Abstract
To determine the clinical recommended dosage regimen of risedronate for the treatment of involutional osteoporosis in Japanese patients, dose-response relationships for the efficacy and safety of this drug were investigated using a multi-center, randomized, double-blind, parallel group comparative design with four dose levels of risedronate (placebo, 1 mg, 2.5 mg and 5 mg per day). A total of 211 patients diagnosed with involutional osteoporosis according to the criteria proposed by the Japanese Society for Bone and Mineral Research were randomized and received one of the four doses once daily for 36 weeks. All patients were supplemented with 200 mg of calcium daily in the form of calcium lactate. The primary efficacy endpoint was the percent change in bone mineral density of the lumbar spine (L2–L4 BMD) determined by dual-energy X-ray absorptiometry (DXA) from baseline to the time of final evaluation. Changes in biochemical markers of bone turnover and safety profile were also compared. Percent changes in L2–L4 BMD at final evaluation in the placebo, and 1-, 2.5-, and 5-mg risedronate groups were 0.79±5.30, 2.71±4.93, 5.29±3.96, and 5.15±4.25% (mean±SD), respectively. A linear dose-response relationship was obtained up to a dose of 2.5 mg, whereas no further increase in BMD was observed at 5 mg. The decrease in bone turnover markers, including N-terminal osteocalcin, phosphorus, and urinary deoxypyridinoline, also showed a linear dose-response relationship up to a dose of 2.5 mg. Alkaline phosphatase level decreased linearly up to a dose of 5 mg. Risedronate was well tolerated in this 36-week study with 1- to 5-mg doses. Neither the overall incidence of adverse events nor the percentage of patients without problem in overall safety assessment differed significantly among the dose groups including the placebo group. Based on these results, a once-daily dose of 2.5 mg of risedronate, which is half that used in Caucasians, is recommended for the treatment of involutional osteoporosis in Japanese patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
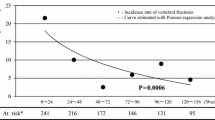
Osteoporosis characterized by the loss of bone mass and deterioration of microarchitecture is one of the common causes of disability in elderly people due to the occurrence of bone fractures. Recent progress in the treatment of osteoporosis has enabled successful reduction of fracture in these patients. Among the several regimens used for the treatment of osteoporosis, bisphosphonates, such as alendronate and risedronate, have been reported to reduce the vertebral fractures in the Caucasian population [1, 2, 3]. Hip fractures are also reduced in postmenopausal women with established osteoporosis [4, 5]. Based on the results obtained in these studies, a once-daily dose of 10 mg alendronate or 5 mg risedronate has been recommended for the treatment of osteoporosis; however, in the case of alendronate, which was recently launched in Japan, a daily dose of 5 mg was recommended for Japanese patients, compared with 10 mg for Caucasians [6, 7]. Although the exact reason why the daily dose of alendronate in Japanese patients should be half that for Caucasians is not fully understood, this difference in recommended dose of alendronate might also apply to risedronate.
In the previous preliminary study, the effect of risedronate on lumbar bone mineral density was examined using placebo, 1 and 5 mg a day [8]. A dose-related increase in lumbar bone mineral density (BMD) was observed. To confirm these preliminary results and to determine the recommended dose of risedronate, we more extensively investigated dose-response relationships for lumbar BMD (L2–L4 BMD) and tolerability of risedronate using three dose levels (1, 2.5, and 5 mg) together with placebo in Japanese patients with osteoporosis.
Subjects and methods
Study design
This randomized, double-blind, parallel group comparative dose-ranging study was conducted at 70 medical institutions throughout Japan between September 1995 and March 1997. The study protocol was approved by each Institutional Review Board prior to initiation of the study, and all patients gave written informed consent before participating in the study, which was conducted in compliance with Good Clinical Practice and in accordance with the spirit of the Declaration of Helsinki.
Eligible patients were randomly assigned to receive one of three doses of risedronate (1, 2.5, and 5 mg/day) or placebo for 36 weeks. All patients were supplemented with a daily dose of 1.54 g of calcium lactate (equivalent to 200 mg of elemental calcium). Tablet formulations of the three doses of risedronate and placebo were identical in appearance. Patients were requested to take one tablet immediately after arising every morning and not to take any food or beverage other than water for 30 min post-administration. Calcium supplementation was given once daily after supper. The patients and investigators, as well as the study coordinating staff, were kept blind to the treatment assignments throughout the treatment period. Concomitant use of any drug known to affect bone metabolism was prohibited.
Patient selection
Ambulatory patients of either gender aged 40–75 years with involutional osteoporosis (senile and postmenopausal) were eligible if they met the criteria which was determined using the diagnostic criteria for involutional osteoporosis established by the Longevity Science Research Project of the Ministry of Health and Welfare, Japan (inclusion criteria 1). The cutoff values of L2–L4 BMD were set at 2.5 SD below the YAM for female and 3.5 SD below YAM for male patients. The actual cutoff values of L2–L4 BMD for instruments used for determination of BMD were set as follows: BMD (g/cm2) corresponding to YAM 2.5 SD for Hologic QDR, Norland XR, and Lunar DPX types were 0.82, 0.80, and 0.94, respectively, and those corresponding to YAM –3.5 SD were 0.74, 0.71 and 0.85, respectively.
Since a new diagnostic standard for primary osteoporosis was established by the Japanese Society for Bone and Mineral Research in 1995 [9], the revised cutoff values of BMD for the selection of patients were applied after February 1996 (inclusion criteria 2). According to the revised criteria, the cutoff values of L2–L4 BMD were set at YAM –2.5 SD in cases without vertebral fracture, or YAM –1.5 SD in cases with vertebral fractures. The actual cutoff values of L2–L4 BMD by instruments used for determination of BMD were set as follows: BMD (g/cm2) corresponding to YAM –2.5 SD for Hologic QDR, Norland XR, and Lunar DPX types were 0.71, 0.70, and 0.83, respectively, and those corresponding to YAM –1.5 SD were 0.83, 0.84, and 0.98, respectively. Patients whose postmenopausal period was less than 10 years could be included in the study if their L2–L4 BMD was less than YAM –1.5 SD.
Patients with any of the following conditions were excluded: secondary osteoporosis or osteopenia or osteomalacia; serious renal, hepatic, or cardiac diseases; malignant tumor under treatment with any anti-tumor agent; history of radiotherapy of the lumbar spines and pelvis; drug hypersensitivity; or past experience with bisphosphonate therapy. In order to avoid interference with BMD determination by DXA, patients with spinal deformity or severe spinal scoliosis, or with fractures, severe deformity, or findings of osteosclerosis of any of L2–L4 were excluded from the study. Patients who were given any drugs known to affect bone metabolism within 8 weeks before entry to the study were also excluded.
Measurements
The primary efficacy endpoint was percent change in mean L2–L4 BMD from baseline to the time of final evaluation. L2–L4 BMD was determined at baseline and 12, 24, and 36 weeks after starting therapy or at the time of withdrawal by dual-energy X-ray absorptiometry (DXA) with the use of QDR type (Hologic, Waltham, Mass.), XR type (Norland, Fort Atkinson, Wis.), or DPX type (Lunar, Madison, Wis.) instruments. The validity of each DXA measurement was assessed by the Central DXA Assessment Committee. At the time this study was conducted, technical issues precluded BMD measurements at the femoral neck and for total hip.
As the secondary endpoints, biochemical markers, including calcium (Ca), phosphorus, alkaline phosphatase (Al-P, colorimetric method), parathyroid hormone (PTH-intact, IRMA; Allegro intact PTH, Sumitomo Seiyaku Biomedical Co., Osaka, Japan) [10], N-terminal osteocalcin (EIA; Teijin, Tokyo, Japan) [11], and 1α,25-dihydroxyvitamin D (1α,25(OH)2D, radioreceptor assay) [12] in serum, and Ca and deoxypyridinoline (DPD, measured by HPLC) [13] in urine, were determined at baseline and 4, 12, 24, and 36 weeks after initiation of therapy. All measurements of these parameters were carried out by Teijin Bio Laboratories (Tokyo), and serum and urine samples were kept frozen at –20°C or lower until analyzed. Urinary parameters were normalized by urinary concentration of creatinine (CRN).
Safety assessment
The objective symptoms and subjective signs related to adverse events were monitored by noting complaints at each visit. Standard laboratory tests, including hematology, blood biochemistry, and urinalysis, were carried out at each institution at baseline, 4, 12, 24, and 36 weeks after initiation of treatment or at the time of withdrawal. All adverse events encountered during the treatment period were documented, including time of onset, duration, severity, outcome and causal relationship to the test drug.
Statistical analysis
The primary endpoint of efficacy and safety in this study were the percent change in L2–L4 BMD from baseline to the time of final evaluation and overall safety assessment, respectively. Per-protocol-set (PPS) analyses were performed for the primary endpoint, and the robustness was confirmed by subsequent full analysis set (FAS). The baseline characteristics and homogeneity in patient background were compared by analysis of variance (ANOVA). Based on the results from the early phase-II study [8], the percent changes in L2–L4 BMD after 36-week administration were estimated to be 0.8, 3.8, 5.0, and 5.0% in the placebo, and 1, 2.5, and 5 mg risedronate group, respectively. The standard deviation in each group was assumed to be 6%. To test dose-response relationships, percent changes in L2–L4 BMD at the time of final evaluation in the four dose groups were analyzed by ANOVA (one-tailed) using three different sets of contrast coefficients, i.e., (a): (−17, −9, 3, 23); (b): (−3, −1, 2, 2); and (c): (−3, 1, 1, 1). Each set of contrast coefficiencies represents the hypotheses of a linear dose-response relationship, dose-response up to a dose of 2.5 mg with no greater response at 5 mg, and a greater response than placebo but no dose-response relationship among the dose groups of risedronate, respectively. The Bonferroni's method was used to adjust multiplicity in examining the contrasts. Under these conditions, the patient number of PPS necessary to generate statistical significance in the contrast efficiency of (−3, −1, 2, 2) with a 90% probability was estimated at 41 patients; thus, considering possible withdrawals and dropouts, the target enrollment for this study was determined at 50 patients for each group. The regression line for changes in L2–L4 BMD over time was estimated individually by the least-squares method, and the slope of the line for each dose group was analyzed to determine dose-response relationship as described above. The dose-response relationships for bone turnover markers at the time of final evaluation were analyzed in similar fashion. The paired t-test was used for rate or amounts of post-dose change in BMD and bone turnover markers. The Chochran-Armitage test (one-tailed) was used for the incidence of adverse events and overall safety assessment. Unless otherwise mentioned, the significance level was set at 5% (two-tailed).
Data handling
The handling of data from individual patients, i.e., determining which patients should be included in or excluded from the data analysis, was discussed and settled before breaking of the key code at the Data Handling Committee consisting of the chief investigator, statistician, and members of the Steering Committee and the Central DXA Assessment Committee.
Results
Patient disposition
A total of 211 patients were included in the study (placebo, n=54, 1 mg, n=52, 2.5 mg, n=49, and 5 mg, n=56). Among them, a total of 36 patients were withdrawn or dropped out and 175 patients (placebo, n=45, 1 mg, n=44, 2.5 mg, n=39, 5 mg, n=47, respectively) completed the planned schedule.
Of the patients enrolled, 8 were excluded from the safety analysis because of insufficiency of medication period (<28 days) and no adverse events occurred, and an additional 35 patients were excluded from BMD analysis because of protocol violations (Fig. 1). As a result, the numbers of patients subjected to the PPS analyses of BMD and safety were 168 and 203, respectively. There were no significant deviations among the dose groups in the ratio of the patients excluded from analyses. The FAS population for additional analyses of BMD and safety were 187 and 210, respectively.
Demographic and baseline characteristics
Table 1 shows demographic and baseline characteristics for the PPS analysis of L2–L4 BMD. The majority of patients were female, and only 2 male patients were included. There were 101 subjects and 67 subjects who met inclusion criteria 1 and 2, respectively, for the diagnosis of osteoporosis, and these two groups' mean baseline T-scores for L2–L4 BMD did not differ significantly, with –2.91 and –2.81, respectively (p=0.285). Of the subjects enrolled according to the inclusion criteria 2, 24 cases were women with reduced BMD (below YAM –1.5 SD) whose postmenopausal period was <10 years. The four treatment groups were well balanced with regard to demographic and other baseline characteristics.
Bone mineral density
As shown in Fig. 2, the percent changes from the baseline in L2–L4 BMD at the time of final evaluation (PPS analysis) in the placebo and 1-, 2.5-, and 5-mg risedronate groups were 0.79±5.30, 2.71±4.93, 5.29±3.96, and 5.15±4.25% (mean±SD) of the basal value, respectively. Of the 168 subjects evaluated for changes in BMD, 161 had DXA data at week 24 or any time point thereafter, and the final evaluation was conducted with the last DXA data obtained from these 161 subjects. The dose-response relationship was studied by ANOVA using three different sets of contrast coefficients representing the following three hypothetical dose-response patterns as described in the Subjects and methods section. All the cases of the hypotheses were significant (p≤0.001). In particular, the effect of risedronate on L2–L4 BMD exhibited a saturable pattern, since no further increase in L2–L4 BMD was observed in a group treated with 5 mg/day of risedronate. In fact, the F value in case (b) was highest, suggesting that 2.5 mg/day of risedronate is the best minimal dose to treat osteoporosis based on efficacy in improving BMD. The result of FAS analysis conducted with all available data (n=187) yielded the same conclusion. The time-course changes in mean L2–L4 BMD expressed as percentage changes from the baseline value are shown in Fig. 3. In all groups other than the placebo, significant increases in L2–L4 BMD were observed at 12 weeks of treatment and thereafter. For secondary analysis of dose-response relationship, the regression line of the percentage change in L2–L4 BMD over the time of observation was estimated for each patient and the mean slopes for treatment groups were analyzed using ANOVA as described previously. The results yielded the same conclusion for changes in L2–L4 BMD at the time of final evaluation as for the analysis of PPS (data not shown).
Biochemical markers
Figure 4 shows the percentage changes in bone turnover markers from the baseline values. Urinary DPD/CRN (Fig. 4a) significantly decreased after 4-week treatment, and the significant declines in this bone resorption marker were maintained during the treatment period in a dose-related manner. The mean percentage changes from the baseline value at 36-week treatment in the 1-, 2.5-, and 5-mg risedronate groups were –15.7, –33.0, and –39.0%, respectively. The same trends were also observed in changes in serum levels of N-terminal osteocalcin (Fig. 4b) and Al-P activity (Fig. 4c); however, in contrast to the response of deoxypyridinoline, early responses (4-week) of bone formation markers to risedronate treatment were not observed, but significant decreases were noted at 12 weeks of treatment and thereafter.
The changes in serum and urinary biochemical markers related to calcium metabolism are shown in Fig. 5. In the highest dose risedronate group (5 mg/day), transient but significant changes in serum levels of Ca, phosphorus, PTH-intact, and 1α,25(OH)2 D were observed. The groups receiving 1 or 2.5 mg/day of risedronate did not exhibit concomitant changes in serum level of calcium or calcium-regulating hormones.
Dose-response patterns of these biochemical markers at the time of final evaluation were examined using the same procedure as for changes in BMD. Dose response of Al-P fitted well to a linear dose-response relationship, and those of urinary deoxypyridinoline, N-terminal osteocalcin, and phosphorus fitted well to a linear dose-response relationship up to a dose of 2.5 mg. Serum Ca demonstrated a pattern in which the response was greater than placebo but not dose related. No significant dose-response relationship was observed for serum PTH-intact, 1α,25(OH)2D, and urinary Ca/CRN (data not shown).
Safety assessment
The overall incidence of adverse events did not differ significantly among the treatment groups including placebo (p=0.170). The most frequently reported adverse events were gastrointestinal symptoms, and most were mild in severity (Table 2). The incidence of abnormal changes in clinical laboratory variables did not differ among the treatment groups (p=0.779). There were no serious adverse drug reactions.
As the primary endpoint for safety, overall safety assessment is given in Table 3. The percentages of patients with no problem in safety in the placebo and 1-, 2.5-, and 5-mg risedronate groups were 76.5, 86.0, 72.9, and 75.5%, respectively. No dose-response relationship was detected with the Cochran-Armitage test (p=0.272).
The results of FAS analysis were consistent with the aforementioned results.
Discussion
The aim of the present study was to determine the recommended dosage regimen of risedronate in Japanese patients with involutional osteoporosis. The efficacy and safety of risedronate in patients with postmenopausal osteoporosis have been extensively studied mainly in North America and Europe [1, 2, 5, 14], and it has been demonstrated that a once-daily dose of 5 mg risedronate consistently increased BMD and decreased the risk of fracture, whereas no clinically relevant differences in safety were observed compared with the 2.5-mg dose. The 5-mg dosage regimen was therefore recommended in these regions; however, due to interracial differences in genetic factors that may affect the safety and efficacy of the drug, the dosage regimen is not universal, and it is not always appropriate to apply the dosage regimen recommended for Caucasians to the treatment of Asians. In fact, a study conducted in Japan in which the safety and efficacy of alendronate were compared with those of alfacalcidol in Japanese patients with postmenopausal osteoporosis revealed that alendronate increased L2–L4 BMD at a daily dose of 5 mg to a comparable extent to that obtained in Caucasians at a dose of 10 mg [7].
The present study demonstrated that L2–L4 BMD in patients with involutional osteoporosis increased dose dependently up to a daily dose of 2.5 mg risedronate, and no further increase was observed at a higher dose of 5 mg (percent changes from baseline at the time of final evaluation in the placebo, 1-, 2.5-, and 5-mg risedronate groups were 0.79, 2.71, 5.29, and 5.15%, respectively). The percent increase in L2–L4 BMD after 6 months of treatment was 3.57% in the present study conducted in Japanese patients (treated at 2.5 mg/day) and 3.3% in a foregoing European study [14] conducted in patients (treated at 5 mg/day) whose characteristics (background data) were similar to those of the Japanese patients. This fact indicates that, in the same manner as observed with alendronate, risedronate administered at a dose one-half of the dose for Caucasians would show an equivalent effect in Japanese patients.
Risedronate was well tolerated in this 36-week study with 1- to 5-mg doses, and no serious adverse drug reactions were encountered. The overall incidence of adverse events did not differ among the dose groups including placebo. Although the incidence of subjective adverse drug reactions was statistically significant among the dosing groups (p=0.050), this difference was not considered clinically significant, and these events were mild or moderate. The blood Ca level decreased significantly, although apparently transiently, in the 5-mg risedronate group, and suggests the possibility that the drug prolongs secondary hyperparathyroidism to a greater extent in populations such as the Japanese, with lower Ca intake [15].
The reason for the difference in recommended dosage regimen between Japanese and Caucasians remains to be elucidated, but the pharmacokinetic data may partly explain this difference. When comparing the pharmacokinetic data obtained in separate studies in Japanese and Caucasian healthy subjects, time-course profiles of blood concentrations following single oral administration of 2.5 mg of risedronate in Japanese subjects was almost comparable to those obtained in Caucasians given 5 mg [16, 17]. Moreover, Cmax and area under the curve obtained at 2.5- and 5-mg doses showed two to three times higher in Japanese as compared with those obtained in Caucasians, suggesting that risedronate may be absorbed more efficiently in Japanese than in Caucasians.
Published data on risedronate support efficiency for the 2.5-mg dose [1, 2]. The 2.5-mg arm in these studies was discontinued because data from other risedronate trials indicated that the 2.5-mg dose seemed to be less efficacious than 5 mg in Caucasian populations [18]. Considering the high absorption rate in Japanese population, these data are encouraging and lend further support that the 2.5-mg dose in Japanese will be effective in reducing the incidence of osteoporotic fractures.
Based on these results, we conclude that a once-daily dose of 2.5-mg risedronate is effective in increasing L2–L4 BMD and inhibiting bone resorption in Japanese patients with involutional osteoporosis. Also with consideration to the effect on calcium metabolism, risedronate was well tolerated at this dose level, and a once-daily dose of 2.5 mg is recommended as the standard dosage regimen in Japan.
References
Harris ST, Watts NB, Genant HK et al. (1999) Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis, a randomized, controlled trial. J Am Med Assoc 282:1344–1352
Reginster J-Y, Minne HW, Sorensen OH et al. (2000) Randomized trial of the effects of risedronate on vertebral fractures in women with established postmenopausal osteoporosis. Osteoporos Int 11:83–91
Liberman UA, Weiss SR, Broll J et al. (1995) Effect of oral alendronate on bone mineral density and the incidence of fracture in postmenopausal osteoporosis. N Engl J Med 333:1437–1443
Black DM, Cummings SR, Karpf DB et al. (1996) Randomised trial of effect of alendronate on risk of facture in women with existing vertebral fractures. Lancet 348:1535–1541
McClung MR, Geusens P, Miller PD et al. (2001) Effect of risedronate on the risk of hip fracture in elderly women. N Engl J Med 344:333–340
Nakamura T, Kushida K, Shiraki M et al. (1998) A placebo-controlled, double blind study to determine the appropriate alendronate dosage in Japanese patients with involutional osteoporosis, and postmenopausal osteopenia or artificially menopausal women. Med Consult New Remedies 35:3–17 [in Japanese]
Shiraki M, Kushida K, Fukunaga M et al. (1999) A double-masked multicenter comparative study between alendronate and alfacalcidol in Japanese patients with osteoporosis. Osteoporos Int 10:183–192
Kishimoto H, Kushida K, Shiraki M et al. (2002) A clinical trial evaluating the efficacy and safety of risedronate (NE-58095) in patients with involutional osteoporosis or bone mineral content loss associated with lack of ovarian function: early phase II study of NE-58095. Osteoporosis Jpn 10:61–83 [in Japanese]
Orimo H, Sugioka Y, Fukunaga M et al. (1995) The Committee of the Japanese Society for Bone and Mineral Research for Development of Diagnostic Criteria of Osteoporosis. Diagnostic criteria of primary osteoporosis. Osteoporosis Jpn 3:669–674 [in Japanese]
Brown RC, Aston JP, Weeks I et al. (1987) Circulating intact parathyroid hormone measured by a two-site immunochemiluminometric assay. J Clin Endocrinol Metab 65:407–414
Eguchi H, Hosoda K, Kurihara N et al. (1995) Sandwich immunoassay specific for the N-terminal sequence of osteocalcin. J Immunol Methods 184:213–240
De Leenheer AP, Bauwens RM (1985) Comparison of a cytosol radioreceptor assay with a radioimmunoassay for 1,25-dihydroxyvitamine D in serum or plasma. Clin Chim Acta 152:143–154
Black D, Dunkan A, Robins SP (1988) Quantitative analysis of the pyridinium crosslinks of collagen in urine using ion-paired reverse-phase high-performance liquid chromatography. Anal Biochem 169:197–203
Fogelman I, Ribot C, Smith R et al. (2000) Risedronate reverses bone loss in postmenopausal women with low bone mass: results from a multinational, double-blind, placebo-controlled trial. J Clin Endocrinol Metab 85:1895–1900
Laboratory of Informatics on Health and Nutrition (1999) Sixth revision of recommended dietary allowances (RDA) for the Japanese: dietary reference intakes. Dai-ichi Shuppan Publishing, Tokyo [in Japanese]
Ogura Y, Gonsyo A, Tei M et al. (in press) Phase I clinical trial of risedronate sodium (NE-58095) hydrate: single and multiple oral dose studies. J Bone Miner Metab
Mitchell DY, Eusebio RA, Sacco-Gibson NA et al. (2000) Dose-proportional pharmacokinetics of risedronate on single-dose oral administration to healthy volunteers. J Clin Pharmacol 40:258–265
McClung M, Bensen W, Bolognese M et al. (1998) Risedronate increases bone mineral density at the hip, spine, and radius in postmenopausal women with low bone mass. Osteoporos Int 8 (Suppl 3):111
Author information
Authors and Affiliations
Appendix
Appendix
Committee Members of the Risedronate Late Phase II Study Group
The committee members of the Risedronate Late Phase II Study Group are:
-
Principal Investigator: H. Orimo
-
Steering Committee: Y. Taketani, H. Minaguchi, T. Inoue, R. Morita, H. Morii, K. Yamamoto
-
Central Assessment Committee: K. Kushida, M. Shiraki, M. Fukunaga, H. Kishimoto
-
Controller: Y. Ohashi
Other members of the Risedronate Late Phase II Study Group
The remaining members of the study group are listed in Table 4.
Rights and permissions
About this article
Cite this article
Shiraki, M., Fukunaga, M., Kushida, K. et al. A double-blind dose-ranging study of risedronate in Japanese patients with osteoporosis (a study by the Risedronate Late Phase II Research Group). Osteoporos Int 14, 225–234 (2003). https://doi.org/10.1007/s00198-002-1369-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-002-1369-9