Abstract
Osteoporosis is the most common metabolic bone disease in humans. It is a special concern not only among postmenopausal women, but men as well. In developing countries where there are meager resources, it will definitely be helpful to search for ways to identify patients with low bone mineral density who have a high risk of future fractures. These people need to be identified for treatment consideration in order to reduce the incidence of the disease and its complications. A simple risk index called the Osteoporosis Screening Tool for Asians (OSTA), based only on two variables, age and body weight, performed well in identifying the risk of osteoporosis among postmenopausal women. This index has been validated in Japan, Korea and other Caucasian populations as a useful tool in identifying individuals who will require BMD measurement. This is the first study that validated the said index in 1,597 Filipino women and men referred to a tertiary center for BMD measurement. It had sensitivity of 97 and 90% and specificity of 59 and 66% with areas under the curve of 0.8506 and 0.8475, respectively, for women and men. We conclude that OSTA performed just as well or even better than other indices used in other populations to identify individuals who are at varying degrees of risk for osteoporosis. The tool also proves to be a useful and practical guide to help clinicians to be more prudent and judicious in employing bone mineral density measurement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recently, much has been published about osteoporosis and the tremendous economic burden it causes worldwide. With the aging population and the projected surge of increase in the prevalence of the disease, much should be done to identify individuals who are at high risk of having osteoporosis. Despite the remarkable advancement in technology, the developed as well as Third World developing countries are limited in the maximal utilization of bone mineral density measurement. Limited access to central BMD machines as well as their costs preclude their use.
Several clinical risk indices were developed based on population samples that consist primarily of Caucasian postmenopausal women to help identify and determine which patients are at increased risk of having osteoporosis. Most of these indices yielded high sensitivity (~90%) with acceptable specificity (~40–50%) [1, 2, 3]. A simple tool was developed in 2001 primarily to identify Asian women at increased risk for osteoporosis [4]. Of the different risk factors identified and considered, the risk index yielded a final tool based only on age and body weight after multiple variable regression analysis. It had a sensitivity of 90% and specificity of 45% and was validated in a population-based sample of postmenopausal Japanese women [5]. This tool was similarly validated in Korean [6] and Belgian women.
Earlier studies presented in the World Congress on Osteoporosis 2000 showed that there was variable prevalence of low bone mass among peri- and postmenopausal Filipino women [7, 8]. Of the respondents who had BMD at the lower 16% of the normal range, 20–26% were between 20−40 years of age, and 13.5% were between 40–49 years of age. Though most of the studies on osteoporosis were focused on postmenopausal women, emphasis should likewise be given to women before reaching their menopausal states. Identifying individuals at an earlier stage before osteoporosis sets in is just as important a step in the overall approach to the diagnosis as well as the treatment of osteoporosis.
The objectives of the current study were to determine the prevalence of osteoporosis using the Osteoporosis Screening Tool for Asians (OSTA) and to evaluate and validate the tool in a cohort of Filipino women and men. This is also the first study that has attempted to assess the utility of the screening tool in a cohort of men.
Materials and methods
The study included the existing data from the medical records of all adults ≥40 years of age who had their central bone densitometry measurements done at a tertiary referral hospital in Manila, The Philippines, from January 2001–June 2004. Patients with pre-existing conditions that affected bone mass, i.e., chronic corticosteroid intake (>7.5 mg/day for 1 year), hyperthyroidism, chronic renal disease, inflammatory arthropathy, i.e., rheumatoid arthritis, ankylosing spondyloarthropathy, fragility fractures, taking anti-resorptive agents and/or hormonal replacement therapy within the recent 6 months were excluded from the study. The risk tool was calculated based on the previously reported (actual body weight–age in years) 0.2, and the decimal digits were dropped (truncated to the integer). Femoral neck BMD was measured using the GE Lunar DPX-IQ. BMD T-scores were based on the number of the standard deviation below the mean for young healthy Asian Chinese women (mean =0.90 g/cm2; SD=0.12 g/cm2) and men (mean =0.950 g/cm2; SD=0.13 g/cm2). The risk categories were classified into low risk (values >−1), medium risk (values between −4 and −1) and high risk (values <−4).
Results
The mean age of the women was 59.8 years (range, 40–89 years), with the average time since menopause 15.75 years (Tables 1, 2). The overall prevalence of osteoporosis in the referred group of women (BMD <70% of young adult women) was 11.26%. The prevalence of osteoporosis among women 40–49 years of age was 0.38% (1/260), 4.3% (19/446) in those between 50–59 years, 12.37% (61/493) between 60–69 years and 31.58% (84/266) for those 70 years and beyond (Table 3). Using the OSTA, the prevalence of osteoporosis among the low risk group was 0.52% (4/774), 12.32% (84/541) for the medium risk group and 51.33% (77/150) for the high-risk group (Table 4).
The mean age of men was 62.9 years (range, 40–89 years), the mean height and weight 1.65 m and 66.52 kg, respectively (Table 1). The overall prevalence of osteoporosis in the referred group of men (BMD <70% of young adult men) was 9.1%. There were no cases of osteoporosis among men 40–49 years of age. The prevalence of osteoporosis among those between 50–59 years was 3.8% (1/26). Between 60–69 years, 10.53% (4/38) were osteoporotic; for those ≥70 years of age, the prevalence was 15.9% (7/44) (Table 3). Using the OSTA, the prevalence of osteoporosis among the low risk group was 1.23% (1/81), 10.81% (4/37) for the medium risk group and 50% (7/14) for the high-risk group (Table 4).
Performance of OSTA in identifying women and men with BMD T-scores ≤−2.0 yielded sensitivities of 89.61 and 72% with specificities of 64.13 and 69.16%, respectively (Table 5). The AUROC curves were 0.8124 for women and 0.7540 for men.
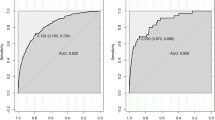
Using the same tool in recognition of women and men with BMD T-scores ≤−2.5 yielded sensitivities of 97.56 and 90.91% with specificities of 59.19 and 66.12%, respectively (Table 6). The AUROC curves were 0.8506 for females (Fig. 1) and 0.8475 for males (Fig. 2). The prevalence of osteoporosis among the referred postmenopausal Filipino women was similarly low to those seen in Japanese and Korean postmenopausal women (Table 7).
Discussion
It is universally accepted that osteoporosis is one of the major causes of morbidity and mortality among postmenopausal women and men worldwide. Bone densitometry remains the standard method for diagnosing osteoporosis preceding a fracture and therefore acts as a powerful tool in convincing health care practitioners to prescribe osteoporosis treatments. Much still needs to be done to increase the level of awareness of different sectors of society and health practitioners globally. Rates of diagnosis and treatment of osteoporosis have remained low, even at this time when effective therapies are very much available. A cross-sectional survey of primary care physicians practicing in New England showed that low referral rates for bone densitometry studies were primarily due to physicians spending less than 50% of their time in patient care and secondly to their seeing a low proportion of postmenopausal women [9].
Based on the Family Income and Expenditure Survey done by the Philippine National Statistics Office in 2000, the primary source for medical expenditure largely comes from private sourcing (80%)—out-of-pocket payment by the people—while 7% comes from social health insurance and 13% from other sources. With this kind of health care system, measures should be taken in order to maximize the limited finances of the people. Other than the issue of cost of BMD, one factor in considering having a central BMD done in our country is its accessibility. Considering the inherent geographical characteristics of The Philippines, the country is an archipelago made up of several thousand islands and islets. More than 80% of the central BMD machines are situated in the heart of the country’s capital, Manila. The populace from up north to down south needs to board an aircraft or cross the sea in order to have access to BMD measurement. Henceforth, prudent and judicious use of BMD measurement should be reinforced among the healthcare practitioners as part of their patient care.
The foremost purpose of a risk assessment tool for osteoporosis is to identify individuals at high risk for osteoporosis for whom BMD measurement will be of the utmost clinical relevance not only in the definite diagnosis and fracture risk prediction, but also when obtaining this information will ultimately influence the treatment decision. With almost half of the referred women and men having low bone mass in this study, we need to focus on ways to address lifestyle risk factors in order to prevent further deterioration. Almost 10% of the individuals whose BMD was in the lower 16% of the normal range belong to the 40–49-year-old age group.
This study, however, has some limitations. Since the data collected are from a tertiary referral center, the tool might perform differently in a general community. On the one hand, this might not be the case since the respondents were residents from different regions of the country. Be that as it may, a potential bias on patient selection is highly probable because only those who were able to have access to BMD measurement were well represented here.
With the high sensitivity and acceptable specificity of this screening tool for the diagnosis of osteoporosis in both women and men, the authors hereby recommend that all general care practitioners as well as specialists make use of this simple and practical tool in their daily patient care. Utilization of this tool will definitely reduce unnecessary bone density examinations in those who are at lowest risk.
References
Cadarette SM, Jaglal SB, Murray TM (1999) Validation of the simple calculated osteoporosis risk estimation (SCORE) for patient selection for bone densitometry. Osteoporos Int 10:85–90
Cadarette SM, Jaglal SB, Kreiger N, et al (2000) Development and validation of the osteoporosis risk assessment instrument to facilitate selection of women for bone densitometry. Can Med Assoc J 162:1289–1294
Black DM, Palermo L, Abbott T, Johnell O (1998) SOFSURF: a simple useful risk factory system can identify the large majority of women with osteoporosis. Bone 23:S605
Koh L, Ben Sedrine W, Torralba T, et al (2001) A simple tool to identify Asian women at increased risk of osteoporosis. Osteoporos Int 12:699–705
Fujiwara S, Masunari N, Suzuki G, et al (2001) Performance of osteoporosis risk indices in a Japanese population. Curr Ther Res 62:586–594
Park HM, Ben Sedrine W, Reginster JY, Ross PD (2003) Korean experience with the OSTA risk index for osteoporosis. J Clin Densitom 6:251–258
Torralba TP, Navarra SV, Saavedra ST, Bermudez CC, Ong MT, Dy SH, Asis LM (2000) Prevalence of low bone mass among young Filipino female nurses at Santo Tomas University Hospital. Publication no. 107, poster presentation from the June 2000 World Congress on Osteoporosis, Chicago
Torralba TP, Saavedra ST, Bermudez CC, Ong MT, Gomez HS, Navarra SV, Dy SH, Asis LM (2000) Prevlance of osteoporosis among perimenopausal and postmenopausal Filipino women studied at Santo Tomas University Hospital. Publication no. 108, poster presentation from the June 2000 World Congress on Osteoporosis, Chicago
Solomon DH, Connelly MT, Rosen CJ, Dawson-Hughes B, et al (2003) Factors related to the use of bone densitometry: survey responses of 494 primary care physicians in New England. Osteoporos Int 14:123–129
Acknowledgements
We would like to thank Ms. Sarah Jane Dy for her help with data retrieval and Ms. Olivia Sison for statistical analysis of the data.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li-Yu, J.T., Llamado, L.J. & Torralba, T.P. Validation of OSTA among Filipinos. Osteoporos Int 16, 1789–1793 (2005). https://doi.org/10.1007/s00198-005-1929-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-005-1929-x