic shape to the BMD curve drawn over a time period that includes measurements made before, during and after the transient period as proposed by Heaney [3]. This assumption was tested statistically by estimating the parameters of a repeated measures mixed ANOVA model containing the terms time and time-squared to test for the adequacy of a quadratic model over the first 18 months of the study. This period was chosen because the change after 18 months was clearly linear. At all sites (except lumbar spine) the addition of time-squared to the linear model was highly significant. We calculated the maximum of these parabolic curves by differentiating the fitted quadratic functions determined by the estimated parameters, setting them to zero and solving for time. This approach was confirmed heuristically by determining the month when each individual patient’s BMD reached a maximum and then calculating the mean month across the sample. This measure was highly correlated with the quadratic approach. Only the quadratic calculated peak is reported.
The P-values cited below were generated using a mixed model ANOVA for all changes over time except for 6-month differences (0–6 and 6–12 months); there a paired t-test was used. Univariate Pearson and (non-parametric) Spearman linear correlations were computed to quantify the concomitant changes over the time periods baseline to three months, baseline to six months (for BMD and BMC) and three to six months, six to 12 months, 12 to 18 months and 18 to 24 months between pairs of variables from the set, including BMD and BMC measures, serum calcium, serum PTH, 25(OH)D, and the bone markers serum osteocalcin and CTX. Multiple linear regression models were tested to determine the independent contribution of these variables on the changes in BMD at the various sites. There were no statistical differences between the Ca and Ca+D groups in all variables, including baseline characteristics and adherence. There were no differences between the groups at any time point with respect to PTH, serum calcium, osteocalcin or CTX. (The only exception, of course, was 25(OH)D.) We, therefore, pooled the two groups in the analyses presented below. When analyzed separately the pattern of results and conclusions are the same.
A p-value below 0.05 was considered statistically significant. Results are presented as mean (standard deviation) and as 95% confidence intervals where appropriate. Alternative hypotheses were two-sided. Pearson correlation analyses were done between the calcitropic hormones, serum 25-OHD, indices of bone turnover, and the bone mineral density measurements. For data analysis, we used the statistical package SAS 9.1 (SAS Institute, Inc., Cary, N.C.).
Results
Baseline characteristics
The baseline demographic profile of the study population is summarized in Table 1. The baseline laboratory values are given in Table 2. There were no significant differences between the two groups. A majority of the participants had some college experience. These black women had a moderately active lifestyle. Approximately 47% of women were taking supplemental calcium and/or vitamins at baseline. Seven percent of subjects were still smoking. The initial BMD at the total hip for the whole cohort ranged from normal (65%) to osteopenic (33.6%) to osteoporotic (1.4%) with a mean T-score of −0.03 (1.08) (range: −3.0, 2.9) using NHANES III young white females as the reference. The age, sex and race adjusted Z-score had a mean of 0.18 (0.85) (range: −2.2, 2.6). The baseline 25-OHD levels ranged from 12.5 nmol/L to 99.7 nmol/L with a mean level of 45.1 ± 18.8 nmol/L in the study population.
Adherence
Pill-count compliance was 87% (8%) of vitamin D pills consumed after the randomization visit. Approximately 96% (7%) of the subsequent visits were kept by our patients. Daily calcium intake including supplements was 1312 ± 153 mg/d in the Ca group and 1349±204 mg/d in the Ca + D group.
Serum PTH, calcium, and 25OHD concentration
The response of PTH to calcium is shown in Fig. 1b. A statistically significant decline at three months in PTH (from 42 (19) pg/ml to 24 (15) pg/ml, p < .0001) was noted (it was present in each group analyzed separately as well). The 6-month values increased to 38.0 (18) pg/ml, p < .003. However, PTH concentration remained below baseline values throughout the 24-month study period. The mechanism for the decline in PTH is suggested by consideration of the concomitant changes in serum calcium. Serum calcium increased significantly from 8.9 (.54) mg/dL to 9.2 (.53) mg/dL, p < .001) at 3 months with no further significant changes thereafter (Fig. 1a). The serum calcium remained above the baseline value throughout the 24-month time period. Serum albumin was not obtained on each study sample so that serum calcium could not be corrected for each study period. However, albumin measured annually remained unchanged, and corrected serum calcium did not differ in its direction from uncorrected calcium.
Concomitant changes with calcium supplementation: Absolute values (+/− 2 SEM). Panel (1a): Serum calcium, Panel (1b): PTH, Panel (1c): CTX, Panel (1d): Osteocalcin, Panel (1e): Total femur BMD, Panel (1f): total body BMD, B: significantly different from baseline, p < .002, b: significantly different from baseline, p < .05, D: significantly different from preceding period, p < .002, d: significantly different from preceding period, p < .05, The dashed line in Panels 1e and 1f represent the quadratic model fitted to the data over 18 months
Mean serum 25-OHD levels increased in the Ca + D group from a baseline of 47 nmol/L (42.9, 50.9) to 71 nmol/L (66.6, 76.3), (p < 0.001) with 3 months of 20 μg/d vitamin D3. The serum 25-OHD levels in the Ca alone group did not change significantly throughout the study.
Bone density
There were no differences in rates of bone loss at any time between the vitamin D + calcium vs. the calcium alone supplement groups, so for purposes of subsequent analyses the bone density data were pooled. Each group, when also analyzed separately, showed no difference in the pattern of changes from the combined analyses, so only the latter are reported here. Over the two-year period, there were statistically significant declines in BMD at each site except the lumbar spine. However, when the first year of data is considered separately, an increase was seen at all sites. The significant change over the first year can be seen to consist of two stages: a highly significant increase over the first six months and a relative lack of change from six to twelve months. During the second year, highly significant decreases are seen in BMD measures (except for the lumbar spine), which is remarkably stable across time in several studies in addition to ours.
Presumably, this initial six-month change represents the temporary reduction in the remodeling space resulting from increased calcium intake and reduction in serum PTH. Table 3 provides the absolute and percent BMD change for the total femur, lumbar spine, mid-radius and total body BMC, at baseline to six months, six months to one year, baseline to one year, and 1 to 2 years of the study.
While the BMD data peaks at the six-month observation, the six-month gap between measurements does not allow us to observe the actual peak directly. The data may more appropriately be viewed in terms of the duration of the remodeling transient by fitting a quadratic function through the first 18-month data points at each site (except the ‘flat’ lumbar spine). The analytic peak was 9.7 months for the total femur, 8.9 months for TBBMC, and 9.6 months for the 1/3 radius. The values for bone density are schematically depicted as Fig. 1e,f before and after the transient. While the DXA data are depicted as the absolute BMD values; Table 3 also includes the percent change from baseline to 6 months, baseline to one year, 6 months to one year and one to two years.
Biomarkers of bone remodeling
The median values at baseline, 3, 6, 12, 18 and 24 months for the serum CTX and osteocalcin are depicted in Fig. 1c,d. A decline at 3 months was statistically significant for both markers, CTX and osteocalcin.
CTX decreased significantly from 2501(1069) pM to 2087 (1160) pM, p < .0001) at 3 months. Osteocalcin decreased significantly from 15.2 (7.7) ng/ml to 14.3 (7.3) ng/ml, p < .0005) at 3 months. The transient increase in BMD at all sites (except lumbar spine) at the six-month measurement was paralleled by a corresponding increase in serum calcium and a statistically significant decline in PTH, CTX and osteocalcin. Mean differences and correlations often present two distinct types of information (e.g., it is possible that two groups of scores may have a mean difference but no correlation or vice versa) [11]. Therefore, Table 4 presents the bivariate correlations of corresponding changes between pairs of variables over all patients across the same time periods depicted in Fig. 1. The PTH changes were positively correlated with changes in the bone markers (CTX and osteocalcin). The six-month changes in the bone markers were highly significantly (negatively) correlated with the femur BMD changes. The linear associations between these variables are confirmed by the pattern of correlations across the other time periods. Serum 25(OH)D was correlated with serum PTH.
By the end of the remodeling transient, when serum calcium and PTH levels reached a steady state (12 months), CTX and osteocalcin were no longer reduced, and levels rose above baseline. BMD resumed its post-menopausal downward trend and BMD was lost from all sites (except the spine).
One can see the correspondence between the means among serum calcium, PTH, osteocalcin, CTX and bone density by the parallelisms and mirror images among the six graphs of Fig. 1. The degree of association is quantitatively summarized by the positive and negative correlations between the change scores over 3, 6 and 12 months from baseline in Table 4. These results are consistent with a model of increased dietary calcium increasing serum calcium (Fig. 1a) which in turn suppresses PTH (Fig. 1b). This results in a reduction in bone turnover (Fig. 1c,d) and a subsequent increase in BMD (Fig. 1e,f). Support for this model is also seen in the positive correlations between PTH and CTX (r = 0.40, p < .0001) and PTH and osteocalcin (r = 0.15, p < .06) in the changes from 3 to 6 months.
Serum 1,25(OH)2D
Figure 2 depicts the response of serum 1,25(OH)2D in the two groups. It may be seen that there was a decline in serum 1,25(OH)2D in the calcium alone group that was sustained throughout the study (for the Ca alone group p-values comparing baseline to each time point were less than .0001 for all months except for month 18 where p = .01; for the Ca + D group, p-values comparing baseline to each time point were always greater than 0.12 except for month 24 where p = .01). The serum level of 1,25(OH)2D did not decline in the Ca + D group, and was maintained throughout the study. The presumed mechanism for reduction in serum calcitriol is seen in Fig. 1 with the increase in serum calcium and decline in PTH. No significant correlations were noted between serum 1,25(OH)2D and the other variables (PTH, 25(OH)D, CTX and osteocalcin).
Initial and sustained changes in 1,25OHD2D in the calcium only group (dashed lines) are not experienced by the vitamin D + calcium group (solid line). p < .01 group comparisons at each line point; p < .01 for all comparisons with baseline for the calcium group but not for the vitamin D + calcium group
Discussion
The primary objective of our study was to investigate the influence of vitamin D supplementation on bone loss in calcium replete, African-American post-menopausal women. We found that there was no influence of vitamin D supplementation in the dose provided on rates of bone loss in these women who were supplied with a daily calcium intake of 1300 mg and were presumably calcium-replete. Indeed, serum 250HD levels were not correlated with rates of bone loss [12]. We did, however, detect an early increase in bone density in both groups which is presumably the result of almost doubling the calcium intake in both groups from mean values of 759 mg/day to 1300 mg/day. The peak of bone density increase was analyzed using a quadratic model which revealed a remodeling peak of 8.9 months for TBBMC. Most of the sites had a similar parabolic shape and remodeling transient duration, except for the lumbar spine which increased at 6 months but did not decline thereafter. This response of the lumbar spine has been noted in other studies [12]. The most plausible explanation given for the failure to observe a decline in the lumbar spine even in placebo groups involves a technical aspect of DXA. There is an increase in vascular calcification and osteophytes which leads to false elevation in lumbar spine DXA values with aging [13, 14].
It is apparent that the results of this study would be interpreted differently if the remodeling transient were not considered. If the study were carried out for one year, it might be suggested that calcium (vitamin D) intake increases bone mass. The difference between rates of loss after the transient interval vs. rates of bone loss during the remodeling transient are depicted in 1e and 1f. In the first year of the study, there was a statistically significant increase of bone density at each skeletal site. However, when the data were analyzed after the first year there were significant losses at every site (except the spine).
Mackerras and Lumley [15] performed a meta-analysis of randomized clinical trials of calcium augmentation with over 2 years of data. They reviewed nine studies to determine if rates of loss with increased calcium intake differed between the first and second year of intervention [16–23]. They concluded that there was a difference in the rate of loss in the first year but no difference in rates over subsequent years. Heaney [24] evaluated three published calcium intervention studies for errors that may occur in interpretation by not considering the remodeling transient. The Dutch menopausal study evaluated adding 1000–2000 mg/d to diets that had a mean intake of 1150 mg/day [25]. An increase in BMD was noted in both groups compared to the placebo group at 1 year followed by a parallel rate of skeletal loss in all 3 groups. Thus, the new steady intake rate of loss was unchanged after a year despite intakes of 2150 or 4150 mg of calcium/day. The Indiana Twins study was a 3-year trial of calcium intervention in identical twins [26]. There was an initial rise in BMD in the supplemented twins followed by a slower rate of increase. After discontinuing the supplement, the difference between the twins diminished. A study by Peacock et al. [27] was also cited. Heaney [3] calculated an 8% reduction in remodeling at year 1. There was a gain in bone density of 0.6%/year at one year, at 2 years it was 0.2%/year, and at years 3 and 4, it was −.012%/year and −.05%/year, respectively.
Calcium supplementation studies have shown that when the supplementation is discontinued rates of bone loss revert to pre-supplementation levels [28]. The effect of calcium supplementation may be limited to the first remodeling cycle; it is expected that when the intervention is discontinued a remodeling cycle with remodeling balance in the opposite direction follows. Several studies carried out over a prolonged period (4 years) suggest a sustained benefit of calcium supplementation on bone mineral density [29–31].
The timing of the changes in the biochemical measurements in this study are of interest, and are consistent with the concept of a calcium intake/PTH mechanism for the remodeling transient. Serum calcium increased slightly after calcium supplements were initiated, and PTH levels declined. This resulted in a temporary decline in bone marker levels (bone turnover). Bone density increased for the first remodeling cycle, presumably as a result of a reduction in the remodeling space. Although serum calcium remained elevated above baseline, PTH levels increased to a level towards baseline. It would have been of interest to measure PTH continuously rather than simply in the fasting state, but this was not planned [32]. After completion of the remodeling cycle (9 months), the markers of bone turnover increased to above baseline. Whether this represents a remodeling cycle in the opposite direction following the remodeling transient is uncertain.
Our estimated length of the remodeling cycle is of interest in comparison to studies using bone histomorphometry. Kimmel et al. [33] performed transiliac biopsies in 34 healthy premenopausal women and 90 women with postmenopausal osteoporosis. The mean remodeling period (years) was .96 ± .75 for osteoporotics and 1.12 ± 1.03 (SD) for normals (N.S.). It is important to appreciate that these studies were performed in white women. Han et al. [34] and Weinstein and Bell [35] reported that bone formation rate is lower in African-American women. The mean formation period (the time required to rebuild a new structural unit) was prolonged in blacks compared to whites (39.5 days vs. 81 days, respectively) [35]. In addition, the bone markers in the current study are lower than in white women, confirming previous reports [36]. Ethnic differences in bone remodeling may have important implications for the design and interpretation of clinical intervention studies that target bone remodeling.
Calcium supplementation suppresses the synthesis of calcitriol, presumably by producing an increase in serum calcium which reduces PTH secretion as observed in this study. Other investigators have also noted reduction of calcitriol levels following increased calcium intake [37, 38]. In a previous study comparing calcium supplementation to hormone replacement therapy (HRT) and to placebo, we found that calcium supplementation suppressed serum levels of 1,25(OH)2D, whereas these levels were maintained in the HRT plus calcium group [39]. Estrogen increases the synthesis of 1,25(OH)2D [39]. This observation is interesting in light of the calcium-vitamin D arm of the Women’s Health Initiative [31]. This study has been criticized because inadequate vitamin D was provided. However, subset analyses revealed a beneficial effect of calcium/D supplements in those who were on HRT. Could the presumably higher levels of calcitriol prevent falls and hip fracture and thereby explain this observation? It can also be suggested that the very high calcium intake with an inadequate vitamin D intake in the WHI could lead to reduced protection against falls and fracture.
Our study limitations include the lack of a control group that did not receive supplementation with calcium or vitamin D. A calcium-deficient control group was not included for ethical concerns in a long-term study. The different findings between the calcium and calcium plus vitamin D group, however, were clear. The strength of this study is that we predicted a priori that there would be a remodeling transient and it was indeed observed.
In conclusion, failure to consider the remodeling transient in study design may result in incorrect conclusions not only in calcium or vitamin D supplementation studies, but in any intervention that temporarily reduces the remodeling space. Heaney [7] applied this reasoning to antiresorptive treatment of osteoporosis. Nonetheless, a recent publication of a promising new bone active agent did not mention the transient even though the study was carried out for only one remodeling cycle [40]. Hopefully, there will be greater awareness of the effect of the remodeling transient in the future. Certainly claims for efficacy of an antiresorptive medication should not be made based on one remodeling cycle.
References
Parfitt A (2002) Targeted and nontargeted bone remodeling: relationship to basic multicellular unit origination and progression. Bone 30(1):5–7
Frost H (1989) Some effects of basic multicellular unit-based remodelling on photon absorptiometry of trabecular bone. Bone Miner 7(1):47–65
Heaney RP (1994) The bone-remodeling transient: implications for the interpretation of clinical studies of bone mass change. J Bone Miner Res 9(10):1515–1523
Parfitt AM (2004) What is the normal rate of bone remodeling? Bone 35:1–3
Frost H (1973) The origin and nature of transients in human bone. remodelling dynamics. In: Frame B, Parfitt AM, Duncan H (eds) Clinical Aspects of Metabolic Bone Disease. Excerpta Medica, Amsterdam, pp 124–140
Heaney RP (2003) Is the paradigm shifting? Bone 33:457–465
Heaney RP, Yates AJ, Santora AC 2nd (1997) Bisphosphonate effects and the bone remodeling transient. J Bone Miner Res 12(8):1143–1151
Aloia JF, Talwar SA et al (2005) A randomized controlled trial of vitamin D3 supplementation in African-American women. Arch Intern Med 165:1618–1623
Kao PC, Jiang NS, Klee GG, Purnell DC (1982) Development and validation of a new radioimmunoassay for parathyrin (PTH). Clin Chem 28(1):69–74
Hollis B (1984) Relative concentrations of 25-hydroxyvitamin D2/D3 and 1,25-dihydroxyvitamin D2/D3 in maternal plasma at delivery. Nutr Res 4:27
McCall RB (1975) Fundamental Statistics for Psychology, 2nd edn. Harcourt Brace Jovanovitch, New York, p 228
Dawson-Hughes B, Harris SS, Krall E, Dallal G (1997) Effect of calcium and vitamin D supplementation on bone density in men and women 65 years of age or older. N Engl J Med 337(10):670–676
Jones G, Nguyen T, Sambrook P et al (1994) Progressive loss of bone in the femoral neck in elderly people: longitudinal findings from the Dubbo osteoporosis epidemiology study. BMJ 309:691–695
Greenspan SL, Maitland LA, Myers ER et al (1994) Femoral bone loss progresses with age: a longitudinal study in women over age 65. J Bone Miner Res 9:1959–1965
Mackerras D, Lumley T (1997) First- and second-year effects in trials of calcium supplementation on the loss of bone density in postmenopausal women. Bone 21:527–533
Aloia JF, Vaswani A, Yeh JK et al (1994) Calcium supplementation with and without hormone replacement therapy to prevent postmenopausal bone loss. Ann Intern Med 120(2):97–103
Dawson-Hughes B, Dallal GE, Krall EA et al (1990) A controlled trial of the effect of calcium supplementation on bone density in postmenopausal women. N Engl J Med 323(13):878–883
Elders P, Netelenbos J, Lips P et al (1991) Calcium supplementation reduces vertebral bone loss in perimenopausal women: a controlled trial in 248 women between 46–55 years of age. J Clin Endocrinol Metab 73:533–540
Hansson T, Roos B (1987) The effect of fluoride and calcium on spinal mineral content: A controlled, prospective (3 years) study. Calcif Tissue Int 40:315–317
Prince RL, Devine A, Dick I et al (1995) The effects of calcium supplementation (milk powder or tablets) and exercise on bone density in postmenopausal women. J Bone Miner Res 10:1068–1075
Prince RL, Smith M, Dick I et al (1991) Prevention of postmenopausal osteoporosis. A comparative study of exercise, calcium supplementation, and hormone-replacement therapy. N Engl J Med 325:1189–1195
Reid IR, Ames RW, Evans MC et al (1993) Effect of calcium supplementation on bone loss in postmenopausal women. N Engl J Med 328(7):460–464
Riis BJ, Thomsen K, Christiansen C (1987) Does calcium supplementation prevent postmenopausal bone loss? N Engl J Med 316:173–177
Heaney RP (2001) The bone remodeling transient: interpreting interventions involving bone-related nutrients. Nutr Rev 59(10):327–333
Elders P, Netelenbos J, Van Ginkel F et al (1994) Long-term effect of calcium supplementation on bone loss in perimenopausal women. J Bone Miner Res 9(7):963–970
Johnston CC, Miller J, Slemenda CW et al (1992) Calcium supplementation and increases in bone mineral density in children. N Engl J Med 327:82–87
Peacock M, Liu G, Carey M et al (2000) Effect of calcium or 25OH vitamin D3 dietary supplementation on bone loss at the hip in men and women over the age of 60. J Clin Endocrinol Metab 85:3011–3019
Dawson-Hughes B, Harris SS, Krall E, Dallal GE (2000) Effect of withdrawal of calcium and vitamin D supplements on bone mass in elderly men and women. Am J Clin Nutr 72(3):745–750
Reid IR, Ames RW, Evans MC et al (1995) Long-term effects of calcium supplementation on bone loss and fractures in postmenopausal women: a randomized controlled trial. Am J Med 98(4):331–335
Dawson-Hughes B, Harris SS, Krall E, Dallal G (1997) Effect of calcium and vitamin D supplementation on bone density in men and women 65 years of age or older. N Engl J Med 337(10):670–676
Jackson R, LaCroix A, Gass M et al (2006) Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med 354(7):669–683
McKane WR, Khosla S, Egan KS et al (1996) Role of calcium intake in modulating age-related increases in parathyroid function and bone resorption. J Clin Endocrinol Metab 81(5):1699–1703
Kimmel D, Recker R, Gallagher J et al (1990) A comparison of iliac bone histomorphometric data in post-menopausal osteoporotic and normal subjects. Bone Miner 11(2):217–235
Han ZH, Palnitkar S, Rao DS et al (1997) Effects of ethnicity and age or menopause on the remodeling and turnover of iliac bone: implications for mechanisms of bone loss. J Bone Miner Res 12(4):498–508
Weinstein R, Bell N (1988) Diminished rates of bone formation in normal black adults. N Engl J Med 319(26):1698–1701
Aloia, JF, Vaswani A, Feuerman M et al (2000) Differences in skeletal and muscle mass with aging in black and white women. Am J Physiol Endocrinol Metab 278(6):E1153–1157
Pattanaungkul S, Riggs BL, Yergey AL et al (2000) Relationship of intestinal calcium absorption to 1,25-dihydroxyvitamin D [1.25(OH)2D] levels in young versus elderly women: evidence for age-related intestinal resistance to 1,25(OH)2D action. J Clin Endocrinol Metab 85(11):4023–4027
Martini L, Wood RJ (2002) Relative bioavailability of calcium-rich dietary sources in the elderly. Am J Clin Nutr 76(6): 1345–1350
Aloia J, Vaswani, A, Yeh J, Russo L (1996) Differential effects of dietary calcium augmentation and hormone replacement therapy on bone turnover and serum levels of calcitrophic hormones. Osteoporos Int 6:55–62
McClung M, Lewiecki E, Cohen S et al (2006) Denosumab in postmenopausal women with low bone mineral density. N Engl J Med 354:821–831
Acknowledgments
We would like to thank Sharon Sprintz, RT, Jane Greensher, R.N., and Marty Feuerman for their expertise and Lynn Maier for preparation of the manuscript.
J.F.A. was the principal investigator for the study, S.A.T. was the co-investigator and was responsible for medical supervision of the study participants; S.P. is the study statistician, performed statistical analyses, analyzed data; J.Y. is laboratory drector and was responsible for biochemical assays in the study.
Funding
This research was funded by National Institute of Aging (RO1 AG15325), NIH.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aloia, J.F., Arunabh-Talwar, S., Pollack, S. et al. The remodeling transient and the calcium economy. Osteoporos Int 19, 1001–1009 (2008). https://doi.org/10.1007/s00198-007-0542-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-007-0542-6