Abstract
The use of HMG-CoA-reductase inhibitors (statins) has been associated with decreased risk of bone fractures in epidemiological studies. In vitro evidence suggests that statins may stimulate bone formation, but the data are still preliminary. We assessed the effects of the HMG-CoA-reductase inhibitor atorvastatin on biochemical parameters of bone metabolism in a multicenter, randomized, double-blind, placebo-controlled trial conducted between October 2001 and October 2002 in three hospital-based outpatient metabolism clinics. Forty-nine postmenopausal women, mean age 61 ± 5 years, mean time postmenopause 12.6 ± 8.8 years, were treated with atorvastatin, 20 mg per day (n=24) or matching placebos (n=25) for 8 weeks. Comparing the differences to baseline between the groups, there were no statistically significant effects of atorvastatin either on the bone formation markers intact osteocalcin and bone-specific alkaline phosphatase or on the bone resorption markers C-telopeptide and intact parathyroid hormone. The marker of bone fractures, undercarboxylated osteocalcin, was also unchanged. When analyzed in dependence of age, atorvastatin increased C-telopeptide and osteocalcin in the younger subjects, while it decreased them in older subjects. Most interestingly, in older subjects, atorvastatin caused a significant decrease in the ratio of C-telopeptide to osteocalcin, an indicator of bone remodeling, while the ratio was increased in younger subjects, suggesting beneficial effects on bone turnover exclusively in older individuals (approx. >63 years). In summary, the present data suggest that short-term treatment with atorvastatin may have age-dependent effects on biochemical markers of bone turnover in postmenopausal women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The statins, 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors, have been shown to reduce blood cholesterol levels and to decrease the risk of cardiovascular disease [1]. In recent years, there has been increasing interest regarding the potential beneficial effects of statins on bone metabolism, especially their putative potential to reduce fracture risk [2]. Various in vitro and in vivo studies tried to verify or disprove this suggestion, but the results have been until now controversial. While some studies, such as the uncontrolled cohort study of Chan et al., showed favorable changes in bone turnover parameters [3], increases in bone density [4, 5, 6, 7, 8], or decreases in fracture risk [5, 9, 10, 11, 12, 13], others failed to show any significant effects on biochemical parameters of bone metabolism [14, 15] or bone density [14, 16], or on fracture risk [17, 18, 19, 20, 21, 22, 23]. There have been no randomized trials with bone mineral density outcomes [24].
There are various possible reasons for these divergent findings, such as the fact that the effects of statins on bone are weak, that control groups were small, obesity was not controlled for, the physical activity of the subjects was not quantified, and the doses used might have been too low (current statins target the liver rather than the bones, and in most of them, less than 5% of a given dose reaches the systemic circulation [25]). Another quite important factor though, could be the extremely limited number of prospective randomized trials available at present, numbering only four. The majority of the studies were observational and thus it cannot be excluded that bias or confounding effects may be responsible for the results showing bone-protective effects of statins. In short, statin users may display other, unidentified characteristics or health behaviors that are associated with decreased rates of fractures, such as lifestyle measures, exercise, supplements, or unreported medications. The prospective studies consist of a small study of 17 patients treated with simvastatin for 4 weeks [10], a study of 20 patients treated with fluvastatin or pravastatin for 1 year [7, 8], a study examining the effects of fluvastatin plus vitamin C vs vitamin C on bone turnover markers [15], and a population-based cohort study examining the effects of statins on BMD [16].
The effects of statins have been attributed to the statin-induced expression of bone morphogenetic protein-2 (BMP-2), a protein playing an important role in stimulating osteoblast differentiation and bone formation [26]. The statins, which exert their effects through influencing the mevalonate pathway, thus became interesting candidates to beneficially influence bone metabolism through anabolic pathways. The importance of the mevalonate pathway in bone metabolism also became evident recently after the discovery that members of the potent, nitrogen-containing class of antiresorptive bisphosphonate drugs inhibit bone resorption by inhibiting one or more enzymes downstream of HMG-CoA reductase in the mevalonate pathway of osteoclasts [27]. However, even though the vast majority of the currently existing studies support the concept that statins work by stimulating bone formation, a recently published in vitro study showed that statins inhibit bone resorption but do not increase bone formation [28]. Most existing antiresorptive and anabolic agents (with the exception of calcitonin [29]) that prevent fractures have substantial effects on biochemical markers of bone resorption and formation, often with changes of up to 50–60% compared with pretreatment levels [30].
We performed the first prospective, randomized, placebo-controlled study to examine the effects of atorvastatin on established anabolic and catabolic markers of bone turnover in postmenopausal women.
Subjects and methods
Study subjects
Subjects were recruited by local advertisements or by word-of-mouth. Fifty women were included into the study after a detailed medical history was obtained and physical examination and laboratory testing was performed. Major inclusion criteria were women >55 years of age with a minimum postmenopause period of 2 years and an appropriate calcium intake of >1,000 mg per day, as ensured by a written dietary questionnaire. Major exclusion criteria were history or evidence of metabolic bone disease other than postmenopausal bone loss (e.g., hyperparathyroidism, hypoparathyroidism, Paget’s disease of the bone, Cushing’s syndrome, osteomalacia), history of parathyroidectomy, untreated hyperthyroidism (defined as fT4 > 1.5 times the upper limit of normal (ULN) and suppressed TSH), untreated or inadequately treated hypothyroidism (defined as TSH greater than twice ULN while being treated with thyroid hormone supplementation), known liver disease and/or elevated serum transaminases >2 times ULN, known kidney disease and/or serum creatinine >1.2 mg/dl, severe heart disease, known muscular or neuromuscular disease and/or serum creatinine kinase >3 times ULN, malignancies, contraindications against or known intolerability of statins, use of statins within 6 months prior to enrollment, use of nonstatin lipid-lowering drugs within 8 weeks prior to enrollment, any kind of estrogen and/or progesterone replacement therapy within 6 months prior to enrollment, use of bisphosphonates for a period >12 months at any time prior to enrollment or within 12 months prior to enrollment, use of calcitonin within 6 months of enrollment, use of fluoride-containing drugs within 12 months prior to enrollment, use of vitamin D >1,000 IU per day within 12 months of enrollment, use of any drugs known to affect bone metabolism, history of long-term corticosteroid use (more than 2 months) in the past year, history of fractures within the last 12 months, history of diabetes mellitus and complete lack of exercise. Current smokers were also excluded.
Study design
This prospective randomized study was conducted at three centers across Germany in outpatient metabolism clinics of large hospitals (one heart center and two university hospitals). Ethics committee approval was obtained for all three study sites. Written informed consent was obtained from all subjects before entry into the study. The study was conducted in accordance with the guidelines of the Declaration of Helsinki.
Intervention
Subjects were randomly assigned (in blocks of six) to one of the following groups: atorvastatin, 20 mg per day (n=25), or matching placebo (n=25), for 8 weeks. Patients returned for safety laboratory measurements after 4 weeks and for a final visit after 8 weeks. Compliance with the treatment regimen was determined at the end of the study by pill count and by measurement of blood lipid concentrations. All investigators were blinded as to the lipid measurements. Dietary questionnaires were performed at baseline and at 8 weeks by use of the 24-hour-recall technique. Blood samples were obtained by venipuncture after an overnight fast, between 7:30 and 9:00 in the morning. The intraindividual variation was not more than 30 minutes. Serum was aliquoted immediately after collection and stored at –25°C until analysis.
Laboratory methods
Analyses were performed in one single batch for each parameter. Two specific osteocalcin forms (intact osteocalcin and undercarboxylated osteocalcin) were measured in the serum samples: Serum intact osteocalcin (intact OC) was measured by an ELISA test kit supplied by DRG Diagnostics (Marburg, Germany). The assay uses monoclonal antibodies against distinct epitopes of human OC. Physiologically inactive N-terminal and C-terminal peptide fragments of osteocalcin do not interfere in this test at their maximum levels found in normal and pathological samples. The intraassay coefficient of variation (CV) is 2.5% at a level of 11.5 ng/ml and the interassay CV is 9.2% at a level of 9.4 ng/ml. Serum undercarboxylated osteocalcin (ucOC) was measured by a commercially available ELISA test kit supplied by Takara Shuzo (Kyoto, Japan). The kit utilizes mouse monoclonal anti-ucOC antibodies to detect ucOC. The kit specifically measures ucOC with 5% cross-reactivity with human bone OC (probably carboxylated type). Thus, the physiological (carboxylated) form of osteocalcin is not determined with this test kit. The intra-assay CV is 4.6% at a level of 6.9 ng/ml and the interassay CV is 5.7% at a level of 6.5 ng/ml. Bone-specific alkaline phosphatase was analyzed by an ELISA test kit supplied by Quidel (Heidelberg, Germany).
Alpha-C-telopeptide of type I collagen (CTx) and intact parathyroid hormone (PTH) were measured by ELISA assays using commercial test kits supplied by Nordic Bioscience Diagnostics (Hamburg, Germany) and DRG Diagnostics (Marburg, Germany), respectively. 17β-Estradiol concentrations were determined by means of an ultrasensitive 125I-labeled RIA test kit supplied by DRG Diagnostics (Marburg, Germany). The intraassay CVs of the bone markers and hormones, were all below 7% and all interassay CVs were below 9%. Concentrations of serum calcium (Ca) and serum albumin were analyzed using flame atomic absorption photometry (AAS 3030, Perkin Elmer, Überlingen, Germany) and a colorimetric test kit (BioMerieux, Nürtingen, Germany), respectively. The CVs for these methods were below 2.5%. Total serum Ca2+ was corrected with ±0.11 mM for each 0.100 mM deviation of concomitant serum albumin from a normal mean of 0.600 mM (CaC) [31].
Statistical analysis
All data available from all patients included in the trial except for one dropout patient were included in the statistical analysis. Thus, no “last observation carried forward” procedure was necessary. Data collection and review procedures were performed blinded to treatment groups. Changes over time within groups were analyzed using two-sided Wilcoxon signed rank tests. Baseline values and relative changes over time between the groups were analyzed by Mann-Whitney U-tests for unpaired data.
To assess interrelationships between variables, the Pearson correlation coefficient was used. Analysis of variance and a multiple regression analysis model were used to identify multiple independent parameters influencing linear dependent parameters.
Sample size was determined a priori using change in the bone formation marker, osteocalcin, as the primary outcome measure and extrapolating changes and SD from the literature. The target sample size was determined to detect a change of 25%.
Variables are reported as mean ± standard deviation (SD) unless otherwise indicated. Results were considered statistically significant at a 2-tailed P<0.05. P values between 0.05 and 0.10 were considered borderline significant. StatView Version 5.0 (SAS Institute) was used for all analyses.
Results
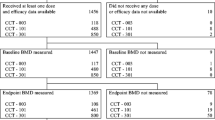
The characteristics of each treatment group were similar at baseline (Table 1) except for slightly but significantly higher body weight and body mass index in the statin group. The women ranged in age from 53 to 78 years, with a mean age of 61 years. All of them were Caucasian. They were all nonsmokers, 67% had never smoked, 33% were ex-smokers for >1 year. Their mean age at menopause was 49 years, the mean time period since menopause was 12 years. The estradiol levels were not different between the groups (Table 1). Physical activity levels were comparable between the groups. The number of women reporting never, 1 to 2 times, 3 to 4 times, or daily endurance activities were 15, 6, 2, and 2 in the control group, and 10, 8, 2, and 4 in the statin group, respectively (χ-square P=0.59).
Of the 25 women randomized into each treatment group one subject (atorvastatin group) terminated the study after 4 weeks because of an episode of viral bronchitis. No serum sample for determination of study parameters was collected from this individual. All other subjects finished the study per protocol. Mean treatment duration was 57 ± 2 days (range 53–68 days). Compliance, as determined by pill count, was between 80% and 107% in all subjects (mean 97±0.5%). There were no differences in treatment duration or compliance between the groups.
Bone metabolism
Parameters of bone metabolism are given in Table 2. Baseline levels of these parameters did not differ significantly between the groups. The bone resorption marker, CTx, as well as the bone formation marker, intact OC, were not significantly different between baseline and 8 weeks in either group. The levels of intact OC did not change in the statin group but increased by 9% (P<0.03) in the placebo group. The percentage change between the two groups though (statin vs placebo) was not significant (P=0.73). The ratio of CTx to osteocalcin, an index of bone remodeling, remained unchanged (mean change –1.9% in the statin and +3.1% in the placebo group). The same was true for ucOC, although there was a 30% increase in the control group which almost reached statistical significance (P=0.06). Since ucOC also increased by about 12% in the atorvastatin group, the comparison of the percentage change between the groups was not significant (P=0.30). The ratio of ucOC to intact OC remained unchanged. There were no changes in intact PTH in both groups. BSAP remained unchanged in the statin group but increased by 7.3% in the placebo group, a small but statistically significant change.
Calcium, phosphate, nutrient intake, and lipoproteins
Calcium and phosphate levels remained constant in both groups (Table 3). Lipoprotein concentrations changed significantly as expected under treatment with atorvastatin. Low density lipoprotein (LDL) decreased significantly by 49±12%, total cholesterol by 33±9%, and triglycerides by 17±27% in the treatment group, while high density lipoprotein (HDL) cholesterol remained unchanged. There were no changes in the control group.
Nutrient intake (total caloric intake, percentage calories from fat, carbohydrates, protein, and alcohol) as well as calcium intake remained constant during the 8-week intervention period as verified by the 24-hour recall technique (data not shown).
Correlation analyses
Correlation analyses are shown in Table 4 and in Fig. 1. Baseline CTx and osteocalcin levels were not correlated with age. The ratio of CTx to osteocalcin, an indicator of bone remodeling, tended to be negatively correlated with age (R=−0.27; P=0.061). Age and the time since menopause were significantly negatively correlated with the change in CTx in the statin group but not in the placebo group. This correlation remained significant even after removal of the two or three oldest subjects. Thus, an association with higher CTx was observed under atorvastatin in younger subjects (<63–64 years), while old age was associated with lower values. Moreover, menopause duration <15 years was associated with higher CTx values, while in menopause of longer duration the values were lower. There was no correlation of this kind in the control group. In the statin group, age was significantly (P=0.055) negatively associated with the change in osteocalcin—i.e., it increased at age <66 years and decreased at age >66 years. The same was seen with the effect of age on the change in the ratio of CTx to osteocalcin in the statin group (P=0.011). The ratio increased at age <62 years, while it decreased at age >62 years, indicating larger beneficial effects of statins on bone remodeling processes with greater age.
Simple linear regression analysis with age as the independent and percentage change in biochemical parameters of bone metabolism as dependents. C-telopeptide: A control group, R=0.103, P=0.63; B atorvastatin group, R=0.76, P<0.0001. Osteocalcin: C control group, R=0.25, P=0.23; D atorvastatin group, R=0.40, P=0.055. Ratio C-telopeptide to osteocalcin: E control group, R=0.008, P=0.97; F atorvastatin group, R=0.51, P=0.011
Multivariate analyses
Analysis of variance (Table 5) indicates that age (P=0.0024) and treatment (P=0.025) have a significant influence on the change in CTx and that there is a significant interaction between the two independent parameters. The change in osteocalcin, however, was only significantly influenced by age (P=0.0295), not by treatment. The change in the ratio of CTx to osteocalcin tended to be influenced by age and by treatment, and there was a trend toward a significant interaction.
A multiple regression model was used to investigate the influence of age, time since menopause, body mass index, estradiol, free thyroxin, and baseline serum calcium on changes in bone metabolic parameters. In the statin group the change in C-telopeptide was significantly determined by age (not in the placebo group). The change in intact OC was significantly determined in the statin group by creatinine, age, and free thyroxin (not in the placebo group). The change in the CTx to osteocalcin ratio was not significantly determined by the aforementioned parameters in either group.
Discussion
The present study investigated the effect of 8 weeks treatment with the HMG-CoA reductase inhibitor atorvastatin on biochemical parameters of bone metabolism in postmenopausal women. Various biomarkers of bone metabolism have been developed during recent years [32, 33]. In this study we measured as markers of bone formation intact OC and the bone-specific alkaline phosphatase (BSAP), and as a marker of bone catabolism, CTx. We also measured undercarboxylated osteocalcin. Serum ucOC can be regarded as an indicator of hip fractures [34, 35]. Our results do not show a significant effect of atorvastatin on bone metabolism in the group as a whole. Taking the age of the subjects into account, however, it could be demonstrated that in the atorvastatin group both CTx and OC, as well as the ratio of the two, were associated with higher values in younger subjects (<63 years of age), while these parameters were lower in older subjects. This observation adds an interesting new aspect to the debate regarding the conflicting results as to whether statins have beneficial effects on bone health and might explain the contradictory findings. Although the epidemiological studies [10, 11, 12, 13] suggesting decreased risk of fractures in subjects exposed to statins showed these effects even after adjusting for age, they may not be able to eliminate the confounding that can only be avoided in prospective studies.
An 8-week treatment should be an adequate time period to observe potential statin effects on bone, based on the following evidence: Intervention with bisphosphonates reduces osteoclastic bone resorption significantly already after 1 week of treatment [36, 37]. An increase in bone formation and some inhibition of osteoclastic activity by statins was seen in a rodent model after only 5 weeks of treatment [26], and simvastatin has been shown in humans to increase OC within 4 weeks of treatment [3]. Furthermore, treatment of merely 180 days has been associated with a reduction in hip fracture in elderly patients [12]. The lipid-lowering effects of statins are visible after a few days and their full development is usually seen after 4–6 weeks of treatment. There is no evidence suggesting that pharmacological effects of statins related to lipids would need more than a few weeks to develop. In the present study, the changes in blood cholesterol served as an indicator of compliance. Based on the excellent compliance of the subjects, a lack of actual treatment cannot be made responsible for the lack of effects on bone metabolism. In addition, non-lipid serum markers that are also affected by statins, such as C-reactive protein, are significantly changed after short-term treatment [38]. The choice of atorvastatin was based on its wide clinical use as well as on its powerful lipid-lowering potency, which was confirmed in the present study. Furthermore, a recently published experimental study showed that the ability of statins to beneficially influence bone metabolism is directly correlated with the potency of the compounds for inhibition of HMG-CoA reductase activity [28]. In addition, atorvastatin was widely used in many of the existing retrospective studies reporting decreased risk of fractures in statin users [10, 11, 12].
While the clinical relevance of serum levels of biochemical markers of bone turnover is still under dispute, the fact that they provide dynamic information about bone metabolism that is not provided by single measurements of BMD or bone histomorphometry has been established [39]. Specifically, a statistically significant relationship between individual bone remodeling markers and BMD at different skeletal sites has been shown [40], and elevated bone resorption markers appear to be associated with increased fracture risk in elderly women [41, 42]. Therefore, our data support very recent reports, which fail to show either BMD increase [14, 16] or fracture prevention [17, 18, 19, 20, 21] among statin users.
A probable explanation for the lack of statin-induced effects on bone metabolism could be the fact that only a small proportion of ingested statins reaches the peripheral circulation after first-pass metabolism [25], the circulating concentrations in humans, unlike rats, are very low—in the submicromolar range—therefore most likely below the threshold of concentrations needed to produce effects on bone. Atorvastatin, in contrast to other statins, has a relatively high systemic bioavailability of about 30%. In our study a daily dose at the upper end of normally recommended doses for cholesterol lowering in humans was used. Mundy et al. [26] used statin doses in their rodent trials that were about tenfold higher than the doses currently recommended for cholesterol lowering. Based on the results from animal experiments it seems that indeed the dose used may have a significant influence on bone metabolism. Specifically, with high doses of simvastatin, an increase in bone formation and absorption was found, but with low doses, a decrease in bone formation and an increase in bone resorption [43].
Our data do not support results of an earlier cross-sectional study, in which 140 postmenopausal women treated with statins (simvastatin 65%, atorvastatin 15%, lovastatin 8.6%, pravastatin 5.7%, fluvastatin 5%, cerivastatin 0.7%) for more than 2 years (median 4 years) were compared with 140 nontreated controls [14]. Results showed that OC, BSAP, and CTx were all significantly decreased by 9% to 14%, while PTH was increased by 16%. There was however no difference in the BMD at the lumbar spine, hip, forearm, and whole body between the two groups [14]. Since preclinical data suggest differences in the bone effects of the various statins [24], a separate analysis concerning the effect of the different statins on bone would have been helpful.
Our results are in agreement with those of Stein et al. [44] who analyzed stored serum samples from a 12-week, randomized, multicenter, open-label study designed to compare the effects of atorvastatin and simvastatin on cardiovascular parameters in 846 hypercholesterolemic patients. They found that 12 weeks of treatment with 20 and 40 mg of atorvastatin had no significant effects either on BSAP or on CTx. Interestingly though, simvastatin 40 mg and 80 mg/day led to significant reductions in BSAP in both men and women, while CTx showed a small, but not statistically significant, decrease. In the first, though small, prospective study examining the effects of simvastatin on metabolic bone parameters after a 4-week period, a significant increase in serum OC was shown, whereas all other bone markers such as BSAP, urine deoxypyridinoline, and urine cross-linked N-telopeptide of type 1 collagen did not change [3]. Since in that study the simvastatin dose was only 20 mg, results on BSAP cannot be directly compared with the data of Stein et al. [44]. Moreover, the aforementioned study can be criticized for its small size (17 subjects) and the heterogeneous structure (6 males, 11 females, age 40–79). Similar to our study results with atorvastatin, no effects of fluvastatin (40 mg/day) on biomarkers of bone turnover such as midterminal OC, total alkaline phosphatase, and CTx was observed in postmenopausal women [15].
Even though the observed increase in BSAP and intact OC concentrations in the placebo group at the end of the study compared with baseline levels (Table 2) remains puzzling (most likely the result of multiple testing), the changes between the groups were not significantly different. An interesting finding of the present study was the unexpected influence of age on the effects of atorvastatin on bone turnover parameters. The fact that older individuals benefit more from statin therapy regarding LDL has already been shown [45]. However, this is the first report demonstrating age-dependent effects of statins on bone. How can this effect be explained? Aging is associated with a decrease in bone formation in both men and women. In postmenopausal women in particular, estrogen deficiency increases remodeling, accelerating bone loss. At each remodeled site, more bone is resorbed and less is formed [46]. Thus, statins may act by attenuating the age-induced decrease in bone formation possibly by up-regulating BMP-2, as shown in vitro and in rodents [26].
In conclusion, the present study provided the first set of prospective data on the effect of atorvastatin on bone metabolism using specific biochemical bone markers. It was a double-blind, prospective, randomized, controlled trial. Atorvastatin given in doses that result in the normally expected lowering of lipids had no effect on bone formation and bone resorption markers in the group as a whole. However, when the age of the subjects is taken into account, it was demonstrated that atorvastatin may influence bone metabolism exerting protective effects mainly in older subjects (age >63–64 years). Large-scale, long-term, randomized, controlled, prospective trials using various statins are needed in order to obtain a final answer regarding the effects (if any) of statins on bone.
References
LaRosa JC, He J, Vupputuri S (1999) Effects of statins on risk of coronary heart disease: a meta-analysis of randomized controlled trials. JAMA 282:2340–2346
Schlienger RG, Meier CR (2003) HMG-CoA reductase inhibitors in osteoporosis—do they reduce the risk of fracture? Drugs Aging 20:321–336
Chan MHM, Mak TWL, Chiu RWK, Chow C-C, Chan IHS, Lam CWK (2001) Simvastatin increases serum osteocalcin concentration in patients treated for hypercholesterolaemia. J Clin Endocrinol Metab 86:4556–4559
Chung YS, Lee MD, Lee SK, Kim HM, Fitzpatrick LA (2000) HMG-CoA reductase inhibitors increase BMD in type 2 diabetes mellitus patients. J Clin Endocrinol Metab 85:1137–1142
Bauer DC, Sklarin PM, Stone KL, Black DM, Nevitt MC, Ensrud KE, Arnaud CD, Genant HK, Garnero P, Delmas PD, Lawaetz H, Cummings SR (1999) Biochemical markers of bone turnover and prediction of hip bone loss in older women: the study of osteoporotic fractures. J Bone Miner Res 14:1404–1410
Edwards CJ, Hart DJ, Spector TD (2000) Oral statins and increased bone mineral density in postmenopausal women. Lancet 355:2218–2219
Watanabe S, Fukomoto S, Takeuchi Y, Nakano T, Fujita T (2000) Effects of one year treatment with statins on bone mass and metabolism (abstract). J Bone Miner Res 15[Suppl]:S194
Watanabe S, Fukomoto S, Takeuchi Y, Nakano T, Fujita T (2000) Effects of 1-year treatment with fluvastatin or pravastatin on bone. Am J Med 110:584–587
Bauer DM, Mundy GR, Jamal SA, Black DM, Cauley JA, Duong T, Cummings SR (1999) Statin use, bone mass and fracture: an analysis of two prospective studies (abstract). J Bone Miner Res 14[Suppl]:S179
Chan KA, Andrade SE, Boles M, Buist DSM, Chase GA, Donahue JG, Goodman MJ, Gurwitz JH, LaCroix AZ, Platt R (2000) Inhibitors of hydroxymethylglutaryl-coenzyme A reductase and risk of fracture among older women. Lancet 355:2185–2188
Meier CR, Schlienger RG, Kraenzlin ME, Schlegel B, Jick H (2000) HMG-CoA reductase inhibitors and the risk of fractures. JAMA 283:3205–3210
Wang PS, Solomon DH, Mogun H, Avorn J (2000) HMG-CoA reductase inhibitors and the risk of hip fractures in elderly patients. JAMA 283:3211–3216
Pasco JA, Kotowicz MA, Henry MJ, Sanders KM, Nicholson GC (2002) Statin use, bone mineral density, and fracture risk: Geelong Osteoporosis Study. Arch Int Med 162:537–540
Rejnmark L, Buus NH, Vestergaard P, Andreasen F, Larsen ML, Mosekilde L (2002) Statins decrease bone turnover in postmenopausal women: a cross-sectional study. Eur J Clin Invest 32:581–589
Bjarnason NH, Riis BJ, Christiansen C (2001) The effect of fluvastatin on parameters of bone remodeling. Osteoporos Int 12:380–384
Sirola J, Sirola J, Honkanen R, Kroger H, Jurvelin JS, Maenpaa P, Saarikoski S (2002) Relation of statin use and bone loss: a prospective population-based cohort study in early postmenopausal women. Osteoporos Int 13:537–541
LaCroix AZ, Cauley JA, Jackson R, McGowen J, Pettinger M, Hsia J, Chen Z, Lewis CE, Bauer D, Daugherty S, McNeeley SG, Passero M (2000) Does statin use reduce risk of fracture in postmenopausal women? Results from women’s health initiative study (WHI-OS) (abstract). J Bone Miner Res 15:S155
van Staa T-P, Wegman S, de Fries F, Leufkens B, Cooper C (2001) Use of statins and risk of fractures. JAMA 285:1850–1855
Reid IR, Hague W, Emberson J, Baker J, Tonkin A, Hunt D, MacMahon S, Sharpe N, The LIPID Study Group (2001) Effect of pravastatin on frequency of fracture in the LIPID study: secondary analysis of a randomized controlled trial. Lancet 357:509–512
Petersen TR, Kjekshus J (2000) Statin drugs and the risk of fracture. JAMA 284:1921–1922
Heart Protection Study Collaborative Group (2002) MRC/BHF heart protection study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet 360:7–22
Ray WA, Daugherty JR, Griffin MR (2002) Lipid-lowering agents and the risk of hip fracture in a Medicaid population. Injury Prevention 8:276–279
LaCroix AZ, Cauley JA, Pettinger M, Hsia J, Bauer DC, McGowan J, Chen Z, Lewis CE, McNeeley SG, Passaro MD, Jackson RD (2003) Statin use, clinical fracture, and bone density in postmenopausal women: Results from the Women’s Health Initiative Observational Study. Ann Int Med 139:97–104
Cummings SR, Bauer DC (2000) Do statins prevent both cardiovascular disease and fracture? JAMA 283:3255–3257
Hamelin BA, Turgeon J (1998) Hydrophilicity/lipophilicity: relevance for the pharmacology and clinical effects of HMG-CoA reductase inhibitors. Trends Pharmacol Sci 19:26–37
Mundy G, Garrett R, Harris S, Chan J, Chen D, Rossini G, Boyce B, Zhao M, Guttierez G (1999) Stimulation of bone formation in vitro and in rodents by statins. Science 286:1946–1949
van Beek E, Loewik C, van der Pluim G, Papapoulos S (1999) The role of geranylgeranylation in bone resorption and its suppression by bisphosphonates in fetal bone explants in vivo: a clue to the mechanism of action of nitrogen-containing bisphosphonates. J Bone Miner Res 14:722–729
Staal A, Frith JC, French MH, Swartz J, Gungor T, Harrity TW, Tamasi J, Rogers MJ, Feyen JH (2003) The ability of statins to inhibit bone resorption is directly related to their inhibitory effect on HMG-CoA reductase activity. J Bone Miner Res 18:88–96
Chesnut CH, Silverman S, Andriano K, Genant H, Gimona A, Harris S, Kiel D, LeBoff M, Maricic M, Miller P, Moniz C, Peacock M, Richardson P, Watts N, Baylink D (2000) A randomized trial of nasal spray salmon calcitonin in postmenopausal women with established osteoporosis: The Prevent Recurrence of Osteoporotic Fractures Study. Am J Med 109:267–276
Bauer DC (2003) HMG CoA reductase inhibitors and the skeleton: a comprehensive review. Osteoporos Int 14:273–282
Klausen T, Breum L, Sorensen HA, Schifter S, Sonne B (1993) Plasma levels of parathyroid hormone, vitamin D, calcitonin, and calcium in association with endurance exercise. Calcif Tissue Int 52:205–208
Fall PM, Kennedy D, Smith JA, Seibel MJ, Raisz LG (2000) Comparison of serum and urine assays for biochemical markers of bone resorption in potsmenopausal women with and without hormone replacement therapy and in men. Osteoporos Int 11:481–485
Woitge HW, Pecherstorfer M, Li Y, Keck AV, Horn E, Ziegler R, Seibel MJ (1999) Novel serum markers of bone resorption: clinical assessment and comparisons with established urinary indices. J Bone Miner Res 14:792–801
Szulc P, Chapuy P, Meunier J, Delmas PD (1993) Serum undercarboxylated osteocalcin is a marker of the risk of hip fracture in elderly women. J Clin Invest 91:1769–1774
Seibel MJ, Robins SP, Bilezikian JP (1997) Serum undercarboxylated osteocalcin and the risk of hip fracture. J Clin Endocrinol Metab 82:717–718
Pedrazzoni M, Alfano FS, Gatti C, Fantuzzi M, Girasole G, Campanini C, Basini G, Passeri M (1995) Acute effects of bisphosphonates on new and traditional markers of bone resorption. Calcif Tissue Int 57:25–29
Gamero P, Shih WJ, Gineyts E, Karpf DB, Delmas PD (1994) Comparison of new biochemical markers of bone turnover in late postmenopausal osteoporotic women in response to alendronate treatment. J Clin Endocrinol Metab 79:1693–1700
Balk EM, Lau J, Goudas LC, Jordan HS, Kupelnick B, Kim LU, Karas RH (2003) Effects of statins on nonlipid serum markers associated with cardiovascular disease. Ann Int Med 139:670–682
Looker AC, Harris TB, Wahner HW (1992) Assessing hip fracture risk in a population-based health survey: the NHANES III osteoporosis component. Aging (Milano) 4:53–60
Melton LJ, Khosla S, Atkinson EJ, O’Fallon WM, Riggs BL (1997) Relationship of bone turnover to bone density and fractures. J Bone Miner Res 12:1083–1091
Garnero P, Hausherr E, Chapuy MC, Marcelli C, Grandjean H, Muller C, Cormier C, Breart G, Meunier PJ, Delmas PD (1996) Markers of bone resorption predict hip fracture in elderly women: the EPIDOS Prospective Study. J Bone Miner Res 11:1531–1538
van Daele PL, Seibel MJ, Burger H, Hofman A, Grobbee DE, van Leeuwen JP, Birkenhager JC, Pols HA (1996) Case-control analysis of bone resorption markers, disability, and hip fracture risk: the Rotterdam study. Br Med J 312:482–483
Maritz FJ, Conradie MM, Hulley PA, Gopal R, Hough S (2001) Effect of statins on bone mineral density and bone histomorphometry in rodents. Arterioscl Thromb Vasc Biol 21:1636–1641
Stein EA, Farnier M, Waldstreicher J, Mercuri M (2001) Effects of statins on biomarkers of bone metabolism: a randomised trial. Nutr Metab Cardiovasc Dis 11:84–87
Streja L, Packard CJ, Shepherd J, Cobbe S, Ford I, WOSCOPS Group (2002) Factors affecting low-density lipoprotein and high-density lipoprotein cholesterol response to pravastatin in the West of Scotland Coronary Prevention Study (WOSCOPS). Am J Cardiol 90:731–736
Seeman E (2002) Pathogenesis of bone fragility in women and men. Lancet 359:1841–1850
Acknowledgements
We thank Dr Michael Holzem for clinical support, Claudia Krapf for her organizational skills, and Adelheid Schuch for her excellent technical support. Funding/support: None of the authors declared any conflicts of interest. This work was supported in part by funds from the Institute for Clinical Research and Department of Clinical Pharmacology, Center for Cardiovascular Diseases, Rotenburg an der Fulda; Medical Policlinic, University of Bonn; and Department of Nutrition, University of Bonn. The study was entirely independent of funds from the pharmaceutical industry and other commercial enterprises.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Berthold, H.K., Unverdorben, S., Zittermann, A. et al. Age-dependent effects of atorvastatin on biochemical bone turnover markers: a randomized controlled trial in postmenopausal women. Osteoporos Int 15, 459–467 (2004). https://doi.org/10.1007/s00198-004-1598-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-004-1598-1