Abstract
Women are at higher risk for osteoporosis, but most of the literature examining the effect of alcohol abuse on bone mineral density (BMD) has been in men. The aim of this study was to determine differences in BMD and fracture prevalence among women in treatment for alcohol abuse, in recovery and non-alcohol-dependent women. This cross-sectional study was completed at two residential substance abuse centers in Iowa (USA). The patients were Caucasian women, aged 18–70 years, in treatment for alcohol abuse and dependence (n=228); in recovery and abstaining from alcohol (n=156); and women with no history of alcohol abuse (n=447). The main outcome measures were femoral neck and lumbar spine BMD measured by dual-energy X-ray absorptiometry (DXA); self-reported lifetime fracture prevalence. After adjusting for age and menopausal status, women in treatment had BMDs that were 7.7% (p<0.01) and 6.3% (p<0.01) lower at the femoral neck and lumbar spine, respectively, than non-alcohol-abusing women, and 4.8% lower at both bone sites (p<0.01) than women in recovery. Femoral neck BMD of women in recovery was 3.1% lower (p<0.01) than in non-alcohol-dependent women; however, the difference was not significant following multivariate analysis. Women in treatment and recovery reported more fractures during childhood and early adolescence than non-alcohol-dependent women (p<0.01). Women in recovery also reported significantly greater numbers of fractures following sobriety than their paired non-alcohol-dependent counterparts. Alcohol abuse and dependence was associated with lower femoral neck and lumbar spine BMD. Women with histories of alcohol dependence had a higher lifetime prevalence of fractures, including time periods before the onset of problem drinking and following abstinence, suggesting that factors other than acute intoxication contributed to the greater fracture prevalence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic alcohol abuse has been recognized as increasing the risk for osteoporosis and fracture [1, 2, 3, 4, 5, 6, 7, 8, 9, 10]. Alcohol in large quantities may be directly toxic to osteoblasts, reducing bone formation, or indirectly affecting bone mineral density (BMD) through several different mechanisms such as impairing liver function and altering vitamin D and calcium metabolism [1, 2, 3, 4, 7, 10, 11, 12]. The increased risk for fracture has largely been attributed to alcohol-related falls and other trauma [2, 13, 14]; however, lower BMD could increase the likelihood of fracture even in the absence of trauma. The lifetime prevalence of alcohol abuse and dependence in women has been estimated to be as high as 10% [15]. If alcohol abuse has a substantial and permanent adverse effect on BMD, then the large proportion of women with such histories may warrant earlier evaluation and intervention in order to prevent fractures and other related morbidity.
Although osteoporosis primarily affects women, most of the published information about the effect of alcohol abuse on BMD and/or fracture has been derived from studies of men. Those few studies that have included women were too small or too diverse with respect to age and menopausal status to report gender-specific analyses [2, 4, 6, 8, 16]. Potentially, chronic alcohol abuse could impact BMD and fracture risk more in women than in men. The adverse biological effects of alcohol in women are generally observed with fewer years of drinking and with lower total alcohol consumption [17, 18]. In premenopausal women, chronic alcohol abuse has been associated with amenorrhea and irregular menses potentially contributing to the achievement of lower peak BMD or compounding any alcohol-related bone loss [19, 20, 21, 22].
The purpose of this study was threefold:
-
1.
To determine if women in treatment for alcohol abuse and dependence had lower BMD than women who were not alcohol dependent, and whether the alcohol-related differences were correlated with body weight, vitamin D concentrations, liver function, selected reproductive characteristics, medical history, and/or cigarette smoking
-
2.
To consider evidence for reversibility of alcohol-related bone loss by comparing BMD of women who had previously abused alcohol, but were in recovery and abstaining, to women who never abused alcohol and women currently in treatment
-
3.
To compare lifetime fracture histories among women in treatment or recovery with non-alcohol-abusing women
Methods
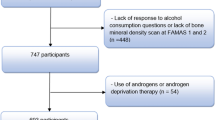
The study sample comprised 834 Caucasian women, aged 18–70 years, representing three groups: women in treatment for alcohol abuse and dependence (alcohol treatment group, n=228); women with histories of alcohol abuse and dependence, now in recovery and abstaining from alcohol (recovery group, n=156); and a group of women without a history of alcohol abuse or dependence (non-abuse group, n=447).
The alcohol treatment group was recruited from women undergoing voluntary treatment for alcohol abuse and dependence at two residential treatment centers in eastern and central Iowa. These women met at least three of the nine criteria for alcohol dependence outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-III-R) [23].
Women in the same geographic areas were recruited for the recovery group from Alcoholics Anonymous support groups, aftercare programs offered by the treatment centers, and through word of mouth. Women in the recovery group self-reported a history of alcohol abuse and dependence, had completed a formal treatment program, and had abstained from alcohol use for the 2 years prior to evaluation.
A comparison group of women with comparable data, but without an alcohol abuse history, were selected from participants in the Iowa Bone Health Study (IBHS), a population-based longitudinal study of BMD in women residing in two Iowa communities. That study population and its selection has been previously described [24]. Women from the IBHS were frequency-matched, by 5-year age group, to approximate the age distribution found in the combined alcohol treatment and recovery groups. Women who were participants in the IBHS and who reported heavy drinking, defined as consuming at least three to five drinks, four to six times or more each week, were excluded from selection (n=5). Evaluation of each of the three groups took place from 1994 to 1999. Study protocols were approved by the Institutional Review Board at the University of Iowa.
Instruments
The BMD was measured at the femoral neck, lumbar spine, and the total body by dual-energy X-ray densitometry (DPXA; Lunar Corporation, Madison, Wis.; DPX-L analysis software version 1.3y). All participants in the three groups, [alcohol treatment (n=64), recovery (n=121), or non-alcohol abuse (n=447)], from central Iowa, were measured using the same densitometer; however, because of the geographic distance, another DPX-L Lunar densitometer was used to measure BMD in those women in the alcohol treatment (n=164) and recovery groups (n=35) from eastern Iowa. Both machines were calibrated daily to evaluate scanner mechanics and quality of attenuation, and weekly using an aluminum calibration wedge in a water bath. Precision between the two densitometers, measured by comparing values for the same aluminum wedge phantom in water bath, was 1.4%. There was no difference in BMD of women in treatment or women in recovery when compared between the two study locations.
Lifetime history of fracture was assessed through detailed direct questioning specific to the anatomical site and date of fracture. Fractures of the arm, wrist, hip, spine, back ribs, or sternum were classified as osteoporotic; all others were considered non-osteoporotic. All fracture information was obtained through self-report.
For all participants, blood was drawn, non-fasting immediately prior to BMD evaluation. For women being treated for alcoholism, blood samples were obtained by venipuncture 14–16 days after admission to the treatment facility. Blood was allowed to clot for 20 min and centrifuged at 3500 rpm for 20 min. Sera was aliquoted to1-ml polypropylene vials and stored at −80°F for up to 24 months.
Liver impairment was evaluated among women in the alcohol treatment and recovery groups, with a series of liver function tests using standard automated spectrophotometric methods and included total alkaline phosphatase (ALP), aspartate aminotransferase (AST), alanine aminotransferase (ALT), gamma glutamyl transpeptidase (GGT), and total bilirubin. These analyses were completed at the University of Iowa Hospital's clinical chemistry laboratory. The day-to-day coefficients of variation (CV) ranged from 0.8 to 4.4%. Serum 25-hydroxyvitamin D (25-0H-D) and 1,25-dihydroxyvitamin D (1,25-0H-D) were measured in all women and analyzed by commercial radioimmunoassay (RIA) (Incstar Corp, Stillwater, Minn.) at the University of South Carolina. The inter-assay and intra-assay CV, combined, were less than 10% for both assays.
Participants were weighed on an electronic scale, in light clothing without shoes. The body mass index (BMI) was calculated by dividing the weight (in kilograms) by the square of the height (in meters). Body composition, measured in kilograms of fat tissue and kilograms of lean tissue, was available as a component of the total-body BMD measurement.
Demographic, reproductive, medical, and smoking histories were obtained through a structured interview. Alcohol consumption among women in treatment and recovery was ascertained using a detailed reconstruction of drinking behavior for a typical week prior to beginning treatment, with women being asked about the amount of alcohol consumed in the morning, afternoon, and evening of each day during the prior week. The amount of alcohol was recorded in standard units of measure (SUM) where one SUM equaled approximately 1 ounce (oz.) or 28.4 g of alcohol and corresponded to one beer, 4 oz. of wine, or 1 oz. of spirits (i.e., vodka or whisky). Alcohol consumption among women of the IBHS was assessed through a forced choice, quantity-frequency method, whereby participants reported the frequency of beer, wine, and spirits as never, one to three times per month, 1/week, etc., for each category, and the total number of ounces consumed with each drinking episode.
Reproductive history was characterized with a series of questions about onset of menstruation, regularity of menses, and current and lifetime amenorrhea among all participants. Women were asked about all pregnancies including the age at conception, the pregnancy outcome, the extent of breastfeeding, and the length of time prior to resumption of menses. Lifetime use of oral contraceptives, including brand names, dosages, and duration of use, was assessed with the aid of color photographs of the contraceptive compacts. In accordance with the World Health Organization's definition, women who had gone through 12 months of amenorrhea, not related to other causes, were considered postmenopausal. Women older than 51 years who had undergone hysterectomy were also considered postmenopausal.
Data analysis
All continuous variables were evaluated for normality. As appropriate, non-normally distributed variables were either log-transformed or categorized. Unadjusted and adjusted mean differences in continuous variables were determined using analysis of variance and analysis of covariance. Differences in categorical variables were evaluated with the chi-square statistics, incorporating an exact procedure when the sample size was small.
Multiple variable regression analyses were used to build models that best predicted femoral neck and lumbar spine BMD. We used a model-building process whereby separate and preliminary models were used to identify only those variables that might predict BMD. These became the variables that were evaluated for inclusion in a final set of models. All models were developed using a forward stepwise procedure. Following identification of the best-fitting model, indicator variables representing alcohol treatment, recovery, and non-alcohol-abuse groups were included to determine the impact of those variables. Least-square means was used to characterize the adjusted mean BMD between the three groups.
The age-adjusted lifetime prevalence of all fractures, as well as osteoporotic and non-osteoporotic fractures, were compared between the three groups using chi-square statistics.
A nested fracture sub-study was developed to compare the fracture frequencies occurring prior to initiation of alcohol abuse or following abstinence, and therefore not resulting from intoxication. Women in treatment and recovery were one-to-one age-matched, separately, to a non-alcohol abuse participant. For the first analysis, the age at first intoxication was identified for women in treatment and recovery, and only those fractures sustained before that age for both the treatment/non-alcohol abuse or the recovery/non-alcohol abuse pair were counted. For the second analysis, the age at last alcohol consumption was identified for women in recovery and only those fractures occurring following that age for the recovery/non-alcohol-abuse pair were counted. Matched-pairs analyses were used to determine the likelihood that women in treatment and recovery were more likely than non-alcohol-abuse participants to have had at least one fracture during the time frames corresponding to the period before drinking began or following abstinence.
Results
Alcohol consumption patterns and characteristics of participants are shown in Table 1. Women in treatment were significantly younger and less likely to have completed menopause than non-alcohol-abusing participants or women in recovery. On average, women in treatment reported 10.8 years (SD=6.9 years) of problem drinking and consumed an average of 124.6 oz. (SD=93.3 oz.) of alcohol in a typical week, during the month prior to admission. Women in recovery had, on average, 13.4 years (SD=7.4 years) of problem drinking, and while drinking, consumed an average of 110.1 oz. (SD=88.4 oz.) of alcohol in a typical week. They had abstained from alcohol for an average of 8.3 years (SD=5.7 years). In addition to alcohol, 88% of women in treatment and 84% of women in recovery reported multiple other drug use, primarily cocaine, methamphetamine, amphetamine, and marijuana. Among women without alcohol abuse, almost 25% (n=110) reported no regular consumption of alcohol of any type. More than 90% of those who drank any alcohol reported drinking less than once per week, and none reported other drug use.
Mean serum measures of liver function (AST, ALT, GGT, total ALP, and total bilirubin) were within the expected laboratory norms for all tests (Table 1). Nine women in treatment and two in recovery had elevated serum AST and ALT values. Total bilirubin was elevated in 4 (2.1%) women in treatment and 2 (1.4%) in recovery.
Bone mineral density
After adjusting for age and menopausal status, on average, the BMD in women being treated was 7.7% (p<0.01) lower at the femoral neck and 6.3% (p<0.01) lower at the lumbar spine compared with non-alcohol-abusing women (Table 2). The BMD of women in treatment was 4.8% lower (p<0.01) at both bone sites compared with women in recovery. On average, women in recovery had a femoral neck BMD that was 3.1% (p=0.01) lower than non-abusing women; however, there was no statistically significant difference between these two groups at the lumbar spine site.
Serum vitamin D
The age-adjusted mean serum 1,25-dihydroxyvitamin D was significantly lower in women undergoing treatment than the non-abusing women, but was not significantly different than the mean value of women in recovery. The age-adjusted serum 25-hydroxyvitamin-D concentrations were significantly lower among women in treatment than those in recovery or non-abusing women (Table 2). Approximately 15.3% (n=31) of women in treatment had 25-hydroxyvitamin-D concentrations that were <15 ng/ml. This was lower than, but not significantly different from, the proportion of women in recovery (11.3%, n=16), or women in the non-abuse group (10.7%, n=44) who had 25-hydroxyvitamin-D concentrations below that level.
Fractures
Approximately 60.5% of women in treatment and 63.5% in recovery reported at least one fracture in their lifetime as compared with 36.5% in the non-abusing women. Fractures were significantly more common in the treatment and recovery groups, regardless of menopausal status or type of fracture (osteoporotic vs non-osteoporotic). Women in the two alcohol groups were more likely to have sustained multiple fractures and to have had their first fracture before age 14 years (Table 2).
In the paired analyses, 54 (27%) of women in treatment and 36 (25%) of women in recovery reported having sustained a fracture prior to the age of their first intoxication. In comparison, 39 (19%) non-alcohol-abusing women paired to women in treatment and 19 (13%) non-alcohol-abusing women paired to women in recovery reported having fractured during childhood and early adolescence. Similarly, women in recovery had significantly more fractures (n=29, 20%) following sobriety than did their paired non-alcohol-abused counterparts (n=13, 9%).
Covariates
Almost all women in treatment were current smokers (n=193, 84.7%) as compared with 52.6% (n=82) of women in recovery and to 19.5% (n=87) of the non-abusing women (Table 3). Women in treatment were significantly more likely than control participants to have had their first pregnancy at age 18 years or earlier (p<0.01), to have used oral contraceptives (OC), to have initiated OC use at early age (<18 years, p<0.01), and to have experienced at least 3 months of non-pregnancy, non-menopause-related amenorrhea (p=0.01). Women in recovery were more likely than non-abusing women to have used OCs (p<0.01), to have initiated OC use at a early age (p<0.01), to report non-pregnancy, non-menopause-related amenorrhea for at least 3 months (p<0.01), and to have used estrogen supplements/hormone replacement therapy following menopause (p<0.01).
Self-reported history of liver disease, including hepatitis, was significantly greater for women in treatment (n=32, 14%) and recovery (n=13, 8.3%) than the non-abusing women (n=9, 2.0%).
Multiple variable models for BMD
Variables found predictive of femoral neck or spinal BMD in the initial modeling included age, BMI, hypertension, menopausal status, episodes of amenorrhea lasting at least 3 months (non-menopausal, non-pregnancy related), initiating use of OCs under 18 years, having a pregnancy under age 16 years, and self-reported hypertension, liver disease, or having fractured any bone prior to age 14 years. In the final models, age, lower BMI, episodes of amenorrhea lasting at least 3 months (non-menopausal, non-pregnancy related), having fractured any bone prior to age 14 years, and current alcohol dependence were consistently associated with lower BMD at the lumbar spine and femoral neck. Additionally, for the lumbar spine only, having hypertension was associated with higher BMD, whereas being postmenopausal status was associated with lower BMD. The lumbar spine and femoral neck BMD of women in treatment remained significantly lower than that of non-alcohol-dependent women after adjusting for these covariates, but the difference in hip BMD between women in recovery and non-alcohol-dependent women was lost hip (Table 4). Smoking status, 25-hydroxyvitamin D, and 1,25-dihydroxyvitamin D were not associated with BMD.
Discussion
Women who were alcohol dependent had lower BMD of the femoral neck and lumbar spine, even in the absence of biochemical evidence of liver disease. If permanent, this lower BMD (approximately 7.7% less at the femoral neck and 6.3% less at the lumbar spine) could increase the lifetime risk of fracture among these alcohol-dependent women by almost twofold [25]. This is an important increase given that as much as 10% of adult women report a lifetime history of alcohol abuse and dependence[15]. The findings of our present study confirm our previous matched case-control study where BMD of the femoral neck and lumbar spine was lower by 6.8 and 6.9%, respectively, in women who were alcohol dependent [26]. The only other study to focus specifically on women found biochemical evidence of reduced bone formation but no difference in BMD [16]. Although 176 women were included in the BMD analysis, only 19 of those women were alcohol dependent, potentially with limited power to detect significant differences if they existed. Women were included in four other studies; however, none of these studies reported gender-specific findings [2, 4, 6, 8].
Whether alcohol-related bone loss is reversed following abstinence is a critical question that has received little attention. Without baseline BMD data prior to recovery, it is not possible to characterize actual change in BMD with abstinence; however, our finding that lumbar spine and femoral neck BMD values were significantly greater for women in recovery than for women in treatment suggests that women abstaining from alcohol for at least 2 years were at less risk for osteoporosis than women in treatment. One explanation is that BMD is regained following abstinence. Alternatively, it is possible that women in treatment and recovery differed in some other quality that contributed to higher initial BMD.
No longitudinal studies have evaluated abstinence-related changes in BMD in women following recovery; however, a longitudinal study of 27 men, aged 28–61 years, found that femoral neck and lumbar spine BMD increased, after 2 years of abstinence, by 2.8 and 2.9%, respectively, in contrast to controls, whose BMD decreased by approximately 1% [27]. Cross-sectional studies comparing men who were current drinkers with former drinkers have methodological problems [small sample sizes, short periods of abstinence (6 months or less)] and inequities among study subjects with respect to age, body weight, and length of alcohol use) that compromise the interpretation of their findings [2, 3, 28, 29].
There is very little published information on fracture prevalence among people who abuse alcohol; however, the prevalence observed in our study for women in treatment (60.5%) and women in recovery (63.5%) was greater than the 32–50% prevalence reported in other studies composed primarily of men [2, 3, 13]. Without prospective fracture data, it is difficult to determine the relationship between lower BMD and fracture in our population; however, because women in recovery were more likely to have had a fracture following abstinence than aged-matched, non-abusing women during the same time period, the increased fracture risk is probably not just related to the physical act of alcohol intoxication.
We found that women in treatment and recovery reported more fractures occurring in childhood and adolescence, prior to the onset of problem drinking, than did non-abusing women during identical time periods. It may be that women with histories of alcohol abuse have risks for childhood fracture not defined by either drinking or BMD, but may instead reflect childhood nutritional or social environment of women who become alcohol dependent. It has been well documented that persons with histories of abuse and dependence are more likely to have grown up in unsupervised or abusive environments [30, 31, 32], possibly leading to a greater number of accidents and injuries. Further studies should more comprehensively evaluate the nutritional and social circumstances surrounding fractures, particularly fracture occurring at an early age.
The total number of fractures occurring before age 14 years predicted femoral neck and lumbar spine BMD as an adult, independent of alcohol group status. There could be a number of factors, including genetics, nutritional status, growth hormone dynamics, and characteristics of bone growth following fracture that could influence the attainment of maximal BMD. This latter hypothesis is supported by several investigators who have reported post-fracture reductions in BMD at non-fracture sites in alcohol-dependent and non-alcohol-dependent men [33, 34, 35].
Our study indicated that while women in treatment had lower mean serum 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D concentrations, these values were not predictive of the concurrently measured BMD, nor did the vitamin D values modify or confound the association between BMD and alcohol dependence. Most studies [2, 4, 6, 7, 16, 36], but not all studies [1, 28], have found lower 25-hydroxyvitamin D among alcohol-dependent women and men; however, in the studies that have evaluated the relationship [2, 6, 36], only one [6] reported a significant association with BMD.
While this study presents comprehensive findings from a large group of treated and recovering women, incorporating a population-based comparison group of women, it has limitations. Firstly, the information was gathered from a cross-sectional not longitudinal design. This precludes us from making definitive statements about the potential for recovery of BMD with abstinence. Secondly, in our present study fracture information was collected through self-report making it difficult to precisely delineating osteoporotic from non-osteoporotic fracture and would likely underestimate the proportion of vertebral fractures. Finally, two behaviors were confounded with alcohol treatment and recovery: almost all women in treatment and more than half of women in recovery smoked cigarettes. Likewise, alcohol was not the only drug being used; 88% of women in treatment and 84% of women in recovery reported multiple other drug use, primarily cocaine, methamphetamine, amphetamine, and marijuana. While it is unlikely that the use of tobacco and other drugs have no effect on BMD, because of the extensive co-occurrence of alcohol use and almost complete co-occurrence of other drug use, alternative models may be required to disaggregate the relative impact of both behaviors in women with abuse histories.
Conclusion
We conclude that alcohol abuse and dependence is associated with lower BMD, and may be compounded by lower body weight and amenorrhea. This lower BMD is not explained by measures of vitamin-D status or liver disease. Women with histories of alcohol abuse and dependence had a higher prevalence of lifetime fractures; however, the study suggests that factors other than acute intoxication contributed to this greater fracture prevalence. A more detailed study of the nature of fractures occurring during childhood and early adolescence, as well as the prospective evaluation of fracture incidence following recovery from alcohol, is necessary to confirm the contribution of these important findings; however, this study provides intriguing evidence that the social environment antecedent to alcohol abuse in women has a major impact in both the short-term and long-term fracture status of these women.
References
Bickle D, Genant H, Cann C, Recker R, Haloran B, Stewler G (1985) Bone disease in alcohol abuse. Ann Intern Med 103:42–48
Diamond T, Steil D, Lunzer M, Wilkinson M, Posen S (1985) Ethanol reduces bone formation and may cause osteoporosis. Am J Med 86:282–288
Crilly R, Anderson C, Hogan D, Delaquerriere-Richardson L (1988) Bone histomorphometry, bone mass and related parameters in alcoholic males. Calcif Tissue Int 43:269–276
Feitelberg S, Epstein S, Ismail F, D'Amanda C (1987) Deranged bone mineral metabolism in chronic alcoholism. Metabolism 36:322–326
Harding A, Dunlap J, Mattalina A, Azar F, O'Brien M, Kester M (1988) Osteoporitic correlates of alcoholism in young males. Orthopedics 11:279–282
Lalor B, France M, Powell P, Adams PH, Counihan TB (1986) Bone and mineral metabolism and chronic alcohol abuse. Q J Med 59:497–511
Peris P, Pares A, Guanabens N et al. (1992) Reduced spinal and femoral bone mass and deranged bone mineral metabolism in chronic alcoholics. Alcohol Alcohol 27:619–625
Schnitzler C, Solomon L (1984) Bone changes after alcohol abuse. S Afr Med J 66:730–733
Spencer H, Rubio N, Rubio E, Indreika M, Seitam A (1986) Chronic alcoholism: frequently overlooked cause of osteoporosis in men. Am J Med 393–397
Chappard D, Plantard B, Petitjean M, Alexandre C, Reffat G (1991) Alcoholic cirrhosis and osteoporosis in men: a light and scanning electron microscopy study. J Stud Alcohol 52:269–274
Farley JR, Fitzsimmons R, Taylor AK, Jorch EM, Lau KHW (1985) Direct effects of ethanol on bone resorption and formation in vitro. Arch Biochem Biophys 238:305–314
Pepersack T, Fuss M, Otero J, Bergmann P, Valsamis J, Corvilain J (1992) Longitudinal study of bone metabolism after ethanol withdrawal in alcoholic patients. J Bone Miner Res 7:383–387
Wilkinson G, Cundy T, Parsons V, Lawson-Mathew P (1985) Metabolic bone disease and fractures in male alcoholics: a pilot study. Br J Addict 80:65–68
Oppenheim W (1977) The battered alcoholic syndrome. J Trauma 11:850–856
Wilsnack S, Wilsnack R (1993) Epidemiological research on women's drinking: eecent progress and directions for the 1990s. In: Lisansky-Gomberg E, Nirenberg T (eds) Women and substance abuse. Ablex Publishing Corporation, Norwood, N.J., 62 pp
Laitinen K, Karkkainen M, Lalla M et al. (1993) Is alcohol an osteoporosis-inducing agent for young and middle-aged women? Metabolism 42:875–881
Frezza M, Padova C di , Pozzato G, Terpin M, Paranona E, Lieber C (1990) High blood alcohol levels in women. N Engl J Med 322:95–99
Lieber C (1993) Women and alcohol: gender differences in metabolism and susceptibility. Recent progress and directions for the 1990s. In: Lisansky-Gomberg E, Nirenberg T (eds) Women and substance abuse. Ablex Publishing Corporation, Norwood, N.J., 62 pp
Gavaler J, Van Thiel D (1987) Reproductive consequences of alcohol abuse: males and females compared and contrasted. Mutation Res 186:269–277
Mello N, Bree M, Mendelson J (1983) Alcohol self-administration disrupts reproductive function in female macaque monkeys. Science 221:677–679
Mello N (1988) Effects of alcohol abuse on reproductive function in women. In: Galanter M (ed) Recent developments in alcoholism. Plenum, New York, pp 253–270
Mendelson J, Mello N (1988) Chronic alcohol effects on anterior pituitary and ovarian hormones in healthy women. J Pharmacol Exp Ther 245:407–412
American Psychiatric Association (1987) Diagnostic and statistical manual of mental disorders, 3rd edn, revised. American Psychiatric Association, Washington, D.C.
Sowers MFR, Clark MK, Jannausch ML, Wallace RB (1991) A prospective study of bone mineral content and fracture in communities with differential fluoride exposure. Am J Epidemiol 133:649–660
Heaney R (1996) Pathophysiology of osteoporosis. Am J Med Sci 312:251–256
Clark K, Sowers MFR (1996) Alcohol dependence, smoking status, reproductive characteristics, and bone mineral density in premenopausal women. Res Nurs Health 19:399–408
Peris P, Pares A, Guanabens N et al. (1994) Bone mass improves in alcoholics after 2 years of abstinence. J Bone Miner Res 11:1607–1612
Laitinen K, Lamberg-Allardt C, Tunninen R, Harkonen M, Valimaki M (1992) Bone mineral density and abstention-induced changes in bone and mineral metabolism in noncirrhotic male alcoholics. Am J Med 93:642–650
Lindholm J, Steiniche T, Rasmussen E et al. (1991) Bone disorder in men with chronic alcoholism: A reversible disease? J Clin Endocrinol Metab 73:118–124
Pollock V, Briere J, Schneider L, Knop J, Mednick S, Goodwin D (1990) Childhood antecedents of antisocial behavior: parental alcoholism and physical abusiveness. Am J Psychiatr 147:1290–1293
Chermack S, Stoltenberg S, Fuller B, Blow F (2000) Gender differences in the development of substance-related problems: the impact of family history of violence and childhood conduct problems. J Stud Alcohol 61:845–852
Hanson R, Cadsky O, Harris A, Lalonde C (1997) Correlates of battering among 997 men: family history, adjustment, and attitudinal differences. Viol Vict 12:191–208
Ulivieri F, Ronzani C, Trevisan C, Montesano A, Ortolani S (1990) Quantification by dual photon absorptiometry of local bone loss after fracture. Clin Orthop 250:291–296
Nyquist F, Karlsson M, Obrant K, Nilsson JA (1997) Osteopenia in alcoholics after tibia shaft fractures. Alcohol Alcohol 32:599–604
Eyres KS, Kanis JA (1995) Bone loss after tibial fractures. J Bone Joint Surg 77B:473–478
Laitinen K, Valimaki M, Lamberg-Allardt C et al. (1990) Deranged vitamin D metabolism but normal bone mineral density in Finnish noncirrhotic male alcoholics. Alcohol Clin Exp Res 14:551–556
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Clark, M.K., Sowers, M.R., Dekordi, F. et al. Bone mineral density and fractures among alcohol-dependent women in treatment and in recovery. Osteoporos Int 14, 396–403 (2003). https://doi.org/10.1007/s00198-003-1387-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-003-1387-2