Abstract
Introduction
The present case study compared bone density, bone geometry and muscle cross-sectional area (CSA) in a male who sustained spinal-cord injury (SCI) at birth (from here called SCI-B) with two matched controls without SCI, and also with four individuals with SCI of similar level and injury completeness but sustained at age 15 or greater.
Methods
All subjects with SCI were at least 3 years post-injury and had experienced motor incomplete lesions at the cervical level. Computed tomography was used to measure volumetric bone density, indices of bone strength [CSA and maximum, minimum and polar area moments of inertia (I max, I min, I pol)] and muscle CSA at the tibia (66% of tibia length, measured proximally from the distal end).
Results
Lower leg muscle CSA of SCI-B was 63±6% of values in non-SCI controls, and 72±12% of values in other males with SCI. In SCI-B, bone CSA was roughly half (52±4%) that of non-SCI controls and 73±16% of bone CSA values in other males with SCI. The magnitudes of the area moment of inertia variables (I max, I min, and I pol) in SCI-B were ~25% of control values. Further, the moment of inertia variables in SCI-B were 27–54% of values obtained in other males with SCI, indicating that experiencing SCI in the early stages of life has a remarkable impact on bone shape. Interestingly, tibia bone density did not appear to be affected; the average difference in bone density between SCI-B and non-SCI controls was −1.2±0.7%. The bone densities of other males with SCI were 4–19% lower than in SCI-B.
Conclusions
Muscle atrophy and bone loss are commonly reported consequences of SCI. This case reveals that important changes in bone geometry occur after SCI, and that mechanical loading during growth plays a vital role in the development of bone size and shape.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
After a spinal cord injury (SCI), there is a dramatic decline in areal bone mineral density (BMD) and muscle mass of the hip and knee region [1]. Recent research has demonstrated that the bone cross-sectional area also decreases after SCI, and that the distribution of bone around axes of bending and torsion can be altered [2]. The majority of research examining skeletal changes after SCI has been conducted in adults. It has been demonstrated that hip BMD values measured using dual-energy absorptiometry in children with SCI were 56–65% of normal values [3]. However, little is known about the impact of immobilization throughout growth on long-bone geometry.
During growth, as body mass increases and children become more active the loads on the skeleton increase. The skeleton responds by increasing the diameter of long bones via periosteal apposition [4]. By distributing bone further away from the bending or torsional axes in response to increased loading, the bone’s ability to resist bending and torsional loads increases. Studies of the effects of physical activity in growing bones demonstrate that increased mechanical loading during growth can positively affect bone shape [5, 6]. The impact of a relative reduction in loading during growth on bone geometry is unknown. Childhood SCI is a unique experiment of nature to explore whether the absence of loading influences bone shape. The purpose of this study was to describe the impact of reduced loading throughout growth on bone and muscle by comparing the muscle area, volumetric bone mineral density and indices of bone structural strength of a male who sustained SCI at birth with two matched controls without SCI and four males with SCI of similar level and completeness, but who sustained SCI in young adulthood after the most rapid period of skeletal growth.
Methods
Participants
All participants were recruited with the approval of the Research Ethics Board of Hamilton Health Sciences. The characteristics of the study participants are listed in Table 1. According to the American Spinal Injury Association, an injury classified as ASIA C means that the injury was incomplete, and that the individual has some motor function below the neurological injury level, including the lowest sacral segment [7]. All of the individuals with SCI studied, including SCI-B, had an ASIA C classification.
In order to determine the impact of reduced loading throughout growth on bone and muscle, the bone geometry, bone density and muscle cross-sectional area of a male who had experienced an incomplete SCI at birth (from here on called SCI-B) were compared with two males without SCI. The non-SCI controls (CON1 and CON2) were matched as follows: same age ±3 years, same height ±12 cm, and same weight ±11 kg. To further delineate how the impact of SCI in childhood on bone and muscle differs from the impact of SCI in young adulthood, the male who sustained SCI at birth was compared to four males with SCI (SCI-1, SCI-2, SCI-3, SCI-4, or collectively, young adult SCI males, SCI-YA). The SCI-YA all had motor incomplete cervical lesions at a level similar to SCI-B. An attempt was made to recruit SCI individuals of comparable height and/or weight to SCI-B.
Outcome measures
A CTI Scanner (GE, Milwaukee, WI, USA) was used to perform computed tomography (CT) scans. The slice used for analysis was taken at the point of maximum lower limb muscle cross-sectional area (CSA), defined to be 66% of the tibia length, starting from the distal end and measuring proximally. A scout scan of the lower limbs was taken prior to determine the length of the tibia. The system parameters used were as follows: slice thickness 5 mm, pixel matrix 512×512, and exposure factors of 120 kV, 200 mA, standard reconstruction algorithm. CT scans were analyzed using a validated software program (BonAlyse 1.3, BonAlyse Oy, Jyvaskyla, Finland) according to the manufacturer’s instructions. Thresholds of −270 to −101 Hounsfield units (HU) were used to identify fat, and thresholds of −101 to 270 HU were used to identify muscle. BonAlyse was used to calculate muscle CSA (mm2), bone CSA (mm2) and volumetric bone mineral density (vBMD, mg/cm3) at the 66% tibia site. Thresholds for outer and inner borders of bone were 280 and 70 mg/cm3, respectively. Maximum (I max) and minimum (I min) cross-sectional moments of inertia and polar cross-sectional moment of inertia (I pol) were also calculated at the tibia. We have determined that muscle and bone variables obtained from CT scans using our scanner can be measured with reproducibility, as assessed via the root mean squared coefficient of variation [8] of less than 2% for area and density variables and less than 2.6% for moment of inertia variables.
Design and analyses
The data are presented as a case study to demonstrate the bone geometry, bone density and muscle cross-sectional area of an individual who sustained SCI at birth. Descriptive data are presented as means and standard deviations. The matched non-SCI controls were recruited to provide comparison data, since there were no available reference data. The additional individuals with SCI were recruited to delineate the impact of SCI before/during growth compared to the impact of SCI during young adulthood. Data from the left and right legs are averaged.
Results
Impact of SCI at birth on muscle area
Muscle CSA in SCI-B was reduced compared to both non-SCI controls and the SCI-YA (Table 2). Calf muscle CSA in SCI-B was 68 and 58% of values in CON1 and CON2, and 60–87% of values in SCI-YA. Calf muscle CSA was less in all of the SCI-YA compared to CON1, but only two of four SCI-YA had lower muscle CSA compared to CON2 (Table 2).
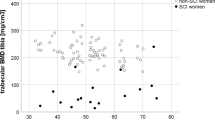
Impact of SCI at birth on volumetric bone density and bone structure
Bone CSA and moments of inertia (maximum, minimum and polar) in all individuals with SCI were much less than those in non-SCI controls. However, the most dramatic differences were noted between SCI-B and controls, where bone CSA and polar moment of inertia values were ~50 and ~25% of control values, respectively. In addition, bone CSA and moment of inertia variables in SCI-B were much smaller than those of the SCI-YA. Bone CSA in SCI-B was 60–67% of values in SCI-1, SCI-2 and SCI-3, and 96% of SCI-4’s bone CSA. Polar moment of inertia in SCI-B was 30–50% of values in SCI-YA. Interestingly, vBMD in SCI-B was not dramatically different from controls, and was higher than values in the SCI-YA. vBMD values in the SCI-YA were 5–17% less than vBMD values in non-SCI controls.
Discussion
The absence of mechanical loading during growth had a remarkable impact on the development of bone size and shape. The impact of reduced loading during growth was most evident in the moment of inertia variables; I max, I min and I pol were substantially lower in SCI-B than in males without SCI and males with similar SCI. Interestingly, vBMD in SCI-B was comparable to controls without SCI, and was slightly greater than other individuals with SCI, suggesting that the absence of mechanical loading did not impede the development of bone as a material, or bone tissue quality, at least at cortical sites. It is possible that SCI-B was genetically predisposed to have small bone size; however his height (191 cm) is not consistent with this hypothesis.
The results are consistent with research demonstrating that mechanical loading during growth has a positive influence on bone geometry. In a recently published study of from the Gothenburg Osteoporosis and Obesity Determinants study, the amount of physical activity reported was significantly associated with cortical bone size and trabecular vBMD, but not with cortical vBMD [9]. Significant side-to-side differences in bone shape have been demonstrated in upper limbs of tennis players, such that bone area, marrow cavity area and cortical wall thickness were greater in the playing arm compared to the non-playing arm, but there were no significant side-to-side differences in vBMD [10]. Similarly, it has been demonstrated that the structural adaptation in bone to tennis and squash playing is manifested as an increase in cortical area, with no difference in marrow area, suggesting that differences are due to increased periosteal apposition [11]. The observed increases were significantly greater in individuals who started playing at a younger age, suggesting that the timing of the initiation of increased loading is important for bone adaptation [11]. A study of males with complete SCI demonstrated that although cortical thickness is reduced at the tibial shaft, cortical bone density decreased slightly during the first 5 years post-SCI, but remained near normal reference values [12]. The current study adds to the growing body of literature supporting the hypothesis that participation in physical activity during growth has a positive impact on cortical bone size, but does not have an impact on the density of the bone at cortical sites.
Muscle CSA in SCI-B was also reduced compared to controls with and without SCI. After SCI there is a rapid and dramatic loss of muscle mass below the level of the lesion. A study of individuals who were only 6 weeks post-SCI demonstrated that average muscle CSAs were 18–46% lower than in control subjects [13]. Prospective study of these patients up to 24 weeks post-SCI revealed further declines in average gastrocnemius and soleus muscle CSAs of 24 and 12%, respectively [14]. Because participants in the current study had motor incomplete SCI, the extent of muscle atrophy was not as severe as is usually evident in individuals with complete SCI. In fact, muscle CSA in two of the five individuals with SCI was comparable to controls, perhaps due to residual motor activity and/or the level of spasticity.
Certain limitations should be acknowledged. The cross-sectional nature of this case study precludes any assumptions of causation. The prevalence of SCI in the general population is low, and SCI at birth is even less common, so it would be difficult to recruit a large number of similar cases or matched SCI controls. Future studies of individuals who suffer SCI or other conditions associated with immobility at various stages of childhood may corroborate the current findings. Further, future studies should incorporate measurements of trabecular bone structure and trabecular vBMD to determine whether the absence of mechanical loading limits bone development in these variables also.
In summary, the current case study demonstrates that the absence of mechanical loading during growth due to SCI early in life has a striking impact on bone size at the tibia shaft, and may also limit growth in muscle size. The absence of a deficit in total volumetric bone density was an interesting finding and supports the theory that mechanical loading during growth has a positive impact on bone growth in size, but may not increase bone density. This case reveals that important changes in bone geometry occur after SCI, and that mechanical loading during growth plays a vital role in the development of bone size and shape.
References
Zehnder Y, Luthi M, Michel D, Knecht H, Perrelet R, Neto I, Kraenzlin M, Zach G, Lippuner K (2004) Long-term changes in bone metabolism, bone mineral density, quantitative ultrasound parameters, and fracture incidence after spinal cord injury: a cross-sectional observational study in 100 paraplegic men. Osteoporos Int 15(3):180–189
de Bruin ED, Herzog R, Rozendal RH, Michel D, Stussi E (2000) Estimation of geometric properties of cortical bone in spinal cord injury. Arch Phys Med Rehabil 81:150–156
Moynahan M, Betz RR, Triolo RJ, Maurer AH (1996) Characterization of the bone mineral density of children with spinal cord injury. J Spinal Cord Med 19(4):249–254
Martin RB (2002) Size, structure and gender: lessons about fracture risk. J Musculoskelet Neuronal Interact 2(3):209–211
Heinonen A, Sievanen H, Kannus P, Oja P, Vuori I (2002) Site-specific skeletal response to long-term weight training seems to be attributable to principal loading modality: a PQCT study of female weightlifters. Calcif Tissue Int 70(6):469–474
Jones HH, Priest JD, Hayes WC, Tichenor CC, Nagel DA (1977) Humeral hypertrophy in response to exercise. J Bone Jt Surg Am 59(2):204–208
Ditunno JF Jr, Young W, Donovan WH, Creasey G (1994) The international standards booklet for neurological and functional classification of spinal cord injury. American Spinal Injury Association. Paraplegia 32(2):70–80
Gluer CC, Blake G, Lu Y, Blunt BA, Jergas M, Genant HK (1995) Accurate assessment of precision errors: how to measure the reproducibility of bone densitometry techniques. Osteoporos Int 5(4):262–270
Lorentzon M, Mellstrom D, Ohlsson C (2005) Association of amount of physical activity with cortical bone size and trabecular volumetric BMD in young adult men: the GOOD study. J Bone Miner Res 20(11):1936–1943
Haapasalo H, Kontulainen S, Sievanen H, Kannus P, Jarvinen M, Vuori I (2000) Exercise-induced bone gain is due to enlargement in bone size without a change in volumetric bone density: a peripheral quantitative computed tomography study of the upper arms of male tennis players. Bone 27(3):351–357
Kontulainen S, Sievanen H, Kannus P, Pasanen M, Vuori I (2003) Effect of long-term impact-loading on mass, size, and estimated strength of humerus and radius of female racquet-sports players: a peripheral quantitative computed tomography study between young and old starters and controls. J Bone Miner Res 18(2):352–359
Eser P, Frotzler A, Zehnder Y, Wick L, Knecht H, Denoth J, Schiessl H (2004) Relationship between the duration of paralysis and bone structure: a PQCT study of spinal cord injured individuals. Bone 34(5):869–880
Castro MJ, Apple DF Jr, Hillegass EA, Dudley GA (1999) Influence of complete spinal cord injury on skeletal muscle cross-sectional area within the first 6 months of injury. Eur J Appl Physiol Occup Physiol 80(4):373–378
Castro MJ, Apple DF Jr, Hillegass EA, Dudley GA (1999) Influence of complete spinal cord injury on skeletal muscle cross-sectional area within the first 6 months of injury. Eur J Appl Physiol Occup Physiol 80(4):373–378
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Giangregorio, L.M., McCartney, N. Reduced loading due to spinal-cord injury at birth results in “slender” bones: a case study. Osteoporos Int 18, 117–120 (2007). https://doi.org/10.1007/s00198-006-0201-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-006-0201-3