Abstract
Background: Osteoporosis is increasingly recognized as a major source of morbidity following renal transplantation. The aim of this cross-sectional study was to determine the prevalence of osteoporosis in a cohort of male transplant recipients and examine factors that may influence their bone loss. Methods: Bone mineral density (BMD) and biochemical markers of bone metabolism were measured in 134 out of 154 male renal allograft recipients in our center. Results: The mean age of the patients was 49.7 years (range 26–76) with a median of 6 years post-transplant. Only 17% had normal BMD, 30% were osteoporotic at either hip or spine, and this proportion rose to 41% if the ultradistal radius was included. Parathyroid hormone (PTH) was negatively correlated with BMD at all skeletal sites. In a multiple regression model, independent predictors of femoral neck BMD included body mass index (p=0.004), diabetes (p=0.025), and PTH (p=0.049). The only independent predictor of BMD at the ultradistal radius was PTH (p<0.001). Nineteen men sustained a total of 25 appendicular fractures after transplantation (median time to fracture was 3 years). Prevalent vertebral fractures were only identified in five men. PTH was elevated in 72.4% of patients (mean PTH 142 ± 118 pg/ml). Bone resorption markers were increased in 48% of patients. PTH was positively correlated with serum carboxyterminal telopeptide of type 1 collagen (r=0.473, p<0.001) and procollagen type 1 amino terminal propeptide (r=0.419, p<0.001). Conclusions: Osteopenia and osteoporosis are common in male transplant recipients, and the hip and radius are the most severely affected sites. Elevated rates of bone resorption driven by hyperparathyroidism appear to be the most important contributing factor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic renal failure exposes patients to the adverse skeletal consequences of perturbations in divalent ion metabolism and vitamin D metabolism, and parathyroid hyperplasia. Although a successful renal transplant may correct many of these abnormalities, many patients continue to have persistent hyperparathyroidism and renal dysfunction, while other factors deleterious to bone such as glucocorticoids or immunosuppressants are introduced [1].
Osteoporosis after renal transplantation is well recognized. Rapid bone loss has been reported in the early post-transplant period and during the 1st year, bone mineral density (BMD) typically falls by 3–7% [2]. This initial bone loss is primarily confined to trabecular bone and is mainly attributed to corticosteroid use. Subsequently rates of bone loss appear to slow to 0–2% per year [3] and these differences may reflect variations in the type and severity of pretransplant renal osteodystrophy and early post-transplant treatment.
Bone loss may predispose to fractures and prevalence rates of 11–19% have been reported, with much higher rates of up to 45%, in patients with insulin-dependent diabetes [4, 5, 6]. In our own recently conducted cross-sectional study the prevalence of low trauma fractures after renal transplantation was 12% [7]. In contrast to other solid organ recipients, fractures in renal transplant recipients tend to occur in the appendicular skeleton, with a low frequency of vertebral deformities [6, 8, 9].
A previous study in female transplant recipients within our center identified osteoporosis at one or more sites in 57% of patients [10]. The present cross-sectional study extends this assessment to male transplant recipients in order to determine the prevalence of reduced bone mineral density, incidence of fracture, and to identify possible causative factors, including the role of hyperparathyroidism and increased bone turnover.
Materials and methods
Patients
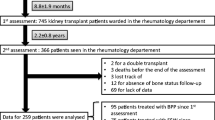
All 154 male patients who were more than 1-year post renal transplantation were invited to take part. The local hospital research ethics committee approved the study, and all patients gave written informed consent. Demographic data was obtained by case note review. Information collected included age, ethnicity, cause of renal failure, presence of diabetes, previous parathyroidectomy, duration of renal replacement therapy (dialysis and transplantation), time since transplant, rejection episodes, cumulative doses of immunosuppressive drugs, and risk factors for osteoporosis.
Immunosuppressive regimes
Prior to 1986 the basic immunosuppressive regime was prednisolone and azathioprine. Between 1986 and 1999, most patients were treated with a triple regime of cyclosporine, prednisolone, and azathioprine. Since 1999 high-risk patients (those with a second transplant, highly sensitized recipients, or those with poorly matched grafts) have received a tacrolimus-based triple regime. Patients with chronic allograft nephropathy are converted to mycophenolate mofetil followed by withdrawal of calcineurin inhibitors.
Bone mineral density
Bone mineral density of the lumbar spine (L2–L4, n=132) and left proximal femur (n=131) were measured by dual-energy X-ray absorptiometry (DXA) using a Lunar Expert-XL densitometer (Lunar). In 111 patients, nondominant forearm bone mineral density was measured at the distal one-third radius and ultradistal radius.
Results are expressed in g/cm2, T- and Z-scores with osteopenia defined as a T-score between –1.0 and –2.5 SD, and osteoporosis as a T-score below –2.5 SD.
Fractures
Fractures were identified through a structured self-administered questionnaire and subsequently verified by reference to medical notes and available radiology. Lateral dorsal and lumbar spine morphometry was assessed with the patient supine, using X-ray absorptiometry. Anterior, middle, and posterior heights were measured, and wedge (anterior/posterior) and midwedge (middle/posterior) ratios were calculated. Scans were assessed quantitatively, and a fracture defined as a 3 SD or greater reduction in either wedge or midwedge ratio. Scans were also reviewed qualitatively by the research team.
Biochemistry and measure of renal function
Routine biochemistry was determined using standard autoanalyzer techniques. Intact parathyroid hormone (PTH) was measured using a chemiluminescent immunometric assay on an automated analyzer (Immulite 2000; Diagnostics Products, Los Angeles, CA, USA) and 25-hydroxyvitamin D using a manual radioimmunoassay kit (Diasonin, Stillwater, MN, USA).
Glomerular filtration rate (GFR) was calculated using a validated Modification of Diet in Renal Disease Study (MDRD) formula that uses the serum creatinine, urea, albumin, patient age, race, and gender [11].
Biochemical markers of bone formation and resorption
Bone turnover was measured in 113 patients. To standardize collection, serum samples were taken after an overnight fast and either analyzed on the same day or frozen at –70°C for later analysis. Bone formation was assessed by measuring serum procollagen type 1 amino terminal propeptide (P1NP), using a radioimmunoassay method (Orion Diagnostica, Espoo, Finland). Bone resorption was assessed by measuring serum carboxyterminal telopeptide of type 1 collagen (S-CTX), using an automated chemiluminescent assay (Roche Diagnostics, Munnheum, Germany).
Analysis of outcome measures
Patient characteristics and treatment factors were those present at the date of BMD measurement. Data analysis was performed using Statistical Package for the Social Sciences 11.0 for Windows (Chicago, IL, USA). Results are expressed as means ± SD, and as median and interquartile range (IR) where appropriate. Variables that were not normally distributed were log-transformed prior to further analysis. Group means were compared using Student’s t-test or one-way analysis of variance (ANOVA). ANOVA post hoc testing was carried out using the least-significant difference. Chi-square test was used to compare proportions. Variables were compared using Pearson product moment correlation analysis. To correct for colinearity with other quantitative variables, partial correlation analysis was used.
Multiple linear regression was used to examine the relationship between BMD and all potential confounding variables. Probability values of <0.05 were considered to be significant.
Results
Patient demographics
Of the 154 patients in our male transplant population, 134 (87%) agreed to participate (mean age 49.7 years, range 26–76). Ninety-six percent were white Europeans. Primary renal diseases included glomerulonephritis (26.3%), polycystic kidney disease (9.7%), reflux nephropathy (9.7%), renovascular disease (7.7%), diabetic nephropathy (3.8%), vasculitis (2.2%), other causes (18.8%), and unknown cause (21.8%). The median time after transplant was 72.4 months. Patients were divided into three groups according to duration of transplant, namely: group 1, less than 5 years (median time post-transplant 33.7 months, IR=15.8–48.5 months), group 2, 5–10 years (median time post-transplant 86.2 months, IR=72.6–99.9 months), and group 3, more than 10 years (median time post-transplant 159.5 months, IR=142.5–199.3 months). Additional demographic details are shown in Table 1.
Immunosuppression
Patients were on a variety of immunosuppressive therapy regimes reflecting the changing patterns of immunosuppressive use with time. The majority were taking a cyclosporine-based triple regime. At the time of the study, 125 (93%) remained on prednisolone, 117 (87%) were taking cyclosporine, 109 (81%) azathioprine, and a smaller number, mycophenolate mofetil (n=17, 13%) and tacrolimus (n=14, 10%).
Bone mineral density data
Mean BMD at the femoral neck, lumbar spine, and radius are shown in Table 2. The prevalence of osteoporosis was 24% at the femoral neck, 23% at the ultradistal radius, 17% at the lumbar spine, and 13% at the distal one-third radius. Only 17% of men had a normal BMD, 30% were osteoporotic at either femoral neck or lumbar spine, rising to 41% if the forearm sites were included.
Bone mineral density data categorized according to time following transplantation is illustrated in Table 2. The prevalence of femoral neck osteoporosis within the first 5 years following transplantation was 22%, rising to 33% 5–10 years following transplantation, and falling to 18% in those transplanted over 10 years previously (χ-square 1.16, p=0.56).
In a univariate analysis of the predictors of BMD (data not shown) there was a negative correlation with PTH at all sites. At the femoral neck there were additional correlations with BMI, time on dialysis, and the presence of diabetes. Ultradistal radius BMD correlated with S-CTX, serum P1NP, and BMI, and distal one-third radius with serum P1NP, corrected calcium, BMI, time on dialysis, and the presence of diabetes.
In an attempt to determine the predictive value of the independent variables identified in the univariate analysis, a multiple linear regression model was constructed (Table 3). Using femoral neck BMD as the dependent variable and adjusting for age (the predominant confounder of BMD), BMI (p=0.004), diabetes (p=0.025), and PTH (p=0.049) produced the best model, however this only explained 16% of the variance (R 2=0.16, p<0.001). At the distal one-third radius PTH (p=0.015) and BMI (p=0.001) were significant independent predictors (R 2=0.17). Analysis of the ultradistal radius only identified PTH as a significant independent predictor (R 2=0.13, p<0.001). We were unable to detect an effect of either cumulative prednisolone or calcineurin dose on BMD at any site.
Fracture data
There were no self-reported spinal fractures. Spinal MXA identified prevalent vertebral fractures in five (3.8%) men. Nineteen men had a total of 25 fractures after transplantation; hip (n=2), pelvis (n=1) limbs (n=9) others (n=7). The fracture incidence rate was 27 fractures per 1,000 post-transplant years. Median time to fracture was 3 years, but there was a wide range (0.5 to 15 years).
Men with a post-transplant fracture had significantly lower Z-scores at all skeletal sites (Fig. 1). There was no influence by age, presence of diabetes, BMI, duration of dialysis or transplantation, cumulative or average daily steroid dose, PTH or bone turnover markers.
Calcium homeostasis
Serum calcium was above the upper limit of normal in 32% of men, and 24% were moderately hypercalcemic (≥2.65 mmol/l). Of those with hypercalcemia, serum calcium was elevated at the time of transplantation in 18%. Hypercalcemic men were significantly older (54.4 ± 10.8 vs 47.4 ± 12.0 years; p=0.001) with a higher PTH (160 ± 146 pg/ml vs 131 ± 116 pg/ml; p=0.22) compared with normocalcemic men. Mean serum calcium did not change with time since transplant.
Twenty-two percent of men were vitamin D deficient (serum 25-hydroxyvitamin D level <30 nmol/l) and had a higher PTH (mean = 185 ± 134 pg/ml vs 124 ± 105 pg/ml; p=0.035) compared with those who were vitamin D replete, but had similar levels of calcium, phosphate, and alkaline phosphatase.
Only 27.6% of men had a normal PTH. In contrast, 29.1% had a PTH greater than twice the upper limit of normal. Nine patients had undergone a parathyroidectomy and were excluded from subsequent analysis. PTH was significantly higher in the 5–10-year group compared with the group <5 years post-transplant (195 ± 149 pg/ml vs 110 ± 48 pg/ml; p=0.003), but without any significant differences in calcium, phosphate, alkaline phosphatase or 25-OH vitamin D concentration (Table 4). Significant correlations were found between PTH and GFR (r=−0.233, p=0.009), serum 25-hydroxyvitamin D (r=−0.228, p=0.017), time on dialysis (r=0.206; p=0.031), and serum phosphate (r=0.173, p=0.046). After controlling for GFR, the correlations with serum 25-hydroxyvitamin D (r=−0.234, p=0.016) and time on dialysis (r=0.212; p=0.029) persisted. No significant correlation between PTH and age, cumulative corticosteroid dose and time after transplantation was found.
Biochemical markers of bone turnover
Bone resorption as measured by S-CTX was elevated in 47.7% of men. P1NP was less frequently elevated (19.6%) and a small group (5.6%) had low values. Time after transplantation did not affect bone turnover markers (Table 4). Serum CTX was correlated with age (r=−0.371, p<0.001), GFR (r=−0.323, p=0.001), serum phosphate (r=0.205, p=0.029), serum 25-hydroxyvitamin D (r=−0.231, p=0.017), PTH (r=0.473, p<0.0001), and P1NP (r=0.775, p<0.001). After controlling for age and GFR, significant correlations remained with serum 25-hydroxyvitamin D (r=−0.214, p=0.032), PTH (r=0.471, p=0.0001), and P1NP (r=0.84, p=0.001).
Serum P1NP was correlated with age (r=−0.253, p=0.009), serum 25-hydroxyvitamin D (r=−0.204, p=0.036), PTH (r=0.419, p<0.0001), and CTX (r=0.775, p<0.001). After controlling for age, the correlation with vitamin D was lost. The correlations with PTH and serum CTX persisted (r=0.4436, p=0.0001 and r=0.808, p=0.0001 respectively).
Discussion
In this study of male transplant recipients the majority (83%) had some reduction in BMD and 41% were osteoporotic at one or more sites. The overall reduction in BMD was approximately 1 SD and emphasizes that bone loss is not just restricted to female transplant recipients; this is consistent with previous data. In contrast to other studies showing an early bone loss following transplantation with subsequent stabilization or recovery of BMD, we found the lowest BMD measurements in the group 5–10 years after transplantation where the mean T-score was on average 0.5 SD units lower than the other groups at all skeletal sites. There is a site-specific pattern to the bone loss with the femoral neck and radius more severely affected than the spine. Our results indicate a significant reduction in BMD at both trabecular and cortical sites. The disparity between the BMD measurements at the spine and ultradistal radius (both sites rich in trabecular bone) is likely to be due to an artifactual elevation in lumbar spine BMD. Measurement of lumbar spine BMD in patients with renal disease is prone to error due to the presence of vertebral osteosclerosis and aortic vascular calcification.
Overall, 14% of men sustained a fracture following transplantation. While many of these were in the peripheral skeleton, there were two hip and one pelvis fracture. The morbidity associated with even relatively minor fractures in the appendicular skeleton can be considerable in renal transplant recipients. We found a very low prevalence of spinal fractures. This is in keeping with previous studies [5, 6], but contrasts sharply with the pattern seen in other solid organ transplants. While many of the fractures occurred early after transplantation (median time 3 years), the range was wide and late fractures did occur. Attention is often focused on bone protection in the early post-transplant period, our data emphasizes the need for continued vigilance and ongoing evaluation of these patients for post-transplant bone disease.
The mechanisms underlying post-transplant bone disease are complex and potentially difficult to elucidate. A number of studies have identified corticosteroid dose and time since transplantation as significant independent risk factors for osteoporosis. However, in transplant centers that do not operate a steroid withdrawal policy these two variables are highly correlated and can be considered as a single time dependent variable. In this study we were unable to demonstrate any effect of either cumulative corticosteroid dose or time since transplantation on BMD. Animal models have suggested that both cyclosporine and tacrolimus induce a high bone turnover state [1], and some human studies have implicated immunosuppressive medication in the pathogenesis of post-transplant osteopenia. We were unable to demonstrate any effect of cumulative doses of calcineurin inhibitors on BMD, although this may in part be due to the cross-sectional design of the study and the cocktail of immunosuppressive therapy the patients were prescribed.
Another important cause of reduced BMD is persistent hyperparathyroidism. Data from our own center has shown that 52.6% of long-term female post-transplant patients had histomorphometric evidence of hyperparathyroid bone disease [10]. Preexisting hyperparathyroidism has been identified as a factor influencing bone loss both in the early post-transplant period [12, 13] and in long-term transplant recipients [14, 15]. We found high levels of PTH in 72.4% of our patients, and a similar prevalence (81%) has been recently reported by Cayco et al. [16]. Cruz et al. reported an increased rate of bone loss in kidney transplant patients with elevated bone turnover [17], but they were unable to demonstrate a correlation between PTH and either BMD or bone resorption (urine pyridinoline and serum deoxypyridinoline). Our data shows a good correlation between PTH and both S-CTX and P1NP, which also strongly correlated with each other. Bone resorption markers were elevated in 48% of our patients, and bone formation markers increased in 20%. While this may reflect a reduced sensitivity of P1NP to detect an increase in bone turnover we suspect it is a result of uncoupling of bone formation and resorption. We postulate that this uncoupling is related to corticosteroid treatment, which is known to impair bone formation. Our data support the hypothesis that hyperparathyroidism contributes to a high bone turnover state resulting in ongoing bone loss particularly at peripheral sites. The combination of a corticosteroid-induced reduction in bone formation and an increase in bone resorption driven by hyperparathyroidism could produce a state of highly disorganized bone turnover that may adversely affect both bone density and bone quality.
Secondary hyperparathyroidism is a well-recognised and significant problem among dialysis patients, and although PTH often decreases following a successful renal transplant it may well remain elevated in those with severe pretransplantation hyperparathyroidism [15]. The important influence of preexisting hyperparathyroidism is consistent with the correlation between PTH and time on dialysis. PTH rises early in chronic renal failure (when creatinine clearance falls below 70 ml/min) and in the present study correlated with GFR, suggesting that the parathyroid hyperplasia is in part a consequence of mild to moderate post-transplant chronic renal failure. A fifth of our patients were vitamin D deficient probably due to reduced sun exposure (as a result of the higher latitude and concerns about skin malignancy after transplantation), and this will also contribute to hyperparathyroidism.
Pretransplant renal osteodystrophy may also reduce bone mineral density, and such patients show a PTH-independent decline in BMD as renal function worsens [18]. Patients on dialysis show an increased prevalence of osteopenia and our own cross-sectional study of hemodialysis patients identified femoral neck osteopenia in 48.9% and osteoporosis in 19.3% [19]. However, those patients were, on average, 10 years older than the current cohort in whom GFR did not correlate with BMD.
Bivariate analysis identified a number of other factors that appeared to influence BMD. Low body mass index is a well-known risk factor for osteoporosis in normal populations with a positive correlation between weight and BMD, so a similar association in the present study is not surprising. Patients with diabetes had a significantly lower BMD at the femoral neck (0.771 g/cm2 vs 0.890 g/cm2; p=0.007), and other studies have shown that diabetes carries a particular risk of fractures, particularly at appendicular sites.
We conclude that in this relatively young cohort of men there is a high prevalence of reduced BMD (83%), with the femoral neck and radius being most severely affected. Increased bone resorption secondary to hyperparathyroidism is an important factor in this loss of bone. Therefore, the medical management of hyperparathyroidism in patients with chronic kidney disease on the transplant waiting list should be intensified. Timely surgical intervention should be utilized in patients who do not respond to medical management before they are transplanted. The recent introduction of calcimimetics offers a promising new therapy enabling control of hyperparathyroidism without the complications of hypercalcemia and hyperphosphatemia which often limit the use of vitamin D sterols in dialysis patients. Following transplantation, regular attention should be paid to calcium, phosphate, and PTH. Transplant recipients should be evaluated for 25-hydroxyvitamin D deficiency and have this treated with parent vitamin D before resorting to the more potent active vitamin D sterols. The use of active vitamin D sterols in this group of patients is likely to be limited by the relatively high prevalence of hypercalcemia and concerns about aggravating vascular calcification. Surgical parathyroidectomy is an additional option, although not without its risks including deterioration in graft function. The increasing evidence that a high resorption state is important in the pathophysiology of bone loss following renal transplantation provides a strong rationale for the use of antiresorptive agents such as bisphosphonates to treat this complication [20]. The role of calcimimetics in this situation is unclear at present, but worthy of further study.
References
Epstein S (1996) Post-transplantation bone disease: the role of immunosuppressive agents and the skeleton. J Bone Miner Res 11:1–7
Julian BA, Laskow DA, Dubovsky J, Dubovsky EV, Curtis JJ, Quarles LD (1991) Rapid loss of vertebral mineral density after renal transplantation. N Engl J Med 325:544–550
Pichette V, Bonnardeaux A, Prudhomme L, Gagne M, Cardinal J, Ouimet D (1996) Long-term bone loss in kidney transplant recipients: a cross-sectional and longitudinal study. Am J Kidney Dis 28:105–114
Grotz WH, Mundinger FA, Gugel B, Exner V, Kirste G, Schollmeyer PJ (1994) Bone fracture and osteodensitometry with dual energy X-ray absorptiometry in kidney transplant recipients. Transplantation 58:912–915
Nisbeth U, Lindh E, Ljunghall S, Backman U, Fellstrom B (1999) Increased fracture rate in diabetes mellitus and females after renal transplantation. Transplantation 67:1218–1222
Ramsey-Goldman R, Dunn JE, Dunlop DD, Stuart FP, Abecassis MM, Kaufman DB, Langman CB, Salinger MH, Sprague SM (1999) Increased risk of fracture in patients receiving solid organ transplants. J Bone Miner Res 14:456–463
Roe SD, Porter CJ, Green D, Hosking DJ, Cassidy MJ (2000) Low energy fractures and vertebral deformities in UK renal allograft recipients. J Am Soc Nephrol 11:3006A
Shane E, Rivas MC, Silverberg SJ, Kim TS, Staron RB, Bilezikian JP (1993) Osteoporosis after cardiac transplantation. Am J Med 94:257–264
Navasa M, Monegal A, Guanabens N, Peris P, Rimola A, Munoz-Gomez J, Visa J, Rodes J (1994) Bone fractures in liver transplant patients. Br J Rheumatol 33:52–55
Parker CR, Freemont AJ, Blackwell PJ, Grainge MJ, Hosking DJ (1999) Cross-sectional analysis of renal transplantation osteoporosis. J Bone Miner Res 14:1943–1951
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 130:461–470
Torregrosa JV, Campistol JM, Montesinos M, Fenollosa B, Pons F, Martinez de Osaba MJ, Oppenheimer F (1995) Factors involved in the loss of bone mineral density after renal transplantation. Transplant Proc 27:2224–2225
Almond MK, Kwan JT, Evans K, Cunningham J (1994) Loss of regional bone mineral density in the first 12 months following renal transplantation. Nephron 66:52–57
Dumoulin G, Hory B, Nguyen NU, Bresson C, Fournier V, Bouhaddi M, Chalopin JM, Saint-Hillier Y, Regnard J (1997) No trend toward a spontaneous improvement of hyperparathyroidism and high bone turnover in normocalcemic long-term renal transplant recipients. Am J Kidney Dis 29:746–753
Torres A, Rodriguez AP, Concepcion MT, Garcia S, Rufino M, Martin B, Perez L, Machado M, de Bonis E, Losada M, Hernandez D, Lorenzo V (1998) Parathyroid function in long-term renal transplant patients: importance of pre-transplant PTH concentrations. Nephrol Dial Transplant 13:94–97
Cayco AV, Wysolmerski J, Simpson C, Mitnick MA, Gundberg C, Kliger A, Lorber M, Silver D, Basadonna G, Friedman A, Insogna K, Cruz D, Bia M (2000) Posttransplant bone disease: evidence for a high bone resorption state. Transplantation 70:1722–1728
Cruz DN, Wysolmerski JJ, Brickel HM, Gundberg CG, Simpson CA, Mitnick MA, Kliger AS, Lorber MI, Basadonna GP, Friedman AL, Insogna KL, Bia MJ (2001) Parameters of high bone-turnover predict bone loss in renal transplant patients: a longitudinal study. Transplantation 72:83–88
Rix M, Andreassen H, Eskildsen P, Langdahl B, Olgaard K (1999) Bone mineral density and biochemical markers of bone turnover in patients with predialysis chronic renal failure. Kidney Int 56:1084–1093
Taal MW, Masud T, Green D, Cassidy MJ (1999) Risk factors for reduced bone density in haemodialysis patients. Nephrol Dial Transplant 14:1922–1928
Fan SL, Almond MK, Ball E, Evans K, Cunningham J (2000) Pamidronate therapy as prevention of bone loss following renal transplantation. Kidney Int 57:684–690
Acknowledgements
This study was supported by a grant from the National Kidney Research Fund.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Roe, S.D., Porter, C.J., Godber, I.M. et al. Reduced bone mineral density in male renal transplant recipients: evidence for persisting hyperparathyroidism. Osteoporos Int 16, 142–148 (2005). https://doi.org/10.1007/s00198-004-1653-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-004-1653-y