Abstract
Patients who suffer osteoporotic fractures do not typically receive medical/pharmaceutical treatment for osteoporosis. Orthopedic surgeons are concerned about, but not always diligent in following up on, the medical treatment of their fracture patients. The objective of this study was to determine whether orthopedic surgeons could effectively and consistently refer patients with osteoporotic fractures to a primary care provider (PCP) for possible work-up and treatment of osteoporosis. Fourteen orthopedic surgeons participated in the program. Sixty-nine qualifying patients were ≥50 years old, had a low-energy fracture, and had no prior treatment for osteoporosis. For each patient, two letters requesting a PCP appointment were sent to their PCP: one within 10 days of fracture and another 3–10 weeks after fracture. Patients were also instructed that they might have osteoporosis, and were directed to see their PCP. Results showed that of 69 patients (59 females, ten males: average age 69.5±10.9 years), 30 (43.5%) did not see a PCP within 84 days. Thirty-nine (56.5%) patients saw a PCP within 84 days, but osteoporosis was not addressed in four (average days to PCP, 39.8±18.6: range 7–78 days). Of patients seen within 84 days, anti-resorptive medications (e.g. bisphosphonate) were started in 21/39 (53.8%), but typically not within 41 days of fracture. Of the 14 orthopedic surgeons, five were non-compliant and seven were inconsistent in their participation, forgetting to send the letters and/or inform patients to make PCP appointments. Standing discharge orders (for medications, PCP follow-up, bone-density scanning, etc.) may be more effective in achieving timely medical treatment for patients of orthopedic surgeons with osteoporotic fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with osteoporotic fractures typically do not receive subsequent medical treatment for this disease [1, 2, 3, 4, 5, 6, 7]. Following an osteoporotic fracture, the timely initiation of pharmacological treatment with an anti-resorptive agent (e.g. some bisphosphonates) can significantly increase bone mineral density (BMD) within months of fracture, which reduces the risk of subsequent fracture [8, 9, 10]. These commonly used agents have also been shown to have minimal or no adverse affects on fracture healing [11]. In turn, orthopedic surgeons are becoming increasingly aware of the necessity of the timely initiation of medical treatment for osteoporosis, especially for their middle-aged or older patients with low-energy fractures [7, 12, 13, 14, 15]. However, a recent survey of 107 orthopedic surgeons showed that most are hesitant to increase the scope of their responsibilities to include anti-resorptive pharmacological agents for patients with osteoporosis [16]. This survey also showed that surgeons would prefer to refer their patients with osteoporotic fractures to a primary care physician or other primary care provider (PCP) for the continuation of medical treatment and further work-up. Yet, the diligence of orthopedic surgeons in making referrals, and their effectiveness in making certain that their patients do indeed see a PCP is uncertain. It is also unclear whether the efforts of orthopedic surgeons in making referrals to PCPs achieve the desired goal of ensuring timely and proper medical care for their patients.
The purpose of this study was to determine: 1) the consistency that patients who are ≥50 years old and have a low-energy fracture followed through in seeing PCPs after being specifically referred by their orthopedic surgeons for the treatment of presumed osteoporosis, and 2) whether efforts made by orthopedic surgeons to refer their patients are worthwhile; in other words, do the PCPs see these patients in a timely manner, and do the PCPs initiate medical treatment for osteoporosis.
Materials and methods
Criteria for selecting surgeons
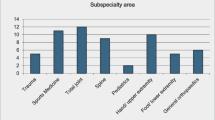
Twenty-three orthopedic surgeons in northern and central Utah, who were within 15 years of the last year of their orthopedic surgery residencies, were approached to participate in this study. Of these 23 surgeons, none routinely participated in facilitating the medical treatment of their patients with low energy fractures. Fourteen surgeons agreed to take part in the study. Twelve of these surgeons had been in private practice for 1–5 years, and the other two surgeons for 10–15 years. All surgeons were male and all participated on orthopedic trauma call schedules in non-university-affiliated community hospitals, each serving potential patient populations over 75,000. One surgeon participated on a trauma call schedule at a non-university-affiliated, level-one trauma center. All surgeons also performed elective surgeries in these community hospitals and/or local outpatient (i.e. ambulatory) surgical centers. None of the hospitals had intervention protocols for the medical treatment of patients with osteoporotic fractures.
The orthopedic surgeons expressly agreed to participate in this study and were offered remuneration for each patient completing the study. Surgeons were interviewed in order to determine how, or if, they usually intervened in facilitating and/or initiating the medical treatment of their hospitalized and non-hospitalized patients with apparent osteoporotic fractures. This was done in order to insure that the follow-up program that they were asked to adhere to (described below) was at least at the standard of care. It was clear that the program was above the standard of care for this group of 14 surgeons.
Enrollment of fracture patients
Patients who qualified for enrollment were men and women ≥50 years old who had osteoporotic- or insufficiency-related fractures, and who had no prior consistent or specific treatment for osteoporosis with approved medications (estrogen, bisphosphonates, calcitonin, raloxifene). These fractures were defined as fractures that occur with minimal (low-energy) trauma (such as a fall from a standing height or from a height less than three feet). Excluded fractures were those that occurred from higher energy motor vehicle accidents and sports-related injuries, or were associated with tumors. Additional enrollment criteria included patients who: 1) were community ambulators without support devices (e.g. cane, crutch, wheelchair), 2) were not residents of nursing homes or other extended-care facilities, and 3) did not have cognitive impairments requiring supervision. These additional criteria insured that the patients potentially had significant control over their medical care, including obtaining transportation to a PCP clinic.
PCP referral program and data collection
Two letters requesting a PCP appointment were sent: the first letter within 10 days of fracture, and the second letter 3–10 weeks after fracture (Fig. 1). This timeline was adjusted for hospitalized patients such that the day of their discharge from the healthcare facility (i.e. a hospital or extended care facility) counted as day zero. At the initial evaluation (e.g. during the patient’s hospitalization, emergency room visit, or initial clinic visit for fracture care), and at each fracture follow-up clinic visit, the surgeon told the patient: 1) that they might have osteoporosis and were at significantly increased risk for a subsequent fracture within the next 2 years, and 2) to make a PCP appointment for probable treatment to increase bone strength, and possible further medical work-up for osteoporosis. If the patient did not have a PCP, then one was recommended from their local community. In this instance, a different PCP letter was sent (see below). All letters were delivered by standard mail through the US Postal Service. The study coordinators prepared the PCP letters on each surgeon’s letterhead (Fig. 2).
Additional measures taken to enhance surgeon compliance
Study charts were provided, and included: 1) a sheet for chronologic documentation of each patient’s surgical and medical clinic follow-up visits, and 2) a risk assessment questionnaire for osteoporosis and osteoporotic fracture.
To enhance consistency and compliance, the principal investigator and the research staff also provided the surgeons and their staff with tutorials about how to enroll and track these patients. Additionally, each clinic received a printed chart showing the timeline of the program to be posted on a wall of the clinic. Once every 2–4 weeks, a member of the research team contacted the surgeon or surgeon’s staff by telephone or in person. The purpose of this contact was to encourage compliance with the fracture follow-up program. Additional financial incentive for each patient completing the study was offered to the surgeon’s medical assistant who was most involved in reminding the patients to make their PCP appointments.
Each surgeon was asked to track 10–15 consecutive fracture patients who met the enrollment criteria. The study began in April 2000 and continued through November 2002.
Outcome measures and statistical analysis
The primary outcome measure was the time to the PCP appointment. The secondary outcome measures included determining: 1) the diagnostic work-up for osteoporosis, if any, that was done, and 2) the time to definitive anti-resorptive treatment for osteoporosis with approved medications (estrogen, bisphosphonates, calcitonin, raloxifene). Comparisons between hospitalized and non-hospitalized groups were evaluated using two-sample t-tests (days to see PCP) or logistic regression analyses (all other comparisons).
Results
Prior to starting this study, none of the surgeons routinely initiated medical treatment for presumed osteoporosis for their 50 years-and-older patients with low-energy fractures. A few of the surgeons would tell some of their fracture patients to see their PCP for the medical treatment of osteoporosis. However, none of these surgeons admitted to being consistent in this regard.
Fracture types and frequencies are shown in Table 1. Of 69 patients (59 females, ten males: average age 69.5±10.9, range 50–90 years), 30 (43.5%) were not seen by a PCP within 84 days (Table 2). Thirty-nine patients (56.5%) saw a PCP within 84 days, but osteoporosis was not addressed in four patients (average days to PCP, 39.8±18.6: range 7–78 days) (Table 3). Of patients seen within 84 days, pharmacologic treatment with an anti-resorptive agent (e.g. bisphosphonate, estrogen) was started in 21/39 (53.8%), but typically not within 41 days of fracture. A calcium supplement, with or without an anti-resorptive agent, was prescribed to 20/39 (51.3%) patients, but this was typically not within 37 days of fracture.
Of the 39 patients who saw PCP within 84 days, 25 (64.1%) were hospitalized following fracture, although none was hospitalized longer than 7 days. A bone-density scan was ordered for 36% (9/25) of hospitalized patients compared to 57.1% (8/14) of non-hospitalized patients, and no patient had a bone-density scan while in the hospital. Slightly more than 50% of both non-hospitalized and hospitalized patients were eventually prescribed oral anti-resorptive treatments and/or calcium or vitamin D supplements. However, none of these medications was started in the hospital. It took hospitalized patients approximately 7 days longer to see their PCP than non-hospitalized patients. These results are summarized in Table 2.
The surgeons were asked to send the first letter within 10 days of fracture, although on average, they sent the first letter 11.0±7.7 days after fracture. There were 27 instances when the letter was sent >10 days after fracture (range: 11–33 days). Second letters were sent for 36 (52.2%) patients, all of which were sent within the prescribed time frame (3–10 weeks). Seven patients did not have a PCP, and of these, three elected not to see a PCP.
Of the 14 participating orthopedic surgeons, five were non-compliant and an additional seven were inconsistent in their participation, forgetting to send the PCP referral letters and to inform their patients to make a PCP appointment. Additionally, nearly all medical assistants (MAs) were inconsistent in carrying out their prescribed role in reminding patients to follow-up with their PCPs. Reasons given for this inconsistency included: 1) the surgeon would forget to inform them that the patient was enrolled in the study, 2) they (the MAs) would forget to remind the patient, and 3) they (the MAs) would lose interest as the surgeon lost interest in participating in the study. It was clear that poor compliance and/or inconsistency among the clinic staff was directly, and primarily, associated with the surgeon’s poor compliance and/or inconsistency in following the program.
Discussion
Of the patients seen through the completion of the program, 56.5% (39/69) saw their PCP within 84 days of fracture. This follow-up rate is substantially better than that reported by a study that has examined the efficiency of letter-sending protocols for outpatient medical follow-up for patients with osteoporotic fractures [17]. However, few of the 14 surgeons complied with the program evaluated in this study. These results contrast with data suggesting orthopedic surgeons generally feel that it is important to ensure timely medical treatment for their patients with osteoporotic fractures [16]. This contradiction, in part, stems from the opinion of orthopedic surgeons that medical follow-up and treatment is not inextricably linked to the surgical care of patients with osteoporotic fractures [16]. Additionally, orthopedic surgeons are reluctant to prescribe many forms of conventional pharmacological treatments because of their concerns about adverse events. Thus, in general, orthopedic surgeons appear to be at an impasse—they recognize the need for the initiation of medical treatment, yet they clearly seem concerned about the implications of the added responsibilities demanded by medical care. These possibilities, in addition to their concern about additional liability and potentially time-consuming responsibilities associated with medical treatment of such patients, seem to deter these surgeons from more aggressively seeking medical care for these patients.
The fact that the orthopedic surgeons who participated in this study were not compelled to initiate medical treatment for patients with osteoporotic fractures is not inconsistent with their training. In the United States, there is currently no mandate that orthopedic surgeons have training for the medical treatment of patients with senescent or metabolic bone diseases such as osteoporosis. However, the American Academy of Orthopedic Surgeons (AAOS) is taking an active role in increasing the awareness of orthopedic surgeons about steps that can be taken of enhancing the care of patients with fragility fractures. Examples of this emphasis can be found on the AAOS Internet web page (http://www.aaos.org/wordhtml/papers/position/1159.htm; http://www.aaos.org/wordhtml/papers/position/1113.htm).
Of the patients who saw a PCP within 84 days of fracture, nearly 50% were not prescribed an anti-resorptive agent. Reasons for this apparent under-treatment were not evaluated. Recent studies have shown that inadequate medical treatment for patients with osteoporotic fractures is common [5]. Strides are being taken to increase the relatively low rate that PCPs currently prescribe anti-resorptive agents for patients with low-energy fractures [7]. These efforts include the education of health-care providers as to the importance of initiating treatment and possible work-up for probable osteopenia or osteoporosis in patients with low-energy fractures. Additionally, there is an increasing prevalence of continuing medical education courses regarding the beneficial effects of exercise, calcium and vitamin D supplementation, as well as the risks and benefits of using anti-resorptive agents for these conditions.
It is suggested that a standardized treatment/intervention program may be useful in helping orthopedic surgeons and PCPs facilitate effective medical treatment for the secondary prevention of osteoporotic fractures. For example, at any given healthcare facility, standard discharge orders could be given to patients who have a low-energy fracture and/or are noted to have other significant risk factors for osteoporosis. These orders would include: 1) a timely (<4 week for fracture patients) follow-up appointment with a PCP, 2) the initiation of a workup of the patient’s metabolic bone status, if deemed necessary at the time of fracture care, 3) an appointment for a DXA scan, and 4) educational materials about preventing and treating osteoporosis and osteoporotic fractures. The patient signs the discharge orders, indicating that they received a copy of them, that they understand the potential implications of non-compliance (i.e. subsequent fracture), and that they bear some responsibility for treatment. The PCP’s clinic is informed that the patient has been asked to make an appointment. If the patient fails to make an appointment, a follow-up telephone call to remind the patient could be made by the PCP’s staff.
Programs with some of these features are currently being used by some health-care organizations, and are considered highly effective (personal communications: Drs. Mark Clapper and Steven Schelkun, San Diego Kaiser Permanente; Dr. Lynn Kohlmeier: Sacred Heart Hospital, Spokane, Wash., USA; Dr. Christine Simonelli, HealthEast Clinics, Woodbury, Minn., USA). Unfortunately, few studies examining the effectiveness of these specific programs have been published [18]. Other examples of medical intervention programs exist. For example, some hospitals have protocols where patients with some low-energy fractures (e.g. hip fractures) automatically have internal medicine or endocrinology consultations, out-patient referrals to a PCP, and/or are seen by an orthopedic specialist nurse for work-up and treatment (e.g. personal communications: Dr. Joel S. Finkelstein, Massachusetts General Hospital, Boston, Mass., USA; Dr. Lorraine Fitzpatrick, Mayo Clinic, Rochester, Minn., USA; Dr. Nancy Lane, University of California San Francisco Medical Center, San Francisco, Calif., USA). There are data suggesting that many of these protocols can be effective [17, 19]. In the author’s experience the most effective method appears to be to call the PCP’s office at the time the patient is in the orthopedic surgeon’s clinic and to make the PCP appointment at that time. However, additional study is needed to firmly establish that the observed difference in a PCP follow-up program based on a phone call versus a program based on a letter of correspondence is significant.
An analogous medical intervention program for the secondary prevention of symptomatic coronary artery disease has been proven highly effective. The Cardiac Hospital Atherosclerosis Management Program (CHAMP) instituted in Los Angeles, California, USA mandated the initiation of several pharmacologic treatments (already proven effective in reducing the mortality of patients following acute myocardial infarction) before patients with established coronary artery disease were discharged from the hospital [20]. CHAMP resulted in a significant increase in the initiation and continuation of established therapies and a subsequent reduction in recurrent myocardial infarctions. This strategy could easily be applied to the problem of osteoporosis as it relates to recurrent fractures. Intervention protocols that include standing discharge orders for patients with osteoporotic fractures, implementing bisphosphonates, calcium, and other treatments, may be similarly effective in reducing the incidence of recurrent fractures.
In conclusion, when the letter-sending program was complied with, it was reasonably effective in facilitating medical follow-up for patients with low-energy fractures. However, the participating private-practice, community-based orthopedic surgeons were highly inconsistent or non-compliant with this program. Additionally, the PCPs often did not prescribe anti-resorptive agents for these patients. In view of these results, and of a recent survey showing the reluctance of orthopedic surgeons in initiating treatment of osteoporosis, several recommendations can be made. It is suggested that a more effective medical treatment/intervention program may be one where the patient receives standing discharge orders (for medical treatment, work-up, and PCP follow-up) from the health-care facility where they are initially evaluated. It is probable that the further education of orthopedic surgeons, primary care physicians, and other healthcare providers concerning the adverse effects and contraindications of anti-resorptive agents would alleviate some of the concerns and, potentially, enhance the role of surgeons in the medical treatment of osteoporosis. Continuing medical education courses for both PCPs and orthopedic surgeons are also needed to enhance their understanding of the importance of recognizing and treating osteopenia/osteoporosis in patients with low-energy fractures.
References
Torgerson DJ, Dolan P (1998) Prescribing by general practitioners after an osteoporotic fracture. Ann Rheum Dis 57:378–379
Freedman KB (1999) Osteoporosis prevention and the orthopaedic surgeon: when fracture care is not enough (editorial response). J Bone Joint Surg 81:1652–1653
Pal G (1999) Questionnaire survey of advice given to patients with fractures. BMJ 318:500–501
Broy SB, Bohren A, Harrington T, Licata A, Shewman D (2000) Are physicians treating osteoporosis after hip fracture? J Bone Miner Res 15:S141
Freedman KB, Kaplan FS, Bilker WB, Strom BL, Lowe RA (2000) Treatment of osteoporosis: are physicians missing an opportunity? J Bone Joint Surg [Am] 82:1063–1070
Cuddihy MT, Gabriel SE, Crowson CS et al. (2002) Osteoporosis intervention following distal forearm fractures: a missed opportunity? Arch Int Med 162:421–426
Gardner MJ, Flik KR, Mooar P, Lane JM (2002) Improvement in the undertreatment of osteoporosis following hip fracture. J Bone Joint Surg [Am] 84-A:1342–1348
McClung MR, Geusens P, Miller PD et al. (2001) Effect of risedronate on the risk of hip fracture in elderly women. N Engl J Med 344:333–340
Lindsay R, Silverman SL, Cooper C et al. (2001) Risk of new vertebral fracture in the year following a fracture. JAMA 285:320–323
Liberman UA, Weiss SR, Broll J et al. (1995) Effect of oral alendronate on bone mineral density and the incidence of fractures in postmenopausal osteoporosis. N Engl J Med 333:1437–1443
Fleisch H (2001) Can bisphosphonates be given to patients with fractures? (editorial). J Bone Miner Res 16:437–440
Smith R (1991) Osteoporosis at the Tivoli. J Bone Joint Surg [Br] 73-B:525–526
Tosi LL, Lane JM (1998) Osteoporosis prevention and the orthopaedic surgeon: when fracture care is not enough (editorial). J Bone Joint Surg [Am] 80-A:1567–1569
Pal B, Morris J, Muddu B (1998) The management of osteoporosis-related fractures: a survey of orthopaedic surgeons’ practice. Clin Exp Rheum 16:61–62
Lane JM, Nydick M (1999) Osteoporosis: current modes of prevention and treatment. J Am Acad Orthop Surg 7:19–31
Skedros JG, Milleson NM, Holyoak JD (2003) Knowledge and opinions of orthopaedic surgeons concerning initiation of treatment for patients with osteoporotic fractures. Trans Orthop Res Soc 28:1058
Edwards BJ, Bunta A, Madison L, Ramsey-Goldman R, Taft L (2000) A fracture intervention program: First year results. J Bone Miner Res 15:S537
Ridout R, Hawker GA, Mahomed N, Bogoch ER (2000) An intervention to increase investigation and treatment of osteoporosis in fragility fracture patients. J Bone Miner Res 15:S294
McLellan AR, Fraser M (2002) A 28 month audit of the efficacy of the fracture liaison service in offering secondary prevention for patients with osteoporotic fractures. J Bone Miner Res 17:S358
Fonarow GC, Gawlinski A, Moughrabi S, Tillisch JH (2001) Improved treatment of coronary heart disease by implementation of a cardiac hospitalization atherosclerosis management program (CHAMP). Am J Cardiol 87:819–822
Acknowledgements
This study was completed with the assistance of orthopedic surgeons in northern and central Utah. The author thanks Dr. Dustin Hunsaker, Joshua Holyoak, Niki Milleson, Geri Henderson and Cyndi Slot for their help in completing this project, and are grateful for the critical reviews of Dr. Philip A. Kithas, Dr. Mark W. Mason, Dr. Kenneth J. Hunt, and Dr. Tony Y. Kuo. This study was supported by a grant from Merck and Co., Inc. and by the Utah Osteoporosis Center, Salt Lake City, Utah.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Skedros, J.G. The orthopaedic surgeon’s role in diagnosing and treating patients with osteoporotic fractures: standing discharge orders may be the solution for timely medical care. Osteoporos Int 15, 405–410 (2004). https://doi.org/10.1007/s00198-003-1561-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-003-1561-6