Abstract
Calcium supplementation is known to increase bone mineral density and decrease fractures, but the relative efficacy of different forms of calcium supplementation is not established. We compared the effects of calcium carbonate and calcium citrate on markers of bone resorption in older postmenopausal women in an open-labeled crossover study. Forty women were randomized to receive 1000 mg/day of either calcium citrate or calcium carbonate for 12 weeks, followed by a 2-week washout without calcium supplements and 12 weeks treatment with the alternate calcium supplement. All women received vitamin D (900 IU/day). Thirty-four women (25 Caucasian, nine Hispanic) completed the study. No significant differences in the decrease in parathyroid hormone (PTH) or bone specific alkaline phosphatase or the increase in urinary calcium/creatinine were detected between the two treatments. However, calcium citrate supplementation decreased the collagen cross-link resorption markers, urinary N-telopeptide (−30%), C-telopeptide (−31%), free deoxypyridinoline (19%) and serum N-telopeptide (−8%), compared to no significant change following calcium carbonate supplementation (+2%, +3%, +2% and +2%, respectively; P<0.05). Calcium citrate decreased markers of bone resorption significantly more than calcium carbonate in postmenopausal women, although no differences in their effects in calcium excretion or PTH were detected.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Calcium supplementation increases bone mineral density and decreases fractures in older men and women [1,2,3,4]. There is debate, however, as to whether different forms of calcium supplementation have differing efficacy, particularly in older women at high risk for osteoporotic fractures. Previous studies demonstrated that calcium citrate was better absorbed in individuals with achlorydia, but there was no difference between calcium carbonate and calcium citrate absorption when given with meals [5]. Using biochemical markers of bone turnover, bone resorption decreased in several trials of older postmenopausal women given calcium carbonate [6], citrate [7,8], calcium lactate-gluconate [9] or citrate malate [10,11]. However, calcium carbonate and calcium citrate have not been directly compared for their effects on bone turnover and calcium regulating hormones.
In the present study, we compared the effects of calcium carbonate and calcium citrate in their commercially available forms on calcium regulating hormones and markers of bone resorption in older postmenopausal women with low bone mass and low calcium intake in an open-labeled crossover study.
Materials and methods
Subjects
The Institutional Review Board at the University of Connecticut Health Center approved the study, and all women gave written informed consent prior to screening evaluation. Mailings were sent to women over age 65 years from a database of women who had previously shown interest in research volunteer opportunities and from newspaper advertisements. Inclusion criteria included women with a bone mineral density (BMD) T-score at the spine or hip of –1 to –3.5, indicating osteopenia or osteoporosis, and N-telopeptide crosslink (NTX) level of >36 BCE/mg creatinine, and hence above the mean for postmenopausal women, using the Osteomark NTX Direct Response assay (Ostex International, Inc., Seattle, Wash., USA). Exclusion criteria were: 1) systemic disease or medication known to affect bone metabolism, such as osteomalacia, hyperparathyroidism, corticosteroids or bisphosphonates; 2) use of any androgens, estrogens or other antiresorptive agents in the last 12 months; 3) any fracture in the previous 6 months; 4) hypercalcuria (>350 mg/g creatinine), hypercalcemia or a history of kidney stones; and 5) inability to swallow the calcium supplements. Any woman on a calcium supplement who wished to be included in the study was instructed to discontinue her supplements 4 weeks prior to her initial visit. One hundred and thirty-six women responded to the recruitment strategies, 89 were eligible after telephone screening, 67 completed BMD and NTX screening and 40 were eligible by all screening criteria randomized into the study.
Treatment
Forty women were randomized to an open-label cross-over study to receive either 1000 mg/day of calcium citrate (Citracal 250+D, two tablets with breakfast and two with supper) or calcium carbonate (OsCal 250+D on the same schedule) for 12 weeks. The study was not blinded because we wished to use the commercially available forms of these supplements in this study. The subjects then had a 2-week washout without calcium supplements and 12 weeks treatment with the alternate calcium supplement. All women received a daily multivitamin containing 400 IU cholecalciferol throughout the study for a total daily vitamin D intake of approximately 900 IU/day.
Evaluations
At the screening visit, participants underwent medical history, physical exam, and measurement of fasting serum ionized calcium (iCa), second voided urinary Ca, Cr and NTX, dietary calcium intake estimate and BMD of the spine and femur. At the beginning of each treatment phase, 4 and 12 weeks, we measured serum markers of bone formation [bone specific alkaline phosphatase (BAP), osteocalcin (OC)] and markers of bone resorption [urine N- and C-telopeptide crosslinks of collagen (NTX, CTX), free deoxypyridinoline crosslinks (DPYR) and serum N-telopeptide crosslinks of collagen (sNTX)]. We also measured parathyroid hormone level (PTH), 25-dihydroxyvitamin D levels (25OHD), ionized calcium and second voided urinary Ca and Cr. We estimated calcium and vitamin D consumption using a standardized calcium/vitamin D food log at baseline, 12 and 26 weeks. Side effects were assessed using a 29-item questionnaire with 4-point Likert response choice including absent, mild, moderate or severe.
Biochemical measurements
Blood and urine samples were collected between 0700 and 0900 hours after a 10- to 12-h fast. Urine and serum were divided into 0.5 ml aliquots and stored at −70°C. Ionized Ca was measured within 2 h of collection. 25-Hydroxyvitamin D [25(OH)D] measurements were performed at Endocrine Sciences Inc., Calabasas Hills, Calif., USA[] using a competitive protein binding assay with an intra-assay CV of <10%. Samples for off-site assay were shipped on dry ice by overnight mail. All bone marker assays and intact PTH were performed on batched serum or urine in the Core Laboratory of the General Clinical Research Center at the University of Connecticut Health Center. All assays for an individual were performed in the same batch. Screening NTX measurements were done using the Osteomark NTX Direct Response assay (Ostex International). Markers of bone formation included BAP and OC measured by ELISA (Metra Biosystems Inc., Palo Alto, Calif., USA; and CIS Bio International, France). Average intra-assay variability was <5% for both measures of bone formation. Markers of bone resorption included NTX, sNTX and CTX measured by ELISA (Ostex International for NTX assays; and Osteometer A/S, Copenhagen, Denmark for CTX assay), DPYR measured by ELISA (Metra Biosystems, Inc., Mountain View, Calif., USA). Intra-assay variability was <10% for measures of bone resorption. Intact PTH is measured by ELISA (Diagnostic Systems Labs, Inc., Webster, Tex., USA) with an average intra-assay variability of 5%.
Statistical analysis
Baseline measures and other clinical characteristics were reported using means and standard deviations, both for all subjects and stratified by treatment group. One-way analysis of variance (ANOVA) was used to assess the difference in baseline characteristics as a function of treatment group. We checked variables for normality of distribution and for the impact of outliers; the log value was used for analysis of variables found not to be normally distributed, namely BAP, OC, NTX and CTX. The study design was a 3 (Time)×2 (Calcium type)×2 (Order) factorial. Repeated-measures analysis of variance was used to detect differential changes over time as a function of treatment group in markers of bone turnover, PTH, 25OHD, serum and urine calcium, as well as in side effects. The model analyzed the within-subjects variables, Time (Baseline, 4- and 12-week Post-test), and Calcium type (carbonate versus citrate), as well as a between-subjects variable, Order of administration (carbonate citrate versus citrate carbonate). All three two-way interactions as well as the three-way interaction were also assessed. All analyses were performed using SPSS version 10.0.
Results
Subject population and disposition
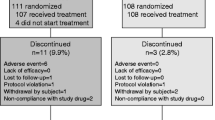
Thirty-four of the 40 women randomized completed the study; six women did not finished for the following reasons: two women were found to be ineligible at baseline visit due to hypercalcemia and history of celiac disease, one women was a difficult blood draw, one women was unable to swallow calcium supplements, one women chose to begin bisphosphonate therapy and one women could not be found for contact after screening was completed. Baseline characteristics of the women are presented in Table 1. Nine subjects were Hispanic by self-report and did not differ from Caucasian subjects in age, baseline NTX, PTH or 25OHD, but did have a higher BMI (32±4 kg/m2; p=0.03)
Biochemical response
Baseline, 4 week and 12 week values for markers of bone resorption, ionized calcium, PTH and urinary calcium excretion are in Table 2. Overall, there was a significant decline in NTX, CTX, DPYR and sNTX after 12 weeks of calcium citrate but not after calcium carbonate (P<0.05 for between treatment period differences; Fig. 1). The responses of osteocalcin, BAP, ionized calcium, PTH, urinary calcium and 25OHD to each calcium preparation from baseline values are outlined in Table 2, although the responses did not differ between the two calcium preparations with the exception of an increase in 25OHD with calcium carbonate. This exception may be explained by higher compliance with calcium carbonate and higher dietary vitamin D intake during the calcium carbonate treatment period (see below). We evaluated for an effect by treatment order and none was found. There was no difference in baseline values between the two treatment periods. There were no differences in response in the subset of Hispanic subjects.
Compliance, measured by pill count, was higher with calcium carbonate (93±11%) than with calcium citrate (85±20%) (P=0.006). As a result, reported mean total calcium intake (diet plus supplement) was higher with calcium carbonate (1650±493 mg/day) compared with calcium citrate (1479±543 mg/day; P=0.026). Similarly, vitamin D intake was 966±146 IU in the calcium carbonate treatment period and 638±150 IU in the calcium citrate treatment period (P<0.001). Side effects were minimal and gastrointestinal side-effects were not different between the two supplements.
Discussion
We compared the effects of calcium carbonate and calcium citrate on bone metabolism in vitamin D replete older women in a randomized, open-label crossover study. After 4 and 12 weeks of calcium supplementation, calcium carbonate and calcium citrate increased urinary calcium excretion and decreased serum PTH concentration to the same degree. However, all four markers of bone resorption, NTX, CTX, Dpyr and sNTX, decreased with calcium citrate, but not with calcium carbonate supplementation. There are few other studies comparing the effects of different calcium supplements on bone turnover markers. One recent short-term study showed decreases of 11–18% in NTX after 1 week of calcium carbonate, milk or orange juice fortified with calcium citrate malate [12]. Studies of response in bone markers with calcium carbonate have included no response in resorption markers [13] as well as decreases of 26% in NTX [6]. Some studies have not specified the source of the calcium but have found an 8% decrease in type I procollagen peptide [14], 8% increase in CTX [15], or increase of 20% in NTX [15]. Studies of response in markers with calcium citrate have shown decreases of 13–35% [7].
The results with biochemical markers suggest that calcium citrate produced a greater inhibition of bone resorption than calcium carbonate. This was not attributable to compliance with calcium supplements since compliance was greater with calcium carbonate. There are a number of other possible explanations for differential effects on these markers. There may have been a differential increase in absorption in the calcium citrate period. Absorption studies have produced variable results. Recker [5] found absorption from calcium citrate and calcium carbonate did not differ when ingested with a meal, although absorption with calcium citrate was greater when given without food. Others have found no differences in absorption following ingestion of food [16] or fasting [17]. However, Pak and associates have reported calcium citrate is better absorbed than calcium carbonate in the fasting state [18,19] and in the non-fasting state [20,21]. It is possible that the average absorption was more rapid with calcium citrate than with calcium carbonate in our study. There is some evidence for this in the study of calcium carbonate and citrate absorption by Heaney et al. [16] in which small and consistent but separately non-significant differences between calcium citrate and calcium carbonate were seen, including a greater rise in ionized calcium at 5–12 h post-calcium ingestion, coincident with greater PTH suppression and higher pooled urinary calcium excretion. Others have found a greater increase in urinary calcium following calcium citrate supplement than with calcium carbonate [21], although not reaching statistical significance in one study [22]. We also saw a slightly higher but not significantly different excretion of calcium in the citrate treatment period.
Another explanation for the differences in the resorption may be related to the differential effects of absorption in calcium carbonate and citrate in the fasting state [5,18,19]. While instructions were to take supplements with the morning and evening meal, compliance with this request may have been incomplete. If some of the women were achlorhydric, this would magnify the difference in calcium absorption in favor of calcium citrate in the fasting state [5]. However, studies in older individuals indicate that nearly 90% do not have impaired gastric acidity [23].
Another possibility is that citrate altered the metabolism of the cross-linked peptides, NTX and CTX. These peptides may be metabolized in the liver and kidney. Clearance studies support the possibility that some of the filtered cross-linked peptide is either reabsorbed or metabolized in the renal tubules [24]. The significant decrease in free Dpyr and in sNTX in those receiving calcium citrate suggests that change in metabolism of the cross-linked peptides is not the cause for the differences between the calcium preparations.
Finally, the calcium citrate complex itself might affect bone resorption directly. Calcium citrate complexes and anion bound calcium complexes were not measured in the present study. Calcium citrate can be absorbed as a complex and thus could have direct effects on bone [25]; however, at present there are no studies examining the possible direct effect of citrate or anion bound calcium. On the other hand, the effect of calcium on parathyroid secretion should be entirely dependent on the ionized calcium concentration [26].
This study has important limitations. The number of subjects studied was relatively small and the duration of calcium loading relatively short. Thus, we cannot determine what effect the differences in effects of the two salts on bone turnover might have on changes in bone mineral density and certainly not on fracture risk. Another limitation is that we did not collect 24-h urine sample and therefore could not rule out the possibility that calcium citrate absorption over the course of the study was substantially greater than calcium carbonate absorption. Multiple collections of calcium excretion might have shown an increased absorption over time. We only measured fasting PTH rather than PTH after calcium loading so again may have missed differences between the calcium preparations. Further, we did not conduct the study using a controlled diet and differences in diet may have introduced error. We do not believe that difference in vitamin D affected our results, since the intake of vitamin D in the calcium carbonate group was higher than the calcium citrate group but the decreases in bone turnover markers occurred during calcium citrate treatment.
Whatever the explanation for the difference in effects on markers of bone resorption, it will be important to determine whether this difference is reproducible and sufficient to produce differential effects on bone mass as measured by densitometry or on activation frequency of bone remodeling units as measured by dynamic histomorphometry. Studies thus far have found decreased fracture rates with calcium citrate malate [3,11] and calcium carbonate[27], and an overall decrease in fracture rate of approximately 22% [28]. Several studies have also found decreased bone loss measured by bone mineral density with calcium supplementation compared to placebo [3,10,11,29].Only Dawson-Hughes has compared different preparations and found better BMD preservation with calcium citrate malate than calcium carbonate, especially at the lumbar spine [2]. Further direct comparisons are needed to evaluate calcium preparations for differences, particularly for anti-fracture efficacy.
References
Scopacasa F, Horowitz M, Wishart JM, Need AG, Morris HA, Wittert G, Nordin BE (1998) Calcium supplementation suppresses bone resorption in early postmenopausal women. Calcif Tissue Int 62:8–12
Dawson-Hughes B, Dallal GE, Krall EA, Sadowski L, Sahoyoun N, Tannebaum S (1990) A controlled trial of the effect of calcium supplementation on bone density in postmenopausal women. N Engl J Med 323:878–883
Dawson Hughes B, Harris SS, Krall EA, Dallai GE (1997) Effect of calcium and vitamin D supplementation on bone density in men and women 65 years of age or older. N Engl J Med 1337:670–676
Chapuy MC, Arlot ME, Duboeuf F, Brun J, Crouzet B, Arnaud S, Delmas PD, Meunier PJ (1992) Vitamin D3 and calcium to prevent hip fractures in the elderly women. N Engl J Med 327:1637–1642
Recker RR (1985) Calcium absorption and achlorhydria. N Engl J Med 313:70–33
Prestwood KM, Thompson DL, Kenny AM, Seibel MJ, Pilbeam CC, Raisz LG (1999) Low dose estrogen and calcium have an additive effect on bone resorption in older women. J Clin Endocrinol Metab 84:179–183
Prestwood KM, Pannullo AM, Kenny AM, Pilbeam CC, Raisz LG (1996) The effect of a short course of calcium and vitamin D on bone turnover in older women. Osteoporos Int 6:314–319
Prestwood KM, Kenny AM, Unson C, Kulldorff M (2000) The effect of low dose micronized 17ss-estradiol on bone turnover, sex hormone levels, and side effects in older women: a randomized, double blind, placebo-controlled study. J Clin Endocrinol Metab 85:4462–4469
Reid IR, Ames RW, Evans MC, Gamble GD, Sharpe SJ (1993) Effect of calcium supplementation on bone loss in postmenopausal women. N Engl J Med 328:460–464
Riggs BL, O’Fallon WM, Muhs J, O’Connor MK, Kumar R, Melton LJ 3rd (1998) Long-term effects of calcium supplementation on serum parathyroid hormone level, bone turnover, and bone loss in elderly women. J Bone Miner Res 13:168–174
Peacock M, Liu G, Carey M et al. (2000) Effect of calcium or 25OH vitamin D3 dietary supplementation on bone loss at the hip in men and women over the age of 60. J Clin Endocrinol Metab 85:3011–3019
Martini L, Wood RJ (2002) Relative bioavailability of calcium-rich dietary sources in the elderly. Am J Clin Nutr 76:1345–1350
Bell NH, Bilezikian JP, Bone HG 3rd, Kaur A, Maragoto A, Santora AC and the MK-063 Study Group (2002) Alendronate increases bone mass and reduces bone markers in postmenopausal African-American women. J Clin Endocrinol Metab 87:2792–2797
Delmas PD, Ensrud KE, Adachi JD, Harper KD, Sarkar S, Gennari C, Reginster JY, Pols HA, Recker RR, Harris ST, Wu W, Genant HK, Black DM, Eastell R (2002) Outcomes of raloxifene evaluation investigators. Efficacy of raloxifene on fracture risk reduction in women with osteoporosis: four-year results from a clinical trial. J Clin Endocrinol Metab 87:3609–3617
Johnell O, Scheele WH, Lu Y, Reginster JY, Need AG, Seeman E (2002) Additive effects of raloxifene and alendronate on bone density and biochemical markers of bone remodeling in postmenopausal women with osteoporosis. J Clin Endocrinol Metab 87:985–992
Heaney RP, Dowell SD, Bierman J, Hale CA, Bendich A (2002) Absorbability and cost effectiveness in calcium supplementation. J Am Coll Nutr 20:239–246
Bo-Linn GW, Davis GR, Buddrus DJ, Morawaski SG, Santa Ana C, Fordtran JS (1984) An evaluation of the importance of gastric acid secretion in the absorption of dietary calcium. J Clin Invest 73:640–647
Nicar MJ, Pak CYC (1985) Calcium bioavailability from calcium carbonate and calcium citrate. J Clin Endocrinol Metab 61:391–393
Harvey JA, Zobitz MM, Pak CYC (1988) Dose dependency of calcium absorption: a comparison of calcium carbonate and calcium citrate. J Bone Miner Res 3:253–258
Heller HJ, Greer LG, Sharon BA, Haynes SD, Poindexter JR, Pak CYC (2000) Pharmacokinetic and pharmacodynamic comparison of two calcium supplements in postmenopausal women. J Clin Pharmacol 40:1237–1244
Heller HJ, Greer LG, Haynes SD, Pointdexter JR, Pak CYC (2000) Pharmaacokinetics and pharmacodynamic comparison of two calcium supplements in postmenopausal women. J Clin Pharmacol 40:1237–1244
Heaney, RP, Dowell MS, Barger-Lux MJ (1999) Absorption of calcium as the carbonate and citrate salts, with some observations on method. Osteoporos Int 9:19–23
Hurwitz A, Brady DA, Schaal SE, Samloff IM, Dedon J, Ruhl CE (1997) Gastric acidity in older adults. JAMA 278:659–662
Fall PM, Kennedy D, Smith A, Seibel MJ, Raisz LG (2000) Comparison of serum and urine assays for biochemical markers of bone resorption in postmenopausal women with and without hormone replacement therapy and in men. Osteoporos Int 11:481–485
Favus MJ, Pak C (2001) Evidence for absorption of ionic calcium and soluble calcium complexes by the duodenum and cecum in the rat. Am J Ther 8:425–431
Brown EM (2000) Calcium receptor and regulation of parathyroid hormone secretion. Rev Endocr Metab Disord 1:307–315
Recker RR, Hinders S, Davies KM, Heaney RP, Stegman MR, Lappe JM, Kimmel DB (1996) Correcting calcium nutritional deficiency prevents spine fractures in elderly women. J Bone Miner Res 11:1961–1966
Cumming RG, Nevitt MC (1997) Calcium for prevention of osteoporotic fractures in postmenopausal women. J Bone Miner Res 12:1321–1329
Ruml LA, Sakhaee K, Peterson R, Adams-Huet B, Pak CY (1999) The effect of calcium citrate on bone density in the early and mid-postmenopausal period: a randomized placebo-controlled study. Am J Ther 6:303–311
Acknowledgements
This work has been supported by the General Clinical Research Center (MO1-RR06192), Claude Pepper OAIC (5P60-AG13631) and Mission Pharmacal. Dr. Kenny has been supported by the Paul Beeson Faculty Scholar Program. In addition, we wish to thank Pamela Fall and Christine Abreu for assistance in the biochemical assays.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kenny, A.M., Prestwood, K.M., Biskup, B. et al. Comparison of the effects of calcium loading with calcium citrate or calcium carbonate on bone turnover in postmenopausal women. Osteoporos Int 15, 290–294 (2004). https://doi.org/10.1007/s00198-003-1567-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-003-1567-0