Abstract
The prevalence of osteoporosis is high among postmenopausal women and individuals sustaining a spinal cord injury (SCI). We assessed the effects of estrogen loss and unloading on the trabecular bone of the knee in women. Pre- and postmenopausal ambulatory women (n=17) were compared to pre- and postmenopausal women with SCI (n=20). High-resolution magnetic resonance imaging was used to compare groups on apparent measures of trabecular bone volume, trabecular number, trabecular spacing, and trabecular thickness in the distal femur and proximal tibia, regions with a high proportion of trabecular bone and the most common fracture site for SCI patients. Trabecular bone was deteriorated in women with SCI compared to ambulatory women. SCI groups had fewer, (−19 and −26% less) and thinner trabeculae (−6%) that were spaced further apart (40% and 62% more space between structures) resulting in less trabecular bone volume (−22% and −33%) compared to the ambulatory groups (tibia and femur, respectively). Postmenopausal women with SCI also had 34% greater trabecular spacing in the tibia compared to the 40-year-old premenopausal women with SCI, showing an interaction between unloading and estrogen loss. Middle-aged postmenopausal, ambulatory women, not taking estrogen or medications that affect bone, did not show the deteriorated trabeculae that were evident in women with SCI, nor did they show differences in distal femur and proximal tibia trabeculae compared to a premenopausal group. We conclude that the effect of unloading on bone architecture is greater than that of estrogen loss in middle-aged women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Estrogen and loading are conceivably the most critical determinants of bone health. Menopause causes women to experience estrogen withdrawal while a complete spinal cord injury (SCI) results in the most extreme form of unloading where people are immediately and permanently paralyzed below their level of injury. Declines in skeletal structure for postmenopausal women are 1–3% per year for cortical bone and 3–5% per year for trabecular bone during the first 5 years or so after cessation of menses [1]. Over the first 2 years following SCI, bone mineral declines ~20–25% in areas composed of cortical bone such as the femoral shaft and ~55% in areas comprised mainly of trabecular bone such as the proximal tibia [2]. Early work has also shown ~33% less trabecular bone volume in the iliac crest 6 months after spinal cord injury [3]. The effect of unloading, estrogen loss, and unloading plus estrogen loss has been investigated in female animals [4,5,6,7,8], but data are lacking in women.
Osteoporosis is a disease characterized by low bone mass and microarchitectural deterioration of bone tissue [9]; however, most studies have primarily focused on changes in bone mass alone. Studying microarchitectural deterioration in postmenopausal women and women with SCI presents a rare opportunity to examine the influences of estrogen loss and unloading. Postmenopausal women with SCI also provide a unique circumstance to examine the influence of both factors simultaneously. While areal bone mineral density (aBMD) is the current gold standard measure of osteoporosis and the paramount predictor of fracture, it does not indicate structural changes. Most notably, it does not indicate trabecular bone architecture. Examining microarchitecture is important because there is an overlap in BMD between those that fracture and those that do not [10,11,12]. In addition, the lost structures may not be re-established because lamellar bone (i.e. trabeculae) only forms on existing bone, thus the removal appears to be irreversible [13]. Furthermore, advances in imaging technology now allow in vivo, non-invasive assessment of trabecular bone through large areas of bone in the knee, calcaneus, and radius via high resolution magnetic resonance imaging (MRI).
Postmenopausal estrogen-free women and women with SCI are two at-risk populations for fractures resulting from bone loss. Indeed, in women over 50 years of age, there is a 20% prevalence of osteoporosis at the hip and a 34–50% prevalence of osteopenia [14], contributing to a 40% lifetime risk of fracture of the hip, radius or spine [15]. Individuals with SCI have alarmingly high rates of osteoporosis. Osteoporosis is observed in approximately 75% of patients with complete SCI [16, 17]. This is associated with a 5- and 23-fold greater fracture rate in the leg and femur, respectively, when compared to able-bodied individuals [18]. Up to 35% of the SCI population will experience a fracture in their lifetime [19,20]. These high rates of fracture in SCI are similar to the rates reported for postmenopausal women. Bone changes in postmenopausal women and spinal cord injured women purportedly occur as a result of different factors, which suggest that women with SCI who also experience menopause may face more deteriorated bone than that observed after menopause or SCI alone. Bone loss following unloading occurs at areas below the level of injury for individuals with SCI such as the femur and the tibia [2,21], sparing regions such as the distal radius or spine that do not experience altered loading [2,22]. In contrast, menopause and/or aging show dramatic losses in vertebral [23,24] and radial [25,26] skeletal mass and structure along with losses in regions such as the proximal femur [27] and calcaneous [23,28]. Therefore, although bone deterioration is elevated in regions comprised largely of trabecular bone in both populations, different skeletal sites are affected in women ensuing SCI and after menopause.
The purpose of this study was to compare the effects of SCI and/or menopause on trabecular bone around the knee, the bone type particularly affected by estrogen and loading. We postulated more diminished trabeculae in women with SCI. In addition, we sought to determine the effect of menopause on trabeculae in women with SCI, postulating that trabeculae would be more deteriorated in postmenopausal compared to premenopausal women with SCI. Lastly, we tested the purported relationship between skeletal muscle and trabeculae.
Materials and methods
Subjects
Five groups of women were recruited for this study: ambulatory premenopausal (AMBPRE), ambulatory postmenopausal (AMBPOST), SCI premenopausal young (<30 years old; SCIPREY), SCI premenopausal older (>35 years of age; SCIPREO), and SCI postmenopausal (SCIPOST). The women with SCI were recruited from the Shepherd Center outpatient database and the ambulatory women were recruited through an advertisement in a local newspaper in Athens, Ga., USA. Attempts were made to match groups for height, weight, and race. AMBPRE and SCIPREO were matched on age and AMBPOST and SCIPOST were matched on age.
Exclusionary criteria included previous or current fracture or hardware in both lower extremities, heterotopic ossification in both lower extremities, long-term medication use known to affect bone (e.g. corticosteroids) and disorders known to influence bone (e.g. hyperthyroidism). Additional inclusion criteria for postmenopausal women included: 1) 5 years postmenopause; menopause was defined according to the World Health Organization (WHO): 12 months after the cessation of normal menstrual cycles [29]; 2) use of medications known to effect bone (estrogen replacement, hormone replacement, bisphosphonates, soy supplements, or estrovan) in the previous 5 years; 3) osteopenia or osteoporosis at one or more site (spine, femoral neck, trochanteric, total hip, or total body). We recruited individuals that were not involved in heavy loading activities such as weight training programs. Additional inclusion criteria for women with SCI were a complete SCI (American Spinal Cord Injury Association rating of A) and ≥2 years post-injury. Women were also asked about fracture history, anatomical location and date of fracture, and were eligible for participation as long as they had not sustained fractures in both lower extremities. The extremity that did not experience a fracture was imaged. We attempted to recruit only non-smoking women.
This study was approved by the Institutional Review Boards at the University of Georgia and Shepherd Center. All participants provided written informed consent prior to enrollment in the study.
Microarchitecture of trabecular bone
Trabecular bone of the distal femur and proximal tibia was assessed using high resolution MRI as done previously [21,30]. Images were acquired on a GE Signa 1.5 T magnetic resonance imager. A 3D fast gradient-echo sequence (TE/TR=4.5/30 ms; 40° flip angle) was used to obtain the high resolution images (10 cm FOV), with a spatial reconstructed resolution of 195×195×1000 µm. A bilateral phased array coil (USA Instruments) was used to collect 60 contiguous 1 mm slices in the axial plane, starting with the distal end of the femur, and another block of 60 starting with the proximal end of the tibia. A 3-D low-pass filter was applied to correct for heterogeneous signal across the phased array surface coil. Images were categorized into bone and non-bone (marrow) using a dual phase limit threshold. Some voxels contained bone and non-bone. This was accounted for by partial volume correction [31]. Regions of interests were manually identified and a set of parallel lines rotated by 5° through the slice to determine mean intercept length. Parameters measured were apparent trabecular bone volume to total volume (app.BV/TV) and apparent trabecular thickness (app.Tb.Th, mm), from which apparent trabecular number (app.Tb.N, mm−1) and separation (app.Tb.Sp, mm) were derived [32,33]. These procedures are both valid [32], reliable [34,35] and discriminate between those that do and do not fracture [31].
Muscle morphology
MRI was used to examine skeletal muscle morphology of the thigh as previously described [36]. Briefly, T1 weighted MR images were taken of one thigh with a 1.5 T magnet using the whole-body coil (TR/TE 500/14 ms, FOV (20–24 cm, 256×256 matrix). Transaxial images, 1 cm thick and 0.5 cm apart, were taken from the knee joint to the hip joint. Skeletal muscle cross sectional area at the level of the middle third of the femur was determined. Images were analyzed on specifically designed software (X-Vessel, East Lansing, Mich., USA). Images were segmented into fat (high intensity), muscle (mid-intensity) and bone (low intensity). A preliminary segmentation of each two-dimensional slice into fat and non-fat regions was obtained by simplex optimization of the correlation between a Sobel gradient image computed from the original image and the corresponding gradient images computed from single-threshold fat-segmented images. The first-pass segmentation corrected for inhomogeneous signal intensity across the image. The image was then re-segmented into three intensity components using a fuzzy c-mean clustering algorithm. To determine thigh skeletal muscle cross sectional area (CSA), manual selection of a pixel of skeletal muscle was done. This highlighted and provided a total number of skeletal muscle pixels (without fat or bone) in the region of interest. Quadriceps femoris CSA was determined by manually tracing the area in each slice and creating a histogram of pixels across signal intensity. Pixels with mid-range signal intensity values (between 80 and 387) defined skeletal muscle. After obtaining the number of pixels in the region of interest corresponding to muscle, muscle CSA was calculated by correcting for field of view (FOV=20–24 cm) and total pixel number; number of muscle pixels×(FOV2/total pixel number). Average muscle CSA is reported for the mid-third region of the thigh and quadriceps femoris. The mid-third region was determined by measuring femur length from coronal scout images. Images were analyzed by a single investigator and test–retest reliability was excellent (r=0.998).
Areal bone mineral density
Dual energy X-ray absorptiometry (DXA; Delphi A, Hologic, Inc., Bedford Mass., USA) was used to determine areal bone mineral density (aBMD) of the whole body, hip (total, neck, trochanteric, and total regions), and spine (L1–L4) in ambulatory postmenopausal women. T-scores are reported along with levels of aBMD. A calibration step wedge, consisting of thermoplastic resin (68% fat) and thermoplastic resin-aluminum steps (~10% fat) calibrated against stearic acid (100% fat) and water (8.6% fat; Hologic, Inc.) was scanned prior to testing to calibrate fat mass and fat-free soft tissue mass. A lumbar spine phantom consisting of calcium hydroxyapatite embedded in a cube of thermoplastic resin (model DPA/QDR-1); Hologic x-caliber anthropometric spine phantom was scanned daily to ensure mineral accuracy.
Statistical analysis
Two-way analysis of variance (ambulatory versus menopause status) was used to detect differences in age, height and weight (SPSS version 11). One-way ANOVA was used to compare time since menopause and duration of spinal cord injury. Two-way ANOVA was used to test differences in app.BV/TV, app.Tb.N, app.Tb.Sp and app.Tb.Th. Simple contrasts were performed using the Bonferroni correction when necessary. Pearson’s r correlation analysis was used to evaluate the relation between thigh or quadriceps skeletal muscle and measures of trabecular bone microarchitecture as well as to examine the relationship between time since injury and trabecular parameters. Significance was set at P<0.05. Effect size using Cohen’s d (d) was calculated when differences approached significance. Small, medium, and large effects are 0.20, 0.50, and 0.80, respectively. All descriptive and outcome measures are reported as mean±SD.
Results
Subjects
Nineteen women with SCI, five SCIPREY, eight SCIPREO and six SCIPOST, met the study criteria. Height, body weight and time since injury were not different between the SCI groups (Table 1). Three of the women with SCI were current smokers (one in each group). Two women in each SCI group were African American; all others were Caucasian. Seven women (one SCIPREO, four SCIPOST, and two SCIPREY) had experienced a fracture to the lower extremity since the accident that caused the spinal cord injury (three distal femur, two proximal tibia, one each of proximal femur and femoral shaft). Most subjects fractured within 8 years following injury (n=6, range 2–8 years), except for one subject who fractured 27 years after SCI.
Seventy-eight premenopausal and 27 postmenopausal women responded to the advertisement. Eight premenopausal women were selected to participate who best represented the SCIPREO group. Postmenopausal women were excluded because of chronic illness or medication use (n=5), length of time post-menopause (n=4) or did not want to be in the study due to claustrophobia (n=5). Thirteen postmenopausal women underwent DXA scans and nine had one or more sites that were osteopenic or osteoporotic. On average, the postmenopausal ambulatory women were in the osteopenic range for trochanteric (t=−1.30±0.72), total hip (t=−1.22±0.67), lumbar spine (t=−1.86±1.19), and total body (t=−1.28±1.02) aBMD. The AMBPOST group comprised these nine subjects.
Height and body weight was not different between the two ambulatory groups (Table 1). No women in the ambulatory groups were current smokers. Two women were African American in the postmenopausal group and one in the premenopausal group; all others were Caucasian.
The AMBPRE and SCIPREO groups were not different in age. The AMBPOST and SCIPOST were also not different in age or years post-menopause. Furthermore, there were no differences in height or body weight in the women with SCI versus the ambulatory women.
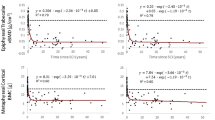
Bone microarchitecture
Five ambulatory women and five women with SCI did not complete the high-resolution scan of the femur due to motion artifact. Representative images of the distal femur of subjects who completed testing satisfactorily are demonstrated in Fig. 1a–e. All of the apparent bone parameters of the distal femur suggested diminished architecture in the SCI groups compared to the ambulatory groups. Women with SCI had 30.9% lower appBV/TV [0.212±0.043 versus 0.307±0.029; F(1,26)=30.7, P<0.001], 26.5% fewer trabeculae [appTb.N=1.021±0.169 mm−1 versus 1.390±0.089 mm−1; F(1,26)=37.9, P<0.001], trabeculae that were 61.7% further apart [appTb.Sp=0.815±0.168 mm versus 0.504±0.060 mm; F(1,26)=30.9, P<0.001] and 6.8% thinner [appTb.Th=0.206±0.013 mm versus 0.221±0.009 mm; F(1,26)=4.8, P=0.039] in the distal femur compared to the ambulatory group (Fig. 2a–d). There were no significant differences in any measure of trabecular bone microarchitecture among the three groups of spinal cord injured women. In addition, there was no interaction or main effect of menopause for any femoral trabecular parameter. In other words, measures of trabecular bone microarchitecture were not different in the postmenopausal versus the premenopausal women.
Representative high resolution magnetic resonance axial images of the distal femur for a AMBPRE (premenopausal ambulatory), b AMBPOST (postmenopausal ambulatory), c SCIPREO (premenopausal SCI >35 years old), d SCIPOST (postmenopausal spinal cord injured) and e SCIPREY (premenopausal SCI <30 years old). Black is bone and white is marrow or fat
Comparison of trabecular parameters of the distal femur. a Apparent trabecular bone volume relative to total bone volume (App.BV/TV), b apparent trabecular number (App.Tb.N), c apparent trabecular spacing (App.Tb.Sp), d Apparent trabecular thickness (App.Tb.Th). AMBPRE premenopausal ambulatory; AMBPOST postmenopausal ambulatory; SCIPREO premenopausal spinal cord injured >35 years old; SCIPOST postmenopausal spinal cord injured; SCIPREY premenopausal <30 years old. *P=0.001, SCI<ambulatory for a, b, d; SCI>ambulatory for c. Values are mean±SD
All subjects completed the high-resolution proximal tibia scans satisfactorily. Representative images are demonstrated in Fig. 3a–e. Results from the proximal tibia are similar to the distal femur. Ambulatory status had a significant effect on trabecular bone microarchitecture (Fig. 4 a–d). The spinal cord injured groups had 22.3% less app.BV/TV [0.202±0.044 versus 0.260±0.024; F(1,35)=21.4, P<0.001], 18.5% less app.Tb.N [1.016±0.170 mm−1 versus 1.244±0.134 mm−1; F(1,35)=22.5, P=0.001] and 5.8% less app.Tb.Th [0.196±0.123 mm versus 0.208±0.006 mm; F(1,35)=8.1, P=0.008] compared to the ambulatory groups. There was a significant interaction for app.Tb.Sp (P=0.042), thus simple effects were examined. Analyses showed a simple effect of ambulatory status with greater spacing in SCI groups compared to ambulatory groups (26%, 60% and 41% for SCIPREO, SCIPOST and SCIPREY, respectively; P≤0.031). There was also a trend for a simple effect of menopause in SCI women (P=0.059). SCIPOST had 33.6% greater app.Tb.Sp in the tibia compared to SCIPREO (P=0.020, d=1.45). For SCI groups, there were no significant relationships between number of years injured and trabecular parameters for both sites (r2≤0.073–0.109, P≥0.330).
Representative high resolution magnetic resonance axial images of the proximal tibia for a AMBPRE (premenopausal ambulatory), b AMBPOST (postmenopausal ambulatory), c SCIPREO (premenopausal SCI >35 years old), d SCIPOST (postmenopausal spinal cord injured) and e SCIPREY (premenopausal SCI <30 years old)
Comparison of trabecular parameters of the proximal tibia. a Apparent trabecular bone volume relative to total bone volume (App.BV/TV), b apparent trabecular number (App.Tb.N), c apparent trabecular spacing (App.Tb.Sp), d apparent trabecular thickness (App.Tb.Th). *P≤0.001, SCI<ambulatory for a, b, d; SCI>ambulatory for c. **P=0.020, SCIPOST>SCIPREY. Values are mean±SD
Muscle CSA
Muscle cross-sectional area of the thigh and quadriceps was ~55% lower for SCI groups compared to the ambulatory groups (thigh ambulatory=93±20.3 cm2, SCI=41±18.3 cm2, P=0.001; quadriceps ambulatory=46±9.6 cm2, SCI=19±8.6 cm2). Skeletal muscle CSA of the thigh was not statistically different between pre- and postmenopausal women (101.1±16.95 cm2 versus 86.4±21.56 cm2, P=0.182), but the effect size was moderate to large (Cohen’s d=0.78). Trabecular bone parameters were correlated to skeletal muscle CSA in the thigh for SCI groups; femur (n=14), r2=0.481, 0.408, 0.405 for app.BV/TV, Tb.N and Tb.Sp; tibia (n=19), r2=0.384, 0.325 and 0.282 for app.BV/TV app.Tb.N, and app.Tb.Sp, respectively, P<0.05). Similar relationships were found in the ambulatory groups; femur (n=10) r2=0.427 and 0.405 for app.Tb.N and appTb.Sp, tibia (n=15) r2=0.424, 0.383, and 0.377 for app.BV/TV, Tb.N and Tb.Sp, P<0.05). In the ambulatory women, the relationship between age and muscle CSA was not significant (P=0.523).
Discussion
The primary finding was that unloaded bone in women with SCI had more deteriorated ultrastructure than bone in postmenopausal estrogen-free women. Findings of large deterioration in women with SCI are similar to findings in men with SCI compared to ambulatory men (femur=26% less app.BV/TV, 21% less app.Tb.N, 7% less app.Tb.Th, 43% more app.Tb.Sp; tibia=19% less app.Tb.N, 18% less app.BV/TV, 32% more app.Tb.Sp [21]. Hence, unloading following SCI substantially diminishes bone architecture around the knee in both men and women. These findings confirm similar findings in animals. Gender differences in deteriorated trabeculae of the tibia were not reported following hind-limb unloading in male and female rats [37]. The reduced microarchitecture in SCI in addition to a reduction in bone mass coincides with the high rate of fracture in this population compared to ambulatory individuals [18]. Among the women with SCI, one-third had fractures to the thigh and leg since the initial injury. This is in accordance with other reports of fracture incidence (29% and 33%) [19,20]. All three groups of women with SCI had deteriorated trabeculae. This is notable considering the variability in chronological age (22–62 years) and time since injury (2–33 years). These findings in conjunction with the lack of relationship between time since injury and trabeculae also show that the influence of unloading on bone architecture occurred independent of chronological age and number of years injured. In other words, bone was not more deteriorated for women that had been injured for a greater number of years or who were older. Previous longitudinal studies have shown that changes in bone mineral content occur 2 years following injury, reaching a steady state thereafter [2]. The lack of correlation from the present study suggests that the deterioration of trabeculae probably occurs early after unloading.
The central purpose of this investigation was to compare the effects of menopause versus SCI on trabecular bone of the knee. Clearly, unloading resulted in substantial microarchitectural deterioration compared to estrogen loss, which showed no differences compared to premenopausal ambulatory women. Although the women in the postmenopausal ambulatory group were young, 50–63 years old, women were approximately 8 years into estrogen withdrawal, a time during which the most rapid changes in trabecular bone have been reported [25,38]. Deteriorated calcaneus trabeculae have been reported in postmenopausal women [34]. Apparent trabecular bone volume was 16% less, thickness 11% less and spacing 17.5% greater for a postmenopausal group compared to a group of premenopausal women. However, the age difference between the groups was 26.5 years and therefore age and estrogen effects independently cannot be discerned. The age difference in our ambulatory pre- and postmenopausal groups was 12 years, thus minimizing the effect of age on bone.
Comparative investigations into the aforementioned determinants of bone health have been examined using rat models of osteoporosis. The trabecular bone was deteriorated in tibial structures of young ovariectomized rats (estrogen free) and rats with sciatic neurectomy (unloaded) compared to sham controls [6]. These data also suggest that estrogen has stronger effects on the trabecular structural parameters compared to unloading. Unloading and ovariectomy have also been shown to result in similar losses in distal femur and proximal tibia trabeculae (relative bone volume, trabecular number, spacing, and thickness) compared to control conditions, suggesting that absence of load and estrogen have similar effects on bone architecture [4,8]. Women in the present study clearly had more deteriorated trabeculae after SCI than after menopause. Thus the effects of estrogen loss on trabeculae in lower mammals appear to be more pronounced than in humans. These data also show significantly greater spacing in SCIPOST compared to SCIPREO. This is an interesting finding which shows an interaction between menopause and SCI, suggesting that lack of estrogen in the unloaded state has greater effects than each parameter alone as previously reported in rats [4,8].
Postmenopausal women had levels of aBMD associated with osteopenia or osteoporosis at one or more sites. This is in agreement with declines in BMD following menopause [25,39,40], although smaller and variable loss have been documented [26,41,42]. An unexpected finding was the lack of difference in trabecular bone for the post- compared to premenopausal ambulatory women. Even within the knee region, there are reported differences in aBMD (9.8% lower) in pre- and postmenopausal groups with mean ages similar to the current study (pre=47.4 years, post=59.4) implying a loss of bone mineral density at the knee with menopause, thus either altered cortical bone or trabecular bone in the knee [43]. While other anatomical regions (hip, for example) experience greater bone mass loss (versus knee) following menopause [43], in vivo high resolution images can only be obtained from limited sites at the present time, the calcaneous, radius and about the knee. The knee was examined in this study because of the high prevalence of fracture incidence observed in this region for persons with SCI [44,45].
How can we explain the lack of differences in bone architecture between the pre- and postmenopausal groups in this study? Changes in aBMD may not reflect structural changes in trabeculae. The postmenopausal ambulatory women showed levels of aBMD associated with osteopenia and osteoporosis for the total hip, trochanteric, lumbar and total body regions as defined by the WHO [1]. Of the sites that were measured with DXA, the lumbar spine has the highest trabecular composition (66% trabecular), which was shown to be osteopenic for AMBPOST, while we did not show differences in trabeculae of the knee. Results have been conflicting as to whether trabecular measures correlate well with aBMD [21,33,34,46]. Correlations between structural measures of the distal radius and radial aBMD were poor (r=0.42 for app.Tb.N and −0.42 for app.Tb.Sp, no significant relation to app.Tb. BV/TV) and there was no relation between any distal radius structural and proximal femur aBMD measures [33] or trabecular measures of the calcaneous and aBMD in the femur [46]. However, the same laboratory showed stronger correlations (r=0.60–0.72) between calcaneous BMD and calcaneal app. BV/TV and others have shown significant correlations between proximal femur aBMD and trabecular parameters in the tibia in men with and without SCI (r=0.62 for appBV/TV, 0.78 for appTb.N and −0.82 for appTb.Sp) [21,34]. These latter studies evaluated aBMD and trabeculae in the same bone regions and also examined bone regions, calcaneous and proximal tibia, which are largely comprised of trabecular bone. Variability in specific changes in cortical and trabecular bone may have contributed to our findings that trabeculae were not different between ambulatory groups. Some early postmenopausal women show decreased trabecular thickness, some lose trabecular bone volume and number in the distal radius, while others lose cortical thickness independently without losses in trabeculae or fail to show any declines [47]. The effects of estrogen on trabecular bone appear to be complex with other, perhaps unidentified, factors substantially influencing skeletal integrity.
This study comprised small groups, which suggests the study may have been underpowered to detect differences in trabecular bone between pre- and postmenopausal women. In addition, all ambulatory women did not have femur images; 12 of 17 women had distal femur images. Based on the studies by Ahlborg et al. and Ouyang et al., and the WHO Technical Report Series, we estimated that postmenopausal women would have 15% less trabecular bone than premenopausal women or 3% loss per year [1,25,28] To detect such a difference, a sample of eight subjects was required (β=0.80). However, the average difference in trabecular bone was less than 1%, suggesting rather that trabecular bone in the tibia is not different between the post- versus premenopausal women.
Finally, it is also plausible that estrogen loss without a concomitant reduction of loading or physical activity did not alter bone microstructure in the loaded plane. While the axial plane is ideal to measure changes in architecture in groups with altered loading, the influence of menopause on trabeculae may be more apparent in the horizontal direction that could be measured in the coronal plane. Some evidence suggests that early losses of trabecular bone are reflected as a greater relative loss of horizontal trabeculae, compared to load bearing or vertical trabeculae [48,49]. Furthermore, it has been shown that load bearing trabeculae may increase in thickness to account for lost horizontal structures [50,51,52]. Among the four measures of apparent trabecular measures presented in this study, trabecular thickness is the least accurate due to the small size of trabeculae walls (78–200 μm) compared to pixel size (195×195 μm) and slice thickness (1000 μm) used in high resolution MR scanning. This is noted as a limitation with the current technology [53].
These data also show moderate correlations between trabecular bone and skeletal muscle size for both ambulatory and SCI women. aBMD has been reported to be related to muscle mass in able-bodied individuals, with 40–60% of the variance in bone explained by skeletal muscle mass [54]. These correlations suggest that increasing skeletal muscle size may have a positive influence on trabeculae. Evoking muscle hypertrophy of the thigh may increase wall thickness and number in the distal femur and proximal tibia. According to the mechanotransduction theory of bone cell activation, a force or bending of the bone plays a critical role in bone formation [55,56], supporting resistance training as an avenue for bone formation. However, in regions where mineralized walls and osteocytes have been lost and connectivity decreased, the bending force may not be realized and thus mechanical stimuli may fail to activate bone growth. In contrast, limited data have shown increases in trabeculae following mechanical interventions. Trabecular bone volume, thickness and number were increased following low strain, high frequency stimulation in sheep [57] and following re-ambulation in tail suspended rats [58], while trabecular bone density was increased following loading exercises in women [59]. Although limited data support recovering lost trabeculae, the relationship between muscle and microarchitecture is encouraging for loading interventions optimized for hypertrophy.
In summary, trabecular bone integrity about the knee was deteriorated in SCI women between the ages of 22–63 compared to ambulatory women; hence unloading had negative effects on trabeculae. These are the first data in women that clearly suggest unloading has larger effects on trabecular architecture of the knee compared to estrogen withdrawal associated with menopause. Additionally, postmenopausal women with SCI had the most deteriorated trabeculae indicating an interaction between these primary bone determinants. Although menopause purportedly decreases trabecular bone integrity, no differences were found regarding menopause in ambulatory women. The lack of differences in trabeculae between the ambulatory groups encourages further investigations into trabecular deterioration due to estrogen loss, explicitly at other skeletal sites. Because loss of trabeculae is evident in individuals with SCI where fracture incidence is high and it is unknown whether lost trabeculae can be re-established in humans, studies should be undertaken to reverse bone loss in this population.
References
WHO (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Organ Tech Rep Ser, 843
Biering-Sorensen F, Bohr HH, Schaadt OP (1990) Longitudinal study of bone mineral content in the lumbar spine, the forearm and the lower extremities after spinal cord injury. Eur J Clin Invest 20:330
Minaire P, Neunier P, Edouard C, Bernard J, Courpron P, Bourret J (1974) Quantitative histological data on disuse osteoporosis: comparison with biological data. Calcif Tissue Res 17:57
Bagi CM, Miller SC (1994) Comparison of osteopenic changes in cancellous bone induced by ovariectomy and/or immobilization in adult rats. Comparison of osteopenic changes in cancellous bone induced by ovariectomy and/or immobilization in adult rats. Anat Rec 239:243–254
Cavolina JM, Evans GL, Harris SA, Zhang M, Westerlind KC, Turner RT (1997) The effects of orbital spaceflight on bone histomorphometry and messenger ribonucleic acid levels for bone matrix proteins and skeletal signaling peptides in ovariectomized growing rats. The effects of orbital spaceflight on bone histomorphometry and messenger ribonucleic acid levels for bone matrix proteins and skeletal signaling peptides in ovariectomized growing rats. Endocrinology 138:1567–1576
Ito M, Nishida A, Nakamura T, Uetani M, Hayashi K (2002) Differences of three-dimensional trabecular microstructure in osteopenic rat models caused by ovariectomy and neurectomy. Bone 30:594
Li XJ, Jee WS, Chow SY, Woodbury DM (1990) Adaptation of cancellous bone to aging and immobilization in the rat: a single photon absorptiometry and histomorphometry study. Anat Rec 227:12
Westerlind KC, Wronski TJ, Ritman EL et al. (1997) Estrogen regulates the rate of bone turnover but bone balance in ovariectomized rats is modulated by prevailing mechanical strain. Estrogen regulates the rate of bone turnover but bone balance in ovariectomized rats is modulated by prevailing mechanical strain. Proc Natl Acad Sci USA 94:4199–4204
Consensus development conference (1991) Diagnosis, prophylaxis and treatment of osteoporosis. Am J Med 90:107
Bell GH, Dunbar O, Beck JS, Gibb A (1967) Variations in strength of vertebrae with age and their relation to osteoporosis. Calcif Tissue Res 1:75
Dempster DW, Shane E, Horbert W, Lindsay R (1986) A simple method for correlative light and scanning electron microscopy of human iliac crest bone biopsies: qualitative observations in normal and osteoporotic subjects. J Bone Miner Res 1:15
Mann T, Oviatt SK, Wilson D, Nelson D, Orwoll ES (1992) Vertebral deformity in men. J Bone Miner Res 7:1259
Parfitt AM (1987) Trabecular bone architecture in the pathogenesis and prevention of fracture. Am J Med 82:68
Looker AC, Johnston CC Jr, Wahner HW, et al. (1995) Prevalence of low femoral bone density in older U.S. women from NHANES III. J Bone Miner Res 10:796
Melton LJ, 3rd, Chrischilles EA, Cooper C, Lane AW, Riggs BL (1992) Perspective. How many women have osteoporosis? J Bone Miner Res 7:1005
Claus-Walker J, Halstead LS (1982) Metabolic and endocrine changes in spinal cord injury: IV. Compounded neurologic dysfunctions. Metabolic and endocrine changes in spinal cord injury: IV. Compounded neurologic dysfunctions 63:632
Lazo MG, Shirazi P, Sam M, Giobbie-Hurder A, Blacconiere MJ, Muppidi M (2001) Osteoporosis and risk of fracture in men with spinal cord injury. Spinal Cord 39:208
Vestergaard P, Krogh K, Rejnmark L, Mosekilde L (1998) Fracture rates and risk factors for fractures in patients with spinal cord injury. Spinal Cord 36:790
Krause JS (2000) Aging after spinal cord injury: an exploratory study. Spinal Cord 38:77
Frisbie JH (1997) Fractures after myelopathy: the risk quantified. J Spinal Cord Med 20:66
Modlesky CM, Majumdar S, Narisimhan A, Dudley GA (2004) Trabecular bone microarchitecture is deteriorated in men with spinal cord injury. J Bone Miner Res 19:48–55
Roberts D, Lee W, Cuneo RC et al. (1998) Longitudinal study of bone turnover after acute spinal cord injury. J Clin Endocrinol Metab 83:415
Harris S, Dawson-Hughes B, Usda Human Nutrition Research Center on Aging TUBMA (1992) Rates of change in bone mineral density of the spine, heel, femoral neck and radius in healthy postmenopausal women. Rates of change in bone mineral density of the spine, heel, femoral neck and radius in healthy postmenopausal women. Bone Miner 17:87–95
Mosekilde L (1990) Consequences of the remodelling process for vertebral trabecular bone structure: a scanning electron microscopy study (uncoupling of unloaded structures). Bone Miner 10:13
Ahlborg HG, Johnell O, Nilsson BE, Jeppsson S, Rannevik G, Karlsson MK (2001) Bone loss in relation to menopause: a prospective study during 16 years. Bone 28:327
Falch JA, Sandvik L (1990) Perimenopausal appendicular bone loss: a 10-year prospective study. Bone 11:425
Ravn P, Hetland ML, Overgaard K, Christiansen C (1994) Premenopausal and postmenopausal changes in bone mineral density of the proximal femur measured by dual-energy X-ray absorptiometry. J Bone Miner Res 9:1975
Ouyang X, Selby K, Lang P et al. (1997) High resolution magnetic resonance imaging of the calcaneus: age-related changes in trabecular structure and comparison with dual X-ray absorptiometry measurements. High resolution magnetic resonance imaging of the calcaneus: age-related changes in trabecular structure and comparison with dual X-ray absorptiometry measurements. Calcif Tissue Int 60:139–147
WHO (1981) Research on the menopause. World Health Organ Tech Rep Ser, 670
Beuf O, Ghosh S, Newitt DC et al. (2002) Magnetic resonance imaging of normal and osteoarthritic trabecular bone structure in the human knee. Arthr Rheum 46:385
Majumdar S, Genant HK, Grampp S et al. (1997) Correlation of trabecular bone structure with age, bone mineral density, and osteoporotic status: in vivo studies in the distal radius using high resolution magnetic resonance imaging. J Bone Miner Res 12:111
Majumdar S, Newitt D, Mathur A et al. (1996) Magnetic resonance imaging of trabecular bone structure in the distal radius: relationship with X-ray tomographic microscopy and biomechanics. Osteoporos Int 6:376
Majumdar S, Link TM, Augat P et al. (1999) Trabecular bone architecture in the distal radius using magnetic resonance imaging in subjects with fractures of the proximal femur. Osteoporos Int 10:231
Ouyang X, Majumdar S, Link TM et al. (1998) Morphometric texture analysis of spinal trabecular bone structure assessed using orthogonal radiographic projections. Med Phys 25:2037
Newitt DC, van Rietbergen B, Majumdar S (2002) Processing and analysis of in vivo high-resolution MR images of trabecular bone for longitudinal studies: reproducibility of structural measures and micro-finite element analysis derived mechanical properties. Osteoporos Int 13:278
Modlesky CM, Bickel CS, Slade JM, Meyer RA, Cureton KC, Dudley GA (2003) Assessment of skeletal muscle mass in men with spinal cord injury using dual-energy X-ray absorptiometry and magnetic resonance imaging. J Appl Physiol epub:
Hefferan TE, Evans GL, Lotinun S, Zhang M, Morey-Holton E, Turner RT (2003) Effect of gender on bone turnover in adult rats during simulated weightlessness. J Appl Physiol 95:1775
Lindsay R (1988) Sex steriods in the pathogenesis and prevention of osteoporosis. In: Riggs BL (ed) Osteoporosis: etiology, diagnosis and management. Raven Press, New York, p 333
Dawson-Hughes B, Harris SS, Krall EA, Dallal GE, Falconer G, Green CL (1995) Rates of bone loss in postmenopausal women randomly assigned to one of two dosages of vitamin D. Am J Clin Nutr 61:1140
Lindsay R, Nieves J, Formica C et al. (1997) Randomised controlled study of effect of parathyroid hormone on vertebral-bone mass and fracture incidence among postmenopausal women on oestrogen with osteoporosis. Lancet 350:550
Patel R, Blake GM, Rymer J, Fogelman I (2000) Long-term precision of DXA scanning assessed over seven years in forty postmenopausal women. Osteoporos Int 11:68
Christiansen C, Riis BJ, Rodbro P (1987) Prediction of rapid bone loss in postmenopausal women. Lancet 1:1105
Garland DE, Adkins RH, Stewart CA, Ashford R, Vigil D (2001) Regional osteoporosis in women who have a complete spinal cord injury. J Bone Joint Surg [Am] 83-A:1195
Comarr AE, Hutchinson, RH, Bors E (1962) Extremity fractures of patients with spinal cord injuries. Am J Surg 103:732
Freehafer AA (1995) Limb fractures in patients with spinal cord injury. Arch Phys Med Rehabil 76:823
Link TM, Majumdar S, Augat P et al. (1998) In vivo high resolution MRI of the calcaneus: differences in trabecular structure in osteoporosis patients. J Bone Miner Res 13:1175
Laib A, Hauselmann HJ, Ruegsegger P (1998) In vivo high resolution 3D-QCT of the human forearm. Technol Health Care 6:329
Oda K, Shibayama Y, Abe M, Onomura T (1998) Morphogenesis of vertebral deformities in involutional osteoporosis. Age-related, three-dimensional trabecular structure. Spine 23:1050
Thomsen JS, Ebbesen EN, Mosekilde LI (2002) Age-related differences between thinning of horizontal and vertical trabeculae in human lumbar bone as assessed by a new computerized method. Bone 31:136
Atkinson PJ (1967) Variation in trabecular structure of vertebrae with age. Calcif Tissue Res 1:24
Frost HM (1999) On the trabecular “thickness”-number problem. J Bone Miner Res 14:1816
Parfitt AM, Mathews CH, Villanueva AR, Kleerekoper M, Frame B, Rao DS (1983) Relationships between surface, volume, and thickness of iliac trabecular bone in aging and in osteoporosis. Implications for the microanatomic and cellular mechanisms of bone loss. Relationships between surface, volume, and thickness of iliac trabecular bone in aging and in osteoporosis. Implications for the microanatomic and cellular mechanisms of bone loss. J Clin Invest 72:1396–1409
Kothari M, Keaveny TM, Lin JC, Newitt DC, Genant HK, Majumdar S (1998) Impact of spatial resolution on the prediction of trabecular architecture parameters. Bone 22:437
Binder EF, Kohrt WM (2000) Relationships between body composition and bone mineral content and density in older women and men. Clinl Exerc Physiol 2:84
Bloomfield SA (2001) Cellular and molecular mechanisms for the bone response to mechanical loading. Int J Sport Nutr Exerc Metab 11 Suppl:S128
Duncan RL, Turner CH (1995) Mechanotransduction and the functional response of bone to mechanical strain. Calcif Tissue Int 57:344
Rubin C, Turner AS, Mèuller R et al. (2002) Quantity and quality of trabecular bone in the femur are enhanced by a strongly anabolic, noninvasive mechanical intervention. J Bone Miner Res 17:349
Bourrin S, Palle S, Genty C, Alexandre C (1995) Physical exercise during remobilization restores a normal bone trabecular network after tail suspension-induced osteopenia in young rats. J Bone Miner Res 10:820
Simkin A, Ayalon J, Leichter I (1987) Increased trabecular bone density due to bone-loading exercises in postmenopausal osteoporotic women. Calcif Tissue Int 40:59
Acknowledgements
The authors would like to thank Carolyn Sharp for her technical expertise and Leslie VanHiel for assistance with subject recruitment. This study was supported by the Biomedical and Health Science Institute at the University of Georgia, Shepherd Center, and the National Institutes of Health (HD40323, GAD).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Slade, J.M., Bickel, C.S., Modlesky, C.M. et al. Trabecular bone is more deteriorated in spinal cord injured versus estrogen-free postmenopausal women. Osteoporos Int 16, 263–272 (2005). https://doi.org/10.1007/s00198-004-1665-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-004-1665-7