Abstract
Introduction
Osteoporotic fractures in older people are a major and increasing public health problem. We examined the effect of vitamin D supplementation on fracture rate in people living in sheltered accommodation.
Methods
In a pragmatic double blind randomised controlled trial of 3 years duration, we examined 3,440 people (2,624 women and 816 men) living in residential or care home. We used four-monthly oral supplementation using 100,000 IU vitamin D2 (ergocalciferol). As a main outcome measure, we used the incidence of first fracture using an intention to treat analysis. This was a multicentre study in 314 care homes or sheltered accommodation complexes in South Wales, UK.
Results
The vitamin D and placebo groups had similar baseline characteristics. In intention-to-treat analysis, 205 first fractures occurred in the intervention group during a total of 2,846 person years of follow-up (7 fractures per 100 people per year of follow-up), with 218 first fractures in the control group over 2,860 person years of follow-up. The hazard ratio of 0.95 (95% confidence interval 0.79–1.15) for intervention compared to control was not statistically significant.
Conclusion
Supplementation with four-monthly 100,000 IU of oral vitamin D2 is not sufficient to affect fracture incidence among older people living in institutional care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporotic fractures in older people are a major and increasing public health problem resulting in much pain and suffering, disability, premature death and cost to health and social services. A quarter of all low trauma fractures in people over the age of 75 occur in institutional care. Fragility fractures are twice as common in nursing and residential home residence compared to people of the same age living in their own homes [1].
The Chapuy et al. study [2] in 1992 examined D3 (cholecalciferol) and calcium in 3,270 healthy ambulatory women. They reported that vitamin D and calcium supplementation substantially reduced fractures [2], but early work with vitamin D alone was more disappointing [3].
In 2003, Trivedi et al. examined 2,686 (3.1 males: 1 female) community living doctors aged 65–85 years for the effect of D3 (colecalciferol) on the rate of fracture. This study reported that four-monthly 100,000 IU oral vitamin D3 supplementation prevented fractures [4]. However, other recent studies and meta-analyses have not given a clear answer as to the effectiveness of vitamin D [4–9].
The most recent systematic review identified a need for further studies of vitamin D supplementation alone in “very high risk populations, such as people in nursing homes” [8].
Vitamin D3 (colecalciferol) is only available in the UK in tablets combined with calcium. This markedly increases the cost and requires a daily dosage that is less attractive to patients. We therefore used the same low cost four-monthly oral approach as the Trivedi et al. study, but used vitamin D2 (ergocalciferol) which is available as 1.25 mg, 50,000 IU tablets [4].
We report the results of a randomised, placebo controlled trial among older people living in care homes and sheltered accommodation complexes (purpose designed apartments for the elderly with warden supervision).
Methods
Study population
All residents, including those with mobility, cognitive, visual, hearing or communication impairments living in nursing homes, residential homes and sheltered housing were invited to participate in the study. We only excluded people already receiving ≥400 IU of vitamin D/day and those already known to have contraindications to vitamin D supplementation.
Recruitment and randomisation
In 1999 there were 30,709 nursing and residential home beds in Wales. Members of the study team approached care homes across South Wales. Following consent or assent from relatives or significant care givers for those with cognitive dysfunction, participants were randomised individually within blocks in homes to obtain equal numbers in intervention and placebo groups. Randomisation sequences were computer generated by the central dispensing pharmacy. Dosing was supervised by the research nurse to ensure adherence, but nurse, participant and analysts were blinded to allocation.
Sample size calculation
Sample size calculations suggested two groups of 4,000 would yield an 82% power (α = 0.05) for detecting a fracture reduction from 20% to 17.5% after 3 years. However, funding difficulties arising during the study meant that we could only recruit 3,440 people (2,624 women). Ages ranged from 62–107 (mean 84) years: 38% lived in residential homes, 55% in nursing or dual-registered care homes and 7% in sheltered accommodation.
Intervention
Participants took two 1.25 mg vitamin D2 tablets (ergocalciferol) or matched placebo three times a year (i.e., 100,000 IU, four-monthly) for three years. Dosing was supervised by the research nurse to record adherence.
Endpoint ascertainment
All participants were followed up between 1999 and 2004 with a research nurse visiting their residence. The primary outcome measure was the incidence of first fracture, analysed on an intention-to-treat basis. These data were obtained from care home visits, cross-checked with care home injury records, and by matching address, date of birth, NHS numbers of patients with similar data held in our All Wales Injury Surveillance System (AWISS), accident and emergency department attendance database [10] and the Patient Episode Database Wales [PEDW] database of hospital admissions [11].
Secondary outcome measures were the incidence of hip fractures, fractures at common osteoporotic sites (hip/wrist/forearm/vertebrae), and mortality rates.
The modest funding for this pragmatic trial precluded before and after measurement of biochemical and endocrine changes. In the second half of 2003, we obtained additional funds to approach all subjects from 20 participating homes in the Swansea area who had received at least five doses of vitamin D or placebo.
Blood samples were taken from the first 102 who agreed to be tested. These were tested for serum 25(OH)D (DiaSorin radioimmunoassay) and PTH (Nichols Advantage Intact PTH chemiluminescence immunoassay).
Fractures were confirmed by matching every participant with computerized health records and searching through emergency department and in-patient records for all participants. All significant fractures in this setting are treated in hospital and be detected by this means. Not all people who fall attend hospital and so we would undercount falls using this mechanism. Consequently falls were not used as an outcome measure.
Statistical analysis
Data were analysed using Kaplan-Meier (time to first fracture) and Cox regression. Censored observations correspond to the end of the follow-up period without fracture or lost to study (i.e., death or moved home). Length of follow-up was calculated from date of the first tablet to date of first fracture for cases. Randomisation achieved virtually perfect matching of baseline characteristics for intervention and control groups (Table 1). There were some imbalances in the characteristics of the 102 who participated in the biochemical assays and regression analysis was used to compare PTH and 25(OH)D levels between intervention and control groups, adjusted for baseline differences in age and gender.
Results
A total of 497 residential or nursing homes, or sheltered accommodation complexes were approached to enter the study. Approximately 20% declined participation or did not reply to information regarding participation. Due to changes in method of funding the care system at the beginning of the study, many participants who did give consent were not randomised to participate in the study as homes closed and participants were moved within short notice and therefore lost to the study.
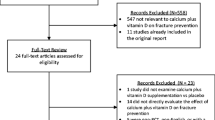
Promised funding from additional sponsors was withdrawn due to financial pressures and reorganisations within the National Health Service. This meant that we were only able to recruit in the south Wales area rather than across Wales. A total of 3,440 people were recruited between December 2000 and January 2003, which equates to 60% of the possible 5,745 subjects living in participating care homes. The mean age of participants was 84 years, and 2,724 (76%) were women. Table 1 shows baseline characteristics and Fig. 1 shows the recruitment profile.
Among the intervention group there were 205 first fractures during 2,846 person years of follow-up; (annual incidence of 7.15%), and 218 first fractures during 2,860 person years (annual incidence of 7.6%) in the control group. The hazard ratio for intervention compared to control was 0.95 (95% CI: 0.79–1.15, p > 0.05). For those who suffered a fracture, the median time to first fracture in the intervention group was 387 days (IQR: 220–582), and 367 days (IQR: 139–618) in the control group (Fig. 2).
There was no significant difference between intervention and control groups if analysis was restricted to fractures occurring at the hip, wrist, forearm, and spine (HR: 1.0, 95% CI: 0.8–1.3), or only hip fractures (HR: 1.1, 95% CI: 0.8–1.1). Overall, 55% of the participants died during the study period, but there was no significant difference between intervention and control in mortality rates [HR: 1.0 (95% CI: 0.9–1.1)].
The research nurses visited each nursing home and gave the participants the medication/placebo. Adherence among participants in the study was 80% overall (percentage of occasions observed to take tablets whilst in the study). Reasons that some participants were not dosed include the following: patient too ill, refused, in hospital, vomited or spat out on repeated occasions. Participants were recorded as not eligible for dosing if they had died or moved.
In the subset of 102 subjects who underwent biochemical testing, mean serum 25(OH)D were 80.1 nmol/l in the intervention group and 54.0 nmo/l in controls; yielding a difference of 26.1 nmol/l (95%CI: 16.6–35.5 nmol/l). After adjustment for age and sex, the mean difference was 23.3 nmol/l (95% CI: 13.8–32.7 nmol/l). After excluding one extremely high value in the control group, we found that mean PTH levels were 5.00 pmol/l in the intervention group and 6.65 pmol/l in the control group (a difference of 1.65, 95%CI: 0.54–2.74). After adjustment for age and sex, the mean difference was 1.42 pmol/l (95%CI: 0.33–2.52).
There was no suggestion of a significant difference in fracture incidence between intervention and control groups in subgroup analyses, stratified by type of care home, mobility, cognitive function or visual acuity (data not shown).
Discussion
Fracture reduction
We found no evidence that four-monthly supplementation with 100,000 IU of oral vitamin D2 is sufficient to substantially affect fracture incidence among older people living in institutional care. Our study recorded 423 fractures in 3,440 individuals making it the second largest in the world to date. Even with this number of fractures it was underpowered, as were a number of previous trials, even though some of these reported positive results. Our non-significant 5% reduction in fractures has confidence intervals compatible with a 21% reduction or a 15% increase. Undoubtedly the less than anticipated recruitment rate reduced the power of our study and increased these confidence intervals, but confirmation of an effect of this magnitude (an annual fracture rate of 7.2%, compared to 7.6% in controls) would have required a study of 89,000 subjects, with a 90% power and significance level of 5%.
Putting the results of our study into context with the other published vitamin D supplement studies is quite difficult as the studies vary in many factors, including the type and setting for participants, their baseline vitamin D and calcium status, and the type and dose of vitamin D used. It is difficult to separate these variables between studies. We have attempted to discuss each factor separately but in many cases simultaneous consideration of several factors is essential.
Our findings are consistent with those recently reported by Law et al. in a cluster randomised study of a similar approach to vitamin D2 supplementation among UK care home residents [9]. They are also in agreement with Anderson et al. [12] which used injected D2, but contrast with the results of two other D2 studies, Heikinheimo et al. [13] and Flicker et al. [14]. Our findings also agree with several D3 studies [5, 6] but are in contrast to the Chapuy et al. and Trivedi et al. studies [2, 4]. The latter study of vitamin D3 in community dwelling older people, reported a 22% reduction in fractures, and achieved significance despite their lower power, with only 268 fractures occurring during follow-up [4].
Differences between our results and those of the Trivedi study and other vitamin D trials could reflect differences in the dose and type of vitamin D used, differences in the study population, or could simply be a chance finding with modest sample sizes.
Dose of vitamin D
The dose of vitamin D used is clearly relevant [14], and a meta-analysis has suggested that a minimum daily dose of 800 IU might be required to affect fracture incidence [7]. We employed the equivalent of 822 IU of vitamin D per day, and this together with the larger sample size and greater number of fractures should have been sufficient for us to be able replicate the effect on fracture incidence of the Trivedi study.
Underlying vitamin D deficiency
Despite being underpowered, we recorded more fractures, with 423 compared to 385 in the Chapuy et al. study[2]. Their controls showed a much greater degree of vitamin D deficiency, with mean 25(OH)D levels of 27.5 nmol/l. This contrasts with 54 nmol/l in the controls of our study, a finding that is very similar to the mean 25(OH) D level of 59 nmol/l reported by Law et al. [9].
The more dramatic difference in 25(OH)D levels between the intervention and control arms of the Chapuy trial (281% higher in their intervention arm, compared with only 48% higher in our trial) may explain their more marked effect in suppressing PTH levels, and in preventing fractures [2]. The relatively high levels of vitamin D in our controls is surprising, given their institutionalised setting, and may explain the lack of efficacy of the vitamin D in our study. However, neither we not the Trivedi study used a random sample of people to test the effectiveness of the intervention on biochemical parameters. In our study patients who underwent biochemical assessment had to have survived to take at least 5 doses and had to have the cognitive ability to consent to a blood test. Therefore, this small sub-sample cannot be claimed to be representative of the entire study population. However, the study did show noteworthy differences between the intervention and control groups, which makes it very likely that the supplements did change 25(OH)D and PTH levels in those receiving at least 5 doses.
Study population
Our population was also more frail than those in studies of community dwelling individuals. Fracture risk will be higher in frail, mobile individuals than in those who are either very active or totally immobile. The Chapuy study [2] recruited older, female care home residents, making it the most similar large scale study to our study. Even so, our subjects were not entirely comparable to the Chapuy study subjects, who had to be mobile and not cognitively impaired. Many of our subjects were less mobile than this, but we found very little difference in the overall fracture risk between groups stratified by initial mobility status, and no suggestion of a beneficial effect of vitamin D in any subgroup. The participants in the Flicker study were also comparable to ours, and vitamin D supplementation was associated with a non-significant reduction in fractures of similar size to the significant reduction in falls [14].
Calcium supplementation
The Chapuy et al. study also differs in that the intervention arm of their study provided 1.2 g of elemental calcium [2]. The inclusion of 500 mg calcium supplementation also appeared effective in the Dawson-Hughes study of community dwelling older people [15]. However, other studies including 1.0 g calcium supplementation have not shown positive results. The Jackson (WHI) study [16] was negative, though it only used 400 IU of vitamin D3, as was the Porthouse et al. study, which used 800 IU vitamin D3 [5]. The RECORD study [6] used 800 IU D3 in older community dwelling individuals who had suffered osteoporotic fracture and was uniformly negative, but was limited by a 46% compliance rate.
Dietary calcium intakes may be important in determining whether subjects will respond to vitamin D supplementation [17], but the size and funding of our study precluded any attempt to quantify dietary calcium intake among participants. As with all very large individually randomised trials, there would be expected to be equal distributions of calcium intake between intervention and control arms of the study, as occurred in the Chapuy et al. study [2], and differences in calcium intake should not be an issue in comparing the two arms of our study for fracture rate.
Effect of D2 compared to D3 on 25(OH)D levels
We used vitamin D2 (ergocalciferol) rather than D3. Some clinical trials that have tested the potency of D2 and D3 have found that serum increase in 25-hydroxyvitamin D with D2 are 3 fold lower than with D3 [18, 19]). Harris et al. [20, 21] showed that the increase in 25-hydroxyvitamin D with age is impaired with D2, while with D3 increase is independent of age. However, there are other studies which show D2 to be effective in raising 25(OH)D levels. In a pilot study we have demonstrated D2 to be effective in increasing (25(OH)D) concentration and suppressing secondary hyperparathyroidism [22]. In addition, two studies have confirmed the biochemical efficacy of high dose oral vitamin D2 in the frail elderly [23] and in Asian immigrants [24]. In these studies, once or twice yearly vitamin D2 resulted in significant prolonged rises over several months in 25(OH)D concentrations.
Our study was not designed to evaluate the effect of supplementation on biochemical parameters, but our analysis in 102 subjects did show a substantial difference in vitamin D levels after adjustment for baseline differences. Indeed our 48% difference was slightly larger than the 39% difference reported in the Trivedi study using equivalent doses of D3 [4]. Furthermore, we showed a significant suppression of PTH levels that they did not achieve.
Other work using vitamin D2 includes a recent study of falls and fracture prevention in 625 older people in residential care in Australia by Flicker et al., which reported a statistically significant 27% reduction in the incidence of falls, and a non-significant 31% reduction in fractures among the intervention group [14]. Their study was powered to detect a change in the proportion falling, but not a change in fracture rates and only included 70 fracture events. Their intervention used a slightly higher dose of vitamin D2 (initially 10,000 IU weekly, then 1,000 IU daily) along with calcium supplementation, but its effect on falls incidence would lend support to belief in the biological activity of vitamin D2.
The recent study of vitamin D2 in UK care homes by Law et al. [9], demonstrated a very similar pattern of biochemical response to vitamin D2 to that we achieved; with a rise in 25(OH)D and suppression of PTH that did not lead to reduction in fracture rates. The only other published studies of vitamin D2 supplementation employed annual intramuscular injection of 300,000 IU. One early study [13] had suggested potential benefit but was underpowered, and a much larger recent study has failed to demonstrate any effect in reducing fracture rates among older people [12].
Two further large scale trials of vitamin D3 supplementation have recently been published, both of which had slightly more fractures in the intervention groups [5, 6]. Their inclusion in the most recent systematic review has cast doubt on the effectiveness of vitamin D supplementation alone for fracture prevention [8]. This led the review to conclude that there remained a need for further studies of vitamin D supplementation in “very high risk populations, such as people in nursing homes”; a need that our work has helped to address.
Carrying out such studies in care home populations is a difficult task with many people unable to give individual consent due to cognitive impairment and assent being required from relatives. Despite these difficulties our study included 60% of the population in care homes. Most of the other studies included highly motivated sub-samples of the population living independently. For example, the Porthouse et al. study had a recruitment rate of only 7% and the Trivedi et al. study only randomised 24% of those invited to participate [4, 5].
In summary: Though small, a 5% reduction in fractures would still be cost-effective given the cheapness of this approach to vitamin D supplementation (around £1 per person per year) but this could only be proven by a very large trial. Given the difficulties of recruiting individuals to such studies, the loss of participants due to death and movement of homes, and lack of funding to support these very large non-pharmaceutical industry trials, the feasibility of running such huge trials must be seriously questioned. Perhaps the best method of scientific progress would be to combine the results of these underpowered trials in an individual level meta-analysis, taking into account differences in type of vitamin D, dosage and populations studied. This might indicate whether any particular group or approach warrants further study, in what would almost certainly need to be a multi-national study.
Conclusion
We found no persuasive evidence that supplementation with 2.5 mg (100,000 IU) of vitamin D2 four-monthly significantly reduces fractures in institutional care residents. This finding contrasts with the results of some previous studies. Differences in results in this group may still be due to differences in the subject populations and their responses to supplemental vitamin D, or from chance due to a lack of statistical power.
There is a need to carry out an individual level meta-analysis across all studies to determine whether there are particular subgroups in which vitamin D supplementation is effective and to determine whether further studies are required. In the meantime vitamin D supplementation cannot be advocated as a public health approach to fracture prevention in care home populations.
Registration
National Research Register No: MOO48086119.
References
Brennan nee Saunders J, Johansen A, Butler J, Stone M, Richmond P, Jones S et al (2003) Place of residence and risk of fracture in older people: a population-based study of over 65-year-olds in Cardiff. Osteoporos Int 14(6):515–519
Chapuy MC, Arlot ME, Duboeuf F, Brun J, Crouzet B, Arnaud S et al (1992) Vitamin D3 and calcium to prevent hip fractures in the elderly women. N Engl J Med 327(23):1637–1642
Lips P, Graafmans WC, Ooms ME, Bezemer PD, Bouter LM (1996) Vitamin D supplementation and fracture incidence in elderly persons. A randomized, placebo-controlled clinical trial. Ann Intern Med 124(4):400–406
Trivedi DP, Doll R, Khaw KT (2003) Effect of four monthly oral vitamin D3 (cholecalciferol) supplementation on fractures and mortality in men and women living in the community: randomised double blind controlled trial. Bmj 326(7387):469
Porthouse J, Cockayne S, King C, Saxon L, Steele E, Aspray T et al (2005) Randomised controlled trial of calcium and supplementation with cholecalciferol (vitamin D3) for prevention of fractures in primary care. Bmj 330(7498):1003
Grant AM, Avenell A, Campbell MK, McDonald AM, MacLennan GS, McPherson GC et al (2005) Oral vitamin D3 and calcium for secondary prevention of low-trauma fractures in elderly people (Randomised Evaluation of Calcium Or vitamin D, RECORD): a randomised placebo-controlled trial. Lancet 365(9471):1621–1628
Bischoff-Ferrari HA, Willett WC, Wong JB, Giovannucci E, Dietrich T, Dawson-Hughes B (2005) Fracture prevention with vitamin D supplementation: a meta-analysis of randomized controlled trials. Jama 293(18):2257–2264
Avenell A, Gillespie WJ, Gillespie LD, O’Connell DL (2005) Vitamin D and vitamin D analogues for preventing fractures associated with involutional and post-menopausal osteoporosis. Cochrane Database Syst Rev 3:CD000227
Law M, Withers H, Morris J, Anderson F (2006) Vitamin D supplementation and the prevention of fractures and falls: results of a randomised trial in elderly people in residential accommodation. Age Ageing 35(5):482–486
Lyons RA, Jones S, Kemp A, Sibert J, Shepherd J, Richmond P et al (2002) Development and use of a population based injury surveillance system: the all Wales Injury Surveillance System (AWISS). Inj Prev 8(1):83–86
Brophy S, John G, Evans E, Lyons RA (2005) Methodological issues in the identification of hip fractures using routine hospital data: a database study. Osteoporos Int
Anderson F (2004) Effect of annual intramuscular vitamin D supplementation on fracture risk in 9,440 community living older people: the Wessex Fracture Prevention Trial. ASBMR abstract 1220
Heikinheimo RJ, Inkovaara JA, Harju EJ, Haavisto MV, Kaarela RH, Kataja JM et al (1992) Annual injection of vitamin D and fractures of aged bones. Calcif Tissue Int 51(2):105–110
Flicker L, MacInnis RJ, Stein MS, Scherer SC, Mead KE, Nowson CA et al (2005) Should older people in residential care receive vitamin D to prevent falls? Results of a randomized trial. J Am Geriatr Soc 53(11):1881–1888
Dawson-Hughes B, Harris SS, Krall EA, Dallal GE (1997) Effect of calcium and vitamin D supplementation on bone density in men and women 65 years of age or older. N Engl J Med 337(10):670–676
Jackson RD, LaCroix AZ, Gass M, Wallace RB, Robbins J, Lewis CE et al (2006) Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med 354(7):669–683
Boonen S (2006) Fracture risk reduction with vitamin D supplementation requires additional calcium: evidence from a comparative meta-analysis. Osteoporos Int 17(Supp 2):13
Armas LA, Hollis BW, Heaney RP (2004) Vitamin D2 is much less effective than vitamin D3 in humans. J Clin Endocrinol Metab 89(11):5387–5391
Trang HM, Cole DE, Rubin LA, Pierratos A, Siu S, Vieth R (1998) Evidence that vitamin D3 increases serum 25-hydroxyvitamin D more efficiently than does vitamin D2. Am J Clin Nutr 68(4):854–858
Harris SS, Dawson-Hughes B, Perrone GA (1999) Plasma 25-hydroxyvitamin D responses of younger and older men to three weeks of supplementation with 1800 IU/day of vitamin D. J Am Coll Nutr 18(5):470–474
Harris SS, Dawson-Hughes B (2002) Plasma vitamin D and 25OHD responses of young and old men to supplementation with vitamin D3. J Am Coll Nutr 21(4):357–362
Grey J et al (1998) Secondary prevention of hip fracture: developing a simple protocol for trauma wards. Age Aging 27(Supp 2):19–20
Davies M, Mawer EB, Hann JT, Stephens WP, Taylor JL (1985) Vitamin D prophylaxis in the elderly: a simple effective method suitable for large populations. Age Ageing 14(6):349–354
Stephens WP, Klimiuk PS, Berry JL, Mawer EB (1981) Annual high-dose vitamin D prophylaxis in Asian immigrants. Lancet 2(8257):1199–1202
Acknowledgements
We would like to thank the trial participants, proprietors of nursing and residential homes and Age Concern Cymru for their participation and support for this study. The study was funded by the Wales Office of Research and Development for Health and Social Care - grant number R99/1/055.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lyons, R.A., Johansen, A., Brophy, S. et al. Preventing fractures among older people living in institutional care: a pragmatic randomised double blind placebo controlled trial of vitamin D supplementation. Osteoporos Int 18, 811–818 (2007). https://doi.org/10.1007/s00198-006-0309-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-006-0309-5