Abstract
Introduction
Older patients with fragility fractures are not commonly tested or treated for osteoporosis. Compared to usual care, a previously reported intervention led to 30% absolute increases in osteoporosis treatment within 6 months of wrist fracture. Our objective was to examine longer-term outcomes, reproducibility, and cost-effectiveness of this intervention.
Methods
We conducted an extended analysis of a non-randomized controlled trial with blinded ascertainment of outcomes that compared a multifaceted intervention to usual care controls. Patients >50 years with a wrist fracture treated in two Emergency Departments in the province of Alberta, Canada were included; those already treated for osteoporosis were excluded. Overall, 102 patients participated in this study (55 intervention and 47 controls; median age: 66 years; 78% were women). The interventions consisted of faxed physician reminders that contained osteoporosis treatment guidelines endorsed by opinion leaders and patient counseling. Controls received usual care; at 6-months post-fracture, when the original trial was completed, all controls were crossed-over to intervention. The main outcomes were rates of osteoporosis testing and treatment within 6 months (original study) and 1 year (delayed intervention) of fracture, and 1-year persistence with treatments started. From the perspective of the healthcare payer, the cost-effectiveness (using a Markov decision-analytic model) of the intervention was compared with usual care over a lifetime horizon.
Results
Overall, 40% of the intervention patients (vs. 10% of the controls) started treatment within 6 months post-fracture, and 82% (95%CI: 67–96%) had persisted with it at 1-year post-fracture. Delaying the intervention to controls for 6 months still led to equivalent rates of bone mineral density (BMD) testing (64 vs. 60% in the original study; p = 0.72) and osteoporosis treatment (43 vs. 40%; p = 0.77) as previously reported. Compared with usual care, the intervention strategy was dominant – per patient, it led to a $13 Canadian (U.S. $9) cost savings and a gain of 0.012 quality-adjusted life years. Base-case results were most sensitive to assumptions about treatment cost; for example, a 50% increase in the price of osteoporosis medication led to an incremental cost-effectiveness ratio of $24,250 Canadian (U.S. $17,218) per quality-adjusted life year gained.
Conclusions
A pragmatic intervention directed at patients and physicians led to substantial improvements in osteoporosis treatment, even when delivered 6-months post-fracture. From the healthcare payer’s perspective, the intervention appears to have led to both cost-savings and gains in life expectancy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Osteoporosis is a chronic and progressive condition that leads to decreased bone mass and skeletal fragility; in turn, this leads to fractures, disability, pain, deformity, and even death [1–6]. It is a common condition, with about 25% of all women and 12% of all men over the age of 50 years affected [1–4]. The annual cost of treating osteoporosis and its sequelae has been estimated at 13.8 billion dollars in the USA, compared with 7.5 billion dollars for heart failure or 6.2 billion dollars for asthma [3]. Unless effective preventive strategies are implemented, the rate of osteoporotic fractures is expected to double over the next 15 years [5].
One useful preventive strategy is to identify people with typical osteoporosis-related fractures (e.g., of the wrist, spine, or hip, often referred to as fragility fractures) and target them for intervention, because this population is at high risk of subsequent fracture and derives the greatest absolute benefit from treatment [3–6]. “Best practice,” that is clinical practice consistent with the evidence and expert consensus, would be to identify older adults with a fragility fracture, determine those at risk for more fractures, and institute preventive measures. Based on our current data, a reasonable strategy would be to measure their bone mineral density (BMD) and treat those with low bone mass. There is, however, a care gap between best practice and day-to-day usual care. For example, most studies report rates of less than 10–20% for testing and treatment of osteoporosis in the 6–12 months following a fracture of the wrist [3–9].
We previously reported the results of a controlled trial of a pragmatic osteoporosis quality improvement intervention directed at older patients with a fracture of the wrist and their primary care physicians [5]. The intervention consisted of physician reminders, local opinion leader endorsed treatment guidelines, and patient education. Compared with usual care, this intervention led to a 45% absolute increase in BMD testing (p value <0.001) and a 30% increase in osteoporosis treatment (p value = 0.002) within 6 months of fracture [5]. Despite these promising results, three questions are asked (but rarely answered) of this and most other quality improvement strategies tested in one-off intervention studies [10, 11]: (1) Did patients continue treatment after the study was finished (“persistence”); (2) Can the results be replicated in different patients (“reproducibility”); (3) Is the intervention worthwhile compared to usual care (“cost-effectiveness”)? To answer these questions, we extended our study results to include a follow-up of all patients up to 1 year, provided the intervention to all control patients at the end of the study proper (6 months post-fracture), and conducted a cost-effectiveness analysis from the perspective of the healthcare payer that would eventually need to make the policy decision to adopt our intervention on a wider scale [11].
Methods
Description of the original study
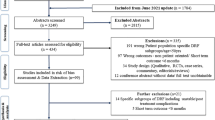
The main study has been described in detail and published [5]. Briefly, we conducted a nonrandomized controlled trial with blinded ascertainment of outcomes that compared our intervention to usual care. The study was conducted at two Emergency Departments in Capital Health (Edmonton, Alberta), the largest integrated health service delivery organization in Canada, with a population of approximately one million people cared for by approximately 1000 primary care physicians. The study took place from January 2001 through September 2002. Overall, 102 consecutive patients 50 years of age or older presenting to the Emergency Department with a fracture of the wrist were included (Table 1); we excluded those already treated for osteoporosis. Rather than randomization, we allocated patients to intervention (n = 55) or control (n = 47) using a monthly “on-off” time series, whereby allocation to experimental arms was based on month of fracture and site of treatment. Outcomes were collected, in an independent and blinded fashion, 6 months after study entry. At the end of the original study, all controls received the intervention, and all study patients had outcomes re-collected 6 months later (i.e., 1 year post-fracture).
Outcomes
The primary study outcome was starting an osteoporosis-indicated prescription medication (bisphosphonates, raloxifene, calcitonin, or hormone therapy) within 6 months of fracture. It was measured by patient self-report and confirmed by pharmacy dispensing records; there was a 100% agreement between the two data sources [5]. The main secondary outcome was receipt of a BMD test. Outcomes were collected at 6 months (original study) and 1 year (extension study), without knowledge of allocation status. We had 100% follow-up for medications and BMD tests, and 75% of patients completed all 3-, 6-, and 12-month telephone follow-up visits and surveys. All patients were analyzed according to the experimental groups to which they were first assigned.
Cost-effectiveness analysis
We hypothesized that our intervention would be cost effective when compared with usual care. Our trial provided data about the population at risk, effects of the intervention, rates of osteoporosis testing and treatment across experimental arms, 1-year persistence with treatment, and health resource use related to wrist fracture. We used a deterministic decision analysis model incorporating Markov processes [12–14] to simulate the osteoporosis experience of a cohort of 100 women with wrist fractures similar to those in our trial but followed over the rest of their lifetime. Cost effectiveness was analyzed by estimating incremental cost-effectiveness ratios based on quality-adjusted life years (QALYs) gained [12–14]. Costs were reported from the healthcare payer perspective, acknowledging that Canadians have universal healthcare coverage that includes prescription medications for this age group. All decisions and assumptions related to model inputs (described below) reflected a generally conservative approach – that is, to err on the side of not accepting the study hypothesis.
Figure 1 illustrates the six unique osteoporosis-related diagnosis and treatment pathways into which patients could be grouped. The proportion of patients within each group (see Appendix 1) was calculated by multiplying the probabilities along each pathway, and the probabilities for the initial distribution of patients were from our trial. A Markov process, through which costs and outcomes were modeled, was associated with each of these groups [12–14]. There were three unique Markov processes differentiated by their transition probabilities (Fig. 1): low bone mass patients receiving osteoporosis treatment (M1), low bone mass patients not receiving treatment (M2), and normal bone mass (M3).
Decision tree of the model with Markov processes. Probabilities associated with the intervention and control arms of the study are denoted by p I and p c , respectively. BMD Bone mineral density, LBM low bone mass, NBM normal bone mass, Rx treatment with alendronate. M1, M2, and M3 refer to the individual Markov processes; also see Methods and Fig. 2
The structure of the Markov process, shown in Fig. 2, was adapted from previous work by Johnell and colleagues [12] and incorporates six health states. The model simulates the movement of a cohort of 100 women, from age 66 until 100 years or death, whichever occurs first. All patients begin in the well state at home, following their fragility fracture of the wrist. Once per annual cycle, a proportion of the cohort moves to one of the other five states, in accordance with pre-specified transition probabilities. These probabilities were derived from fracture rates specific to the type of fracture incurred, presence of low bone mass, age-specific death rates and, for patients receiving osteoporosis treatment, fracture type-specific reductions in the risk of future fractures.
Structure of the Markov process (adapted from Johnell and colleagues [12]). There are potential transitions from each health state to the Death state that are not shown in the figure for purposes of clarity
We made a number of broad simplifying assumptions. Because of the absolute paucity of data related to osteoporosis treatments and outcomes for men (22% of our study cohort), our models included only women. Wrist fracture patients were considered to have low bone mass (based on measurements of either osteopenic or osteoporotic BMD derived from our trial) or normal bone mass. Alendronate was considered to be the medication prescribed to all patients receiving treatment because in our original study, only one patient who was treated for osteoporosis received any other treatment (this patient inhaled calcitonin); everyone else was prescribed 70 mg per week of alendronate. In addition, it was assumed that once a patient had a hip fracture, no additional wrist or spine fractures occurred, although repeat hip fractures were permitted. Last, only the Death state was defined as “absorbing.”
Model inputs
Fracture rates
Fracture rates were type-specific and assumed to be constant with respect to age. Each type-specific fracture rate was estimated by multiplying U.S. general population rates by the relative risk of recurrent fracture. For example, the annual rate of 0.68% for hip fracture following wrist fracture (Appendix 2) was calculated as the product of 0.36% (annual rate of hip fracture in the U.S. population) and 1.9 (relative risk of hip fracture, given a prior wrist fracture). We used published U.S. population type-specific annual fracture rates [12] and relative risk estimates from a systematic review and meta-analysis [15]. Fracture rates for low bone mass patients not treated for osteoporosis are presented in Appendix 2. Because the risk of a second and subsequent hip fracture is much higher than that for the first hip fracture, we used actual fracture rates reported in a large Canadian cohort study [16]. We could not find re-fracture rates for patients with normal bone mass, and so considered them to have the same rates as low bone mass patients taking alendronate.
Reductions in fracture risk with treatment
Estimates of a reduction in fracture risk with alendronate were obtained from a series of systematic reviews conducted by Cranney et al. [17]. Alendronate was associated with a 49% relative reduction in the risk of hip and spine fractures, and a 48% reduction for wrist fractures [17]. Risk reduction was assumed to be constant with respect to age. In the base case analysis, alendronate treatment was for a 5-year duration. In the first year of treatment, the beneficial effect of alendronate was assumed to be 50% of the full achievable benefit. However, a further residual positive effect of alendronate treatment was also assumed to occur for an additional 5 years following discontinuation [18, 19]. This residual beneficial effect was assumed to decline at a linear rate over the 5-year “set time” following the discontinuation of treatment [18, 19]. In our study, overall 1-year persistence with osteoporosis treatment was about 80% (see Results); we assumed this would continue to be the case for the next 4 years. It was also assumed that the 20% of patients who discontinued treatment did so in the first year and that they received no fracture reduction benefits whatsoever.
Costs
All costs were expressed in constant 2004 Canadian dollars. In the base case analysis, all costs and outcomes were discounted at a rate of 3% per annum after the first year [14]. The one-time cost of the intervention [identifying eligible patients and producing and delivering physician and patient materials (6 min of clerical time = $2.84 per patient), patient counseling (4 min of nursing time = $4.41 per patient), and facility overhead (33% = $2.39)] was based on time-motion studies performed for ten study patients and amounted to $9.64 (rounded to $10 in all calculations). It should be noted, however, that the time, expertise, and influence of our opinion leaders was provided to us at no cost and thus not included as part of the “intervention” costs. Based on the totality of the opinion leader literature, we believe that such would be the case in any setting attempting to harness their local opinion leaders to improve the quality of care [20]. The one-time cost of providing a BMD test with a physician visit was $199 [21].
-
Costs of osteoporosis treatment: As mentioned above, one patient did receive calcitonin, but all others received alendronate at 70 mg per week. For clarity and consistency, we assumed for the cost-effectiveness analysis that all patients would receive alendronate for the duration of treatment. The provincial drug plan covers the generic form of alendronate for elderly persons who have had a fragility fracture [22]. Total annual cost of medication and one annual physician visit related to osteoxporosis were estimated at $573 per patient [21, 22]. As have others, we assumed alendronate would generate only trivial direct medical costs related to side-effects [14]. Patients who discontinued treatment in the first year were assumed to incur the full treatment costs for that year.
-
Costs of subsequent fractures: Table 2 summarizes estimated annual costs for the health states related to treatment of subsequent hip, spine, or wrist fractures. Cost estimates were based on data relating to use of health services and unit values obtained from regional [23] or national [24] databases. Fees for all physician services were obtained from the Alberta fee schedule [21].
-
We assumed the hip fracture state would require surgical fixation and a 16-day hospital stay, based on Canadian hospitalization records [24]. A case-mix method was used to estimate inpatient hospital costs, based on relative resource weights and the Alberta average cost per weighted case [23, 24]. Orthopedic surgeon and internist costs were based on one visit each per day. It was assumed that 80% of the patients were discharged home after hip fracture and 20% to long-term care facilities; costs of long-term care were based on standard Alberta per diem [23].
-
We only considered clinically symptomatic spine fractures in our analyses, although it is known that “silent” fractures contribute to morbidity and mortality [1–4]. Only 10% of patients with a symptomatic fracture of the spine were assumed to require inpatient care. Hospital costs were estimated in similar manner as hip fractures, with daily internist visits for an average stay of 15 days [24]. Following discharge, nine follow-up physician visits and one spinal radiograph were assumed. The 90% of spine fracture patients not hospitalized had two physician visits and one spinal radiograph. Patients received seven visits of outpatient rehabilitation.
-
In our study cohort, all patients experiencing a wrist fracture presented to an Emergency Department for treatment, and in general had one closed fracture reduction procedure, two physician follow-up visits, and one follow-up wrist radiograph. Patients with a wrist fracture received seven outpatient rehabilitation visits.
Mortality rates
Patients were assumed to have the same risk of death as the general population, except in the year following a hip fracture. The 1995–1997 provincial life tables were the source of age-specific death rates for the general source population [25]. Age-specific rates of death for the first year following hip fracture were obtained from previous estimates used by Johnell and colleagues [12]; aggregated, these rates are very similar to those previously published from our health region [26].
Health-related quality of life
The age-specific quality of life weights for each health state that we used had also been previously estimated and published by Johnell and colleagues [12] and are shown in Appendix 3. The state with the lowest weight, other than Death, is Hip Fracture. Conversely, the Well state (following the original wrist fracture) has the highest quality of life.
Sensitivity analyses
Conventional one-way deterministic sensitivity analyses were conducted to evaluate the robustness of the model with respect to the following key parameters: intervention costs ($20 and $50, rather than $10 in the base case); the rate of treatment persistence (50%, rather than 80%), the risk of re-fracture for patients with normal bone mass (50% of the base case rather than equal to the rate of those who have low bone mass and were treated with alendronate), osteoporosis treatment costs (increased by 50% over the base case costs of alendronate), the duration of osteoporosis treatment (10 years, rather than 5 years), and the discount rate for costs and outcomes (0 and 5%, rather than 3% in the base case). We also considered a “worst-case” and “best-case” multi-way sensitivity analysis that varied intervention costs, treatment costs, and treatment duration simultaneously.
Results
The study patients were elderly (median age: 66 years; range: 50–96 years) and 78% were women. By design, none were taking osteoporosis treatment at study entry, although 70% reported a fracture before their study-qualifying wrist fracture. Other baseline characteristics of intervention and control patients are presented in Table 1. Of note, of the 67 patients that had a BMD measured during the study, 20 (30%) had normal bone mass.
Persistence with osteoporosis treatment
Of the 22 intervention patients that started osteoporosis treatment within 6 months of fracture in the original study, 18 [82%, 95% confidence intervals (95%CI): 67–96%] were still filling their prescriptions at 1 year post-fracture; all were taking bisphosphonates. Of those who responded to survey items about adherence at 1 year (14/18), all reported taking 75% or more of their osteoporosis medication as prescribed.
Reproducibility of the intervention effect
Our main results are illustrated in Fig. 3. Within 6 months of wrist fracture, the original intervention led to a rate of BMD testing of 60% (33/55) and a rate of osteoporosis treatment of 40% (22/55); the corresponding rates of testing and treatment for the controls were 17 (8/47) and 10% (5/47). Six months after delayed exposure to the intervention, however, former controls had a rate of BMD testing of 64% (95%CI: 50–78%) and a rate of osteoporosis treatment of 43% (95%CI: 28–57%). The within-control group differences before and after exposure to the intervention for BMD testing (p < 0.001 by McNemar’s test) and osteoporosis treatment (p = 0.002) were statistically significant. On the other hand, there was no difference in effectiveness of the intervention whether it was delivered at the time of the fracture or after a 6-month delay (p = 0.72 for BMD testing and p = 0.77 for treatment).
Rates of osteoporosis testing and treatment at 6 months (original study) and 1 year (extension study). Controls (n = 47) and original intervention (n = 55) refer to the experimental arms of the previously reported study [5]. The 6-month delayed intervention refers to patients that were formerly in the control group (n = 47), with their outcomes re-ascertained 6 months after receiving the intervention
Cost effectiveness of the intervention
The base case analysis is presented in Table 3. Our model suggests that, over their lifetime, patients with a wrist fracture exposed to our intervention would be less likely to incur a subsequent fracture than controls: for every 100 patients, about one hip fracture and four fractures in total would be avoided. There was also an associated increase in quality-adjusted life expectancy (0.012 QALYs gained). Lifetime costs were similar for all patients, although the intervention was associated with a small incremental cost saving of $13 (U.S. $9) per patient. Thus, the quality improvement strategy that we studied was dominant – it cost less and added more QALYs than usual care.
One-way sensitivity analyses, presented in Table 4, suggest that the results of the base case are fairly robust to a variety of assumptions. Although the intervention did incur positive incremental costs in all but two of these sensitivity analyses, in all cases the incremental cost-effectiveness ratios were below $25,000 (U.S. $18,000) per QALY gained. The single parameter that had greatest impact on cost-effectiveness was treatment cost: a 50% increase in the price of alendronate led to an incremental cost-effectiveness ratio of $24,250 (U.S. $17,218) per QALY gained.
In multi-way sensitivity analyses, the worst-case scenario (intervention costs increased from $10 to $50, a 50% increase in osteoporosis medication costs, and 5-year duration of therapy) yielded an incremental cost-effectiveness ratio of $27,583 (U.S. $19,584) per QALY gained. Conversely, compared with the base case analysis, the best-case scenario (intervention costs held at $10, a 50% decrease in osteoporosis medication costs, and an increase in the duration of therapy from 5 to 10 years) yielded a much larger incremental cost saving of $469 (U.S. $333) per patient exposed to the intervention.
Discussion
Despite the wealth of evidence [17–19], the promulgation of guidelines [1, 2], and the exhortations of experts [6], older patients with fragility fractures are not commonly tested or treated for osteoporosis. We previously reported substantial increases in testing and treating for osteoporosis in patients with wrist fractures as a result of a quality improvement intervention directed at both patients and their physicians [5]. We now report that 82% of patients who started osteoporosis treatment persisted with that treatment for 1 year after their fracture. Furthermore, we have shown some degree of reproducibility – delivering the same intervention to different patients (i.e., former controls) at a different point in time (i.e., after a 6-month delay) resulted in equivalent rates of testing and treatment for osteoporosis as the original study. Lastly, we demonstrated that our intervention was cost-effective, even in the broadest sense of efficient resource allocation [11, 27]. Indeed, the base case analysis suggests that it was a dominant strategy, resulting in both a small cost savings and a small gain in life expectancy.
It could be argued that improving the quality of evidence-based testing and treatment of osteoporosis in fragility fracture patients – patients at high risk of future fractures – should be a sufficient end, in and of itself [5]. In fact, the recently validated “Assessing Care of Vulnerable Elders” quality measures (which explicitly include secondary prevention of osteoporosis in fracture patients) recognize this as a guiding principle [28]. Nevertheless, cost-effectiveness analyses also demonstrated that our intervention strategy dominated usual care. Our strategy, or indeed any quality improvement strategy that costs a similar amount per patient (approximately $10) and results in similar rates of osteoporosis testing (approximately 60%) and treatment (approximately 40%), should be attractive from the perspective of a healthcare payer making long-term policy decisions for a given population [11]. Our analyses were most sensitive to assumptions regarding treatment costs – for alendronate, $573 (U.S. $407) per patient per year in the base case. Fortunately, it is more than likely that medication costs will decrease, not increase, over time. For example, as of August 2006, the cost of alendronate treatment in Alberta had already decreased to $377 (U.S. $268) per year.
Several limitations should be considered when interpreting our results. First, our main findings are based on a nonrandomized controlled trial with blinded ascertainment of outcomes. This fact should not, however, influence interpretations related to persistence with treatment or reproducibility of effect. Second, we studied only 102 patients and followed them up for 1 year. We were not adequately powered to detect differences in fracture rates, necessitating the use of a health economic model. As with all such models, the primary limitations are related to assumptions and inputs. In particular, we were dependent on the literature for important parameters, such as the rates of re-fractures, the benefits of alendronate therapy, and the utilities associated with various fracture-related health states. On the other hand, we incorporated primary data on initial testing and treatment patterns and intervention costs from our trial, and utilization and unit cost data from relevant regional and national sources. Still, our model likely underestimates true cost-effectiveness, because most of our assumptions favored the null hypothesis. For example, we ascribed no benefits to reduction in radiographic (i.e., not clinically apparent) vertebral fractures; we did not model the potential effect of preventing a vertebral fracture on subsequent mortality [29, 30]; we did not acknowledge that without treatment patients continue to lose bone mass over time; we did not permit benefits of future non-hip fracture reduction once a hip fracture had occurred; and we did not include expensive but potentially avoidable fracture-related treatments, such as surgical fixation for wrist fractures or kyphoplasty for vertebral fractures. Finally, some might be concerned about the broader generalizability of our results, which were based on a study with a small number of patients with universal health care coverage drawn from one Canadian health region, when trying to implement our intervention strategy in different settings.
In conclusion, we found that a pragmatic quality improvement intervention directed at patients and their physicians led to substantial increases in the testing and treatment of osteoporosis when implemented at any time up to 6 months post-fracture. When modeled from the perspective of the healthcare payer and compared with usual care, the intervention might be expected to eventually lead to a reduction in fractures, a gain in life expectancy, and net cost savings.
References
Physicians’ guide to prevention and treatment of osteoporosis. National Osteoporosis Foundation, 2002 (http://www/nof.org/physguide.html; last accessed on August 1st, 2006)
Scientific Advisory Council, Osteoporosis Society of Canada (2002) 2002 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada. Can Med Assoc J 167[Suppl]:S1–S34
Andrade SE, Majumdar SR, Chan KA, Buist DS, Go AS et al (2003) Low frequency of treatment of osteoporosis among postmenopausal women following a fracture. Arch Intern Med 163:2052–2057
Feldstein A, Elmer PJ, Orwoll E, Herson M, Hillier T (2003) Bone mineral density measurement and treatment for osteoporosis in older individuals with fractures. Arch Intern Med 163:2165–2172
Majumdar SR, Rowe BH, Folk D, Johnson JA, Holroyd BH et al (2004) A controlled trial to increase detection and treatment of osteoporosis in older patients with a wrist fracture. Ann Intern Med 141:366–373
Siris ES, Bilezikian JP, Rubin MR, Black DM, Bockman RS et al (2003) Pins and plaster aren’t enough: a call for the evaluation and treatment of patients with osteoporotic fractures. J Clin Endocrinol Metab 88:3482–3486
Hajcsar EE, Hawker G, Bogoch ER (2000) Investigation and treatment of osteoporosis in patients with fragility fractures. Can Med Assoc J 163:819–822
Cuddihy MT, Gabriel SE, Crowson CS, Atkinson EJ, Tabini C et al (2002) Osteoporosis interventions following distal forearm fractures: a missed opportunity. Arch Intern Med 162:421–426
Eliot-Gibson V, Bogoch ER, Jamal SA, Beaton DE (2004) Practice patterns in the diagnosis and treatment of osteoporosis after fragility fracture: a systematic review. Osteoporos Int 15:767–778
Johnson JA, Eurich DT, Toth EL, Lewanczuk RZ, Lee TK, Majumdar SR (2005) Generalizability and persistence of a multifaceted intervention for improving quality of care for rural patients with type-2 diabetes. Diabetes Care 28:783–788
Mason J, Freemantle N, Nazareth I, Eccles M, Haines A, Drummond M (2001) When is it cost-effective to change the behavior of health professionals? JAMA 286:2988–2992
Johnell O, Jönsson B, Jönsson L, Black D (2003) Cost effectiveness of alendronate for the treatment of osteoporosis and prevention of fractures. Pharmaco-economics 21:305–314
Tosteson AN, Jonsson B, Grima DT, O’Brien BJ, Black DM, Adachi JD (2001) Challenges for model-based economic evaluations of postmenopausal osteoporosis interventions. Osteoporos Int 12:849–857
Schousboe JT, Nyman JA, Kane RL, Ensrud KE (2005) Cost-effectiveness of alendronate therapy for osteopenic postmenopausal women. Ann Intern Med 142:734–741
Klotzbuecher CM, Ross PD, Landsman PB, Abbott III TA, Berger M (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 15:721–739
Wiktorowicz ME, Goeree R, Papaioannou A, Adachi JD, Papadimitropoulos E (2001) Economic implications of hip fracture: health service use, institutional care and cost in Canada. Osteoporos Int 12:271–278
Cranney A, Guyatt GH, Griffith L, Wells G, Tugwell P, for the Osteoporosis Research Advisory Group (2002) Summary of meta-analyses of therapies for postmenopausal osteoporosis. IX. Endocrinol Rev 23:570–578
Tonino RP, Meunier PJ, Emkey RD, Rodriguez-Portales JA, Menkes CJ et al for the Phase III Osteoporosis Treatment Study Group (2000) Skeletal benefits of alendronate: 7-year treatment of postmenopausal osteoporotic women. J Clin Endocrinol Metab 85:3109–3115
Bone HG, Hosking D, Devogelaer JP, Tucci JR, Emkey RD et al for the Alendronate Phase III Osteoporosis Treatment Study Group (2004) Ten years’ experience with alendronate for osteoporosis in postmenopausal women. N Engl J Med 350:1189–1199
Thomson MA, Oxman AD, Haynes RB (2005) Local opinion leaders to improve health professional practice and health care outcomes. The Cochrane Library. The Cochrane Database of Systematic Reviews, Issue 4
Alberta Health Care Insurance Plan (2004) Schedule of medical benefits (procedures and price list). Alberta Health and Wellness, Edmonton, Alberta, Canada
Alberta Health and Wellness (2004) Drug benefits list. Edmonton, Alberta, Canada
Alberta Health and Wellness (2003) Health Costing in Alberta – Annual Report. Edmonton, Alberta, Canada
Canadian Institute for Health Information (2003) Resource intensity weights and expected length of stay. Ottawa, Ontario, Canada
Statistics Canada (2002) Life tables-Canada, provinces and territories, 1995–1997 (84-537-XIE). Ottawa, Ontario, Canada
Jiang HX, Majumdar SR, Dick DA, Moreau M, Raso J et al (2005) Development and initial validation of a risk score for predicting in-hospital and one-year mortality in patients with hip fractures. J Bone Miner Res 20:494–500
Donaldson C, Currie G, Mitton C (2002) Cost effectiveness analysis in healthcare: contraindications. Br Med J 325:891–894
Higashi T, Shekelle PG, Adams JL, Kamberg CJ, Roth CP et al (2005) Quality of care is associated with survival in vulnerable older patients. Ann Intern Med 143:274–281
Cooper C, Atkinson EJ, Jacobsen SJ, O’Fallon WM, Melton LJ 3rd (1993) Population-based study of survival after osteoporotic fractures. Am J Epidemiol 137:1001–1005
Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA (1999) Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet 353:878–882
Acknowledgements
This investigation was supported by grants from the Medical Services Budget Innovation Fund (Alberta Medical Association Medical and Alberta Health and Wellness) and the Alberta Heritage Foundation for Medical Research. Dr. Majumdar is a Population Health Investigator, Dr. Johnson is a Health Scholar, and Dr. Maksymowych is a Senior Scholar, all of the Alberta Heritage Foundation for Medical Research; Dr. Majumdar is a New Investigator of the Canadian Institutes of Health Research; Drs. Rowe and Johnson hold Canada Research Chairs. The authors would like to acknowledge the substantial efforts of other members of the research team – Charles Harley, MD; Brian Wirzba, MD; Debbie Bellerose, RN – who made important contributions to this and earlier work. The authors also thank the Orthopedic Plaster Room Technicians at the University of Alberta Hospital and the Royal Alexandra Hospital for their time and efforts for the study and the Epidemiology Coordinating and Research (EPICORE) Centre of the University of Alberta for providing services related to trial coordination and data management. Finally, the authors dedicate this work to the memory of Deb Folk, RN, our project coordinator, who was not able to see the final study results published. Without her enthusiasm and tireless efforts on our behalf, this study would not have been possible.
Author information
Authors and Affiliations
Corresponding author
Additional information
Role of the funding sources: The study was funded by peer-reviewed grants from the Alberta Medical Association, Alberta Health and Wellness, and the Alberta Heritage Foundation for Medical Research. The funding sources had no role in the design and conduct of the study, the collection, analysis, or interpretation of the data, or the decision to submit the manuscript for publication.
Trial Registry: NCT00175214
Rights and permissions
About this article
Cite this article
Majumdar, S.R., Johnson, J.A., Lier, D.A. et al. Persistence, reproducibility, and cost-effectiveness of an intervention to improve the quality of osteoporosis care after a fracture of the wrist: results of a controlled trial. Osteoporos Int 18, 261–270 (2007). https://doi.org/10.1007/s00198-006-0248-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-006-0248-1