Abstract
Introduction
The objective of this study was to determine the effect of a moderate reduction of dietary magnesium [50% of nutrient requirement (50% NR)] on bone and mineral metabolism in the rat, and to explore possible mechanisms for the resultant reduced bone mass.
Methods
Female rats were 6 weeks of age at the start of study. Serum magnesium (Mg), calcium (Ca), parathyroid hormone (PTH), 1,25(OH)2-vitamin D, alkaline phosphatase, osteocalcin, and pyridinoline were measured during the study at 3- and 6-month time points in control (dietary Mg of 100% NR) and Mg-deficient animals (dietary Mg at 50% NR). Femurs and tibias were also collected for mineral content analyses, micro-computerized tomography, histomorphometry, and immunohistochemical localization of substance P, TNFα, and IL-1β at 3 and 6 months.
Results
Although no significant change in serum Mg was observed, Mg deficiency developed, as assessed by the reduction in bone Mg content at the 3- and 6-month time points (0.69±0.05 and 0.62±0.04% ash, respectively, in the Mg depletion group compared to 0.74±0.04 and 0.67±0.04% ash, respectively, in the control group; p=0.0009). Hypercalcemia did not develop. Although serum Ca level remained in the normal range, it fell significantly with Mg depletion at 3 and 6 months (10.4±0.3 and 9.6±0.3 mg/dl, respectively, compared to 10.5±0.4 and 10.1±0.6 mg/dl, respectively, in the control group; p=0.0076). The fall in serum Ca in the Mg-depleted animals was associated with a fall in serum PTH concentration between 3 and 6 months (603±286 and 505±302 pg/ml, respectively, although it was still higher than the control). The serum 1,25(OH)2-vitamin D level was significantly lower in the Mg depletion group at 6 months (10.6±7.1 pg/ml) than in the control (23.5± 12.7 pg/ml) (p<0.01 by the t-test). In Mg-deficient animals, no difference was noted in markers of bone turnover. Trabecular bone mineral content gain was less over time in the distal femur with Mg deficiency at 3 and 6 months (0.028±0.005 and 0.038±0.007 g, respectively, compared to 0.027±0.004 and 0.048±0.006 g, respectively, in the control group; p<0.005). Histomorphometry at these time points demonstrated decreased trabecular bone volume (15.76±1.93 and 14.19±1.85%, respectively, compared to 19.24±3.10 and 17.30±2.59%, respectively, in the control group; p=0.001). Osteoclast number was also significantly increased with Mg depletion (9.07±1.21 and 13.84±2.06, respectively, compared to 7.02±1.89 and 10.47±1.33, respectively, in the control group; p=0.0003). Relative to the control, immunohistochemical staining intensity of the neurotransmitter substance P and of the cytokines TNFα and IL-1β was increased in cells of the bone microenvironment in the Mg depletion group, suggesting that inflammatory cytokines may contribute to bone loss.
Conclusion
These data demonstrate that Mg intake of 50% NR in the rat causes a reduced bone mineral content and reduced volume of the distal femur. These changes may be related to altered PTH and 1,25(OH)2-vitamin D formation or action as well as to an increase release of substance P and the inflammatory cytokines TNFα and IL-1β.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epidemiologic studies have demonstrated a positive correlation between dietary magnesium (Mg) intake and bone density and/or an increased rate of bone loss with low dietary Mg intake, which suggests that dietary Mg deficiency may be a risk factor for osteoporosis [1–6]. The Recommend Daily Allowance (RDA) for Mg for adult males is 420 mg/day and for adult females, 320 mg/day [7, 8]; the usual dietary Mg intake, however, falls below this recommendation in a large proportion of the population of all ages, from adolescence to old age [9]. Other nutrient deficits, such as calcium (Ca) and potassium (K), also influence bone mass and probably coexist with dietary Mg deficiency [7, 8]. In order to assess the effect of selective Mg deficiency on bone, severe Mg deficiency [approximately 0.4% of the Nutrient Requirement (NR)] [10] has been induced in rodent models; this results in osteoporosis characterized by decreased bone formation, increased bone resorption, and increased skeletal fragility [11–18]. This degree of Mg depletion, however, probably rarely exists in humans. We have recently reported that more moderate dietary Mg restrictions, at levels of 10% NR and 25% of NR, also results in bone loss in the rat [19, 20]. Although this deficit of dietary Mg may also be unusual in humans, these findings do suggest that extremes of Mg intake may place humans at risk for osteoporosis. The cause of this effect of Mg depletion on bone is unclear, although abnormal parathyroid hormone (PTH) and 1,25(OH)2-vitamin D formation and/or action as well as increased amounts of inflammatory cytokines in the bone of Mg-deficient mice and rats may play a role, as discussed below.
The objective of this study was to assess the effect of a diet containing 50% of the NR in the rat model and to determine whether this degree of Mg depletion affects bone mass and/or Ca metabolism, or alters the presence of inflammatory cytokines in bone.
Materials and methods
Experimental methods
The studies reported here were approved by the IACUC of the University of Southern California. Dietary Mg deficiency was induced for 3 and 6 months in 6-week-old, 150- to 175-g female Sprague Dawley rats (Charles Rivers Laboratory, Wilmington, Mass.). We have previously reported the adverse effects of severe Mg deficiency on bone in more mature (290 g) rats [15]. We purposely selected younger rats in this study in order to be able to assess the effects of dietary Mg deprivation throughout the aging process. This is an important factor of the experimental design since dietary Mg intake in humans falls below the RDA from adolescence to old age [7, 8]. In addition, in our mouse studies [16] immunohistochemical identification of cytokines were more apparent in younger animals, thus allowing a greater opportunity to identify changes that may adversely affect bone.
After acclimation to the vivarium as previously described [19], experimental diets were instituted. Since bone mass is closely correlated with body mass, group pair feeding based on food weight was performed daily in order to keep weight gain as close as possible in the Mg-deficient and control groups. Distilled deionized water containing <3×10−5 g Mg/l was used for hydration. Rats were fed either a normal control Mg diet (100% NR) or a Mg-deficient diet (50% of NR) (Harlan Teklad, Madison, Wis.). The dietary intake of Ca was at or near the recommended intake level for rats. The actual composition of these diets is shown in Table 1.
No baseline or zero time values were obtained as the Mg-deficient groups had their appropriate diet-matched control adjusted so that there was no difference in body weight (Table 1). After 3 and 6 months on the experimental diets, rats were anesthetized (ketamine, 50 mg/kg, and xylazine, 10 mg/kg, intramuscularly; Phoenix Pharmaceuticals, St. Joseph, Mo.). Blood samples from the anesthetized rats were obtained by cardiac puncture, and the rats were then euthanized by open thoracotomy. The femurs and tibias were harvested at each time point for mineral analysis, micro-computerized tomography (μCT), histomorphometry, and immunohistochemistry.
Biochemical determinations
Blood samples were allowed to clot for 30 min and then centrifuged at 10,000 rpm in a Labnet Hermle Centrifuge, Model MR-2 for 10 min at room temperature. Serum was separated from the clot and frozen at −70°C.
Serum Ca and Mg concentrations
Serum Ca and Mg concentrations were determined by atomic absorption spectrophotometry (Spectra AA-220, Varian, Walnut Creek, Calif.).
Serum parathyroid hormone
PTH was determined utilizing a two-site enzyme-linked immunosorbent assay (ELISA) kit (Rat Intact PTH ELISA kit; Immutopics, San Clemente, Calif.). This assay has a sensitivity of 1.6 pg/ml, an intra-assay precision of 2.1–2.4%, and an inter-assay precision of 5.1–6.0% at low to high serum PTH concentrations.
Serum 1,25(OH)2-vitamin D
A competitive equilibrium radio-immunoassay (RIA) was used for quantitative determination of 1,25(OH)2-vitamin D (DiaSorin, Stillwater, Minn.). This assay consisted of a two-step procedure involving a preliminary extraction and subsequent purification of 1,25(OH)2-vitamin D from serum using C18OH “Extra Clean” cartridges. Following extraction, the treated sample was assayed using a competitive RIA method based on a polyclonal antibody that is 100% specific for both 1,25(OH)2-vitamin D2 and D3. This assay measures 1,25(OH)2-vitamin D in the range of 5–200 pg/ml and has a sensitivity of <2 pg/ml. The intra- and inter-assay variation for low levels (25.8 pg/ml) is 6.8 and 14.6% respectively; for mid levels (41.3 pg/ml), 7.7 and 11.1%, respectively; for high levels (105.2 pg/ml), 11.3 and 11.2% respectively.
Serum osteocalcin
Rat serum osteocalcin was determined utilizing a sandwiched ELISA kit (Biomedical Technologies, Stoughton, Mass.). This assay measures osteocalcin in the range of 0.78–50 ng/ml and has a sensitivity of 0.5 ng/ml, an intra-assay variation of 4% (95% limits) and an inter-assay variation of 7% (95% limits).
Serum alkaline phosphatase
Alkaline phosphatase activity in rat serum was measured using an endpoint colorimetric spectroscopy (Sigma-Aldrich, St. Louis, Mo.) using a procedure modified to accommodate small sample volumes. Enzymatic activity was determined by measuring the release of p-nitrophenol from substrate p-nitrophenylphosphate. The spectrophotometric reading was made at 405 nm (Spectra MAX 250; Molecular Devices, Sunnyvale, Calif.), and the unknown was compared to p-nitrophenol standards. Enzymatic activity was expressed in U/l. The total CV% for low levels (<1.0 SU/ml) is 6%; for normal levels, 2%, for high levels, 1%.
Serum pyridinoline assay
Pyridinoline (Pyd) crosslinks in rat serum were determined utilizing the Metra Serum PYD EIA kit (Quidel, Mountain View, Calif.). This competitive enzyme immunoassay utilized a rabbit polyclonal anti-Pyd antibody to measure Pyd in serum in a microassay stripwell format. Sample filtering was required prior to assaying. This assay has a detection limit of 0.4 nmol/l, a 0–12 nmol/l range of detection, an intra-assay precision of 6.3–14.8%CV, and an inter-assay precision of 8.7–11.6%CV.
Skeletal studies
Mineral content of bone by ashing
To assess the effect of Mg deficiency on bone mineral content, the right femur, stripped of soft tissue, was frozen in liquid nitrogen and stored at −70°C prior to bone ashing [15]. Mg, Ca, and phosphorus (P) content were determined as previously described [16].
Bone mineral content by μCT
Analyses were performed using the SkyScan 1074 X-ray microtomograph (Skyscan, Belgium; Micro Photonics, Allentown, Pa.) and associated three-dimensional (3D)-Calc, cone reconstruction and ANT model building software. Left tibias were fixed in formalin for 24 h, stored in 70% ethanol, cleaned of soft tissue, dissected so that the proximal tibia section was 1.2 cm in length, and dried overnight. Specimens were placed in the chamber, oriented with the proximal end up such that two thirds of the specimen’s upper segment fell within the X-ray field. An exposure time of 1440 msec was used with a step value of 0.9. A reconstruction of the bitmap data set (consisting of 400–500 sections) was obtained and used to build the 3-D model. The model was bisected with a plane down the anterior/posterior midline, and a data set was obtained with from a total of 30 sections (15 on each side of the bisecting plane). Each final data set was based on a standardized analysis of a tissue volume which averaged 3.255 mm3. Care was taken so that the region of interest contained only trabecular bone.
Quantitative bone histomorphometry
Left femurs were harvested and prepared and histomorphometry performed as previously described [19, 21, 22]. Quantitative bone histomorphometry utilized the OsteoMeasure software of OsteoMetrics (Atlanta, Ga.) and standard nomenclature [21]. The following histomorphometric variables were collected and analyzed: BV/TV (percentage trabecular bone volume); OV/BV (percentage of bone volume occupied by osteoid); NOb/BPm (the number of osteoblasts per millimeter bone surface); ES/BS (the total proportion of bone surface involved in resorption); OcS/BS (percentage of bone surface covered by TRAP-positive osteoclasts); NOc/BPm (the number of TRAP-positive osteoclasts per millimeter of bone surface); TTh (mean trabecular width, in micrometers).
Bone immunohistochemical staining
Tibia were dissected and fixed in 2% formalin for 24 h. The bone was demineralized in 10% EDTA at pH 7 for 1 week and then embedded in paraffin, oriented so that a sagittal section, including the epiphysis and metaphysis, was obtained. Sections were stained with hematoxylin and eosin (H & E) for analysis of the growth plate. Tartrate-resistant acid phosphatase (Sigma) was used to stain osteoclasts which were identified at a magnification of 25× and counted at a magnification of 10× using a graticule in the eyepiece to determine the number per square millimeter in the primary and secondary spongiosa.
Indirect immunohistochemistry
Indirect immunohistochemistry was used to localize substance P, TNFα, and IL-1β in bone cells and marrow cells of the metaphysis. The antibodies were goat and rabbit in origin and obtained from R&D Systems, Minneapolis, Minn. (TNFα and IL-1β) and Chemicon, Temecula, Calif. (substance P) [23, 24]. Following deparaffinization and rehydration, hydrogen peroxide was applied to quench any endogenous peroxidase. Incubation in 20% normal serum of the same species as the secondary antibody eliminated nonspecific staining. Polyclonal antibodies at optimized dilutions were applied for a predetermined optimized time and temperature. Biotin conjugated anti-species in which the antibody was made were applied followed by streptavidin horseradish peroxidase. Localization was visualized in the light microscope using Nova Red (Vector Laboratories, Burlingame, Calif.) counterstained with hematoxylin. The results were photographed in a Zeiss photomicroscope (Carl Zeiss, Thornwood, N.Y.) using a 40× objective.
Evaluation of staining
Evaluation of staining was carried out under conditions where the background staining was minimal compared with the positive and negative controls. Cells and tissues must stain specifically as described for the antigen in the literature [23, 24]. The entire section of the growth plate and primary spongiosa was examined (an average of ten fields at 25×). Proliferating chondrocytes, osteoclasts, osteoblasts, megakaryocytes, and mononuclear cells were evaluated. Intensity was graded as 0 = no stain, 1 = weak stain, 2 = moderate, and 3 = strong stain. The quantitative estimate of numbers of cells staining was grade a = <20%, grade b = 20–60%, grade c = >60%. Mean relative positivity for bar or line graphical presentation was <1b = 0; 2a and 2b = 1; 3b and 3c = 2 [23, 24].
Statistical analysis
Data were analyzed using SAS version 8.2. A p value of less than 0.05 was considered to be statistically significant. Standard statistical methods were used. Descriptive statistics, including means and standard deviations, were calculated. When data were not normally distributed, the Wilcoxon rank sum test or Kruskal-Wallis test was employed. Spearman’s correlation coefficients were calculated to determine relationships among the outcome variables. Two-way ANOVA was used to assess differences between low Mg-treated rats and control rats at 3 and 6 months into the experiment. In two-way analysis of variance, an interaction between the two factors signifies that the effect of one factor is dependent on a particular level of the other factor. In this study, a significant interaction means that the difference between the low magnesium diet and the control diet was not uniform across the time points. (For instance, the difference between a parameter in the two dietary groups may be increasing over time.)
Results
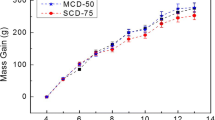
Rat nutrition and weight
The composition of the rat diet is shown in Table 1. Initial body weight and weight at 3 and 6 months in control and Mg-deficient rats are shown in Table 2. Although weight increased in both groups, with pair feeding no difference in body weight was observed between the Mg-deficient and control groups.
Serum parameters
It is commonly known that severe Mg deficiency results in hypercalcemia in the rat; however, at this dietary intake, the serum Ca fell significantly lower (although still within the normal range) over time in the low Mg group from 3 months to 6 months, as shown in Table 3 (10.4±0.3 to 9.6±0.3 mg/dl in the low Mg group compared to 10.5±0.4 to 10.1±0.6 mg/dl in the control group; p=0.0076). No significant difference was observed in the level of serum Mg. The low Mg diet had a significant effect on PTH and 1,25(OH)2-vitamin D levels, with these values remaining stable in the controls but falling in the Mg-deficient animals. As Mg has one-third the affinity of calcium for the parathyroid Ca-sensing receptor [25], early in the Mg depletion treatment (at 3 months) PTH levels were significantly elevated versus controls (603±286 pg/ml in the low Mg group and 355±204 pg/ml in controls; p<0.01 by t-test); this explains the high 1,25(OH)2-vitamin D levels in the Mg-deficient animals at this time point (39.6±14.9 pg/ml in the Mg-deficient group compared to 25.7±7.4 pg/ml in the controls; p<0.01 by t-test ). As the cell becomes Mg-deficient, PTH cannot respond appropriately, and renal resistance to PTH also occurs [26–29]. Therefore, at 6 months note the significantly lower 1,25(OH)2-vitamin D level of 10.6±7.1 pg/ml when compared to the corresponding control value of 23.5±12.7 pg/ml (p<0.01 by t-test) and the reduction in serum PTH from the 3-month time point onwards (505±302 pg/ml) despite the lower serum Ca.. The slight elevation in alkaline phosphatase levels in the low Mg animals at 3 months can also be explained on the basis of the changes in PTH levels (33.8±5.1 U/l compared to 27.7±7.0 U/l; p<0.05 by t-test). These findings are similar to our observations in experimental human Mg deficiency [30]. No difference was noted in serum pyridinoline levels.
Bone mineral content
As noted in Table 4, there was a significantly greater decrease in bone Mg in the Mg-depleted animals between 3 and 6 months (0.69±0.05 and 0.62±0.04% ash, respectively, compared to 0.74±0.04 and 0.67±0.04% ash, respectively, of the control; p=0.0009). This probably occurred because the bone served as a Mg reservoir for the serum Mg. No significant change was observed in Ca or P contents.
Bone mineral density by μCT
The data in Table 5 show a lower trabecular bone mineral density gain of the distal femur at 3 and 6 months in the Mg-deficient group (0.028±0.005 and 0.038±0.007 g, respectively, compared to 0.027±0.004 and 0.048±0.006 g, respectively, of the control; p<0.005), and indicates that the low-Mg animals are gaining a significantly lower amount of bone at this site across time than are the control animals. No significance difference was observed in cortical bone mass.
Quantitative histomorphometry
Histomorphometric features of low-Mg and control animals at the 3- and 6-month time points are shown in Table 6. Trabecular bone volume (BV/TV) was significantly lower in the Mg-depleted group (15.76±1.93 and 14.19±1.85%, respectively, compared to 19.24±3.10 and 17.30±2.59%, respectively, of the control group; p=0.001). Osteoclast numbers (Noc/BPm) increased significantly more in the Mg-deficient animals (9.07±1.21 and 13.84±2.06, respectively, compared to 7.02±1.89 and 10.47±1.33, respectively, of the control group; p=0.0003. Osteoclast surface (OcS/BS) also increased more in Mg-depleted animals, 17.96±2.85 and 25.02±5.24, respectively, compared to14.56±3.85 and 17.96±2.26 of the control group; p=0.001. Osteoclast morphology appeared to be normal in Mg-depleted animals, and scalloped surfaces were present on the bone underlying the osteoclasts, suggesting normal activity.
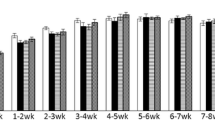
Immunohistology
Immunohistochemical staining for substance P was observed to be low at both time points; however, in Mg-depleted animals it was 56% higher in mononuclear cells at 3 months, and 76% higher at 6 months. Little staining was observed in other cell types. TNFα was 149% greater in osteoclasts, and 58% greater in megakaryocytes at 3 months; at 6 months, no increase was present, and no difference in localization in other cell types was present. Staining for IL-1β was 106% greater in osteoclasts, and 92% greater in megakaryocytes at 3 months, but no increase was observed at 6 months. Of interest is the observation that there was also a 147% increase of IL-1β in the cartilage at 3 months and a 100% increase at 6 months. No difference in IL-1β was noted in other cell types.
Discussion
Osteoporosis is a major health concern which accounts for 1.5 million fractures in the United States each year and a cost of over US$15 billion [31–33]. Women with postmenopausal osteoporosis have decreased nutrition markers, suggesting that osteoporosis may be associated with nutritional deficiencies [34].
Mg, the second most prevalent intracellular cation in the body, plays an important role in enzyme activity, membrane stability, and ion transport [35]. Mg exists in macronutrient quantities in bone (0.5–1% bone ash), and dietary Mg shortfall has been implicated as a risk factor for osteoporosis [36–39].
The U.S. Food Nutrition Board of the Institute of Medicine established the RDA for Mg for adult males at 420 mg/day and for adult females at 320 mg/day [7]. The usual dietary Mg intake, however, falls below this recommendation. According to the USDA [9], the mean Mg intake for males is 323 mg/day (81% of the RDA) and that for females is 228 mg/day (68% of RDA). This deficiency is present from adolescence to old age. In females, the mean Mg intake for ages 14–18 is 225 mg/day (RDA: 360 mg); for ages 31–50, 236 mg/day (RDA: 320 mg); for ages 51–70, 239 mg/day (RDA: 320 mg).
This substantial dietary Mg deficit is particularly important in an aging population where gastrointestinal and renal mechanisms for Mg conservation may not be as efficient as in a younger population [40–42]. Ten percent of elderly women in the U.S. consume <136 mg of Mg per day (<43% of RDA) [7]. In women aged 14 and over, the mean intake at the 10th percentile was 145 mg/day (45% of RDA) and at the 25th percentile, 177 mg/day (55% of RDA) [7]. Morbid conditions producing body Mg loss (diabetes, alcoholism, malabsorption) and medications (diuretics, cyclosporine, aminoglycosides, cisplatin, amphotericin B) also exacerbate the problem [35].
The data presented here demonstrate that, in the rat, a Mg intake at a level of even 50% NR causes decreased amounts of trabecular bone. The finding of this study is of importance in as much as this Mg intake level is present in some members of our society, as stated above, and therefore contributes significantly to the growing problem of osteoporosis. The consumption of Mg (per nutritional/energy value) in the rat diets (Table 1) is similar to what may be consumed by humans.
Low dietary Ca intake is also a recognized risk factor for osteoporosis [31, 43–45]. Low dietary Ca has been reported to be a predictor of bone density as well as fracture rate [43–50]. From adolescence to old age, dietary Ca intake falls far below the established Adequate Intake (AI) set by the U.S. Food Nutrition Board [8]. Low Ca intake is particularly critical during adolescence when much of the skeleton is formed. Peak bone mass is an important predictor of osteoporosis in later life [51, 52]. Ten to twenty percent of adolescent girls have a Ca intake less than 500 mg/day [53]. A recent study reported that pubertal girls only partially adapt to low dietary Ca intake, thereby placing themselves at greater risk for inadequate Ca retention [53]. This inability to adapt may be linked to other nutritional deficiencies, since previous studies have suggested that other dietary factors also impact bone mass [54–58]. As discussed below, Mg deficiency has a profound impact on Ca and skeletal homeostasis.
The mechanistic reasons for Mg deficiency-induced reduction of trabecular bone are probably multifactorial. Mg deficiency in man results in impaired PTH secretion and hypocalcemia [26–28]. A major difference in severe Mg deficiency between humans and rodents is that hypocalcemia develops in humans [26], while hypercalcemia develops in rodents [15, 16, 19]. PTH levels are low in both humans and rodents. The low PTH level in humans is thought to be due to a defect in PTH secretion [26]. This may also be true in rodents; however hypercalcemia could be responsible. The reason for the hypercalcemia in rodents is unclear, but it does not appear to be due to an increase in bone resorption as the administration of osteoprotegerin does not prevent hypercalcemia in Mg-deficient mice [59]. Ca and Mg share a common intestinal Mg transport system [60], and it is probable that, in the absence of dietary Mg, fractional absorption of Ca is increased. Indeed, a low Ca diet prevents hypercalcemia in the Mg-deficient rodent [16]. All of the aforementioned studies occurred during severe Mg depletion. It appears that the degree of Mg depletion may alter these observations. We have recently administered Mg diets to rats at 10% NR [19], 25% NR [20], and, in this report, 50% NR. With the 10% NR diet, serum Ca, with Mg depletion, continued to be slightly higher than control. PTH levels, while initially higher, fell over the course of 6 months to below the level of the control. As an acute fall in serum Mg affects the Ca-sensing receptor in a manner similar to an acute fall in serum Ca [25], this may explain the initial rise in PTH.
With the 25% NR diet, hypercalcemia did not occur in the rat [20]. PTH levels fell significantly below those of the control by the end of the study (6 months). In study reported here – 50% NR – serum Ca was significantly lower than that of the control. PTH was higher than the control despite the absence of a significant difference in serum Mg or Ca at 3 months. However, serum PTH fell over time in the Mg-deficient animals, as determined at the 6-month time point, despite the decrease in serum Ca. It appears that the effect of Mg deficiency on rat parathyroid function is qualitatively similar to that in humans, but it is not as susceptible to inhibition of PTH secretion. The adverse effect of dietary Mg restriction was also reflected in the bone. The Mg content of bone was reduced 51% in the 10% NR diet and 27% in the 25% NR diet [19, 20]. BV/TV was reduced 54% on the 10% NR diet and 42% on the 25% NR diet [19, 20].
Mg deficiency also impairs the effect of PTH on bone and kidney. The rise in serum Ca and in urine hydroxyproline, P, and cyclic AMP, which is produced in response to PTH administration, is decreased in human Mg depletion [26, 29]. Following Mg therapy, the PTH response normalizes [26, 29]. Similar findings have been reported in animal models [60]. These data indicate that Mg deficiency impairs both PTH secretion and PTH action on the kidney and bone.
As we have confirmed in experimental human Mg deficiency studies [28], patients with Mg depletion also have reduced serum levels of 1,25(OH)2-vitamin D [61]. This feature can be explained on the basis of impaired PTH secretion with subsequent loss of the trophic effect of PTH on 1,25(OH)2-vitamin D synthesis, or by a direct effect whereby Mg depletion impairs the metabolism of 1,25(OH)2-vitamin D (since in vitro studies have demonstrated that the renal 1α-hydroxylase enzyme is Mg-dependent) [62].
Thus, it is clear that even mild Mg depletion can perturb Ca homeostasis and result in a fall in both serum PTH and 1,25(OH)2-vitamin D. We have demonstrated in this study that a moderate reduction in Mg intake in the rat also results in a fall in 1,25(OH)2-vitamin D. Since PTH and 1,25(OH)2-vitamin D stimulate osteoblast activity and/or the synthesis of osteocalcin and procollagen [63, 64], any decreased formation of, and/or end-organ resistance to PTH or 1,25(OH)2-vitamin D may be a major cause of decreased bone formation [19, 65–67]. In addition, the Mg deficiency-induced fall in serum 1,25(OH)2-vitamin D may also decrease intestinal Ca absorption, creating a Ca deficit – a known risk factor for osteoporosis. Diabetic children who were hypomagnesemic have been shown to have an impaired rise in serum 1,25(OH)2-vitamin D when challenged with a low Ca diet [68]. This was reversed with Mg repletion. Mg deficiency has also been demonstrated to impair the rise in serum 1,25(OH)2-vitamin D during dietary Ca deprivation in a rat model [69].
Although changes in PTH and 1,25(OH)2-vitamin D action or formation may explain low bone formation, it does not explain our previous and current observation of an increase in osteoclast bone resorption at various dietary Mg intakes [15, 19]. Each year, approximately 25% of trabecular bone is resorbed and replaced in human adults; in contrast, only 3% of cortical bone undergoes remodeling [70]. Such data suggest that the rate of locally controlled bone remodeling is important in the development of osteoporosis.
Mg has been shown to inhibit the N-methyl-D-aspartate (NMDA) receptor [71], the activation of which induces the release of neurotransmitters, such as substance P [71]. A reduction in extracellular Mg lowers the threshold levels of excitatory amino acids (i.e., glutamate) necessary to activate this receptor. In one rodent study, dietary Mg deficiency produced raised serum levels of neuropeptides (such as substance P) [72]. This neurogenic response is followed by the release of proinflammatory cytokines (TNFα, IL-1β, IL-6) by T lymphocytes during the first week of dietary Mg depletion [72–74]. This finding, however, has not been observed in all studies [75–77]. Many of the actions of substance P are mediated through the neurokinin 1 (NK-1) receptor. Elevated plasma cytokines and the inflammatory cardiac lesions observed in Mg-deficient rats have been shown to be prevented by the administration of a NK-1 receptor antagonist [72–76].
Recent studies have demonstrated that there are nerve fibers containing a number of neuropeptides, including substance P, in bone [78, 79]. Substance P has been shown to increase the release of IL-1β and IL-6 by bone marrow cells [79]. These cytokines, which are systemically released as well as locally produced in the bone micro-environment, are known to stimulate the recruitment and activity of osteoclasts and increase bone resorption [80, 81]. We have found a greater intensity of immunohistochemical staining for substance P, TNFα, and IL-1β in bone from Mg-depleted mice [16] and rats [19, 20]. Increased production of these cytokines has been implicated in the development of sex steroid deficiency or postmenopausal osteoporosis [82, 83]. Recent evidence suggests that inducible nitric oxide synthetase is stimulated by these cytokines and may mediate localized bone destruction associated with metabolic bone diseases [84, 85]. Mg-deficient rodents have increased free radical formation which may affect the cytokine cascade and influence skeletal metabolism [74]. These cytokines could contribute to an increase in osteoclastic bone resorption and explain the uncoupling of bone formation and bone resorption observed in the rat [15, 17]. Our finding of an increase in osteoclast activity and an increase in the histochemical staining for inflammatory cytokines in bones of animals maintained at a dietary Mg level of 50% NR strongly suggests that dietary Mg deprivation plays a role in human osteoporosis. The lack of change in pyridinoline does not reflect our observation of an increase in osteoclast numbers. This may reflect that serum pyridinoline is not a very specific marker of bone resorption, and a more specific marker such as deoxypyridinoline will be used in future studies.
Several other potential mechanisms may account for a decrease in bone mass/strength during Mg deficiency. Mg is mitogenic for bone cell growth and, therefore, Mg deficiency may result in a decrease in bone formation [86]. Mg also affects crystal formation; a lack of Mg results in a larger, more perfect crystals which may affect bone strength [87]. Serum IGF-1 levels have also been observed to be low in the Mg-deficient rat; decreased IGF-1 may adversely influence skeletal growth [88].
This study demonstrates for the first time that Mg intake at the 50% NR level – a nutritional level consumed by a substantial proportion of our population – may be another risk factor for osteoporosis. The mechanism for disturbed bone metabolism may include altered PTH and 1,25(OH)2-vitamin D secretion and/or action as well as increased formation of substance P and inflammatory cytokines. In future studies, it will be critical to assess the influence of additional concomitant nutritional deficits, especially Ca deficiency.
References
Yano K, Heilbrun LK, Wasnich RD, Hankin JH, Vogel JM (1985) The relationship between diet and bone mineral content of multiple skeletal sites in elderly Japanese American men and women living in Hawaii. Am J Clin Nutr 42:877–888
New SA, Bolton-Smith C, Grubb DA, Reid DM (1997) Nutritional influences on bone mineral density: a cross-sectional study in premenopausal women. Am J Clin Nutr 65:1831–1839
New SA, Robins SP, Campbell MK, Martin JC, Garton MJ, Bolton-Smith C, Grubb DA, Lee SJ, Reid DM (2000) Dietary influences on bone mass and bone metabolism: further evidence of a positive link between fruit and vegetable consumption and bone health? Am J Clin Nutr 71:142–151
Tucker KL, Hannan MT, Chen H, Cupples LA, Wilson PW, Kiel DP (1999) Potassium, magnesium and fruit and vegetable intakes are associated with greater bone mineral density in elderly men and women. Am J Clin Nutr 69:727–736
Carpenter TO, Barton CN, Park YK (2000) Usual dietary magnesium intake in NHANES III is associated with femoral bone mass. J Bone Min Res 15[Suppl 1]:S292
Wang MC, Moore EC, Crawford PB, Hudes M, Sabry ZI, Marcus R, Bachrach LK (1999) Influence of pre-adolescent diet on quantitative ultrasound measurements of the calcaneus in young adult women. Osteoporos Int 9:532–535
Dietary Reference Intakes for calcium, phosphorus, magnesium, vitamin D, and fluoride (1997). National Academy Press, Washington, DC, pp 71–145, 190–249, 392–393
Dietary intake of selected minerals for the United States population: 1999–2000 (April 27, 2004). Department of Health and Human Services, Number 341, pp 1–6
Cleveland LE, Goldman JD, Borrude LG (eds) (1994) Data tables: results from USDA 1994 continuing survey of food intakes by individuals and 1994 diet and health knowledge survey. Agricultural Research Service, U.S. Department of Agriculture, Beltsville, Md.
Nutrient requirements of laboratory animals, 4th edn (1995). National Academy Press, Washington, D.C.
Kenney MA, McCoy H, Williams L (1994) Effects of magnesium deficiency on strength, mass and composition of rat femur. Calcif Tissue Int 54:44–49
Boskey AL, Rimnac CM, Bansal M, Lian J, Boyan BD (1992) Effect of short-term hypomagnesemia on the chemical and mechanical properties of rat bone. J Orthop Res 10:774–783
Mirra JM, Alcock NW, Shils ME, Tannenbaum P (1982) Effects of calcium and magnesium deficiencies on rat skeletal development and parathyroid gland area. Magnesium 1:16–33
Carpenter TO, Mackowiak SJ, Troiano N, Gundberg CM (1992) Osteocalcin and its message: relationship to bone histology in magnesium-deprived rats. Am J Physiol 263:E107–E114
Rude RK, Kirchen ME, Gruber HE, Meyer MH, Luck JS, Crawford DL (1999) Magnesium deficiency-induced osteoporosis in the rat: uncoupling of bone formation and bone resorption. Magnes Res 12:257–267
Rude RK, Gruber HE, Wei LY, Frausto A, Mills BG (2003) Magnesium Deficiency: Effect on bone and mineral metabolism in the mouse. Calcif Tissue Int 72:32–41
Gruber HE, Rude RK, Wei LY, Frausto A, Mills BG, Norton HJ (2003) Magnesium deficiency: effect on bone mineral density in the mouse appendicular skeleton. BMC Musculoskelet Disord 4:7–11
Stendig-Lindberg G, Koeller W, Bauer A, Rob PM (2004) Prolonged magnesium deficiency causes osteoporosis in the rat. J Am Coll Nutr 23:704S–711S
Rude RK, Gruber HE, Norton HJ, Wei LY, Frausto A, Mills BG (2004) Bone loss induced by dietary magnesium reduction to 10% of the nutrient requirement in rats is associated with increased release of substance P and tumor necrosis factor-α. J Nutr 134:79–85
Rude RK (2005) Dietary magnesium reduction to 25% of nutrient requirement disrupts bone and mineral metabolism in the rat. Bone 37:211–219
Gruber HE, Marshall GJ, Nolasco LM, Kirchen ME, Rimoin DL (1988) Alkaline and acid phosphate demonstration in human bone and cartilage: effects of fixation intervals and methacrylate embedments. Stain Technol 63:299–305
Gruber HE (1992) Adaptations of Goldner’s-Masson trichrome stain for the study of undecalcified plastic-embedded bone. Biotech Histochem 67:30–34
Mills BG, Frausto A (1997) Cytokines expressed in multinucleated cells: Paget’s disease and giant cell tumors versus normal bone. Calcif Tissue Int 61:16–21
Mills BG, Frausto A, Brien E (2000) Cytokines associated with the pathophysiology of aggressive fibromatosis. J Orthop Res 18:655–662
Brown EB, Gamba G, Ricarrdi D, Lombardi M, Butters R, Kilfor O, Sun GA, Hediger MA, Herbert SC (1993) Cloning and characterization of an extracelluar Ca2+ sensing receptor from bovine parathyroid. Nature 366:575–580
Rude RK, Oldham SB, Singer FR (1976) Functional hypoparathyroidism and parathyroid hormone end-organ resistance in human Mg deficiency. Clin Endocrinol 5:209–224
Rude RK, Oldham SB, Sharp Jr CF, Singer FR (1978) Parathyroid hormone secretion in magnesium deficiency. J Clin Endocrinol Metab 47:800–806
Fatemi S, Ryzen E, Flores J, Endres DB, Rude RK (1991) Effect of experimental human magnesium depletion on parathyroid hormone secretion and 1,25-dihydroxyvitamin D metabolism. J Clin Endocrinol Metab 73:1067–1072
Estep H, Shaw WA, Watlington C, Hobe R, Holland W, Tucker StG (1969) Hypocalcemia due to hypomagnesmia and reversible parathyroid hormone unresponsiveness. J Clin Endocrinol Metab 29:842–848
Fatemi S, Ryzen E, Flores JF, Endres DB, Rude RK (1991) Effect of experimental human magnesium depletion on PTH secretion and 1,25(OH)2-vitamin D metabolism. J Clin Endocrinol Metab 72:1067–1072
Consensus Development Conference (1991) Prophylaxis and treatment of osteoporosis. Am J Med 90:107–110
Riggs BL, Melton LJ (1992) The prevention and treatment of osteoporosis. N Engl J Med 327:620–627
Aloia JF, Cohn SH, Vaswani A, Yeh JK, Yuen K, Ellis K (1985) Risk factors for postmenopausal osteoporosis. Am J Med 78:95–100
Rico H, Relea P, Revilla M, Hernandez ER, Arribas I, Villa LF (1993) Biochemical markers of nutrition in osteoporosis. Calcif Tissue Int 52:331–333
Rude RK (1998) Magnesium deficiency: a heterogeneous cause of disease in humans. J Bone Miner Res 13:749–758
Stendig-Lindberg G, Tepper R, Leichter I (1993) Trabecular bone density in a two-year controlled trial of peroral magnesium in osteoporosis. Magnes Res 6:155–163
Sojka JE, Weaver CM (1995) Magnesium supplementation and osteoporosis. Nutr Rev 53:71–80
Cohen L, Kitzes R (1981) Infrared spectroscopy and magnesium content of bone mineral in osteoporotic women. Isr J Med Sci 17:1123–1125
Wallach S (1990) Effects of magnesium on skeletal metabolism. Magnes Trace Elem 9:1–14
Mountokalakis T, Singhellakis P, Alevizaki C, Virvadakis K, Ikkos D (1980) Relationship between degree of renal failure and impairment of intestinal magnesium absorption. In: Seelig MS (ed) (1980) Magnesium in Health and Disease. Spectrum, New York pp 453–458
Lowik MRH, van Dokkum W, Kistemaker C, Schaafasma G, Ockhuizen T (1993) Body composition, health status and urinary magnesium excretion among elderly people (Dutch nutrition surveillance system). Magnes Res 63:223–232
Martin BJ (1990) The magnesium load test: Experience in elderly subjects. Aging 2:291–296
Optimal calcium intake (1994) NIH Consens Statement 12:1–24
Heaney RP (2000) Calcium, dairy products and osteoporosis. J Am Coll Nutr 19:83S–99S
Flynn A (2003) The role of dietary calcium in bone health. Proc Nutr Soc 62:851–858
Cashman KD, Flynn A (1999) Optimal nutrition: calcium, magnesium and phosphorus. Proc Nutr Soc 58:477–487
Dawson-Hughes B, Gallai GE, Drall EA, Sadowski L, Sahyoun N, Tannenbaum S (1990) A controlled trial of the effect of calcium supplementation on bone density in postmenopausal women. N Eng J Med 323:878–883
Chapuy MC, Arlot ME, Duboeuf F, Brun J, Crouzet B, Amaus S, Delmas PD, Heunier PJ (1992) Vitamin D3 and calcium to prevent hip fractures in the elderly women. N Eng J Med 327:1637–1642
Meyer HE (2004) Calcium and osteoporotic fractures. Brit J Nutr 91:505–506
Prentice A (2003) Diet, nutrition and the prevention of osteoporosis. Pub Health Nutr 7:227–243
Bachrach LK (2001) Acquisition of optimal bone mass in childhood and adolescence. Trends Endocrinol Metab 12:22–28
Weaver CM (2000) Calcium and magnesium requirements of children and adolescents and peak bone mass. Nutrition 16:514–516
Abrams SA, Griffin IJ, Hicks PD, Gunn SK (2004) Pubertal girls only partially adapt to low dietary calcium intakes. J Bone Miner Res 19:759–763
Yano K, Heilbrun LK, Wasnich RD, Hankin JH, Vogel JM (2985) The relationship between diet and bone mineral content of multiple skeletal sites in elderly Japanese-American men and women living in Hawaii. Am J Clin Nutr 42:877–888
Freudenheim JL, Johnson NE, Smith EL (1986) Relationships between usual nutrient intake and bone-mineral content of women 35–65 years of age: longitudinal and cross-sectional analysis. Am J Clin Nutr 44:863–876
Tranquilli AL, Lucino E, Garzetti GG, Romanini C (1994) Calcium, phosphorus and magnesium intakes correlate with bone mineral content in postmenopausal women. Gynecol Endocrinol 8:55–58
New SA, Bolton-Smith C, Grubb DA, Reid DM (1997) Nutritional influences on bone mineral density: A cross-sectional study in premenopausal women. Am J Clin Nutr 65:1831–1839
Macdonald HM, New SA, Golden MHN, Campbell MK, Reid DM (2004) Nutritional associations with bone loss during the menopausal transition: evidence of a beneficial effect of calcium, alcohol, and fruit and vegetable nutrients and of a detrimental effect of fatty acids. Am Soc Clin Nutr 79:155–165
Gruber HE, Rude RK (2003) Alterations in osteoclast morphology following osteoprotegerin administration in the magnesium-deficient mouse. Biotechnic Histochem 78:231–236
Rude RK (1996) Magnesium metabolism. In: Bilezikian JP, Raisz L, Rodan G, Markovac J (eds) (1996) Principles of bone biology, 1st edn. Academic Press, San Diego pp 277–293
Rude RK, Adams JS, Ryzen E (1985) Low serum concentrations of 1,25-dihydroxy-vitamin D in human magnesium deficiency. J Clin Endocrinol Metab 61:933–940
Risco F, Traba MaL (1992) Influence of magnesium on the in vitro synthesis of 24, 25-dihydroxyvitamin D3 and 1-α, 25-dihydroxyvitamin D3. Magnes Res 5:5–14
Toba T, Kajita Y, Masuyama R, Takada Y, Suzuki K, Aoe S (2000) Dietary magnesium supplementation affects bone metabolkism and dynamic strength of bone in ovariectomized rats. J Nutr 130:216–220
Francheschi RT, Romano PR, Park K-H, Young J (1988) Regulation of fibronectin and collagen synthesis by 1,25-dihydroxyvitamin D3. In: Norman AW, Schaefer HG, Grigoleit HG, Herrath DV (eds) Vitamin D molecular cellular and clinical endocrinology. W. de Gruyter, Berlin pp 624–625
Kenney MA, McCoy H, Williams L (1994) Effects of magnesium deficiency on strength, mass and composition of rat femur. Calcif Tissue Int 54:44–49
Rude RK, Kirchen ME, Gruber HE, Stasky AA, Meyer MH (1998) Magnesium deficiency induces bone loss in the rat. Miner Electrolyte Metab 24:314–320
Heroux O, Peter D, Tanner A (1974) Effect of a chronic suboptimal intake of magnesium on magnesium and calcium content of bone and on bone strength of the rat. Can J Physiol Pharmacol 53:304–310
Saggese G, Federico G, Bertelloni S, Baroncelli GI, Calisti L (1991) Hypomagnesemia and the parathyroid hormone-vitamin D endocrine system in children with insulin-dependent diabetes mellitus: effect of magnesium administration. J Pediatr 118:220–225
Welsh JJ, Weaver VM (1988) Adaptation to low dietary calcium in magnesium-deficient rats. J Nutr 118:729–734
Papanicolou DA, Wilder RL, Manolagas SC, Chrousos GP (1998) The Pathophysiologic roles in interleukin-6 in human disease. Ann Int Med 128:127–137
McIntosh TK (1993) Novel pharmacologic therapies in the treatment of experimental traumatic brain injury: a review. J Am Chem Soc 89:2719–2725
Weglicki WB, Dickens BF, Wagner TL, Chemielinska JJ, Phillips TM (1996) Immunoregulation by neuropeptides in magnesium deficiency: Ex vivo effect of enhanced substance P production on circulation T lymphocytes from magnesium-deficient mice. Magnes Res 9:3–11
Weglicki WB, Mak IT, Dramer JH, Dickens BF, Cassidy MM, Stafford RE, Phillips TM (1996) Role of free radicals and substance P in magnesium deficiency. Cardiovasc Res 31:677–682
Kramer JH, Phillips TM, Weglicki WB (1997) Magnesium-deficiency-enhanced post-ischemic myocardial injury is reduced by substance P receptor blockade. J Mol Cell Cardiol 29:97–110
Malpuech-Brugere C, Nowacki W, Rock E, Gueux E, Mazur A, Rayssiguier Y (1999) Enhanced tumor necrosis factor-a production following endotoxin challenge in rats is an early event during magnesium deficiency. Biochim Biophys Acta 1453:35–40
Nakagawa M Oono H, Nishio A (2001) Enhanced productrion of IL-1β and IL-6 following endotoxin challenge in rats with dietary magnesium deficiency J Vet Med Sci 6:467–469
Malpuech-Brugere C, Nowacki W, Daveau M, Gueux E, Linard C, Rock E, Lebreton JP, Mazur A, Rayssiguier Y (2000) Inflammatory response following acute magnesium deficiency in the rat. Biochim Biophys Acta 1501:91–98
Lerner UH (2000) The role of skeletal nerve fibers in bone metabolism. The Endocrinologist 10:377–382
Rameshwar P, Ganea D, Gascon P (1994) Induction of IL-3 and granulocyte-macrophage colony stimulating factor by substance P in bone marrow cells in partially mediated through the release of IL-1 and IL-6. J Immunol 152:4044–4054
Miyaura C, Kusano K, Masuzawa T, Chaki O, Onoe Y, Aoyagi M, Sasaki T, Tamura T, Koishihara Y, Ohsugi Y, Suda T (1995) Endogenous bone-resorbing factors in estrogen deficiency: cooperative effect of IL-1β and IL-6. J Bone Miner Res 10:1365–1373
Nanes MS (2003) Tumor necrosis factor-a: molecular and cellular mechanism in skeletal pathology. Gene 321:1–15
Pacifici R (1996) Estrogens, cytokines, and pathogenesis of postmenopausal osteoporosis. J Bone Miner Res 11:1043–1051
Manolagas SC, Bellido T, Jilka RL (1995) New insights into the cellular, biochemical, and molecular basis of postmenopausal and senile osteoporosis: roles of IL-6 and gp130. Int J Immunopharmac 17:109–116
Ralston SH (1994) Analysis of gene expression in human bone biopsies by polymerase chain reaction: Evidence for enhanced cytokine expression in postmenopausal osteoporosis. J Bone Miner Res 9:883–890
Brandi ML, Hukkanen M, Umeda T, Moradi-Bidendi N, Biancche SD, Gross SS, Polak JM, MacIntyre I (1995) Bidirectional regulation of osteoclast function by nitric oxide synthase isoforms. Proc Natl Acad Sci USA 92:2954–2958
Liu CC, Yeh JK, Aloia JF (1988) Magnesium directly stimulates osteoblast proliferation. J Bone Miner Res 3[Suppl 1]:S104
Cohen L, Laor A, Kitzes R (1983) Bone magnesium, crystallinity index and state of body magnesium in subjects with senile osteoporosis, maturity-onset diabetes and women treated with contraceptive preparations. Magnesium 2:70–75
Dorup I, Flyvbjerg A, Everts ME, Clausen T (1991) Role of insulin-like growth factor-1 and growth hormone in growth inhibition induced by magnesium and zinc deficiencies. Brit J Nutr 66:505–521
Acknowledgements
This work was supported by grant 1 R01 DK060545-01 from the National Institutes of Health and funds from the Orthopaedic Hospital.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rude, R.K., Gruber, H.E., Norton, H.J. et al. Reduction of dietary magnesium by only 50% in the rat disrupts bone and mineral metabolism. Osteoporos Int 17, 1022–1032 (2006). https://doi.org/10.1007/s00198-006-0104-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-006-0104-3