Abstract
Rheumatoid arthritis (RA) is a major cause of secondary osteoporosis and is frequently associated with both paraarticular and generalized osteoporosis. The present study was designed to investigate the preferential sites of reduction of bone mineral density (BMD), in the early stage of RA, with special emphasis on the differential effect of RA on BMD in trabecular and cortical components. The participants (30 RA patients and 26 healthy participants) were all female with disease duration of less than 1 year. BMD in the radius was measured at 4% (ultradistal site) and 20% (midshaft) to the ulnar length proximal to the end of radius by peripheral quantitative computed tomography. BMD in lumbar spine was measured by dual X-ray absorptiometry and the osteo-sono assessment index (OSI) of the calcaneus by ultrasound. RA patients showed lower BMD preferentially in the trabecular component, but not in cortical bone component of the ultradistal radius than age-matched normal controls. Calcaneus OSI was also significantly reduced. The radial midshaft and lumbar spine did not differ significantly between RA patients and normal controls. Trabecular BMD in the ultradistal radius exhibited negative correlations with serum CRP, ESR, and RF, and calcaneus OSI with M-HAQ score. In conclusion, it was suggested that disease activity of RA and impairment of daily physical activity might be a significant determinant of deterioration of bone structure in paraartciular distal radius and calcaneus, respectively, in early-stage RA patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is frequently associated with paraartciular and generalized osteoporosis, although the exact mechanism is as yet unknown [1, 2]. We have reported that several mechanisms are involved in the development of osteoporosis in RA patients [3, 4, 5]. One of the major mechanisms of paraarticular osteoporosis involves increased release into affected joints of inflammatory cytokines with bone-resorptive activity, such as interleukin 1 (IL-1), interleukin 6 (IL-6), and tumor necrosis factor (TNF) [4, 5, 6, 7, 8]. Malnutrition [9], impairment of physical activity [10], and drugs for RA such as steroids [11] and methotrexate [12] may play an important role in the development of generalized osteoporosis.
Since several mechanisms contribute to the development of osteoporosis in RA and the importance of each mechanism in the development of osteoporosis at each site may differ, it is possible that reduction of bone mass in RA patients may develop at different sites with different kinetics. Previous study reported that loss of trabecular bone in the distal radius was more rapid than those of the radial midshaft or lumbar spine in earlier stages of RA, although its mechanism and the data on changes in cortical bone component were not known exactly [13]. The clinical application of peripheral quantitative computed tomography (pQCT) made it possible to measure volumetric bone densities of total, trabecular, and cortical bone components separately in the radius [14]. We measured bone mineral density (BMD) in the radius at 4% (ultradistal site) and 20% (midshaft) to the ulnar length proximal to the end of radius by pQCT, as indexes of paraarticular and generalized osteoporosis [13, 14]. Furthermore, lumbar spine (L2-L4) BMD and calcaneus osteo-sono-assessment index (OSI) were measured as indexes of generalized osteoporosis.
This background prompted us to determine the preferential site of reduced BMD in early RA patients among ultradistal and midshaft of radius, lumbar spine, and calcaneus, and its mechanism, particularly focusing on the different effect of RA on the trabecular and cortical components.
Patients and methods
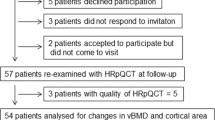
Participants
The participants were all female and consisted of 30 RA patients and 26 healthy controls, from whom written informed consent was obtained. The study was approved by Ethics Committee of Osaka City University Hospital. The RA patients were recruited consecutively from the patients of the Outpatient Clinic of Rheumatology at Osaka City University Hospital and were diagnosed according to the 1987 revised American Rheumatism Association criteria [15]. As controls, we selected 26 healthy participants from people who participated in a local health check program at the Osaka City University Hospital. The mean ages of the RA patients and healthy controls were 52.1±11.9 years and 54.4±11.3 years, respectively. The duration of RA was less than 1 year.
To avoid confounding by other known risk factors of osteoporosis, we selected participants using the following exclusion criteria: (1) smoking, (2) renal disease possibly causing secondary hyperparathyroidism, (3) endocrine disorders, (4) liver disease, (5) malnutrition (serum albumin <3.0 g/dl), (6) the administration of any medication including steroid and methotrexate that might affect bone and mineral metabolism, and (7) severely disabled patients unable to walk unassisted.
Serum samples were collected from the 30 RA patients and relevant laboratory variables measured (blood sedimentation rate, blood concentration of hemoglobin [Hb], platelets, serum concentrations of C-reactive protein [CRP], rheumatoid factor [RF], immunoglobulin G [IgG], IgA and IgM, and albumin). All of the 30 RA patients were receiving multiple medication, with 21 patients taking nonsteroidal anti-inflammatory drugs (NSAIDs), 9 gold, 11 salazosulfapyridine, and 15 bucillamine.
Assessment of activity of daily life (ADL) score
Physical function and health-related quality of life were assessed using a self-administered questionnaire modified from the Stanford Health Assessment Questionnaire, named the modified Health Assessment Questionnaire (M-HAQ) [16]. M-HAQ score is relevant to assess ADL in Japanese RA patients [17, 18].
Peripheral quantitative computed tomography (pQCT)
pQCT measurements were performed at 4% (ultradistal site) and 20% (midshaft site) to the ulnar length proximal to the end of radius with a single 2.5-mm thick CT slice on the nondominant side using an XCT-960 scanner (Stratec Inc, Pforzheim, Germany), as described previously [19, 20, 21]. Briefly, the bone mineral content (g/mm), the cross-sectional bone area, and the bone mineral density (g/cm3) were determined at the ultradistal site for the entire cross section as well as for the trabecular compartment. After the determination of the entire bone contour, the outer 55% of voxels were concentrically peeled off. The remaining 45% of voxels were defined as the trabecular region [19, 20]. The peeled-off area was defined as the cortical plus subcortical area [19, 20]. At the midshaft site, BMD was measured only for the entire cross section as the cortical component because of the paucity of trabecular bone at this site [19, 21]. The former measurement site was chosen to analyze the effect of RA on the trabecular volumetric component of paraarticular bone separately from the cortical component [13, 20], and the latter to measure the effect of RA on the cortical volumetric component of generalized bone [21]. Image processing and calculation of numerical values were performed using the manufacturer's software package. The precision of the pQCT procedure ranged from 1% to 2%, depending upon the parameter assessed [22].
BMD measurement at lumbar spine
BMD was measured in the lumbar spine (L2-L4) by dual-energy X-ray absorptiometry (DXA; QDR-4500A, Hologic, Waltham, MA), essentially as previously described [23]. The precision of the measurement of lumbar spine BMD using DXA was less than 1.8%.
Quantitative ultrasound assessment of calcaneus
Quantitative ultrasound assessment of calcaneus was performed using an ultrasound system (Acoustic Osteo-Screener, AOS-100; Aloka, Tokyo, Japan), as previously described [24]. Briefly, the AOS-100 measures both speed of sound (SOS) and an attenuation-related parameter called the transmission index (TI). These measurements yield a derived parameter, the osteo sono-assessment index (OSI), which has been proposed to be an estimate of the elastic modulus of the calcaneus. Precision of the OSI parameter was 2.2% [25].
Statistical analysis
Values are expressed as mean ± SD unless otherwise indicated. Statistical analysis was performed with the Stat View V system (Abacus Concepts, Berkeley CA) for the Apple computer. Comparison of mean values between the two groups was performed by Student's t-test. The correlation coefficients were calculated by simple regression analysis. P values of less than 0.05 were considered significant.
Results
Clinical profiles of RA patients and healthy controls
The RA patients and healthy controls chosen were all female to exclude the effect of gender on bone mass. There were no significant between-group differences in the proportion of premenopausal and postmenopausal women, or in age, height, body weight, or body mass index (Table 1).
BMD at various sites in RA patients and controls
Table 2 shows that BMD measured by pQCT in trabecular bone at the ultradistal radius was significantly lower in RA patients than in normal controls (p<0.0001). Interestingly, however, total bone BMD at the ultradistal radius in RA patients did not differ significantly from that in controls (p>0.10). Cortical and plus subcortical bone BMD at ultradistal radius did not differ significantly between RA patients and normal controls (p>0.10). BMD at midshaft radius did not differ significantly between RA patients and normal controls. Nor did BMD at the lumbar spine measured by DXA differ significantly, although calcaneus OSI measured ultrasonographically was significantly lower in RA patients (p<0.05).
Correlation of RA activity with trabecular BMD in the ultradistal radius and with calcaneus OSI in RA patients
We next determined the significance of the effect of RA on trabecular bone component in the radius and calcaneus. Table 3 shows the summary of simple correlations of trabecular BMD in ultradistal radius and calcaneus OSI with various variables indicating RA disease activity. Of the clinical variables, blood sedimentation rate and rheumatoid factor showed a significant and negative correlation, and C-reactive protein a tendency to negative correlation with trabecular BMD in the ultradistal radius. In contrast, none of RA disease marker correlated significantly with calcaneus OSI.
Correlation between calcaneus OSI Z-score and M-HAQ score
We next examined the effect of daily physical activity on calcaneus OSI, and on BMDs in radius and lumbar spine. A negative correlation, although not significant probably due to the small number of RA patients, was found between the two parameters (r=−0.313, p=0.087) (Fig. 1). However, M-HAQ score did not correlate either with BMDs in trabecular bone at the ultradistal radius (r=−0.194, p=0.323), in midshaft radius (r=−0.222, p=0.237), or lumbar spine (r=−0.281, p=0.125).
Discussion
The present study demonstrated that early-stage RA patients showed significant reductions in the trabecular BMD of the paraarticular ultradistal radius and in the trabecular bone-rich calcaneus OSI compared with healthy controls. However, the mechanisms of lower bone mass in these sites may differ. Negative correlations of trabecular BMD in the paraarticular ultradistal radius with CRP, BSG, and RF in RA patients suggests that local inflammation in the affected joints may be an important factor for BMD reduction in paraarticular trabecular bone. In contrast, a negative correlation of calcaneus OSI with M-HAQ score, but not with any inflammation marker, suggests the impairment of physical activity as a major factor for reduction of calcaneus OSI.
pQCT is able to measure the BMD of the trabecular component of the distal radius separately from the cortical component [19, 20, 21]. However, the measured cortical bone component does not exactly comprise cortical bone because of the inclusion of subcortical bone, the endosteal portion of the cortex, and also trabecular bone component, since the Stratec pQCT system defines outer 55% of voxels as cortical bone area [19, 26]. Since the present study showed that trabecular BMD, but not total or cortical plus subcortical BMD, in the ultradistal radius was reduced in early RA patients (Table 2), it was concluded that the BMD of the trabecular component of the ultradistal radius was preferentially reduced in early RA patients compared with age- and gender-matched controls, in contrast to the maintenance of BMD observed in the cortical component. A previous report demonstrated that loss of trabecular bone component in the ultradistal radius was more rapid in RA than those of the radial midshaft or lumbar spine, although they did not measure the rate of cortical bone loss in the ultradistal radius [13]. Furthermore, we elucidated the importance of RA-induced inflammation on the loss of paraarticular trabecular bone as evidenced by a negative correlation between inflammation marker and trabecular BMD in the ultradistal radius.
Previous reports of ours have indicated that humoral factors with bone resorptive activity, such as IL-1, IL-6, TNF [5], and hepatocyte growth factor [3], and extrarenal activation of vitamin D [4], may contribute to BMD reduction in paraarticular trabecular bone. Since these are humoral factors that activate bone resorption, it is reasonable to suppose that metabolically active trabecular bone is more susceptible than cortical bone to the enhancement of bone resorption by humoral bone resorptive factors. Previous reports have shown that DXA-determined total BMD in the forearm, which consists of 85% cortical bone and 15% trabecular bone, is significantly reduced in RA patients compared with control participants and that number of years since menopause, M-HAQ score for the upper extremities, and BSG appear to be significant determinants of forearm BMD [26]. Since DXA cannot discriminate trabecular BMD from cortical BMD and since the RA patients analyzed were at a more advanced stage, the conclusion drawn from the previous study may contrast with that of the present study. Furthermore, a longitudinal study has shown that RA patients lose bone mass in spine, femoral neck, and Ward's triangle more rapidly than healthy controls, resulting in generalized bone loss at a more advanced stages of RA [27]. Recent reports have shown that the risk factors for generalized osteoporosis in RA patients increase with longer duration and greater severity of the disease [20], suggesting that the sites of osteoporosis may differ between RA patients in an early stage and those in more advanced stages.
Although the measurement of calcaneus ultrasound includes not only bone density but also bone elasticity and architecture, parameters of quantitative ultrasound assessment of the calcaneus are mostly related to BMD [28, 29]. In fact, daily physical activity has a beneficial effect on bone mass in weight-bearing bone such as the lumbar spine and calcaneus [30]. The validity of quantitative ultrasound measurement of calcaneus was demonstrated in advanced stage RA patients with disease duration of more than 10 years, as evidenced d by a significant reduction of ultrasound measures in RA patients and a significant association of radiological modified Larsen score with ultrasound measures [31]. We have shown that the calcaneus OSI was significantly reduced probably due to reduced physical activity in RA patients, as reflected by a negative correlation between two parameters (Fig. 1). However, although bone mass in lumbar spine is also heavily influenced by physical activity [32], a significant reduction was not observed (Table 2). Aerobics and weight training increase both the calcaneus OSI and the lumbar spine BMD significantly, but to a lesser extent at the latter site [30, 32]. Since the calcaneus is thus more susceptible than the lumbar spine to physical activity and since the RA patients analyzed in the present study were restricted to those with disease duration of less than 1 year, it is possible that calcaneus OSI, but not lumbar spine BMD, decreased significantly.
To precisely know the effect of RA on bone mass in early RA patients, patients who are now, or have a history of, taking drugs that might affect bone metabolism, such as steroid and methotrexate, were excluded, although the latter drug might not have any adverse effect on bone metabolism [33, 34].
In summary, it was demonstrated that RA patients in the early stage of the disease showed significant reductions in the trabecular BMD of the ultradistal radius and OSI of the calcaneus. BMD at the former site exhibited significant and positive correlations with biochemical indicators for RA disease activity, and the calcaneus OSI negative correlation with daily physical activity score. The findings therefore suggest that joint inflammation is a significant determinant of paraarticular osteoporosis, and impairment of daily activity of calcaneus osteoporosis in early stage RA patients.
References
Inaba M. Ishimura E (2002) Secondary osteoporosis. In: Morii H, Nishizawa Y, Massry SG (eds) Calcium in internal medicine. Springer, Berlin Heidelberg New York, pp 347–360
Deodhar AA, Woolf AD (1996) Bone mass measurement and bone metabolism in rheumatoid arthritis: a review. Br J Rheumatol 35:309–322
Yukioka K, Inaba M, Furumitsu Y et al (1994) Levels of hepatocyte growth factor in synovial fluid and serum of patients with rheumatoid arthritis and release of hepatocyte growth factor by rheumatoid synovial fluid cells. J Rheumatol 21:2184–2189
Inaba M, Yukioka K, Furumitsu Y et al (1997) Positive correlation between levels of IL-1 or IL-2 and 1,25(OH)2D/25-OH-D ratio in synovial fluid of patients with rheumatoid arthritis. Life Sciences 61:977–985
Furumitsu Y, Inaba M, Yukioka K et al (2000) Levels of serum and synovial fluid pyridinium crosslinks in patients with rheumatoid arthritis. J Rheumatol 27:64–70
Manolagas SC (1995) Role of cytokines in bone resorption. Bone 17 [Suppl]:63s–67s
Miyasaka N, Sato K, Goto M et al (1988) Augmented interleukin-1 production and HLA-DR expression in the synovium of rheumatoid arthritis patients. Arthritis Rheum 31:480–486
Gowen M, Wood DD, Ihrie EJ et al (1983) An interleukin 1 like factor stimulates bone resorption in vitro. Nature 306:378–380
Inaba M, Morii H, Katsumata T et al (2000) Hyperparathyroidism is augmented by ovariectomy in Nagase analbuminemic rats. J Nutr 130:1543–1547
Neville CE, Murray LJ, Boreham CA et al (2002) Relationship between physical activity and bone mineral status in young adults: the Northern Ireland young hearts project. Bone 30:792–798
Canalis E, Delany AM (2002) Mechanisms of glucocorticoid action in bone. Ann N Y Acad Sci 966:73–81
Minaur NJ, Kounali D, Vedi S et al (2002) Methotrexate in the treatment of rheumatoid arthritis. II. In vivo effects on bone mineral density. Rheumatology 41:741–749
Sambrook PN, Ansell BM, Foster S, Gumpel JM, Hesp R, Reeve J (1985) Bone turnover in early rheumatoid arthritis. 2. Longitudinal bone densities. Ann Rheum Dis 44:58–584
Boonen S, Cheng XG, Nijs J et al (1997) Factors associated with cortical and trabecular bone loss as quantified by peripheral computed tomography (pQCT) at the ultradistal radius in aging women. Calcif Tissue Int 60:164–170
Arnett FC, Edworthy SM, Bloch DA et al (1988) The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 31:315–324
Pincus T, Summey JA, Soraci SA Jr et al (1983) Assessment of patient satisfaction in activities of daily living using a modified Stanford Health Assessment Questionnaire. Arthritis Rheum 26:1346–1353
Maeda T, Yamada T, Nagamine R et al (2002) Involvement of CD4+, CD57+ T cells in the disease activity of rheumatoid arthritis. Arthritis Rheum 46:379–384
Nakamura H, Ueki Y, Sakito S et al (2000) Clinical effects of actarit in rheumatoid arthritis: improvement of early disease activity mediated by reduction of serum concentrations of nitric oxide. Clin Exp Rheumatol 18:445–450
Gorai I, Nonaka K, Kishimoto H et al (2001) Cut-off values determined for vertebral fracture by peripheral quantitative computed tomography in Japanese women. Osteoporos Int 12:741–748
Shibuya K, Hagino H, Morio Y et al (2002) Cross-sectional and longitudinal study of osteoporosis in patients with rheumatoid arthritis. Clin Rheumatol 21:150–158
Lochmuller, E-ML, Lill CA, Kuhn V et al (2002) Radius bone strength in bending, compression, and falling and its correlation with clinical densitometry at multiple sites. J Bone Miner Res 17:1629–1638
Ashizawa N, Nonaka K, Michikami S et al (1999) Tomographical description of tennis-loaded radius: reciprocal relation between bone size and volumetric BMD. J Appl Physiol 86:1347–1351
Inaba M, Nishizawa Y, Mita K et al (1999) Poor glycemic control impairs the response of biochemical parameters of bone formation and resorption to exogenous 1,25-dihydroxyvitamin D3 in patients with type 2 diabetes. Osteoporos Int 9:525–531
Kumeda Y, Inaba M, Goto H et al (2002) Increased thickness of the arterial intima-media detected by ultrasonography in patients with rheumatoid arthritis. Arthritis Rheum 46:1489–1497
Tsuda-Futami E, Hans D, Njeh CF, Fuerst T, Fan B, Li J et al (1999) An evaluation of a new gel-coupled ultrasound device for the quantitative assessment of bone. Br J Radiol 72:691–700
Iwamoto J, Takeda T, Ichimura S (2002) Forearm bone mineral density in postmenopausal women with rheumatoid arthritis. Calcif Tissue Int 70:1–8
Gough AKS, Lilley J, Eyre S et al (1994) Generalised bone loss in patients with early rheumatoid arthritis. Lancet 344:23–27
Hans D, Wu C, Njeh CF et al (1999) Ultrasound velocity of trabecular cubes reflects mainly bone density and elasticity. Calcif Tissue Int 64:18–23
Njeh CF, Fuerst T, Diessel E, Genant HK (2001) Is quantitative ultrasound dependent on bone structure? A reflection. Osteoporos Int 12:1–15
Friedlander AL, Genant HK, Sadowsky S, Byl NN, Gluer CC (1995) A two-year program of aerobics and weight training enhances bone mineral density of young women. J Bone Miner Res 10:574–585
Sambrook P, Raj A, Hunter D et al (2001) Osteoporosis with low dose corticosteorids: Contribution of underlying disease effects and discriminatory ability of ultrasound versus bone densitometry. J Rheumatol 28:1063–1067
Van Marken Lichtenbelt WD, Fogelholm M, Ottenheijim R, Westerterp KR (1995) Physical activity, body composition and bone density in ballet dancers. Br J Nutr 74:439–451
Minaur NJ, Kounali D, Vedi S, Compston JE, Beresford JN, Bhalla AK (2002) Methotrexate in the treatment of rheumatoid arthritis. II. In vivo effects on bone mineral density. Rheumatology (Oxford) 41:741–749
Cranney AB, McKendry RJ, Wells GA, Ooi DS, Kanigsberg ND, Kraag GR, Smith CD (2001) The effect of low dose methotrexate on bone density. J Rheumatol 28:2395–2399
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Inaba, M., Nagata, M., Goto, H. et al. Preferential reductions of paraarticular trabecular bone component in ultradistal radius and of calcaneus ultrasonography in early-stage rheumatoid arthritis. Osteoporos Int 14, 683–687 (2003). https://doi.org/10.1007/s00198-003-1427-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-003-1427-y