Abstract
Introduction
Although it has been established that hyperthyroidism leads to reduced bone mineral density (BMD), with accelerated bone turnover promoting bone resorption in female patients, there is a dearth of data for male patients with hyperthyroidism. This study evaluated BMD and bone metabolism in male patients with Graves’ disease.
Methods
The study included 56 Japanese male patients with newly diagnosed Graves’ disease and 34 normal Japanese male control subjects of similar age and body mass index. We used dual energy x-ray absorptiometry to measure BMD at sites with different cortical/cancellous bone ratios (lumbar spine, femoral neck, and distal radius).
Results
At the lumbar spine and the distal radius, BMD and T-scores were significantly lower for patients than for controls. At the femoral neck, on the other hand, the same values were relatively, but not significantly, lower in patients than in controls. However, Z-scores at all three sites were significantly lower for patients than for controls. The Z -score at the distal radius of patients was significantly lower than that at their lumbar spine and femoral neck. In addition, Z-score at the distal radius correlated negatively with age, free thyroxine, thyroid stimulating hormone receptor antibodies, thyroid stimulating antibody, and urinary N-terminal telopeptide of type I collagen normalized by creatinine.
Conclusions
These results indicate a high prevalence of cortical bone loss in male patients with Graves’ disease, especially elderly patients. We conclude that BMD measurement is crucial in all Graves’ disease patients regardless of their gender and that the radial BMD as well as BMD at the lumbar spine and femoral neck should be monitored to effectively prevent bone loss and subsequent fracture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Reduction in bone mineral density (BMD) following hyperthyroidism in female subjects has been described in many reports [1–7]. However, as Greenspan et al. [8] mentioned in their review of the published data, far fewer studies have been conducted for male subjects. Although normal BMD has been reported in male patients with subclinical hyperthyroidism [9–11], only limited information is available on BMD in men with active hyperthyroidism. In addition, interpretation of the effects of hyperthyroidism on bone metabolism is hampered by the background of involutional osteoporosis in female patients [12]. In this study, we therefore examined the BMD of male patients, in whom the influence of involutional osteoporosis should be much less, who had newly diagnosed and untreated Graves’ disease (GD) accompanied by active hyperthyroidism.
A bone histomorphometric study of hyperthyroidism has shown that the increase in osteoclastic resorption is more prominent in cortical than in cancellous bone [13], so that bone loss, especially in cortical bone, is considered one of the characteristics of osteoporosis resulting from hyperthyroidism [6, 8]. In patients with hyperthyroidism, therefore, bone and mineral metabolism at different sites can be expected to be affected differently, depending on the cortical/cancellous bone ratio at a given site. Because previous studies have often examined BMD at a single site, however, we used dual energy x-ray absorptiometry (DXA) to measure BMD of patients with GD at three sites with different cortical/cancellous bone ratios: the lumbar spine (LS), the femoral neck (FN), and the distal third of the radius (DR). We also assessed the relationship among BMD values at the three sites and included the clinical parameters—age, thyroid hormone levels, thyroid stimulating hormone (TSH) receptor antibodies (TRAb), thyroid stimulating antibody (TSAb), and bone markers—that have often been reported as risk factors for reduced BMD in hyperthyroidism [4, 5, 14–20].
The purpose of our study was to determine 1) whether BMD decreases and bone turnover increases in male patients with overt hyperthyroidism associated with GD, as has been determined in female patients, 2) whether BMD at different sites is affected differently by hyperthyroidism, 3) which patients with overt hyperthyroidism associated with GD are more likely to have reduced BMD, and 4) whether TRAb or TSAb, or both, influence bone metabolism and BMD in untreated GD.
Subjects and methods
Subjects
The study included 56 Japanese men (mean age 43.6±10.0 years) with newly diagnosed GD who were treated at the Clinic of Rakuwakai Otowa Hospital between April 2003 and January 2005. Their clinical data are shown in Table 1. The diagnosis of GD was established on the basis of clinical signs and symptoms and laboratory test results, including positivity for TSAb and/or TRAb and an elevated technetium-99m thyroid scan (>5%). The control group comprised 34 Japanese healthy male volunteers without past or present history of thyroid disease; they were all employees of Rakuwakai Otowa Hospital and were similar to the patients in age, height, and weight (Table 1). Study and control group subjects were also similar in exercise history and calcium intake.
All subjects completed a questionnaire administered by the physician or nurse and underwent laboratory blood tests. We excluded subjects who had a history of fracture or disease (liver disease, renal dysfunction, malignancy, diabetes mellitus, hyperparathyroidism, hypercorticoidism, or hypogonadism) and those taking medications that could influence bone metabolism (active vitamin D3, bisphosphonates, calcitonin, testosterones, steroids, thyroid hormones, diuretics, heparin, or anticonvulsants). All subjects underwent plain x-ray (anteroposterior and lateral views) of the LS, and those found to have scoliosis, compression fractures, or ectopic calcifications that could interfere with the bone mineral results were excluded. None of the subjects were smokers or alcoholics.
This study was approved by the ethics committee of Rakuwakai Otowa Hospital, and all participants provided written informed consent.
BMD measurements
BMD was measured at the LS (L2-L4), the FN, and DR by DXA (Hologic QDR 4,500c; Hologic, Waltham, MA, USA). To avoid technical discrepancies, the same operator measured all the subjects. Values of BMD at the LS were calculated as the mean of those at L2-L4, and T-scores and Z-scores were calculated on the basis of the normal reference values of the age- and gender-matched Japanese group provided by the DXA system manufacturer.
Biochemical measurements
Serum samples were obtained before 0800 after overnight fasting and were immediately processed and kept frozen at −20°C until the assays were done. Serum free T3 (FT3), free T4 (FT4), and TSH were measured with the aid of an electrochemiluminescence immunoassay (ECLUSISU; Roche Diagnostics, Tokyo, Japan; normal values: FT3, 2.30–4.30 pg/ml; FT4, 0.90–1.70 ng/dl; TSH 0.500–5.000 μIU/ml). The minimum detection limit of the TSH assay was 0.005 μIU/ml. TRAb was measured with a radioreceptor assay (COSMIC III; Cosmic, Tokyo, Japan; normal range 0.0–15.0%), and TSAb with a bioassay radioimmunoassay (TSAB-Kit-Yamasa; Yamasa, Chiba, Japan; normal range <180%). Serum calcium, phosphate, creatinine, and alkaline phosphatase (ALP) were measured by using standard laboratory methods. Bone-specific alkaline phosphatase (BAP) was measured with an enzyme immunoassay kit (Osteolinks-BAP; Sumitomo Pharmaceuticals, Tokyo, Japan; normal range 13.0–33.9 U/l) as a marker of bone formation. Urinary N-terminal telopeptide of type I collagen normalized by creatinine (U.NTx) was measured in the morning in the second voided urine sample by means of an enzyme-linked immunosorbent assay (OSTEOMARK; Mochida Pharmaceutical, Tokyo, Japan; normal range 13.0–66.2 nmolBCE/mmolCre) as a marker of bone resorption.
Statistical analysis
Data were analyzed by t-test for differences between two groups, by one-way factorial ANOVA and Fisher’s protected least significant difference (PLSD) method for differences among three groups, and by Pearson’s correlation test for determining correlations. Statistics were calculated with Statview version 4.0 (Abacus Concepts, Berkeley, CA, USA). A P-value <0.05 was considered statistically significant.
Results
Table 1 shows a comparison of GD patients and controls. There were no significant differences between the two groups in age, height, weight, or body mass index (BMI). However, serum calcium, ALP, BAP, and U.NTx levels of the GD patients were significantly higher than those of controls. U.NTx was about four times higher, and BAP was about twice as high. The levels of thyroid hormones were also elevated, while TSH levels were suppressed below sensitivity in all the patients with GD.
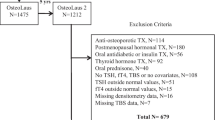
Table 2 and Fig. 1 show a comparison of BMD and T- and Z-scores for the patient and control groups. At the LS and the DR, BMD and T-scores were significantly lower for patients than for controls. At the FN, on the other hand, the same values were relatively, but not significantly, lower in patients than in controls. However, Z-scores at all three sites were significantly lower for patients than for controls.
Figure 2a,b shows comparisons of T- and Z-scores among different sites in patients with GD, analyzed by one-way factorial ANOVA and Fisher’s PLSD test. Both T-score and Z-score at the DR were significantly lower than those at the LS and FN (P=0.0126 and 0.0008 for T-score, and P<0.0001 and P<0.0001 for Z-score, respectively), whereas neither T-score nor Z-score showed any marked differences between the LS and the FN.
a Comparison of T-scores at the lumbar spine, femoral neck, and distal radius of patients with Graves’ disease (white columns). b Comparison of Z-scores at the lumbar spine, femoral neck, and distal radius of patients with Graves’ disease (white columns). Black columns show data of controls. Each column represents the mean value ± SEM. *P<0.05, †P<0.01
Table 3 shows correlations of BMD, T-score, and Z-score with age, height, weight, BMI, and the biochemical parameters in patients with GD. There was a significant negative correlation between age and both BMD and T-score at all three sites. Otherwise, however, there was no statistically significant correlation at either the LS or the FN. On the other hand, Z-scores as well as BMD and T-scores at the DR correlated negatively with FT4, TRAb, TSAb, and U.NTx, but not so at the LS or the FN. These significant negative correlations of the Z-score at the DR with age, FT4, TRAb, TSAb, and U.NTx are shown in Fig. 3.
Correlations between Z-score at the radius and clinical parameters (a age, b FT4, c TSAb, d TRAb, e U.NTx) and between TSAb and U.NTx (f) for patients with Graves’ disease. For each figure, Z-score measurements at the radius were plotted against the clinical parameters a∼e, and U.NTx measurements were plotted against TSAb (f). The line reflects the regression, and r mean the correlation coefficients and P-values for correlations between Z-score at the radius and the clinical parameters (a–e), and between TSAb and U.NTx (f)
Furthermore, multiple regression analysis was performed with the Z-score at the DR as the dependent variable and all the clinical parameters listed in Table 3 as the independent variables. A forward stepwise procedure identified two variables, age and FT4, as significant predictors in the following equation:
Table 4 shows correlations of bone metabolic markers with thyroid function and thyroid autoantibodies. There was a significant positive correlation between TSAb and U.NTx (Fig. 3). Otherwise, relatively positive correlations between bone metabolic markers with thyroid function and thyroid autoantibodies were found, but none of them reached significance.
Discussion
Most [1–7, 14–16, 21], but not all [20, 22], studies have reported a decrease in BMD in female patients with active hyperthyroidism, as Greenspan et al. [8] reviewed in a metaanalysis of the published data. However, fewer studies have been conducted for men. Only small numbers (from two to eight) of male patients with hyperthyroidism have been examined in some previous studies [14, 15, 20, 21]. In other studies, separate data for the male patients or the actual values of their BMD were unfortunately not given [16, 23]. Indeed, BMD of male subjects on TSH suppressive and replacement levothyroxine therapy or with subclinical hyperthyroidism has been examined in some papers [9–11]. However, there is still little information available in the literature about the BMD of male patients with active hyperthyroidism.
In the study presented here, we examined men with untreated GD accompanied by active hyperthyroidism and found that their BMD (Z-scores) at all three sites was significantly lower than that of age-matched controls. Toh et al. [24], using single photon absorptiometry, also observed significant radial bone loss in 24 male patients with active hyperthyroidism. Our results agree with theirs, thus suggesting the importance of measuring the BMD of male patients with thyrotoxic GD. There is ample evidence to indicate that osteoporosis in men is already a public health problem, and most osteoporotic men were found to have secondary causes of osteoporosis, including hyperthyroidism [25]. Therefore, we should not underestimate the significance of reduced BMD in male patients with hyperthyroidism.
We were able to show that the Z-score is lowest at the DR among the three sites (LS, FN, and DR) we studied in male patients with GD. In addition, we found a negative correlation between the Z-score at the DR and FT4, TRAb, and TSAb in our patients. These results suggest that selective loss of cortical rather than cancellous bone may occur in GD. This selective cortical bone loss in hyperthyroidism has often been postulated in the literature [6, 8, 13], although again mostly in female patients, and these findings are supported by a great deal of evidence in rats [26]. Bone morphometric studies have also demonstrated that enhanced osteoclastic bone resorption is more prominent in cortical than in cancellous bone [13], which may lead to an increased risk of forearm fracture in patients with hyperthyroidism [27, 28]. These observations are compatible with our results and suggest the clinical importance of evaluating BMD at the radius.
Likewise, an increased risk of hip fracture [27–31] and reduced BMD at the FN [1, 3, 6, 7, 15, 16, 21], which contains much cortical bone, has been reported in mostly female patients with hyperthyroidism. In our study, however, BMD at the FN showed no significant difference between male patients with GD and matched controls. A possible reason might be the higher impact of gravity or exercise on bone mass, or the difference in the cortical-cancellous bone ratio between FN and DR (FN<DR). This finding agrees the results of some previous studies that showed unaltered BMD at the FN [2, 14, 20, 22]. It is different, however, from the findings of other studies [1, 3, 6, 7, 15, 16, 21] that show a reduction in BMD of the FN. Gender and racial differences of the subjects or the severity and duration of hyperthyroidism could explain these discrepancies between our study and other investigations [20].
It is clinically important to predict which patients with GD are at higher risk of losing bone, although that remains unclear at present [20]. We found a significant correlation between BMD at the DR and age, FT4, TRAb, TSAb, and U.NTx. After stepwise multiple regression analyses, higher FT4 and higher age remained as independent risk factors for reduced BMD at the DR in our study. Mudde et al. [17] also reported the significant inverse relationship between FT4 and Z-score at the DR in 23 women with subclinical hyperthyroidism. On the other hand, Fraser et al. [18] also reported that the loss of metacarpal bone mass worsened with age. Furthermore, Vestergaard et al. [29] concluded in their review of the literature that the increased risk of fractures in patients with hyperthyroidism [27, 28, 30, 31] became larger with advancing age and that the close relationship between observed and estimated fracture risk from BMD could indicate that most of the changes in fracture risk were related to changes in BMD. These results indicate the importance of examining BMD at the DR as well as at the LS or the FN, especially in elderly patients with active hyperthyroidism, in the context of fracture prevention.
Both higher TRAb and TSAb significantly correlated with a reduction in BMD at the DR in our study. In addition, higher TSAb significantly correlated with higher U.NTx. These results suggest some deleterious effects of TRAb and TSAb on bone metabolism, probably via TSH receptors in osteoblasts or osteoclasts [32, 33]. Previous studies have suggested that the past history of GD itself, not the current state of thyroid function, is responsible for bone loss in women receiving long-term levothyroxine therapy [34], indicating some autoimmune effects of TRAb on bone metabolism. A decreased fracture risk in patients with hyperthyroidism treated with surgery and an increased fracture risk in patients treated with radioiodine [28] could also support this hypothesis of TRAb being involved in bone metabolism, considering that surgical treatment of GD is associated with a less pronounced elevation of TRAb, whereas radioiodine treatment is associated with its higher elevation [35]. In addition, Wakasugi et al. [15] and Jodar et al. [16] previously showed significant negative correlation between TRAb and lumbar BMD in hyperthyroid patients, and Kumeda et al. [19] reported that TRAb did not correlate with FT3 or FT4, but correlated closely with bone metabolic markers in GD. They suggested direct adverse effect of higher TRAb on bone metabolism regardless of thyroid function [15, 16, 19].
Furthermore, it has been recently demonstrated that TSH directly affects bone metabolism via the TSH receptor found on osteoblast and osteoclast precursors in mice [32]. These studies support our findings of an inverse correlation between both TRAb and TSAb and BMD at the DR, and a positive correlation between TSAb and U.NTx. One of the questions would concern why, if these antibodies play a direct role in reducing BMD by accelerating bone turnover in similar mechanisms to TSH, the present results seem to be opposite those reported in the study by Abe et al. [32], where reduced TSH receptor expression led to profound osteoporosis, suggesting an inhibitory effect of TSH on bone turnover. However, more recently, Morimura et al. [33] showed that TSH positively regulates intracellular T3 production by controlling type 2 iodothyronine deiodinase in human osteoblasts. It is, therefore, tempting to speculate that both higher TSH receptor antibodies and lower TSH might be directly associated with lower bone mass, but not in the same way. Namely, higher TSH receptor antibodies might overproduce intracellular T3 to decrease bone mass by accelerating bone turnover while lower TSH could hardly produce intracellular T3, essential for bone growth, to decrease bone mass as well. Alternatively, higher TSH receptor antibodies might reduce bone by their effect of lowering TSH [36].
Further studies are needed to clarify these issues. Although we cannot completely exclude the possibility that these correlations in our study may have only reflected the correlation with the severity of hyperthyroidism, as Kumeda et al. [19] stated, we believe our results are clinically important in indicating that efforts should be directed not only to early restoration of euthyroidism but also to correction of TRAb and TSAb to prevent bone loss in GD.
It also remains unclear whether the gender difference in the effects of thyroid hormone on BMD exists. Compared with previous reports, our patients' Z-scores seem to be rather high, which may indicate less susceptibility to hyperthyroid-induced bone loss in male patients. Greenspan et al. [8] also referred to the possibility that the influence of excessive thyroid hormones on bone is not as striking in men as in women. And more recently, Schneider et al. [37] showed in their review of the literature that BMD in men did not decline as a result of TSH suppression in several studies [8–10], whereas in women it has often been reported to diminish [8]. In addition, while several animal studies have shown that T3 reduced BMD in ovariectomized female rats [38], Fitts et al. [38] found that T3 alone had no effect on BMD in male rats. Larger studies are needed to identify gender differences, if any, in the effects of hyperthyroidism on bone metabolism.
In summary, we found a significant reduction in the BMD of male patients with hyperthyroidism associated with GD. We also found that the Z-score at the DR was significantly lower than that at the LS and FN in male patients with GD. The Z-score at the DR correlated negatively with age, FT4, TRAb, TSAb, and U.NTx, and TSAb correlated positively with U.NTx in male patients with GD. These results indicate a high prevalence of cortical bone loss in male patients with GD, especially elderly patients. We conclude that BMD measurement is crucial in all Graves’ patients regardless of gender and that the radial BMD as well as that in the LS and the FN should be monitored to effectively prevent bone loss and subsequent fracture.
References
Campos-Pastor MM, Munoz-Torres M, Escobar-Jimenez F, Ruiz de Almodovar M, Jodar Gimeno E (1993) Bone mass in females with different thyroid disorders: influence of menopausal status. Bone Miner 21:1–8
Diamond T, Vine J, Smart R, Butler P (1994) Thyrotoxic bone disease in women: a potentially reversible disorder. Ann Intern Med 120:8–11
Gomez Acotto C, Schott AM, Hans D, Niepomniszcze H, Mautalen CA, Meunier PJ (1998) Hyperthyroidism influences ultrasound bone measurement on the Os calcis. Osteoporos Int 8:455–459
Olkawa M, Kushida K, Takahashi M, Ohishi T, Hoshino H, Suzuki M, Ogihara H, Ishigaki J, Inoue T (1999) Bone turnover and cortical bone mineral density in the distal radius in patients with hyperthyroidism being treated with antithyroid drugs for various periods of time. Clin Endocrinol (Oxf) 50:171–176
Mora S, Pitukcheewanont P, Kaufman FR, Nelson JC, Gilsanz V (1999) Biochemical markers of bone turnover and the volume and the density of bone in children at different stages of sexual development. J Bone Miner Res 14:1664–1671
Ben-Shlomo A, Hagag P, Evans S, Weiss M (2001) Early postmenopausal bone loss in hyperthyroidism. Maturitas 39:19–27
Karga H, Papapetrou PD, Korakovouni A, Papandroulaki F, Polymeris A, Pampouras G (2004) Bone mineral density in hyperthyroidism. Clin Endocrinol (Oxf) 61:466–472
Greenspan SL, Greenspan FS (1999) The effect of thyroid hormone on skeletal integrity. Ann Intern Med 130:750–758
Marcocci C, Golia F, Vignali E, Pinchera A (1997) Skeletal integrity in men chronically treated with suppressive doses of L-thyroxine. J Bone Miner Res 12:72–77
Rosen HN, Moses AC, Garber J, Ross DS, Lee SL, Ferguson L, Chen V, Lee K, Greenspan SL (1998) Randomized trial of pamidronate in patients with thyroid cancer: bone density is not reduced by suppressive doses of thyroxine, but is increased by cyclic intravenous pamidronate. J Clin Endocrinol Metab 83:2324–2330
Jodar E, Martinez-Diaz-Guerra G, Azriel S, Hawkins F (2001) Bone mineral density in male patients with L-thyroxine suppressive therapy and Graves disease. Calcif Tissue Int 69:84–87
Riggs BL, Melton LJ 3rd (1986) Involutional osteoporosis. N Engl J Med 26:1676–1686
Mosekilde L, Eriksen EF, Charles P (1990) Effects of thyroid hormones on bone and mineral metabolism. Endocrinol Metab Clin North Am 19:35–63
Lee MS, Kim SY, Lee MC, Cho BY, Lee HK, Koh CS, Min HK (1990) Negative correlation between the change in bone mineral density and serum osteocalcin in patients with hyperthyroidism. J Clin Endocrinol Metab 70:766–770
Wakasugi M, Wakao R, Tawata M, Gan N, Koizumi K, Onaya T (1993) Bone mineral density in patients with hyperthyroidism measured by dual energy X-ray absorptiometry. Clin Endocrinol (Oxf) 38:283–286
Jodar E, Munoz-Torres M, Escobar-Jimenez F, Quesada-Charneco M, Lund del Castillo JD (1997) Bone loss in hyperthyroid patients and in former hyperthyroid patients controlled on medical therapy: influence of aetiology and menopause. Clin Endocrinol (Oxf) 47:279–285
Mudde AH, Reijnders FJ, Kruseman AC (1992) Peripheral bone density in women with untreated multinodular goitre. Clin Endocrinol (Oxf) 37:35–39
Fraser SA, Anderson JB, Smith DA, Wilson GM (1971) Osteoporosis and fractures following thyrotoxicosis. Lancet 1:981–983
Kumeda Y, Inaba M, Tahara H, Kurioka Y, Ishikawa T, Morii H, Nishizawa Y (2000) Persistent increase in bone turnover in Graves’ patients with subclinical hyperthyroidism. J Clin Endocrinol Metab 85:4157–4161
Siddiqi A, Burrin JM, Noonan K, James I, Wood DF, Price CP, Monson JP (1997) A longitudinal study of markers of bone turnover in Graves’ disease and their value in predicting bone mineral density. J Clin Endocrinol Metab 82:753–759
Lucidarme N, Ruiz JC, Czernichow P, Leger J (2000) Reduced bone mineral density at diagnosis and bone mineral recovery during treatment in children with Graves’ disease. J Pediatr 137:56–62
Ugur-Altun B, Altun A, Arikan E, Guldiken S, Tugrul A (2003) Relationships existing between the serum cytokine levels and bone mineral density in women in the premenopausal period affected by Graves’ disease with subclinical hyperthyroidism. Endocr Res 29:389–398
Fittipaldi MR, Fonderico F, Vitale G, Ciccarelli A, Lupoli GA, Cascella T, Panico A, Lupoli G (2002) Osteoporosis treatment in elderly hyperthyroid male patients. J Endocrinol Invest 25:98–100
Toh SH, Claunch BC, Brown PH (1985) Effect of hyperthyroidism and its treatment on bone mineral content. Arch Intern Med 145:883–886
Bilezikian JP (1999) Osteoporosis in men. J Clin Endocrinol Metab 84:3431–3434
Milne M, Kang MI, Quail JM, Baran DT (1998) Thyroid hormone excess increases insulin-like growth factor I transcripts in bone marrow cell cultures: divergent effects on vertebral and femoral cell cultures. Endocrinology 139:2527–2534
Vestergaard P, Rejnmark L, Weeke J, Mosekilde L (2000) Fracture risk in patients treated for hyperthyroidism. Thyroid 10:341–348
Vestergaard P, Mosekilde L (2002) Fractures in patients with hyperthyroidism and hypothyroidism: a nationwide follow-up study in 16,249 patients. Thyroid 12:411–419
Vestergaard P, Mosekilde L (2003) Hyperthyroidism, bone mineral, and fracture risk-a meta-analysis. Thyroid 13:585–593
Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, Cauley J, Black D, Vogt TM (1995) Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med 332:767–773
Wejda B, Hintze G, Katschinski B, Olbricht T, Benker G (1995) Hip fractures and the thyroid: a case-control study. J Intern Med 237:241–247
Abe E, Marians RC, Yu W, Wu XB, Ando T, Li Y, Iqbal J, Eldeiry L, Rajendren G, Blair HC, Davies TF, Zaidi M (2003) TSH is a negative regulator of skeletal remodeling. Cell 115:151–162
Morimura T, Tsunekawa K, Kasahara T, Seki K, Ogiwara T, Mori M, Murakami M (2005) Expression of type 2 iodothyronine deiodinase in human osteoblast is stimulated by thyrotropin. Endocrinology 146:2077–2084
Greenspan SL, Greenspan FS, Resnick NM, Block JE, Friedlander AL, Genant HK (1991) Skeletal integrity in premenopausal and postmenopausal women receiving long-term L-thyroxine therapy. Am J Med 91:5–14
Torring O, Tallstedt L, Wallin G, Lundell G, Ljunggren JG, Taube A, Saaf M, Hamberger B (1996) Graves’ hyperthyroidism: treatment with antithyroid drugs, surgery, or radioiodine–a prospective, randomized study. Thyroid Study Group. J Clin Endocrinol Metab 81:2986–2993
Brokken LJ, Wiersinga WM, Prummel MF (2003) Thyrotropin receptor autoantibodies are associated with continued thyrotropin suppression in treated euthyroid Graves’ disease patients. J Clin Endocrinol Metab 88:4135–4138
Schneider R, Reiners C (2003) The effect of levothyroxine therapy on bone mineral density: a systematic review of the literature. Exp Clin Endocrinol Diabetes 111:455–470
Fitts JM, Klein RM, Powers CA (2001) Estrogen and tamoxifen interplay with T(3) in male rats: pharmacologically distinct classes of estrogen responses affecting growth, bone, and lipid metabolism, and their relation to serum GH and IGF-I. Endocrinology 142:4223–4235
Acknowledgements
This work was supported in part by a Grant-in-Aid from the Japanese Ministry of Health, Labour and Welfare (#H17-Saisei-003), the Japanese Ministry of Education, Science, Sports, and Culture (#17590958), the Smoking Research Foundation, and the Foundation of Growth Science.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Majima, T., Komatsu, Y., Doi, K. et al. Negative correlation between bone mineral density and TSH receptor antibodies in male patients with untreated Graves’ disease. Osteoporos Int 17, 1103–1110 (2006). https://doi.org/10.1007/s00198-006-0091-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-006-0091-4